ANA 852 Guyton Practice Questions Quiz
1/56
Earn XP
Description and Tags
https://quizlet.com/170036734/respiratory-physiology-practice-problems-flash-cards/
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
1. A patient with no respiratory problems is given a blood transfusion. Which of the following
will occur?
A. Arterial pO2 will increase
B. Arterial pCO2 will decrease
C. Arterial saturation will increase
D. Arterial oxygen content will decrease
E. Arterial oxygen content will increase
E. Arterial oxygen content will increase
2. Which of the following should decrease the affinity of hemoglobin for oxygen?
A. Low pCO2
B. Alkalosis
C. Acidosis
D. Decreased body temperature
C. Acidosis
3. An otherwise healthy person has lost enough blood to decrease his body's hemoglobin
concentration from 15 g/100 mL blood to 12 g/100 mL blood. Which of the following would
be expected to decrease?
A. Arterial pO2
B. Blood oxygen-carrying capacity
C. Arterial hemoglobin saturation
D. Arterial carbon dioxide content
B. Blood oxygen-carrying capacity
4. Using the following values, calculate saturation:
• Hemoglobin concentration = 11 g/dL
• Oxygen content = 12 mL/dL
A. 100%
B. 81%
C. 65%
D. 56%
E. 43%
B. 81%
\O₂ content≈1.34×Hb×SaO
12=1.34×11×SaO₂
1.34×11=14.74
SaO₂=12/ 14.74 ≈0.81=81%
5. Acute hemorrhage causes a reduction of hemoglobin concentration to 60% of normal in an
otherwise healthy individual. If the alveolar ventilation and oxygen consumption rates remain
the same as before the hemorrhage, which of the following will occur after the hemorrhage?
A. Normal arterial pO2, normal venous pO2
B. Low arterial pO2, normal venous pO2
C. Low arterial pO2, Low venous pO2
D. Normal arterial pO2, low venous pO2
E. High arterial pO2, normal venous pO2
D. Normal arterial pO2, low venous pO2
6. An increase in carbon monoxide will result in which of the following?
A. Increased firing from the peripheral chemoreceptors
B. Increased pCO2
C. Decreased arterial pO2
D. Decreased in arterial oxygen content
D. Decreased in arterial oxygen content
7. Arterial pO2 is 100 mm Hg and arterial pCO2 is 40 mm Hg. Total blood flow to all muscle is 700 mL/min. There is a sympathetic activation resulting in a decrease in blood flow to 350 mL/min. Which of the following will occur?
Venous pO2 Venous pCO2
A. Inc, Dec
B. Dec, inc
C. Dec, no change
D. no change, inc
E. inc, inc
F. dec, dec
G. no change; no change
B. Dec, inc
8. If the blood lacked red blood cells but the lungs were functioning normally, which of the
following would be true?
A. The arterial pO2 would be normal
B. The oxygen content of arterial blood would be normal
C. Both A and B
D. Neither A nor B
A. The arterial pO2 would be normal
9. When red cells flow through the systemic capillaries, which of the following will occur?
A. A shift to the left of the hemoglobin dissociation curve
B. A binding of hydrogen ions to hemoglobin
C. Chloride movement out of the red cell
D. Bicarbonate movement into the red blood cell
B. A binding of hydrogen ions to hemoglobin
10. A human experiment is being performed in which forearm blood flow is measured under a
variety of conditions. The forearm is infused with a vasodilator, resulting in an increase in
blood flow. Which of the following will occur?
A. Tissue interstitial PO2 will increase
B. Tissue interstitial PCO2 will increase
C. Tissue pH will decrease
A. Tissue interstitial PO2 will increase
11. Initial conditions for a healthy man are the following (in the steady state):
• Arterial PO2 = 92 mmHg
• Arterial O2 saturation = 97%
• Venous O2 saturation = 20%
• Venous PO2 = 30 mm Hg
• Cardiac output = 5600 ml/min
• Oxygen consumption = 256 ml/min
• Hb concentration = 12 gm/dl
If you ignore the contribution of dissolved O2 to the O2 content, what is the venous O2
content?
A. 2.2 ml O2/100 ml blood
B. 3.2 ml O2/100 ml blood
C. 4 ml O2/100 ml blood
D. 4.6 ml O2/100 ml blood
E. 6.2 ml O2/100 ml blood
F. 10.8 ml O2/100 ml blood
G. 16 ml O2/100 ml blood
B. 3.2 ml O2/100 ml blood
Venous O2 content × Venous O2 saturation × 1.34). Given a Hb concentration of 12 gm/dl and a venous O2 saturation of 20%, the result is 3.2 ml O2/100 ml blood.
8. Initial conditions for a normal female subject (12 g Hb/100 mL blood) are the
following (in the steady state).
Arterial pO2 = 100 mmHg
Arterial O2 saturation = 90%
Venous O2 saturation = 28%
Venous pO2 = 25 mmHg
Cardiac output = 5,000 mL/min
Oxygen consumption = 500 mL/min
If you ignore the contribution of dissolved O2 to the total O2 content, what is the venous
O2 content?
A. 3.3 mL O2/100 mL blood
B. 4.5 mL O2/100 mL blood
C. 5.6 mL O2/100 mL blood
D. 7.5 mL O2/100 mL blood
B. 4.5 mL O2/100 mL blood
12. A man fell asleep in his running car one evening. He was brought into the emergency
department unconscious. With carbon monoxide poisoning, you would expect his PaO2 to be
_______, while his CaO2 would be ______.
A. Normal, decreased
B. Decreased, decreased
C. Increased, normal
D. Increased, normal
A. Normal, decreased
15. A 22-year-old man was involved in a fight and received a blow to the head. On arrival
to emergency department he was unconscious and was receiving assisted ventilation via a
manual bag. His blood gases were:
pO2 = 45 mmHg
pCO2 = 80 mmHg
pH = 7.05
HCO3 = 27 mM
In which form was most CO2 being transported in this patient?
A. Dissolved
B. Bicarbonate ions
C. Carbaminohemoglobin compounds
D. CO2 bound to plasma proteins
B. Bicarbonate ions
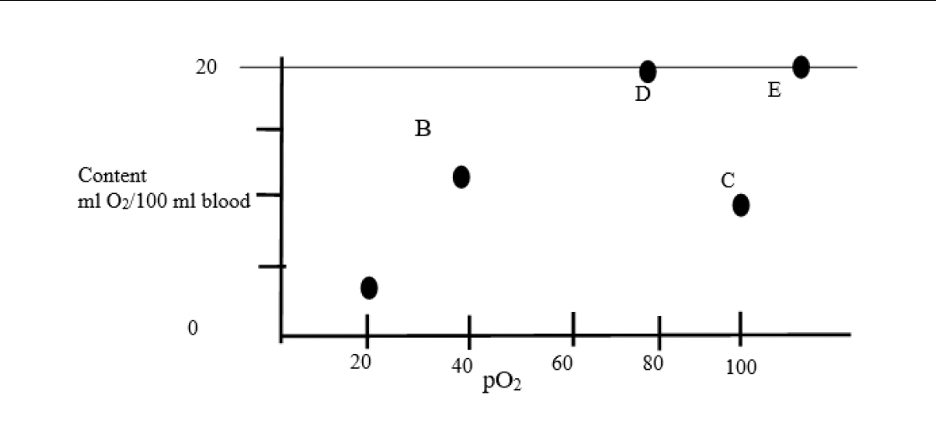
MATCHING
Determine which points describe the following conditions.
1. Coronary sinus blood.
2. Arterial blood in a person with end-stage renal disease.
3. Arterial blood in a normal person.
4. Mixed venous blood of person at 500 feet above sea level.
1. ANS: A
2. ANS: C
3. ANS: D
4. ANS: B
3. A person with anemia has a Hb concentration of 12 g/dL. He starts exercising and uses 12 mL O2/dL. What is the mixed venous pO2?
A. 0 mmHg
B. 10 mmHg
C. 20 mmHg
D. 40 mmHg
E. 100 mmHg
C. 20 mmHg
1. Five hours after an uneventful knee surgery, a conscious 50-year-old woman has minor heart pain and a decrease in systolic blood pressure from 110 to 90 mm Hg. ABG analysis on her breathing room air shows:
• pH = 7.30
• pCO2= 52 mm Hg
• pO2 = 58 mm Hg
Which of the following is the most likely cause of these findings?
A. Alveolar hypoventilation
B. Cardiac failure
C. Hypoxia due to anesthetic gases
D. Pulmonary hypertension
A. Alveolar hypoventilation
2. Which of the following plays a part in the increase in ventilation with moderate exercise?
A. Reflexes from moving limbs
B. Decrease in body temperature
C. Fall in arterial pO2
D. Rise in arterial pCO2
A. Reflexes from moving limbs
3. A 9-year-old boy decided to find out how long he could breathe into and out of a paper bag.
After approximately 2 minutes, his friends noticed that he was breathing very rapidly and
forced him to stop. Which of the following was the most potent stimulus for the boy’s
hyperventilation?
A. Decreased arterial PO2
B. Increased arterial PO2
C. Increased arterial PCO2
D. Decreased arterial PCO2
E. Increased pH
C. Increased arterial PCO2
4. Which of the following conditions would be expected to stimulate the arterial
chemoreceptors?
A. Mild anemia
B. Normal breathing
C. Hypoxia due to ascent to high altitude
D. Hyperventilation
E. Exposure to carbon monoxide
C. Hypoxia due to ascent to high altitude
5. Which of the following would result in a decrease in nerve activity from the peripheral chemoreceptors?
A. A decrease in arterial oxygen content
B. A decrease in blood pH
C. A decrease in arterial blood pressure
D. An increase in arterial pO2
D. An increase in arterial pO2
6. While playing ball, a child fell and injured his head, producing a lesion in the respiratory
center. As a result, he is hypoventilating. Twenty minutes after the accident, which set of
findings would best fit his condition?
pH pCO2 pO2
A. 7.50 30 60
B. 7.35 60 100
C. 7.25 60 60
D. 7.30 70 80
E. 7.40 50 90
C. 7.25 60 60
7. The main reason that respiratory compensation occurs in metabolic acidosis is due to
stimulation of which of the following?
A. The carotid bodies by CO2
B. The carotid bodies by H+
C. The central chemoreceptors by CO2
D. The central chemoreceptors by H+
E. The central chemoreceptors by O2
D. The central chemoreceptors by H+
8. Which set of findings occurs with carbon monoxide inhalation?
Alveolar pO2 Alveolar pCO2 Peripheral Chemoreceptor Activity
A. INC, NO CHANGE, NO CHANGE
B. NO CHANGE, NO CHANGE, NO CHANGE
C. DEC, NO CHANGE, INC
D. DEC, DEC, DEC
E. DEC, DEC, INC
F. NO CHANGE, DEC, INCREASE
B. NO CHANGE, NO CHANGE, NO CHANGE
9. During moderate aerobic exercise, which of the following occurs?
A. Arterial pO2 increases
B. Arterial pCO2 increases
C. Arterial pH increases
D. Blood lactate level decreases
A. Arterial pO2 increases
10. Where are the afferent (sensory) endings for the Hering-Breuer reflex located?
A. Carotid arteries
B. Alveoli
C. External intercostals
D. Bronchi and bronchioles
E. Diaphragm
D. Bronchi and bronchioles
11. A stroke that destroys the respiratory area of the medulla would be expected to lead to which
of the following?
A. Immediate cessation of breathing
B. Apneustic breathing
C. Ataxic breathing
D. Rapid breathing (hyperpnea)
E. Breathing would remain normal
A. Immediate cessation of breathing
12. Which of the following are the most important afferent (sensory) receptors for the respiratory
response to systemic arterial carbon dioxide (Pa-CO2)?
A. CO2 receptors of the aortic and carotid bodies
B. H+ receptors of the aortic and carotid bodies
C. CO2 receptors in the medulla of the brain
D. H+ receptors in the medulla of the brain
E. CO2 receptors in the airways and lungs
D. H+ receptors in the medulla of the brain
2. Voluntary apnea (breath-holding) for 60 seconds will:
A. Decrease alveolar pCO2
B. Increase arterial pO2
C. Inhibit the arterial chemoreceptors
D. Increase alveolar pCO2
D. Increase alveolar pCO2
6. Hyperventilation will result from:
A. A decrease in arterial pCO2 to less than 30 mmHg
B. Direct stimulation of the medulla chemosensitive area caused by an increase in pH
C. An increase in alveolar pCO2
D. An increase in alveolar pO2
C. An increase in alveolar pCO2
12. Peripheral and central chemoreceptors may both contribute to the increased ventilation that occurs as a result of:
A. A decrease in arterial oxygen content
B. A decrease in arterial blood pressure
C. An increase in arterial carbon dioxide tension
D. A decrease in arterial oxygen tension
E. An increase in arterial pH
C. An increase in arterial carbon dioxide tension
causes left shift 7
low temp
low H (increased ph)
low PCO2
low 2,3 DPG
Fetal hgb
carboxyhgb
methemoglobin
factors that cause right shift 6
raised temp
raised H+ (decrease ph)
raised pCO2
raised 2,3 DPG
maternal hb
sickle cell
P50 ____ when right shift in oxyhgb discc curve; and _____ when left shift in curve
increased; decreases
opioid effect on hgb curve
opioids l/t resp depression so CO2 accumulates and curve shift to the right
when there is a left shift in curve, amount of O2 carried by hgb
increased (loading to O2) is facilitated
When there is a right shift in curve, amount of O2 carried by hgb is
reduced (unloading of O2 is facilitated)
the oxyhemoflobin discc curve becomes steep when PaO2 falls below
A. 60mmhg
b. 70 mmhg
c. 80 mmhg
d. 90 mmhg
A. 60 mmhg
the oxyhgb diss curve shift left in response to
A. hypercap
B. hypothermia
C. increased 2,3 DPG
D. metabolic acidosis
B. hypothermia
which of the following conditions is A/W increased in P50
A. sickle cell
B. fetal hgb
C. carboxyhgb
D. methemoglobin
A. sickle cell
the patient is given meperidine for premedication. wheat happens to oxyhgb discc ruve and CO@ blood diss curve
oxyhgb; CO2 diss curve
A. shifts left; shifts left
B. shifts left; shifts right
C. shifts right; shifts right
D. shifts right, shifts left
D. shifts right, shifts left
pacemaker of resp system is found in
A. apneustic center
B. pneumotaxic center
C. ventral resp group
D. dorsal resp group
D. dorsal resp group
central chemoreceptors are stimulated directly by
A. CO2
B. H+
C. both
D. neither
B. H+
peripheral chemoreceptors are most sensitive to
A. increased CO2
B. increased H ions
C. decreased PAO2 <60
D. increased temp
C. decreased PAO2 <60
what nerve carries sensory info from carotid and what nerve carries sensory info from aortic bodies
carotid bodies; aortic bodies
A. vagus; glossopharyngeal
B. vagus; vagus
C. glossopharyngeal; vagus
D. glossopharyngeal; glossopharyngeal
C. glossopharyngeal; vagus
what resp center in pons participates in shutting off inspiration
A, pneumatic center
B. apneustic center
C. both
D. neither
A, pneumatic center
Respiratory center composed of
neurons located bilaterally in medulla oblongata and pons of brain stem
•three major collections of neurons:
•Dorsal respiratory group (DRG)
Located in dorsal portion of medulla
Mainly causes inspiration
•Ventral respiratory group (VRG)
Located in ventrolateral part of medulla
Mainly causes expiration
•Pneumotaxic center (PnC)
Located dorsally in superior portion of pons
Mainly controls rate and depth of breathing
where are the majority of the neurons located
•in nucleus of the tractus solitarius (NTS)
•Additional neurons also in adjacent reticular substance of medulla
What is the nucleus of the tractus solitarius (NTS)
•NTS is sensory termination of both vagal and glossopharyngeal nerves which:
Transmit sensory signals into respiratory center from:
Peripheral chemoreceptors
Baroreceptors
Several types of receptors in lungs
• Basic rhythm of respiration is generated in DRG (pacemaker)
DRG sends action potentials via phrenic and external intercostal nerves to diaphragm and external intercostal muscles
pneumotaxic center limits the Duration of Inspiration and Increases the Respiratory Rate
•Located dorsally in nucleus parabrachialis of upper pons
•Transmits signals to inspiratory area
•Function primarily to limit inspiration controlling the duration of filling phase of lung cycle
•Secondary effect of ↑ rate of breathing d/t limitation of inspiration also shortens expiration and entire period of each respiration
•A strong signal can ↑ rate to 30-40 bpm
•Weak signal can ↓ rate to only 3-5 bpm
•Now called the PRG (pontine respiratory group) in many texts
Ventral Respiratory Group of Neurons-Functions in Both Inspiration and Expiration
•Located in each side of medulla
•Neurons remain almost totally inactive during normal quiet respiration
•Normal quiet breathing is caused only by repetitive inspiratory signals from DRG
•Does not participate in basic rhythmical oscillation that controls respiration
•When respiratory drive for ↑ pulmonary ventilation becomes > normal, VRG contributes extra respiratory drive
•Electrical stimulation of some neurons in VRG cause inspiration, others cause expiration (internal intercostal nerve)
•Especially important in providing powerful expiratory signals to abdominal muscles during very heavy expiration
•Operates as an overdrive mechanism when high levels of pulmonary ventilation are required, especially during heavy exercise
Lung Inflation Signals Limit Inspiration-The Hering-Breuer Inflation Reflex
•Sensory nerve signals from lungs also help control respiration (in addition to CNS mechanisms in brain stem)
•Hering-Breuer inflation reflex:
Stretch receptors located in smooth muscle in walls of bronchi and bronchioles throughout lungs
Transmit afferent (sensory) signals through vagi into DRG neurons when lungs are overstretched
Activates feedback response that "switches off" inspiratory ramp stopping further inspiration (like PnC)
↑ RR like PnC
Probably not activated until VT ↑ > 3 x’s normal (>≈ 1.5 liters per breath)
•In neonates Hering-Breuer reflex is strong and physiologically relevant
•Mainly a protective mechanism preventing excess lung inflation
•Not important factor in normal control of ventilation
Excess CO2 or H+ in blood
•act directly on respiratory center, ↑↑ strength of inspiratory and expiratory motor signals to respiratory muscles
•O2 does not have a significant direct effect
•Acts on peripheral chemoreceptors in carotid and aortic bodies, which transmit signals to respiratory center
What tends to decrease airway resistance?
Asthma
Stimulation by sympathetic fibers
Treatment with acetylcholine
Exhalation to residual volume
Stimulation by sympathetic fibers
A decrease in airway resistance is due to an increase in the diameter of the airway. Asthma causes bronchoconstriction, which is prevented by β-agonists. Sympathetic stimulation of the airways results in a relaxation of airways, decreasing resistance. Acetylcholine is a bronchoconstrictor, increasing resistance. With low lung volumes there is a collapse of the airways, leading to decreased diameter and increased resistance.
A 62-year-old woman is admitted to the hospital with a fever and flu-like symptoms. How does her clinical status influence her HbO2 dissociation curve?
A) shift to the left
B) shift to the right
C) no change
D) downward shift
E) upward shift
B) shift to the right
Which of the following is an appropriate compensatory mechanism for a patient with metabolic alkalosis?
A) Hyperventilation
B) Hypoventilation
C) Increased H+ removal by kidneys
D) Decreased H+ removal by kidneys
E) Both A and C
F) Both B and D
B) Hypoventilation