Pharmacology for Nurses Chapter 26
5.0(1)
Card Sorting
1/91
Earn XP
Description and Tags
Michael P. Adams, Norman Holland, Carol Quam Urban - Pharmacology for Nurses_ A Pathophysiologic Approach (2020)
Last updated 5:16 PM on 2/20/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
92 Terms
1
New cards
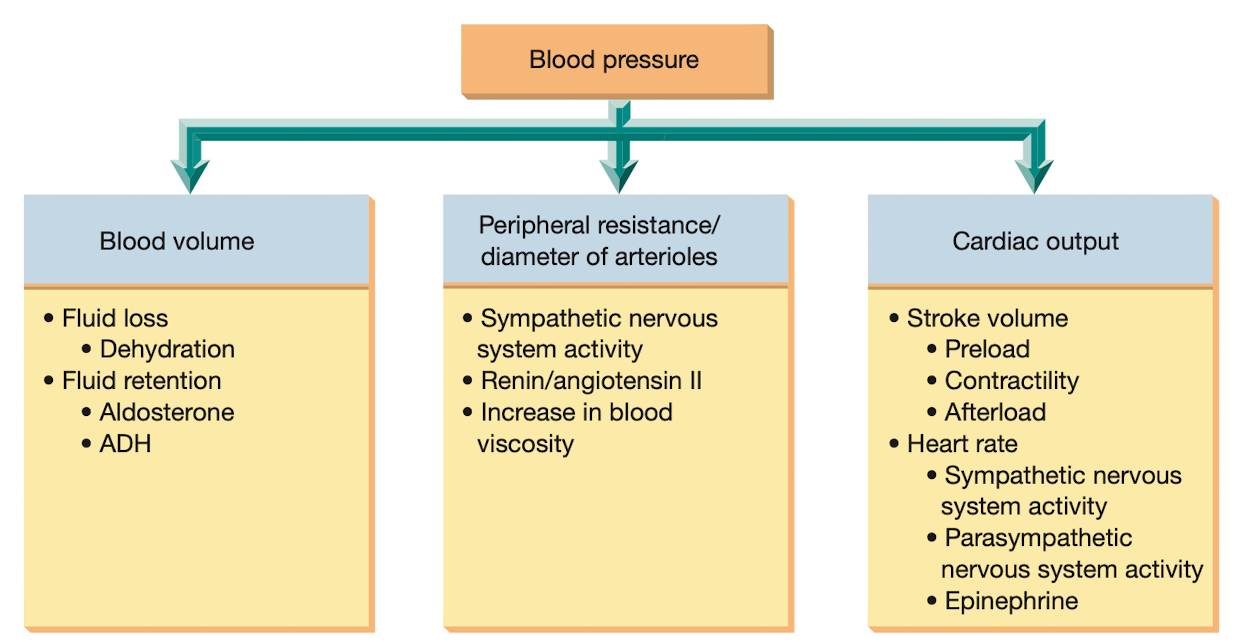
what are the 3 primary factors controlling BP?
* cardiac output
* peripheral resistance
* blood volume
* peripheral resistance
* blood volume
2
New cards
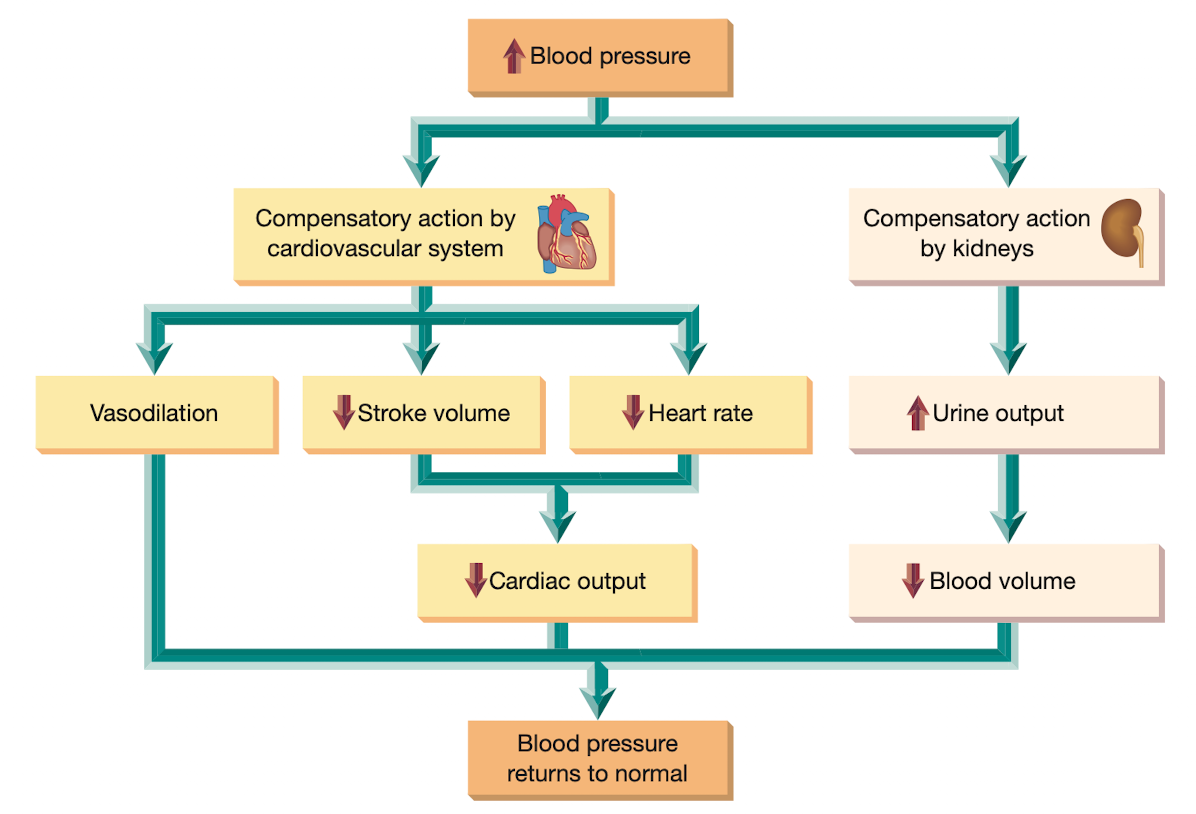
what factors help regulate BP?
* vasomotor center
* baroreceptros
* chemoreceptors in the aorta and internal carotid arteries
* renin-angiotensin system
* baroreceptros
* chemoreceptors in the aorta and internal carotid arteries
* renin-angiotensin system
3
New cards
high BP is classified as what?
primary (idiopathic or essential) or secondary
4
New cards
uncontrolled HTN can lead to?
chronic and debilitating disorders like stroke, heart attack, and HF
5
New cards
because antihypertensive meds may have adverse effects, what must change?
* lifestyle
* proper diet
* exercise should eb implemented
* proper diet
* exercise should eb implemented
6
New cards
pharmacotherapy of HTN often begins with what?
low doses of a single med. if this med proves ineffective, a second drug from a different class may be added to the regimen
7
New cards
what are the first-line meds for HTN bc they have few adverse effects and can effectively control minor-moderate HTN?
diuretics
8
New cards
blocking what prevents the intense vasoconstriction caused by angiotensin II. these drugs also decrease blood volume, which enhances their antihypertensive effect
renin-angiotensin-aldosterone system (RAAS)
9
New cards
what block calcium ions from entering cells and cause smooth muscle in arterioles to relax, thus reducing blood pressure. and have emerged as major drug in the treatment of HTN
calcium channel blockers
10
New cards
The patient has been given a prescription of hydrochlorothiazide (Microzide) as an adjunct to treatment of hypertension and returns for a follow-up check. Which is the most objective data for determining the therapeutic effectiveness of the furosemide?
1. Absence of edema in lower extremities
2. Weight loss of 13 kg (6 lb)
3. Blood pressure log notes blood pressure 120 /70 mmHig to 134/88 mmHg since discharge
4. Frequency of voiding of at least 6 times per day
1. Absence of edema in lower extremities
2. Weight loss of 13 kg (6 lb)
3. Blood pressure log notes blood pressure 120 /70 mmHig to 134/88 mmHg since discharge
4. Frequency of voiding of at least 6 times per day
**Answer**: 3
Rationale: Hydrochlorothiazide (Microzide) was prescribed as an adjunct treatment for HTN. Blood pressure decrease toward normal limits indicates that the use of this treatment has been effective.
**Options** 1, 2,and 4 are incorrect. Although absence of edema, weight loss, and frequency of voiding are related to fluid status and are other effects of furosemide, they are not related to the primary reason this drug was given (adjunctive therapy in HTN). Cognitive Level: Analyzing. Nursing Process: Evaluation. Client Need: Physiological Integrity.
Rationale: Hydrochlorothiazide (Microzide) was prescribed as an adjunct treatment for HTN. Blood pressure decrease toward normal limits indicates that the use of this treatment has been effective.
**Options** 1, 2,and 4 are incorrect. Although absence of edema, weight loss, and frequency of voiding are related to fluid status and are other effects of furosemide, they are not related to the primary reason this drug was given (adjunctive therapy in HTN). Cognitive Level: Analyzing. Nursing Process: Evaluation. Client Need: Physiological Integrity.
11
New cards
Nifedipine (Procardia XL) has been ordered for a patient with hypertension. In the care plan, the nurse includes the need to monitor for which adverse effect?
1. Rash and chills
2. Reflex tachycardia
3. Increased urinary output
4. Weight loss
1. Rash and chills
2. Reflex tachycardia
3. Increased urinary output
4. Weight loss
**Answer**: 2
**Rationale**: Nifedipine (Procardia XL) may cause hypotension with reflex tachycardia.
**Options** 1, 3, and 4 are incorrect. Rash, chills, increased urine out-put, and weight loss are not adverse effects of CCBs. \\n Cognitive Level: Applying. Nursing Process: Planning. \\n Client Need: Physiological Integrity.
**Rationale**: Nifedipine (Procardia XL) may cause hypotension with reflex tachycardia.
**Options** 1, 3, and 4 are incorrect. Rash, chills, increased urine out-put, and weight loss are not adverse effects of CCBs. \\n Cognitive Level: Applying. Nursing Process: Planning. \\n Client Need: Physiological Integrity.
12
New cards
The patient is taking atenolol (Tenormin) and doxazosin (Cardura). What is the rationale for combining two antihypertensive drugs?
1. The blood pressure will decrease faster.
2. Lower doses of both drugs may be given with fewer adverse effects.
3. There is less daily medication dosing.
4. Combination therapy will treat the patient's other medical conditions.
1. The blood pressure will decrease faster.
2. Lower doses of both drugs may be given with fewer adverse effects.
3. There is less daily medication dosing.
4. Combination therapy will treat the patient's other medical conditions.
**Answer**: 2
**Rationale**: The advantage of using a combi nation of two drugs such as atenolol (Tenormin; a beta blocker) and doxazosin (Cardura; an alpha-1 antago-nist) is that lower doses of each may be used, resulting in fewer side effects.
**Options** 1, 3, and 4 are incorrect. \\n With careful dosing, the BP should be gradually lowered to a safe limit. The number of doses per day is dependent on the half-life of the drug, not the combina-tion. Other conditions may be treated, but the primary reason to combine antihypertensives is not in treatment of additional conditions. Cognitive Level: Applying. \\n Nursing Process: Implementation. Client Need: Physiological Integrity.
**Rationale**: The advantage of using a combi nation of two drugs such as atenolol (Tenormin; a beta blocker) and doxazosin (Cardura; an alpha-1 antago-nist) is that lower doses of each may be used, resulting in fewer side effects.
**Options** 1, 3, and 4 are incorrect. \\n With careful dosing, the BP should be gradually lowered to a safe limit. The number of doses per day is dependent on the half-life of the drug, not the combina-tion. Other conditions may be treated, but the primary reason to combine antihypertensives is not in treatment of additional conditions. Cognitive Level: Applying. \\n Nursing Process: Implementation. Client Need: Physiological Integrity.
13
New cards
What health teaching should the nurse provide for the patient receiving nadolol (Corgard)?
1. Increase fluids and fiber to prevent constipation.
2. Report a weight gain of 1 kg per month or more.
3. Immediately stop taking the medication if sexual dysfunction occurs.
4. Rise slowly after prolonged periods of sitting or lying down.
1. Increase fluids and fiber to prevent constipation.
2. Report a weight gain of 1 kg per month or more.
3. Immediately stop taking the medication if sexual dysfunction occurs.
4. Rise slowly after prolonged periods of sitting or lying down.
**Answer**: 4
**Rationale**: Nadolol (Corgard) may increase the risk of orthostatic hypotension, and the patient should be taught to rise slowly to standing from a sitting or lying position.
**Options** 1, 2, and 3 are incorrect. \\n The drug does not cause constipation, and extra fluids and fiber are not required. A weight gain of over 1 kg per day should be reported but a gain of 1 kg per month may be insignificant or unrelated to the drug. The drug should never be stopped abruptly because of possible HIN and tachycardia. Cognitive Level: Applying. \\n Nursing Process: Implementation. Client Need: Health Promotion and Maintenance.
**Rationale**: Nadolol (Corgard) may increase the risk of orthostatic hypotension, and the patient should be taught to rise slowly to standing from a sitting or lying position.
**Options** 1, 2, and 3 are incorrect. \\n The drug does not cause constipation, and extra fluids and fiber are not required. A weight gain of over 1 kg per day should be reported but a gain of 1 kg per month may be insignificant or unrelated to the drug. The drug should never be stopped abruptly because of possible HIN and tachycardia. Cognitive Level: Applying. \\n Nursing Process: Implementation. Client Need: Health Promotion and Maintenance.
14
New cards
The nurse is caring for a patient with chronic hypertension. The patient is receiving losartan (Cozaar) daily. Which patient manifestations would the nurse conclude is an adverse effect of this medication? (Select all that apply.)
1. Tremors
2. Dizziness
3. Drowsiness
4. Hypoglycemia
5. Angioedema
1. Tremors
2. Dizziness
3. Drowsiness
4. Hypoglycemia
5. Angioedema
**Answer**: 2, 4, 5
**Rationale**: Adverse effects of ARBs such as losartan (Cozaar) include dizziness, fatigue, hypoglycemia, urinary tract infections, and anemia. Though rare, angioedema and acute kidney injury may occur.
**Option** 1 and 3 are incorrect. Drowsiness and tremors are not expected adverse effects of losartan. Cognitive Level: Analyzing. Nursing Process: Evaluation. Client Need: Physiological Integrity.
**Rationale**: Adverse effects of ARBs such as losartan (Cozaar) include dizziness, fatigue, hypoglycemia, urinary tract infections, and anemia. Though rare, angioedema and acute kidney injury may occur.
**Option** 1 and 3 are incorrect. Drowsiness and tremors are not expected adverse effects of losartan. Cognitive Level: Analyzing. Nursing Process: Evaluation. Client Need: Physiological Integrity.
15
New cards
A patient with significant hypertension unresponsive to other medications is given a prescription for hydralazine. An additional prescription of propranolol (Inderal) is also given to the patient. The patient inquires why two drugs are needed. What is the nurse's best response?
1. Giving the two drugs together will lower the blood pressure even more than just one alone.
2. The hydralazine may cause tachycardia and the propranolol will help keep the heart rate within normal limits.
3. The propranolol is to prevent lupus erythemato-sus from developing.
4. Direct-acting vasodilators such as hydralazine cause fluid retention, and the propranolol will prevent excessive fluid buildup.
1. Giving the two drugs together will lower the blood pressure even more than just one alone.
2. The hydralazine may cause tachycardia and the propranolol will help keep the heart rate within normal limits.
3. The propranolol is to prevent lupus erythemato-sus from developing.
4. Direct-acting vasodilators such as hydralazine cause fluid retention, and the propranolol will prevent excessive fluid buildup.
**Answer**: 2
**Rationale**: Propranolol (Inderal) and other beta-blocking drugs are used to prevent reflex tachycardia that may occur as a result of treatment with direct-acting vasodilators. Giving two antihypertensive drugs together may also lower blood pressure further; how-ever, the beta-blocking drugs also lower the heart rate and are given in this case to reduce the chance for reflex tachycardia.
**Options** 1, 3, and 4 are incorrect. Propranolol has not been demonstrated to have effects in preventing lupus and is not a diuretic, although judicious diuretic therapy may be necessary if excessive fluid gain is an adverse effect of direct-acting vasodilator therapy. Cognitive Level: Analyzing. Nursing Process:
Implementation. Client Need: Physiological Integrity.
**Rationale**: Propranolol (Inderal) and other beta-blocking drugs are used to prevent reflex tachycardia that may occur as a result of treatment with direct-acting vasodilators. Giving two antihypertensive drugs together may also lower blood pressure further; how-ever, the beta-blocking drugs also lower the heart rate and are given in this case to reduce the chance for reflex tachycardia.
**Options** 1, 3, and 4 are incorrect. Propranolol has not been demonstrated to have effects in preventing lupus and is not a diuretic, although judicious diuretic therapy may be necessary if excessive fluid gain is an adverse effect of direct-acting vasodilator therapy. Cognitive Level: Analyzing. Nursing Process:
Implementation. Client Need: Physiological Integrity.
16
New cards
Leo Marshall is a 72-year-old with a history of HTN, CKD, and angina. He is on a low-sodium, low-protein diet and has been adhering to his treatment plan. He has been admitted to the short-stay surgical unit for a minor procedure and will stay overnight. His blood pressure prior to discharge is 106/84.
1. What blood pressure parameters are commonly used to determine whether an antihypertensive dose is given or not?
2. Should the nurse give the patient benazepril (Loten-sin) as scheduled in the morning after surgery?
3. What other patient data or assessments should the nurse check?
1. What blood pressure parameters are commonly used to determine whether an antihypertensive dose is given or not?
2. Should the nurse give the patient benazepril (Loten-sin) as scheduled in the morning after surgery?
3. What other patient data or assessments should the nurse check?
1. Unless the provider sets different parameters, anti-hypertensive medication is usually held if the blood pressure is 90/60 or below. The provider should be contacted if the blood pressure is below the set parameter or any time there are other symptoms, such as a weight gain of over 1 kg (2 pounds) in a 24-hour period, chest pain, or shortness of breath.
\
2. Because the BP is above 90/60, the nurse should give the dose of benazepril (Lotensin). Mr. Marshall should be cautioned about orthostatic hypotension and the appropriate safety measures taken (e.g., rising slowly to standing).
\
3. Mr. Marshall is on a low-sodium, low-protein diet, which may contribute to hypotension. Because the patient has CKD, the excretion of the drug may be prolonged and also contribute to the hypotensive effects. The nurse should recheck the BP more frequently (e.g., 30 and 60 minutes after giving the dose, then every 4 hours to assess for hypotension. Assessing ortho-static blood pressures as the patient rises from lying to sitting to standing will also provide valuable data. The serum creatinine and protein levels may also be checked to assess renal status. Finally, because this drug is an ACE inhibitor, the nurse should assess for the development of a cough or angioedema. Both are potential adverse effects of this drug classification that may require additional treatment.
17
New cards
A patient with diabetes is on atenolol (Tenormin) for HTN. Identify a teaching plan for this patient.
Atenolol (Tenormin) is a beta,-adrenergic blocker that works directly on the heart. The nurse and the patient need to be aware that despite increased activity or stress, the patient's heart rate may not increase significantly because of the action of the medication. Tachycardia is one of the adrenergic signs of hypoglycemia that would not be readily evident in this patient. Both the nurse and patient need to be aware of the more subtle signs of hypoglycemia such as nervousness, irritability, or sweating that would not be evident with a patient on beta-blocking medications.
18
New cards
A patient is having a hypertensive crisis (230/130), and the blood pressure needs to be lowered. The patient has an IV drip of nitroprusside (Nitropress) initiated. How much would the nurse want to lower this patient's blood pressure? Identify three nursing interventions that
The nurse must ensure that the patient's blood pressure is not lowered too rapidly or too significantly because hypotension and reflex tachycardia may occur. The blood pressure should be lowered gradually and to parameters set by the healthcare provider. The patient is reevaluated frequently for decrease in blood pres-sure, reflex tachycardia, urine output, and other signs of cardiac output and tissue perfusion. This drug is light sensitive and must remain covered with foil or an amber protective wrapper during infusion. Once prepared, the drip is stable for only 24 hours.
19
New cards
what do you call the volume of blood pumped per minute?
cardiac output (CO); the higher the CO is the higher the BP
20
New cards
hypotension can cause?
* dizziness
* lack of adequate urine formation
* lack of adequate urine formation
21
New cards
extreme HTN can cause
blood vessels to rupture or restrict blood flow to critical organs
22
New cards
what is a potent vasoconstrictor that can also increase BP by raising blood volume?
antidiuretic hormone (ADH)
23
New cards
HTN having no identifiable cause is called?
primary HTN
24
New cards
HTN with a specific cause can be identified as?
secondary HTN
25
New cards
what is the therapeutic goal of secondary HTN?
to treat or remove the underlying condition that is causing the BP elevation
26
New cards
nonpharm management of HTN
* limit intake of alcohol
* restrict Na consumption
* increase K intake
* reduce intake of saturated fat and cholesterol and increase consumption of fresh fruits and veggies
* increase physical activity
* discontinue use of tobacco products
* reduce sources of stress
* maintain optimal weight
* restrict Na consumption
* increase K intake
* reduce intake of saturated fat and cholesterol and increase consumption of fresh fruits and veggies
* increase physical activity
* discontinue use of tobacco products
* reduce sources of stress
* maintain optimal weight
27
New cards
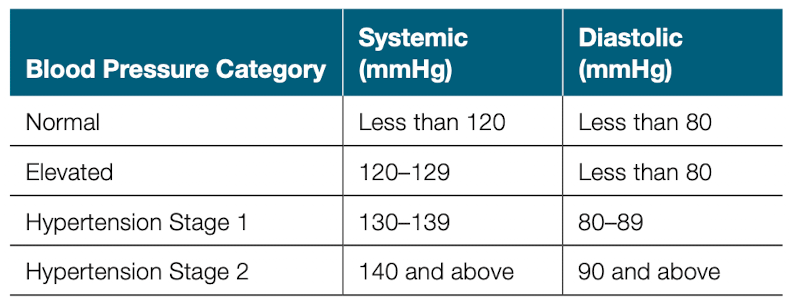
BP categories
\
28
New cards
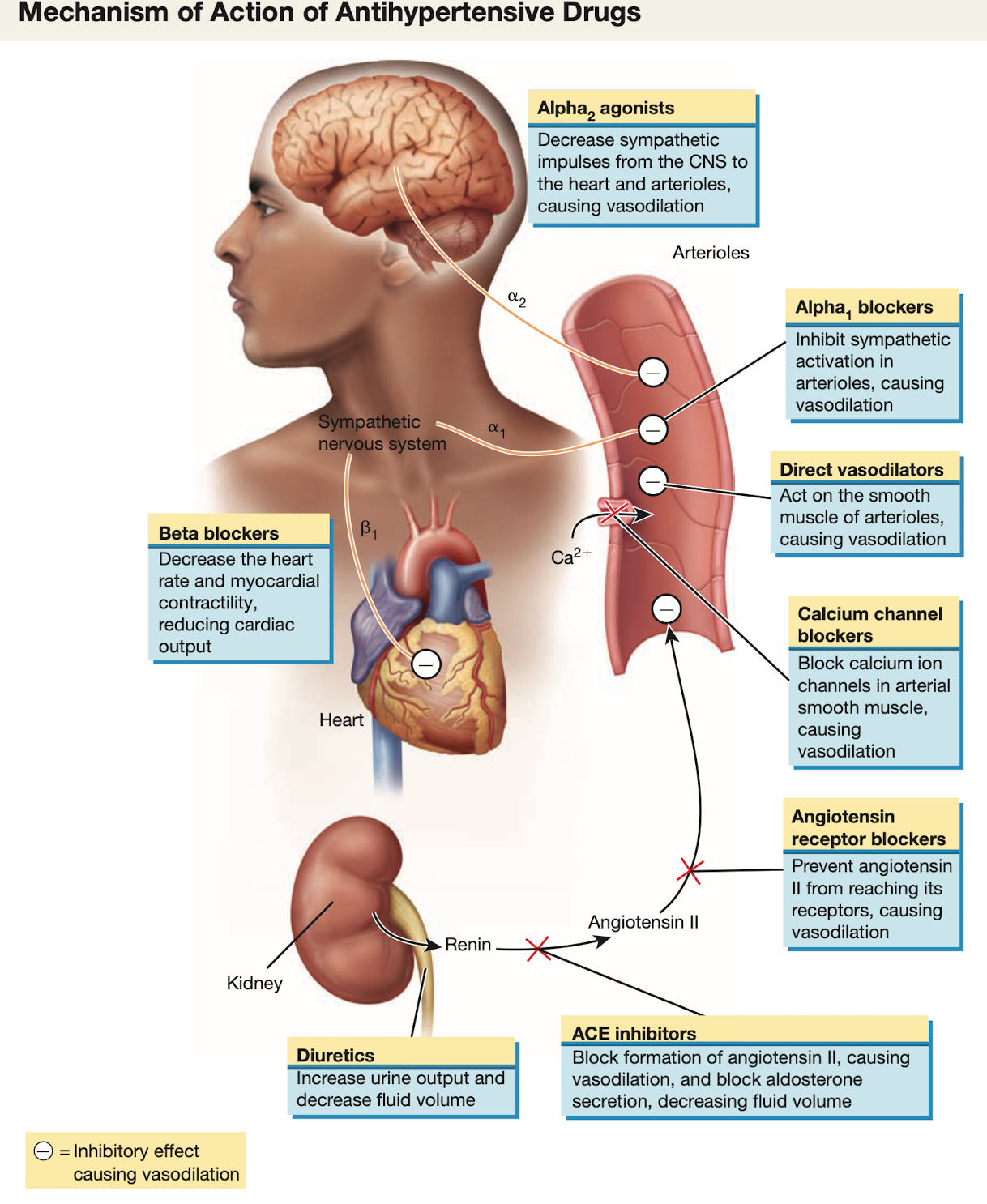
what decrease sympathetic impulses from the CNS to the heart and arterioles, causing vasodilation?
alpha 2 agonist
29
New cards
what decrease the heart rate and myocardial contractility, reducing CO?
beta blockers
30
New cards
what inhibit sympathetic activation in arterioles, causing vasodilation?
alpha 1 blockers
31
New cards
what act on the smooth muscle of arterioles, causing vasodilation?
direct vasodilators
32
New cards
what block calcium ion channels in arterial smooth muscle, causing vasodilation?
calcium channel blockers
33
New cards
what prevent angiotensin II from reaching its receptors, causing vasodilation?
angiotensin receptor blockers
34
New cards
what block formation of angiotensin II, causing vasodilation, and block aldosterone secretion, decreasing fluid volume
ACE inhibitors (ACEI)
35
New cards
what increase urine output and decrease fluid volume?
diuretics
36
New cards
mechanism of action of antihypertensive drugs
37
New cards
what is the advantage of prescribing 2 drugs?
lower doses of each may be used, resulting in fewer side effects and better patient adherence to the therapy
38
New cards
what drug classes for HTN is the first-line drug
* angiotensin converting enzyme (ACE) inhibitors
* angiotensin receptor blockers (ARBs)
* calcium channel blockers (CCBs)
* thiazide diuretics
* angiotensin receptor blockers (ARBs)
* calcium channel blockers (CCBs)
* thiazide diuretics
39
New cards
what drug classes for HTN is second-line drug?
* alpha 1 adrenergic blockers
* alpha 2 adrenergic agonist
* beta adrenergic blockers
* centrally acting alpha and beta blockers
* direct-acting vasodilators
* direct renin inhibitors
* alpha 2 adrenergic agonist
* beta adrenergic blockers
* centrally acting alpha and beta blockers
* direct-acting vasodilators
* direct renin inhibitors
40
New cards
what CAM to give for HTN patients?
* grape seed extract
41
New cards
what diuretic is safe, with urinary potassium loss being the primary adverse effect?
thiazide and thiazide-like diuretics
42
New cards
what diuretics is also used to HTN but its primary advantage is that it doesn’t cause potassium depletion?
potassium-sparing diuretics; also a primary concern is retaining too much potassium
43
New cards
adverse effect of taking potassium-sparing diuretics?
* dysrhythmias (from hyperK)
* dehydration
* hyponatremia
* agranulocytosis
* other blood dyscrasia
* dehydration
* hyponatremia
* agranulocytosis
* other blood dyscrasia
44
New cards
adverse effect of taking thiazide and thiazide-like diuretics?
* significant hypokalemia
* electrolyte depletion
* dehydration
* hypotension
* hyponatremia
* hyperglycemia
* coma
* blood dyscrasias
* electrolyte depletion
* dehydration
* hypotension
* hyponatremia
* hyperglycemia
* coma
* blood dyscrasias
45
New cards
adverse effect of taking loop/high-ceiling diuretics?
* serious hypokalemia
* blood dyscrasias
* dehydration
* ototoxicity
* electrolyte imbalance
* circulatory collapse
* blood dyscrasias
* dehydration
* ototoxicity
* electrolyte imbalance
* circulatory collapse
46
New cards
what is one of the primary homeostatic mechanism controlling BP and fluid balance in the body? and increase urine volume
renin-angiotensin-aldosterone system (RAAS)
47
New cards
what drug is widely used in pharmacotherapy of HTN, HF< and myocardial infarction?
renin-angiotensin-aldosterone system (RAAS)
48
New cards
what secretion does angiotensin II stimulate? a hormone from the adrenal cortex
aldosterone
49
New cards
this hormone increase Na reabsorption in the kidney
aldosterone
50
New cards
Angiotensin II increases BP through 2 distinct mechanisms. what are they?
direct vasoconstriction and increase water retention
51
New cards
adverse effect of taking ACE inhibitors?
* angioedema
* acute renal failure
* first-dose phenomenon
* fetal toxicity
* hyperkalemia
* acute renal failure
* first-dose phenomenon
* fetal toxicity
* hyperkalemia
52
New cards
adverse effect of taking angiotensin II receptor blockers?
* angioedema
* acute renal failure
* first-dose phenomenon
* fetal toxicity
* hyperkalemia
* nephrotoxicity
* acute renal failure
* first-dose phenomenon
* fetal toxicity
* hyperkalemia
* nephrotoxicity
53
New cards
what is the prototype drug of angiotensin II receptor blocker (ARBs)? is a drug for HTN
losartan (Cozaar)
54
New cards
administration alerts when taking losartan?
* may produce dizziness and fainting; patient should change position slowly
* dont give to preggy women
* dont give to preggy women
55
New cards
adverse effects of losartan?
* hypoglycemia
* dizziness
* UTI
* fatigue
* anemia
Serous A/E:
* angioedema
* AKI
* dizziness
* UTI
* fatigue
* anemia
Serous A/E:
* angioedema
* AKI
56
New cards
black box waring of losartan?
fetal injury and death during pregnancy
57
New cards
contraindication of taking losartan?
* hypersensitivty
* concurrent use with aliskiren is contraindicated
* concurrent use with aliskiren is contraindicated
58
New cards
what labs to monitor while taking losartan?
may increase:
* BUN
* potassium
* creatinine
* ALT
* AST
* BUN
* potassium
* creatinine
* ALT
* AST
59
New cards
what treatment needed for losartan overdose?
* signs of overdose include severe dizziness and fainting due to hypotensiojn
* treated with IV infusion of normal saline solution
* treated with IV infusion of normal saline solution
60
New cards
what drug class is used to treat angina pectoris, dysrhythmias, and HTN
calcium channel blockers (CCBs)
61
New cards
what 2 CCBs, are sued to treat patients who present with serious, life-threatening HTN?
clevidipine (Cleviprex) and nicardipine (Cardene)
62
New cards
what CCBs have an ultrashort half-life of 1 min, which allows for rapid adjustments to BP. is indicated only by IV route for hypertensive emergencies
clevidipine
63
New cards
what CCBs is given in PO route for primary HTN and angina
nicardipine
64
New cards
CCBs drugs for blood vessels (selective)
* nicardipine
* nifedipine
* amlodipine
* nifedipine
* amlodipine
65
New cards
CCBs drugs for both blood vessels and heart (nonselective)
* dilitiazem
* verapamil
* verapamil
66
New cards
adverse effects of CCBs?
* hepatotoxicity
* MI
* HF
* confusion
* mood changes
* angioedema
* MI
* HF
* confusion
* mood changes
* angioedema
67
New cards
what prototype drug does CCBs have and is drug or HTN and angina?
nifedipine
68
New cards
administration alerts when taking nifedipine?
* dont give immediate-release formulation if an impending MI is suspected or within 2 wks following confirmed MI
* give capsules or tablets whole
* give capsules or tablets whole
69
New cards
what lab tests to monitor when taking nifedipine?
may increase:
* a;la;ome phsophatase
* ALT
* CPK
* AST
* a;la;ome phsophatase
* ALT
* CPK
* AST
70
New cards
what is the treatment for nifedipine overdose?
* sign of overdose: hypotension
* treated with vasopressors
* calcium infusion may be indicated
* treated with vasopressors
* calcium infusion may be indicated
71
New cards
For most patients, what are the most common drug classes chosen for the initial treatment of hypertension?
For most patients, thiazide diuretics, ACE inhibitors, ARBs, or CCBs are the most commonly recommended drug classifications for the initial treatment of HTN, per the INC-8 guidelines.
72
New cards
adverse effect of beta adrenergic antagonists
* fatigue
* insomnia
* drowsiness
* impotence or decreased libido
* **angranulocytosis**
* **stevens-johnson syndrome**
* **anaphylaxis**
* **rebound HTN**
* **MI**
* **dysrhythmias**
* insomnia
* drowsiness
* impotence or decreased libido
* **angranulocytosis**
* **stevens-johnson syndrome**
* **anaphylaxis**
* **rebound HTN**
* **MI**
* **dysrhythmias**
73
New cards
adverse effect of alpha1-adrenergic antagonists
* orthostatic hypotension
* dizziness
* HA
* fatigue
* **first-dose phenomenon**
* **tachycardia**
* **dyspnea**
* dizziness
* HA
* fatigue
* **first-dose phenomenon**
* **tachycardia**
* **dyspnea**
74
New cards
adverse effect of alpha2-adrenergic agonist (centrally acting)
* peripheral edema
* sedation
* depression
* HA
* dry mouth
* decreased libido
* **hepatotoxicity**
* **hemolytic anemia**
* **granulocytopenia**
* sedation
* depression
* HA
* dry mouth
* decreased libido
* **hepatotoxicity**
* **hemolytic anemia**
* **granulocytopenia**
75
New cards
adverse effect of alpha1 and beta blockers
* dizziness
* fatigue
* weight gain
* hyperglycemia
* diarrhea
* **bradycardia**
* **may worsen HF and mask symptoms of hypoglycemia**
* fatigue
* weight gain
* hyperglycemia
* diarrhea
* **bradycardia**
* **may worsen HF and mask symptoms of hypoglycemia**
76
New cards
what does alpha1 adrenergic blockers do?
lower BP directly by blocking sympathetic receptors in arterioles. causing the vessels to dilate
77
New cards
what does alpha2 adrenergic agonists do?
decrease the outflow of sympathetic nerve impulses from the CNS to the heart and arterioles
78
New cards
what does alpha2 adrenergic agonists do causes?
* sedation
* dizziness
* other CNS effects
* leukopenia
* thrombocytopenia
* lupus
* dizziness
* other CNS effects
* leukopenia
* thrombocytopenia
* lupus
79
New cards
what prototype drug does alpha1-adrenergic blocker have. its a drug for HTN and BPH
doxazosin
80
New cards
administration alerts when taking doxazosin?
* monitor patients closely for profound hypotension, possible syncope 2-6 hrs following first few doses due to first-dose phenomenon
* first-dose phenomenon can recur when med is resumed after period of withdrawal and dosage increases
* first-dose phenomenon can recur when med is resumed after period of withdrawal and dosage increases
81
New cards
adverse effects of doxazosin
* dizziness
* dyspnea
* asthenia
* HA
* hypotension
* orthostatic hypotension
* somnolence
* dyspnea
* asthenia
* HA
* hypotension
* orthostatic hypotension
* somnolence
82
New cards
what is the treatment for doxazosin overdose>
* sign of overdose is hypotension
* treated with vasopressor or IV infusion of fluids
* treated with vasopressor or IV infusion of fluids
83
New cards
what drug class produce **reflex** tachycardia and sodium and water retention?
direct vasodilators
84
New cards
Why is a diuretic sometimes needed along with some classes of antihypertensive medication?
The drop in blood pressure caused by antihypertensive medication may trigger the RAAS mechanism and the release of aldosterone, increasing sodium and, thus, water retention and edema.
85
New cards
what is considered a hypertensive emergency?
* systolic: >180
* diastolic: >120
* with evidence of impending end-organ damage, usually to the heart, kidney, or brain
* diastolic: >120
* with evidence of impending end-organ damage, usually to the heart, kidney, or brain
86
New cards
what is the common cause of hypertensive emergency?
uncontrolled or poorly controlled primary HTN
87
New cards
what is the traditional preferred drug for hypertensive emergencies?
nitroprusside (nitro press)
* with a half-life of only 2 min, has the ability to lower BP almost instantaneously on IV
* with a half-life of only 2 min, has the ability to lower BP almost instantaneously on IV
88
New cards
what prototype drug does direct-acting vasodilator have? its drug for HTN and HF
hydralazine
89
New cards
administration alerts when taking hydralazine?
abrupt withdrawal of drug may cause rebound HTN and anxiety
90
New cards
adverse effect when taking hydralazine?
* HA
* reflex tachycardia (take beta-adrenergic blocker to counter)
* palpitations
* flusing
* nausea
* diarrhea
* reflex tachycardia (take beta-adrenergic blocker to counter)
* palpitations
* flusing
* nausea
* diarrhea
91
New cards
contraindication when taking hydralazine?
* in patients with angina or rheumatic mitral valve heart disease
* patient with lupus can’t take this as it worsen symptoms
* patient with lupus can’t take this as it worsen symptoms
92
New cards
what is the treatment for hydralazine overdose?
* sign of overdose is hypotension
* treated with a vasopressor or an IV infusion of fluids
* treated with a vasopressor or an IV infusion of fluids