Gas Exchange
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
What is Minute ventilation (VE)?
The total air entering the lungs per minute.
VE = TV x Breathing Frequency
VE = 500 mL x 12 breaths/min = 6 L/min
What is Alveolar ventilation (VA)?
Accounts for air reaching the alveoli that’s available for gas exchange.
VA = (TV - Dead space) x Breathing frequency
VA = (500 mL - 150 mL) x 12 breaths/min = 4.2 L/min
What is dead space (DS)?
It is the fraction of tidal volume that does not participate in gas exchange:
Anatomical DS: about 150 mL, parts of the respiratory system that does not partake in gas exchange due to their anatomical position, like the trachea and bronchi
Physiological DS: includes anatomical dead space, and alveolar dead space = alveoli not partaking gas exchange due to dysfunctionality/poor blood flow
In healthy individuals, alveolar DS is 0
Barometric pressure of gases
Barometric (atmospheric) pressure at sea level is around 760 mmHg, consisiting of atmospheric gases: N2 (79%) and O2 (21%)
Partial pressure = Absolute pressure x gas (%)
PN2 = 760 × 0.79 = 600 mmHg
PO2 = 760 × 0.21 = 160 mmHg
At increasing altitudes, the barometric pressure decreases:
4000m → 460 mmHg
8800m → 253 mmHg
What are the alveolar gas pressures?
Alveolar PO2 = 195 mmHg
Alveolar PCO2 = 40 mmHg
Why do alveolar partial pressures not match barometric?
Alveolar partial pressures does not match ambient air partial pressures because our ventilation frequency is not large enough to renew the alveolar air with each breath fast enough, and tissues consume O2 and produce CO2.
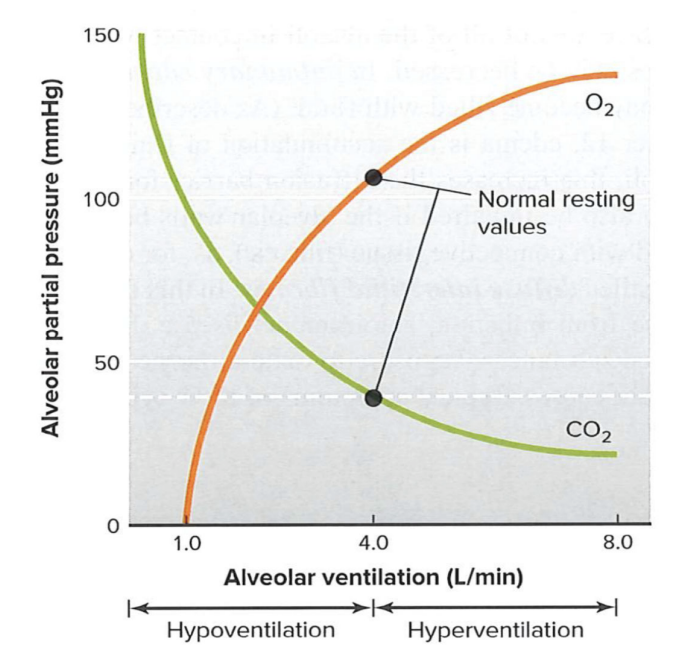
What is Hypoventilation and Hyperventilation?
Hypoventilation: when metabolic CO2 exceeds what alveolar ventilation can eliminate
Hyperventilation: when alveolar ventilation exceeds the rate of metabolic CO2 production
Not the same as increased ventilation during exercise, where alveolar ventilation matches the demand of expelling CO2 production
What does Henry’s Law state?
Gases dissolve in liquid in proportion to their partial pressure, moving from high to low. At equilibrium, partial pressures are equal.
Gas exchange: Alveoli ←→ Blood
Deoxygenated blood arriving from pulmonary arteries:
PO2: 40 mmHg
PCO2: 46 mmHg
Oxygenated blood leaving from pulmonary veins:
PO2: 100 mmHg
PCO2: 40 mmHg
In healthy individuals, rates of O2 and CO2 diffusion are high enough and blood flow slow enough to reach equilibrium. Net diffusion stops when capillary and alveoli partial pressures are equal (oxygenated blood gas pressures = alveolar gas pressures).
Gas transport: Blood ←→ Tissues
Tissue metabolism consumes O2 and produces CO2, creating a concentration gradient of low PO2 and high PCO2 in tissues
Mitochondria uses O2, lowest PO2 <5 mmHg
O2 travels from blood to tissue, down its partial pressure gradient
Capillary → interstitial fluid → cell → mitochondria
CO2 diffuses oppositely, from tissue to blood
Mitochondria → cell → interstitial fluid → capillary
What is ventilation-perfusion mismatching, and what are two mechanisms to counter it?
Ventilation-perfusion mismatching is the cause for inadequate gas transfer, and is countered by:
Oxygen driven vasoconstriction
In tissues, low PO2 leads to vasodilation to increase perfusion and O2 delivery to working cells
However, in alveoli, low PO2 leads to vasoconstriction to divert blood to better-ventilated alveoli with higher PO2
CO2-driven bronchoreactivity
If blood flow to the lungs decreases, e.g. due to blood clot, the drop in PCO2 triggers bronchoconstriction to decrease air flow and reduce ventilation to poorly perfused areas
How does high altitude cause lung edema?
At high altitudes, the barometric pressure (and thus PO2) is decreased, leading to reduced alveolar and arterial PO2
In response, pulmonary arterioles constrict
Normally, this helps to divert blood to better ventilated alveoli, but at high altitudes, all alveoli are hypoxic
Widespread vasoconstriction raises resistance in pulmonary circulation and leads to elevated pulmonary blood pressure
High pressure forces fluid out of capillaries into the interstitial space and into alveoli, and its accumulation results in lung edema