Chapter 11- Book Integrated dynamics of innate and adaptive immune system
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
Innate lymphoid cells
ILCs
Lack antigen specific receptors
SImilar to CD4 + CD9 T cells
Most abundant in barrier tissues
Primary immune response vs secondary response
Primary: When a pathogen is encountered for the first time
Secondary: second time, provides long time protection through immunological memory
Acute infection stages
Infectious agent colonizes and replicates- the innate immune system is initiated after detection
Antigen presentation by dendritic cells to lymphocytes→ adaptive immune response is triggered→ pathogen continuous to grow, restrained by innate response. AT this stage: immunological memory starts to be induced.
After 4-7 days effector cells and molecules of the adaptive immune response begin to contribute to the host response and act to clear infection.
When infection has been cleared an antigen becomes undetectable → immune response ceased but antibodies and T and B memory cells provide lasting protection.
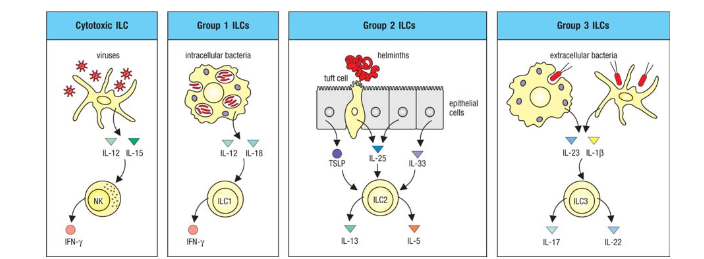
ILCs
Cytokines produced by innate sensor cells activate ILCs
Cytotoxic ILCs: Viruses→IL-12 and IL- 15 → NK cell→ IFN-gamma
Group 1 ILCs: Intracellular bacteria→ IL-12 and IL-18 → ILC1→ IFN-gamma
Group 2: Parasites→ ILC2→ IL-13 and IL-5
Group 3: Extracellular bacteria→ ILC3→ Il-17 and IL-22
Innate sensor cells
Secrete cytokines which activates ILCs which secreted cytokines
Ex: dendritic cells, macrophages, epithelial cells
ILCs + T helper cells
ILC cells and TH cells coordinate their functions to eradicate the pathogen
ILC1 and TH1→ macrophages are enhanced
ILC2 and TH2→ enhance eosinophils, basophils and mast cells
ILC3 + TH17→ enhance neutrophils
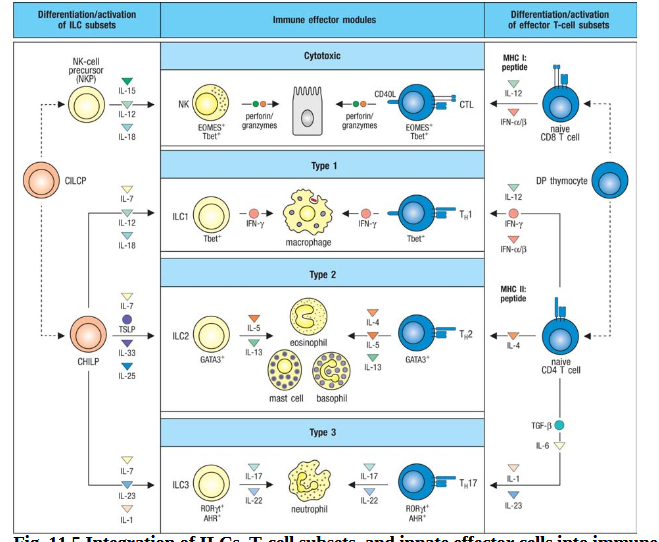
Cytotoxic response
Characterized by actions of NK cells and CTLs→ specialized in killing cells with intracellular pathogens, stressed or damaged cells, tumor cells.
NK cells can be armed by IgG for ADCC
Produce IFN-gamma→ activated macrophages
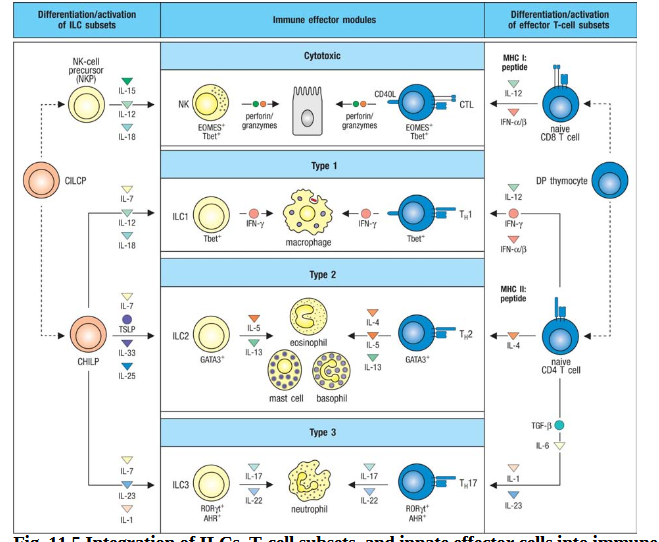
Type 1 response
Characterized by ILCs (group 1), YH1 cells → opsonizing IgG antibody isotypes and macrophages
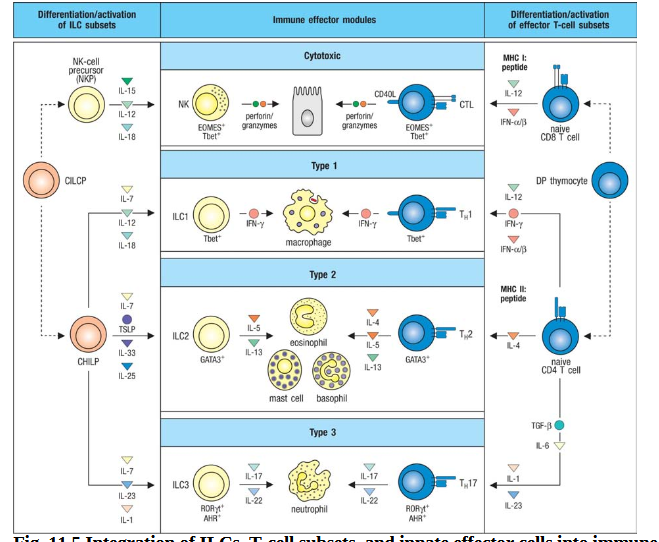
Type 2 response
Characterized by ILC (group 2), TH2, IgE, innate effector cells: eosinophils, basophils, mast cells
Induced by multicellular parasites
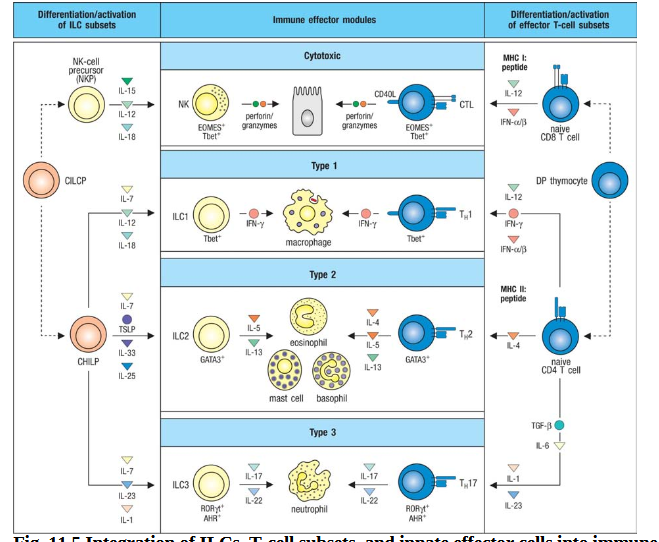
Type 3 response
Characterized by ILCs (group 3), TH17, opsonizing IgG isotypes, neutrophils
Respond to extracellular fungi or bacteria
Characterization of ILCs
Respond rapidly
Expand in number
Nonmotile→ bind barriers
NK cells
Produce IFN-gamma
Cytotoxic granules with perforin and granzymes
Circulate the blood
Mobile
Inhibitory and activating receptors
Have no antigenic receptors but can by IgG to their Fc receprtor
TH1 + ILC1
Lack cytotoxic granules
Clearance of intracellular mostly
Release IFN-gamma
IL-12 + IL-18→ induce ILC1 production of IFN-gamma→ induce killing through macro
ILC3
Extracellular bacteria and fungi
Th17
Responsive to IL-23, IL-1Beta→ leads to IL-17 and IL- 22
Activation of ILCs
Innate sensor cells produce (when pathogen invades) cytokines which activates the ILCs→ recruit innate effector cells before CD4 and CD8 cells arrive (work similar)
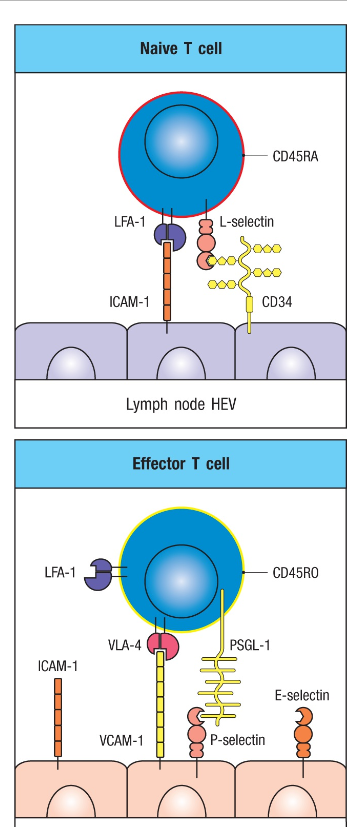
Effector T cells and adhesion
Change their surface molecules allowing them top sites of infections
Naive T cells stay in lymph nodes through binding of L-selectin to carbohydrates on HEV
After encounter with pathogen many diff effector cells loose L-selectin→ leave the lymph and express VÖA-4 instead (integrin) + LFA-1 which bind to VCAM-1 and ICAM-1 in infected site
TH1 response-macrophages
Enhance macrophages to kill their intracellular pathogen
Heighten their microbicidal function
Macro display peptide on MHC class 2 molecules→ TH1 cells recognize
Require signal by IFN-gamma R + IFN gamma, CD40+CD40L
MHC class 2 peptide+ TH1
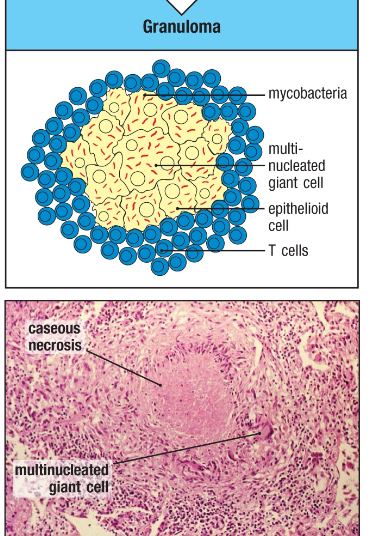
Granulomas
Pathogens incompletely killed by a TH1 response in macrophage
Gives rise to a chronic, low level infection that requires an ongoing TH1 response to limit the spread of pathogen
Granuloma is formed=microbes are held in a macro surrounded by activated lymphocytes
Fuse of macro leads to multinucleated giant cells
TH2 response
In response to helminths and parasites
TH2 cells produce IL-13 induce mucus→ prevents adherence
Recruits macrophages + mast cells
Generation of IgE→ binds FC epsilon R on mast cells, eosinophils, basophils→ antigen specific recognition and activation
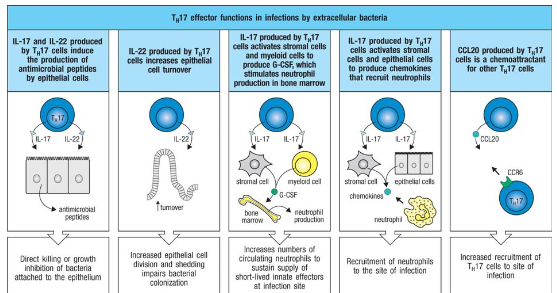
Th17 cells and type 3 response
Clearance of extracellular bacteria and fungi
Produces IL-17
Production of antimicrobial peptides, chemokines
What happens with T effector cells after infection is cleared?
When a pathogen is eliminated→ antigen is gone→ most T effector cells undergo apoptosis
The cells that survive turn to be memory T cells
Intrinsic pathway of apoptosis:IL-2 production loss + loss of IL2R→ apoptosis
Extrinsic (death) patway of apoptosis→ Fas signaling → DISC→ apoptosis
Memory T cells subsets
Central memory T cells
Effector memory T cells
Tissue resident memory T cells
Express IL-7Ralfa→ respond to pro survival cytokine Il-7
Difference: Naive T cell require signals from self peptide: self MHC and IL7 for survival
Effector memory T cells→ require IL-7 but not as dependent on peptide:self MHC for survival
Memory B cells
Response is more rapid and higher affinity for antigen when memory B cells are present and not naive
Arise from GC reaction during a primary response and may have undergone isotype switching + somatic mutations OR not from GC reaction
Memory B cell marker: class switching IgG, IgA or IgE, CD27
Naive marker: IgM and IgD