Platelet physiology II - stages of maturation
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
What is the origin of platelets?
megakaryocytes
Where do megakaryocytes originate?
the bone marrow
What is thrombopoesis?
platelet production
What molecule regulates thrombopoesis?
TPO, or thrombopoetin
Through the maturation stages of megakaryocytes, describe the general characteristics observed (size, cytoplasm stain, granule presence, nucleus:cytoplasm ratio, and nuclear lobing).
Size: goes from small to large
cytoplasm stain: goes from basophilic (deep blue) to acidophilic (pink)
granule presence: no granules to more
nucleus:cytoplasm ratio: high to low
aka nucleus shrinks and cytoplasm grows
nuclear lobing: no lobing to multilobed
What is the normal lifespan of a platelet?
8-10 days
What is the reference range of platelets in peripheral blood?
150-450 × 103/uL
Describe the megakaryocyte stage of maturation.
derive from a unipotential stem cell
nucleus is round, no lobes
basophilic cytoplasm
very small
many copies of DNA due to endomitosis
Describe the promegakaryocyte stage of maturation.
less DNA replication occurring
deeper purple nucleus
cytoplasm begins to lighten
a few granules present
Describe the granular megakaryocyte stage of maturation.
cytoplasm still lightening
cytoplasm grows more, nucleus size decreases
pinker granules
no visible nucleoli
multilobed, condensed nucleus
Describe the mature megakaryocyte stage of maturation.
multilobed nucleus
platelet fields (demarcation zones) form from granules
acidophilic cytoplasm
eventual breakage of the megakaryocyte releasing platelets and the nucleus
How are platelets removed?
macrophage consumption
How are platelets consumed?
through primary hemostasis, or storage in the spleen
What is the normal distribution of platelets?
2/3 in circulation, 1/3 in spleen
What is a splenectomy? How does it impact platelet distribution?
when the spleen is removed
Platelet distribution is increased in circulation
What is splenomegaly? How does it impact platelet distribution?
When the spleen is overactive/dysfunctional
Platelet distribution decreases in circulation (spleen basically hogs the platelets)
What is thrombopoetin (TPO)?
a regulator of megakaryocyte maturation and platelet development
regulates endomitosis
regulates production of megakaryocytes from unipotential cells
increases platelet numbers and volumes in circulation
If a person receives a platelet transfusion, how does that impact their platelet count and free TPO availability?
Platelet count increases, therefore more platelet receptors for TPO, and thus decreased free TPO
If a person endures trauma (loss of platelets), how does that impact their platelet count and free TPO availability?
Platelet count decreases, therefore there are less platelet receptors for TPO, and thus increased free TPO
What are conditions that lead to increased bleeding time?
von Willebrands disease (platelet aggregation with vWF forming multimers)
platelet abnormalities
aspirin medication (TXA2 inhibitor)
thrombocytopenia (low platelet count)
Describe the platelet aggregation test.
Platelet rich plasma is stirred, and inoculated with collagen or epinephrine to induce aggregation
As the platelet changes shape for aggregation, the light transmittance changes
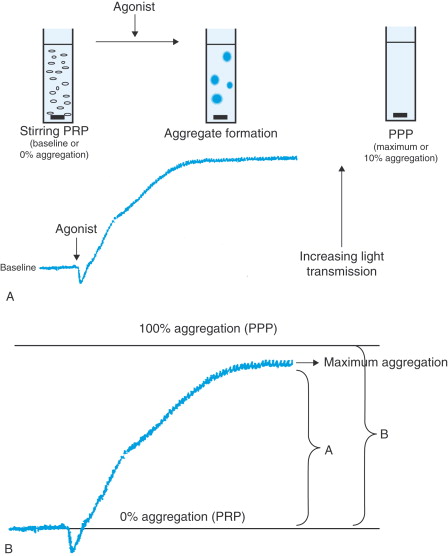
What is the relationship between platelet aggregation and light transmittance?
Initially, when a platelet agonist is added, light transmittance decreases as platelets change shape.
Then, as the platelets reach 100% aggregation, light transmittance increases as the aggregate falls to the bottom of the tube.
For the platelet function assay, if a sample of blood has a normal closure time after only COL/EPI, what is the interpretation?
Normal platelet fx
For the platelet function assay, if a sample of blood has a prolonged closure time with COL/EPI and a normal closure time with COL/ADP, what is the interpretation?
Normal closure time, likely thrown off by an aspirin medication
For the platelet function assay, if a sample of blood has a prolonged closure time with COL/EPI and a prolonged closure time with COL/ADP, what is the interpretation?
Potential disease such as von Willebrand’s disease, thrombocytopenia (low platelet count), or a platelet defect