Nephrology Exam
0.0(0)
0.0(0)
Card Sorting
1/287
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
288 Terms
1
New cards
What are the top 5 functions of the kidneys?
-remove waste
-control BP by secreting renin which initiates RAAS
-stimulates RBC production by secretion of EPO
-maintains bone health by secreting calcitriol --> reducing Ca2+ loss
-controls pH
-control BP by secreting renin which initiates RAAS
-stimulates RBC production by secretion of EPO
-maintains bone health by secreting calcitriol --> reducing Ca2+ loss
-controls pH
2
New cards
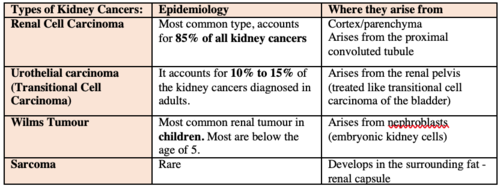
What make up about 90% of all renal cancers?
renal cell carcinoma (parenchyma)- includes adenocarcinomas
3
New cards
What are the types of renal cancers?
-renal cell carcinoma (includes adenocarcinoma)
-transitional cell carcinoma - renal pelvis (linked with cigarette smoking)
-wilms' tumor
renal sarcoma- originated from vasculature or connective tissue of kidney
-transitional cell carcinoma - renal pelvis (linked with cigarette smoking)
-wilms' tumor
renal sarcoma- originated from vasculature or connective tissue of kidney
4
New cards
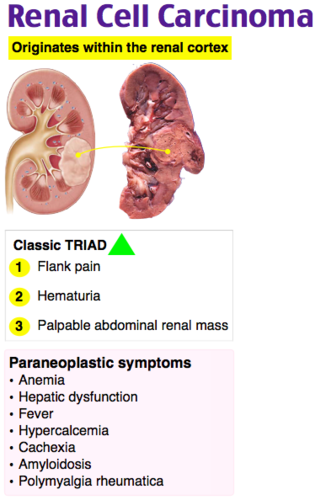
Describe the presentation of a patient with renal cell carcinoma.
-*gross or microscopic hematuria*
-flank pain or mass
-fever, weight loss
-solid renal mass on imaging
-night sweats, fever, malaise, weight loss
-*erythrocytosis but anemia is more common*
-*hypercalcemia*
-*stauffer syndrome* - hepatic dysfunction in absence of liver metastasis
-flank pain or mass
-fever, weight loss
-solid renal mass on imaging
-night sweats, fever, malaise, weight loss
-*erythrocytosis but anemia is more common*
-*hypercalcemia*
-*stauffer syndrome* - hepatic dysfunction in absence of liver metastasis
5
New cards
What are risk factors for renal cell carcinoma?
-*cigarette smoking is the only environmental risk factor*
-obesity, HTN, acquired cystic kidney disease associated with dialysis, ADPKD
-familial causes
-obesity, HTN, acquired cystic kidney disease associated with dialysis, ADPKD
-familial causes
6
New cards
Which renal cancer is associated with paraneoplastic syndrome?
renal cell carcinoma
-Paraneoplastic syndrome is symptoms due to remote effects of cancer
-Paraneoplastic syndrome is symptoms due to remote effects of cancer
7
New cards
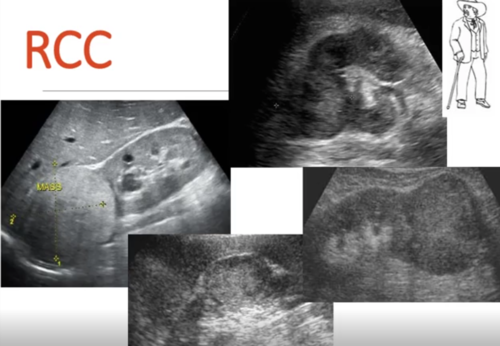
What is the best initial test for renal cell carcinoma?
-US because it is inexpensive, without radiation and high sensitivity
-then do CT or MRI
-then *biopsy or nephrectomy*
-bone scan if metastasis is suspected
-then do CT or MRI
-then *biopsy or nephrectomy*
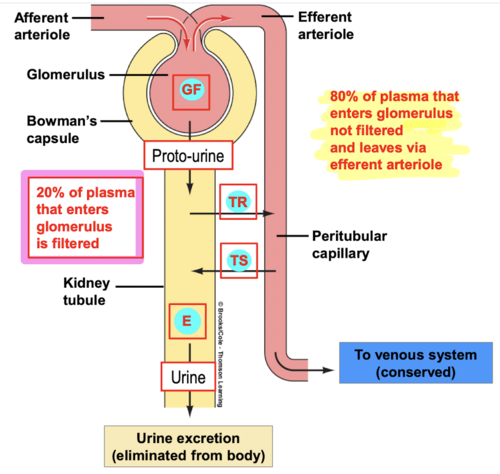
-bone scan if metastasis is suspected
8
New cards
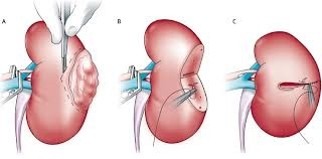
What is the treatment for renal cell carcinoma?
-*surgery is gold standard* - partial or radical- curative in stages 1-3
-resistant to chemo or radiation
-resistant to chemo or radiation
9
New cards
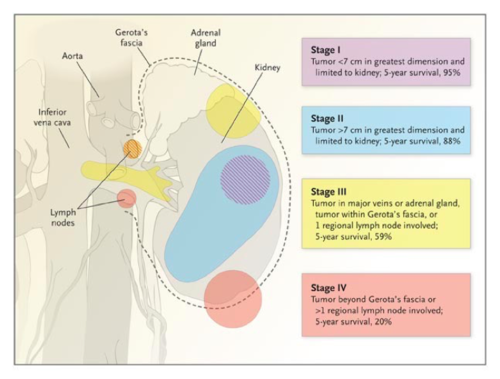
Describe renal cell carcinoma staging.
I: confined to renal capsule and
10
New cards
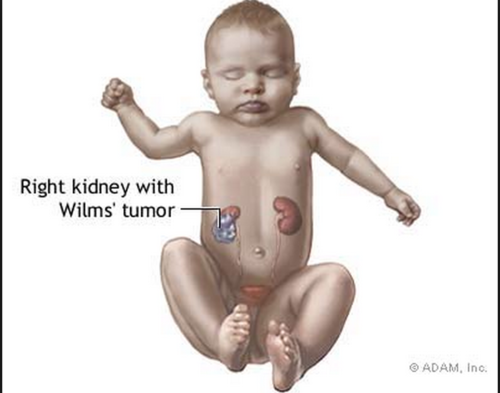
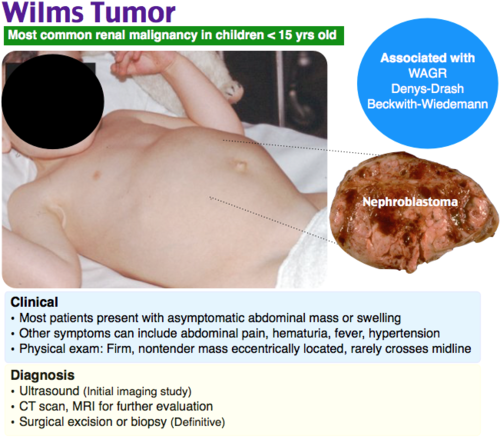
What is Wilms' tumor?
-nephroblastoma
-most common renal malignancy in *children*
-African Americans are more at risk
-most common renal malignancy in *children*
-African Americans are more at risk
11
New cards
Describe the presentation of a patient with Wilms' tumor?
-abdominal swelling or mass w/o other symptoms- rarely crosses midline
-abdominal pain
-hematuria
-HTN
-may have subcapsular hemorrhage (fever, rapid abd enlargement, anemia, HTN)
-abdominal pain
-hematuria
-HTN
-may have subcapsular hemorrhage (fever, rapid abd enlargement, anemia, HTN)
12
New cards
Which patients should be screened for Wilms' tumor?
-Beckwith-Wiedmann syndrome every 3 months until age 7
-WAGR syndrome every 3 months until age 5
-WAGR syndrome every 3 months until age 5
13
New cards
Describe the workup in a patient with a Wilms' tumor?
-*US* then CT or MRI
-*evaluate for lung metastasis*
-SCr, CMP, UA, maybe coagulation studies if indicated
-*evaluate for lung metastasis*
-SCr, CMP, UA, maybe coagulation studies if indicated

14
New cards
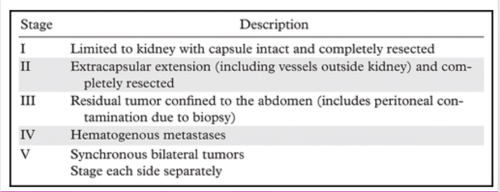
Describe the staging of a Wilms' tumor.
I: limited to kidney and completely excised w/o rupture or biopsy- renal capsule intact
II: tumor extends through renal capsule but all is removed- vessels outside kidney contain tumor - OR "local spillage on removal"
III: residual tumor confined to abd - involvement of abd lymph nodes- "diffuse" contamination by rupture- microscopic margins positive post resection
IV: hematogenous metastasis at any site
V: bilateral renal involvement
II: tumor extends through renal capsule but all is removed- vessels outside kidney contain tumor - OR "local spillage on removal"
III: residual tumor confined to abd - involvement of abd lymph nodes- "diffuse" contamination by rupture- microscopic margins positive post resection
IV: hematogenous metastasis at any site
V: bilateral renal involvement
15
New cards
How are Wilms' tumors treated?
-*surgical excision*
-CTX (chemotherapy) with low risk tumors
-XRT (radiation) for advanced stage and histology
-CTX (chemotherapy) with low risk tumors
-XRT (radiation) for advanced stage and histology
16
New cards
What is the prognosis of Wilms' tumor?
5 year survival of 90%
follow with CT - pulmonary and abdominal Q3mo/2 years then Q6mo/2 more years
follow with CT - pulmonary and abdominal Q3mo/2 years then Q6mo/2 more years
17
New cards
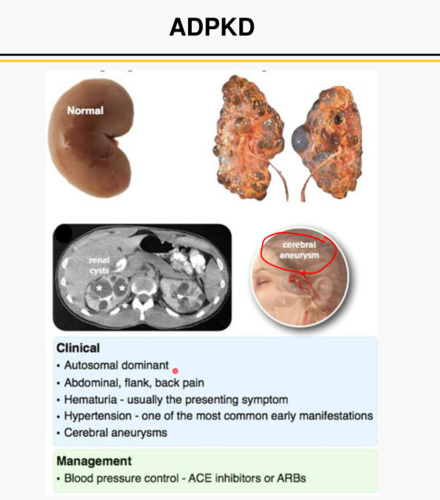
What is ADPKD?
Autosomal dominant polycystic kidney disease
-cysts increase with age
-most common hereditary disorder in the US
-cysts increase with age
-most common hereditary disorder in the US

18
New cards
Describe the presentation of ADPKD.
-often have HTN and abdominal mass (palpable kidneys)
-*family history*
-abdominal/ flank pain
-hematuria
-Hx of UTI/ nephrolithiasis
-*family history*
-abdominal/ flank pain
-hematuria
-Hx of UTI/ nephrolithiasis
19
New cards
What genetic mutations were found for ADPKD?
PKD1 and PKD2
-PKD1 has worse prognosis and faster progression of disease
-PKD1 has worse prognosis and faster progression of disease
20
New cards
How is ADPKD treated?
treat symptoms
-Abd/ flank pain: *cyst decompression/drainage/ removal and analgesics*
-Hematuria: *bed rest, hydration*
-renal infection: *ABX- fluoroquinolones, bactrim, chloramphenicol*
-nephrolithiasis: *hydration*
-HTN: *cyst decompression and aggressive pharmacotherapy to prolong ESRD*
-cerebral aneurysms and other vascular problems may occur
-Vasopressin receptor antagonist can slow worsening of kidney function
-avoid caffeine, low protein, low salt diet
-Abd/ flank pain: *cyst decompression/drainage/ removal and analgesics*
-Hematuria: *bed rest, hydration*
-renal infection: *ABX- fluoroquinolones, bactrim, chloramphenicol*
-nephrolithiasis: *hydration*
-HTN: *cyst decompression and aggressive pharmacotherapy to prolong ESRD*
-cerebral aneurysms and other vascular problems may occur
-Vasopressin receptor antagonist can slow worsening of kidney function
-avoid caffeine, low protein, low salt diet
21
New cards
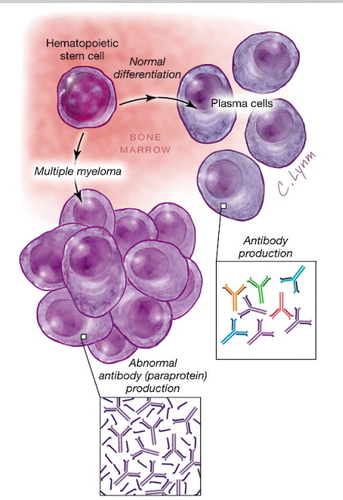
A patient has a urinalysis done and it comes back with Bence Jones protein, what might they have?
multiple myeloma
-Bence Jones protein is light chain Ig - causes renal toxicity and obstruction
-*hypercalcemia* is also found
-Bence Jones protein is light chain Ig - causes renal toxicity and obstruction
-*hypercalcemia* is also found
22
New cards
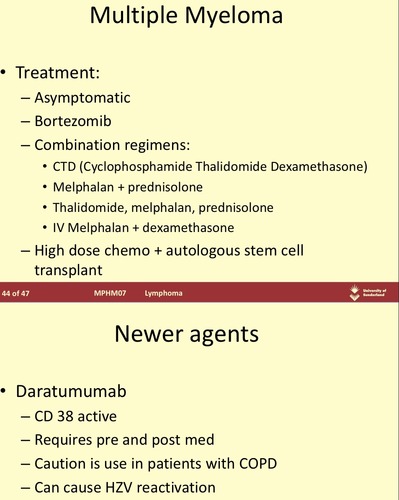
How is multiple myeloma treated?
-correct hypercalcemia
-volume repletion
-chemo for MM
-volume repletion
-chemo for MM
23
New cards
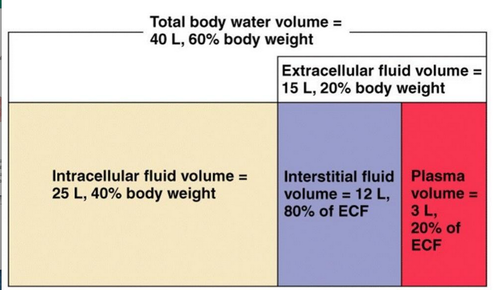
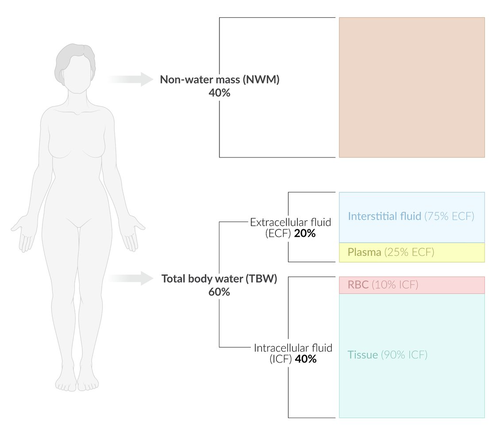
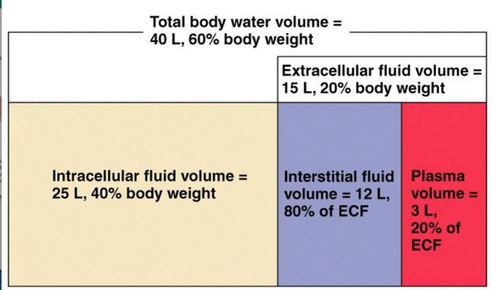
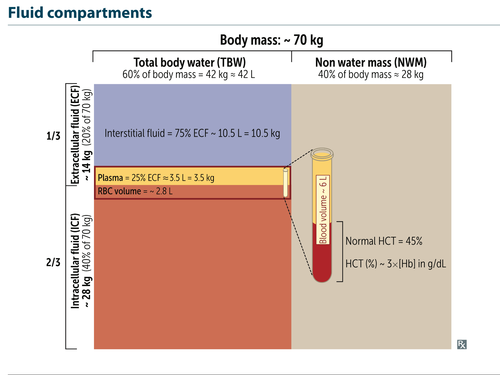
How much of the total body water does ICF make up? Which ions are found there?
2/3
K+, Phosphate, Sulfate
K+, Phosphate, Sulfate
24
New cards
How much of the total body water does ECF make up? Which ions are found there?
1/3
Na+, Cl-, Bicarb
Na+, Cl-, Bicarb
25
New cards
How much of the ECF does plasma make up?
1/4
26
New cards
How much of the ECF does the interstitial fluid make up?
3/4
27
New cards
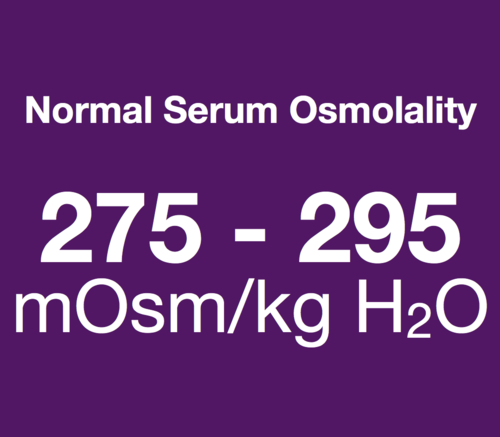
What is a normal serum osmolality?
290 mosm/kg H2O
28
New cards
What is the gold standard for evaluating renal electrolytes?
24 hour urine collection
29
New cards
What does low (
-fractional excretion of Na+ (FENA)
-renal reabsorption (prerenal)
-renal reabsorption (prerenal)
30
New cards
What does high (>1%) FENA indicate?
-fractional excretion of Na+ (FENA)
-renal wasting (intrinsic)
-renal wasting (intrinsic)
31
New cards
What is an osmolar gap?
-difference between serum osmolality and calculated osmolality *>10 mm/kg* indicated gap
-suggests unmeasured fluids such as ethanol, ethylene glycol, methanol
-suggests unmeasured fluids such as ethanol, ethylene glycol, methanol
32
New cards
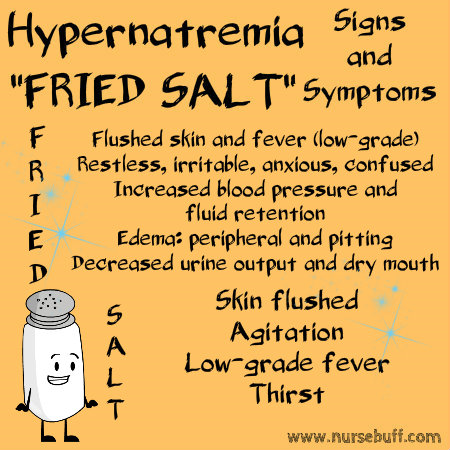
How is serum osmolality calculated?
should = 285-295 mmol/kg
33
New cards
What is the normal physiologic response to hypernatremia?
increased thirst mechanism
34
New cards
What usually causes hypernatremia?
-free water loss, hypotonic fluid loss (diabetes insipidus), urinary loss, GI loss, and insensible loss
-renal losses of glucose or osmotic diuresis with mannitol
-non renal losses such as excessive sweating, excessive bowel movements, osmotic diarrhea
-renal losses of glucose or osmotic diuresis with mannitol
-non renal losses such as excessive sweating, excessive bowel movements, osmotic diarrhea
35
New cards
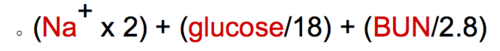
Describe the presentation of a patient with hypernatremia.
-*dehydration
-positive orthostatic hypotension*
-flushed skin
-hyperthermia, fever
-*oliguria* and anuria
-hyperventilation
-hyperreflexia
-neurologic manifestations
-thirst, restlessness, irritability
-*lethargy, weakness*, disorientation
-*delirium, seizures, coma*
-positive orthostatic hypotension*
-flushed skin
-hyperthermia, fever
-*oliguria* and anuria
-hyperventilation
-hyperreflexia
-neurologic manifestations
-thirst, restlessness, irritability
-*lethargy, weakness*, disorientation
-*delirium, seizures, coma*
36
New cards
What findings occur in *central* diabetes insipidus?
low urine sodium and polyuria
37
New cards
What finding occur in *nephrogenic* diabetes insipidus?
antidiuretic stimulation does *not* increase urine osmolality
38
New cards
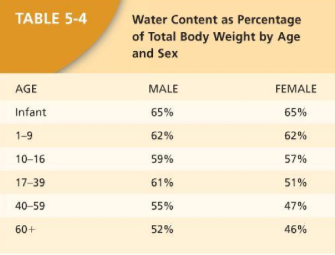
What is the formula for total body water?
TBW= patient weight in kg x % (based on gender and age)
usually 40-60% of patients weight
-Example =70kg*.55 for a 55 y/o male= 38.5L
usually 40-60% of patients weight
-Example =70kg*.55 for a 55 y/o male= 38.5L
39
New cards
How is total water deficit calculated for acute hypernatremia with acute volume loss?
water deficit= current TBW* ((serum [Na]/140)-1)
![water deficit= current TBW* ((serum [Na]/140)-1)](https://knowt-user-attachments.s3.amazonaws.com/7cfba228859d4cca8c416bb21f54d546.png)
40
New cards
What is the total water deficit of a 70kg, 55 y/o male with a Na+ of 160 (water content 55% for this age/sex) who has acute hypernatremia?
(70kg x .55) x ((160/140)-1) = 5.4999L
41
New cards
How do you calculate flow rate in acute hypernatremia? What is considered acute?
-total water deficit is calculated them divided by 24 hours and multiply by 1000ml which gives you the hourly rate for a 24 hour infusion
-acute if under 48 hours
-acute if under 48 hours
42
New cards
How do you calculate flow rate for chronic hypernatremia? What is considered chronic?
-patients weight in kg * 1.35mL/hr which will give you the hourly rate for a 24 hour infusion
-chronic >48 hours
-chronic >48 hours
43
New cards
Why is it important to not correct chronic hypernatremia too quickly?
it can cause increase in ICP (cerebral edema) and pulmonary edema
44
New cards
How is hypernatremia treated?
-underlying cause
-replace water orally preferred or IV *5% dextrose solution (D5W)*
•hypovolemic: replace with isotonic fluid (NS)
•euvolemic: 5% dextrose to allow excess Na+ to be excreted
•hypervolemic: loop diuretics or dialysis (if Na+ >200Eq/L)
-replace electrolytes if needed
-replace water orally preferred or IV *5% dextrose solution (D5W)*
•hypovolemic: replace with isotonic fluid (NS)
•euvolemic: 5% dextrose to allow excess Na+ to be excreted
•hypervolemic: loop diuretics or dialysis (if Na+ >200Eq/L)
-replace electrolytes if needed
45
New cards
How is hypovolemic hypernatremia treated?
-replace with normal saline (isotonic fluid)
-replacing electrolytes PRN
-replacing electrolytes PRN
46
New cards
How is euvolemic hypernatremia treated?
-replace fluid with D5W to allow excess Na+ to be excreted
-replacing electrolytes PRN
-replacing electrolytes PRN
47
New cards
How is hypervolemic hypernatremia treated?
-loop diuretics or dialysis (if Na>200mEq/L
-replacing electrolytes PRN
-replacing electrolytes PRN
48
New cards
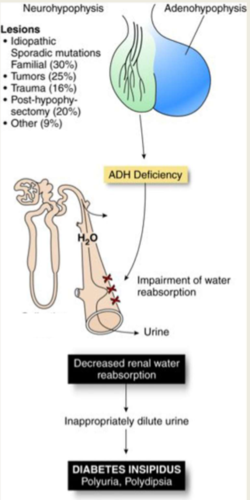
What is neurogenic diabetes insipidus?
-deficient secretion of arginine vasopressin (AVP) from posterior pituitary
49
New cards
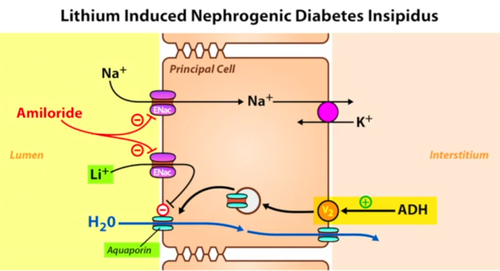
What is nephrogenic diabetes insipidus? What causes it?
-kidneys are unresponsive to normal vasopressin levels
-inherited X-linked trait or acquired (lithium therapy, hypokalemia, hypercalcemia, or renal disease)
-inherited X-linked trait or acquired (lithium therapy, hypokalemia, hypercalcemia, or renal disease)
50
New cards
Describe the presentation of diabetes insipidus? What labs would be normal/ abnormal?
-*polyuria, nocturia, polydipsia*
-glucose - normal
-serum Na over 145 and urine osmolality < 300mOsm/kg
-glucose - normal
-serum Na over 145 and urine osmolality < 300mOsm/kg
51
New cards
How can you differentiate between neurogenic and nephrogenic diabetes insipidus in a patient?
desmopressin challenge
-if urine osmolality improves (>400) then its central (neurogenic)
-if urine osmolality doesn't change them its nephrogenic
-if urine osmolality improves (>400) then its central (neurogenic)
-if urine osmolality doesn't change them its nephrogenic
52
New cards
How is neurogenic diabetes insipidus treated?
-parenteral or intranasal desmopressin
-OR thiazide diuretics, chlorpropamide, carbamazepine for mild disease
-OR thiazide diuretics, chlorpropamide, carbamazepine for mild disease
53
New cards
How is nephrogenic diabetes insipidus treated?
-thiazide diuretics or indomethacin
-dietary measures, limiting salt and proteins intake can be helpful
-dietary measures, limiting salt and proteins intake can be helpful
54
New cards
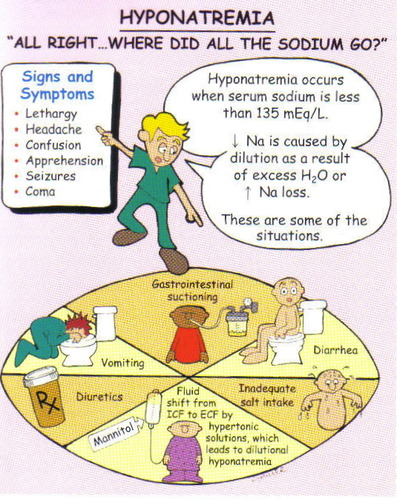
What is the most common electrolyte abnormality in hospitalized patients?
hyponatremia
55
New cards
What levels of serum Na+ indicate a high mortality rate?
•
56
New cards
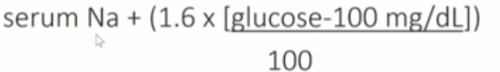
What is a corrected Na+?
Corrected Na+ = serum Na+ +. ( (glucose serum-100) * 0.016)
-use this if patient is hyperglycemic to get true Na value
-use this if patient is hyperglycemic to get true Na value
57
New cards
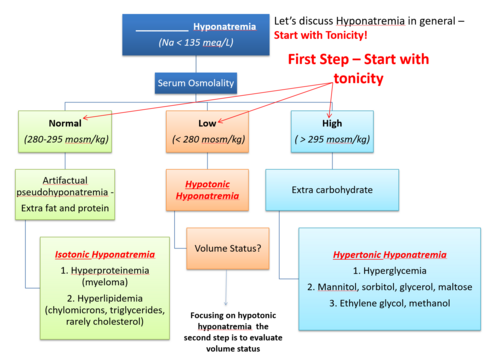
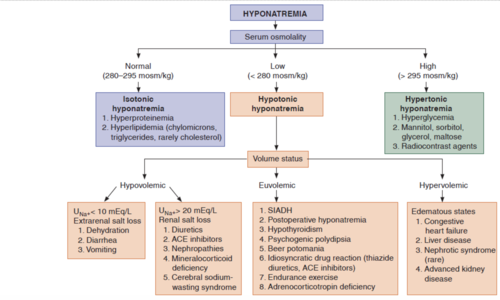
What causes isotonic hyponatremia?
-hyper*protein*emia/ hyperalbuminemia - due to multiple myeloma or macroglobulinemia
-hyper*lipid*emia (milky appearing serum) - due to famlial hyperlipidemia or nephrotic syndrome
-Pseudohyponatremia - increase in plasma solids such as *lipid or protein* - lowers the proportion of each liquids per L of plasma which lowers the plasma Na+ concentration w/o altering the Na+ in the liquid compartment
-hyper*lipid*emia (milky appearing serum) - due to famlial hyperlipidemia or nephrotic syndrome
-Pseudohyponatremia - increase in plasma solids such as *lipid or protein* - lowers the proportion of each liquids per L of plasma which lowers the plasma Na+ concentration w/o altering the Na+ in the liquid compartment
58
New cards
What causes hypertonic hyponatremia?
-*hyperglycemia*
-mannitol administration
-these cause shift of H2O from the ICF to the ECF and lowers serum Na+ concentration
-mannitol administration
-these cause shift of H2O from the ICF to the ECF and lowers serum Na+ concentration
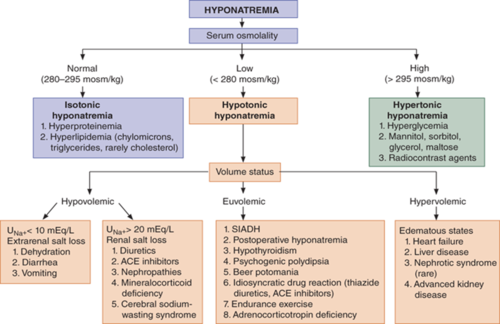
59
New cards
What causes hypervolemic hypotonic hyponatremia?
CHF, Nephrotic syndrome, Renal failure (late stage/ ESRD), Hepatic cirrhosis
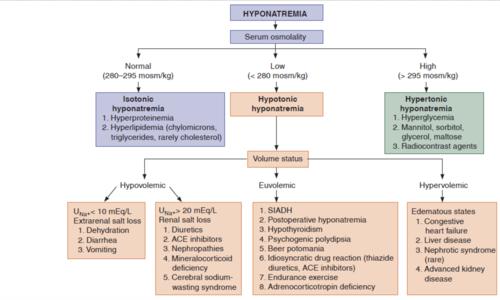
60
New cards
What causes euvolemic hypotonic hyponatremia?
-severe hypothyroidism, drugs, psychogenic polydipsia, addison's disease
-*SIADH (most common)* can be due to malignancy or drugs
-renal failure- no excretion of free water
-post surgery
-HIV infection
-endurance exercise hyponatremia (combination of excess hypotonic fluid intake and continued ADH secretion)
-malignancy
-*SIADH (most common)* can be due to malignancy or drugs
-renal failure- no excretion of free water
-post surgery
-HIV infection
-endurance exercise hyponatremia (combination of excess hypotonic fluid intake and continued ADH secretion)
-malignancy
61
New cards
What causes hypovolemic hypotonic hyponatremia?
-renal losses
diuretic use, nephropathy (salt wasting), addison's disease (adrenal insufficiency, GU obstruction)
-nonrenal sodium loss
•GI losses (diarrhea, vomiting), insensible losses (skin and respiratory tract), third spacing (ileus, burns)
-thiazide diuretics
diuretic use, nephropathy (salt wasting), addison's disease (adrenal insufficiency, GU obstruction)
-nonrenal sodium loss
•GI losses (diarrhea, vomiting), insensible losses (skin and respiratory tract), third spacing (ileus, burns)
-thiazide diuretics
62
New cards
What is ADH independent hyponatremia?
Uosm (urine osmolarity)
63
New cards
Describe the presentation of hypovolemic hypotonic hyponatremia? What labs would be normal/ abnormal?
-s/s: orthostatic hypotension, dry mucous membranes
-labs: increased BUN/ Creatinine (if renal), decreased urine Na+
-labs: increased BUN/ Creatinine (if renal), decreased urine Na+
64
New cards
Describe the presentation of hyponatremia.
-Symptoms: HA, lethargy, nausea, disorientation, marked confusion, emesis, seizures, coma, brain herniation, death
-chronic may be asymptomatic
-Signs: weakness, hyporeflexia, orthostatic hypotension, Cheyne-stokes respirations, delirium, coma, stupor
-chronic may be asymptomatic
-Signs: weakness, hyporeflexia, orthostatic hypotension, Cheyne-stokes respirations, delirium, coma, stupor
65
New cards
Describe the workup in a patient you suspect has hyponatremia?
-serum Na+
66
New cards
What is the urine Na+ content in euvolemic hypotonic hyponatremia?
>20mEq/L
67
New cards
A patient has low serum sodium, low plasma osmolality and decreased urine sodium. What is the cause?
*Nonrenal*
Hypervolemic hypotonic hyponatremia
-nephrotic syndrome, CHF, cirrhosis
Hypervolemic hypotonic hyponatremia
-nephrotic syndrome, CHF, cirrhosis
68
New cards
A patient has low serum sodium, low plasma osmolality and increased urine sodium. What is the cause?
*Renal*
Hypervolemic hypotonic hyponatremia
-acute and chronic renal failure
Hypervolemic hypotonic hyponatremia
-acute and chronic renal failure
69
New cards
How is hypovolemic hypotonic hyponatremia treated?
-*isotonic saline* to replace volume
-if 2º to diuretics may need K+ repletion
-if 2º to diuretics may need K+ repletion
70
New cards
How is hypervolemic hypotonic hyponatremia treated?
-salt and fluid restriction + *loop diuretic*
-V2 receptor antagonist may be considered
-dialysis is last resort
-V2 receptor antagonist may be considered
-dialysis is last resort
71
New cards
How is euvolemic hypotonic hyponatremia treated?
-*free water restriction* is treatment of choice
-vasopressin antagonist (Tolvaptan/ Conivatan) if severe
-vasopressin antagonist (Tolvaptan/ Conivatan) if severe
72
New cards
When is Tolvaptan (Samsca)/ Conivaptan indicated and what is their action?
-euvolemic and hypervolemic hyponatremia
-*contraindicated* in hypovolemic
-V1A and V2 vasopressin receptor antagonist - induces both water and Na diuresis with improvement in plasma Na+ levels
-*contraindicated* in hypovolemic
-V1A and V2 vasopressin receptor antagonist - induces both water and Na diuresis with improvement in plasma Na+ levels
73
New cards
How is severe symptomatic hyponatremia (Na
*hypertonic saline (3%)*
consult nephrology
consult nephrology
74
New cards
How is chronic hyponatremia treated if it is unresponsive to fluid restriction?
demeclocycline - induces nephrogenic diabetes insipidus
75
New cards
What happens when hyponatremia is overcorrected too quickly?
-central pointe myelinolysis AKA iatrogenic cerebral osmotic demyelination or osmotic demyelination syndrome (ODS)
76
New cards
How is symptomatic acute hyponatremia managed?
-urgent correction by 4-6mmol/L (i think per day)
-if severe symptoms: 100mL of 3%NaCl infused over 10 min x 3 as needed
-mild-mod symptoms with low risk of herniation: 3% NaCl infused at 0.5-2mL/kg/h
-if severe symptoms: 100mL of 3%NaCl infused over 10 min x 3 as needed
-mild-mod symptoms with low risk of herniation: 3% NaCl infused at 0.5-2mL/kg/h
77
New cards
How is symptomatic chronic hyponatremia managed?
minimum correction of serum Na+ by 4-8mmol/L per day with lower goal (4-6) if high risk of ODS
-max correction of 10-12mmol/L per day; 18mmol/L in 48 hours
-max correction of 10-12mmol/L per day; 18mmol/L in 48 hours
78
New cards
How is hyponatremia due to SIADH managed?
-*fluid restriction at 1500mL to start* is first line
-if low renal electrolyte-free water excretion or if serum Na+ does not correct over 24-48 hours of fluid restriction --> consider demeclocycline, urea, and vasopressin receptor antagonist
-if low renal electrolyte-free water excretion or if serum Na+ does not correct over 24-48 hours of fluid restriction --> consider demeclocycline, urea, and vasopressin receptor antagonist
79
New cards
How much plasma is filtered by the glomerulus?
20%
80
New cards
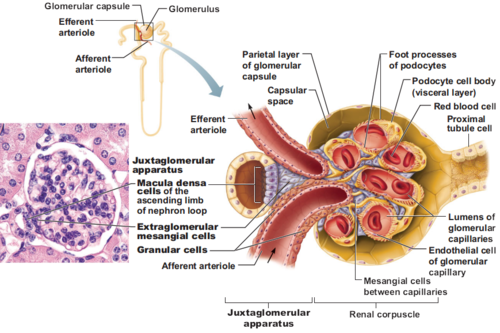
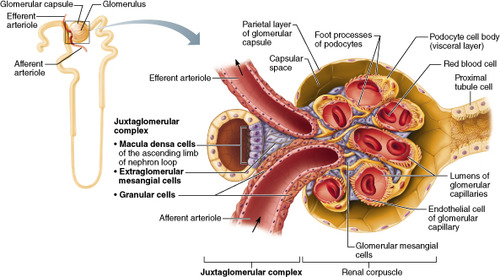
What are juxtaglomerular cells?
-"baroreceptors" sensing afferent arteriole pressure
-increase renin release when there is a drop in pressure
-increase renin release when there is a drop in pressure
81
New cards
What are macula densa cells?
-cells of the early distal tubule- sense NaCl delivery (ion concentration)
-release vasoactive substances when there is a drop in solute levels
-release vasoactive substances when there is a drop in solute levels
82
New cards
What is azotemia?
excess urea or other nitrogenous waste products in the blood as a result of kidney insufficiency- measured by BUN and/or creatinine
83
New cards
What is uremia?
clinical manifestation of azotemia (increased nitrogenous waste products in the blood)
84
New cards
What is the difference between oliguria and anuria?
oliguria: decreased urine output (100-400mL (cc) /day)
anuria:
anuria:

85
New cards
What is an acute kidney injury?
-sudden increase in serum BUN and/or creatinine
-reversible
-results in inability to maintain acid-base, fluid and electrolyte balance or to excrete nitrogenous waste
-reversible
-results in inability to maintain acid-base, fluid and electrolyte balance or to excrete nitrogenous waste
86
New cards
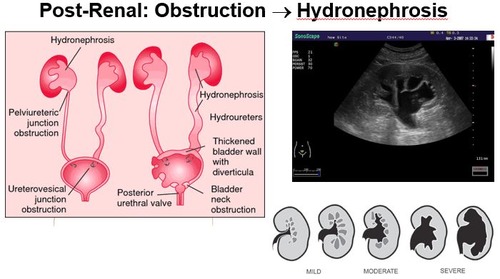
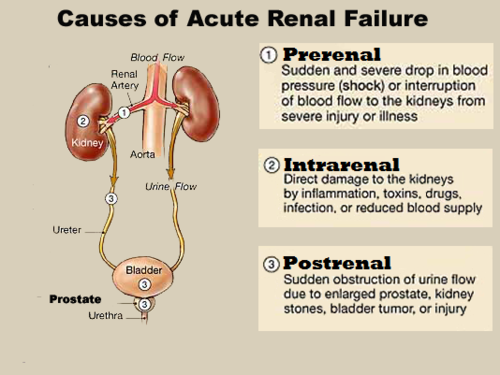
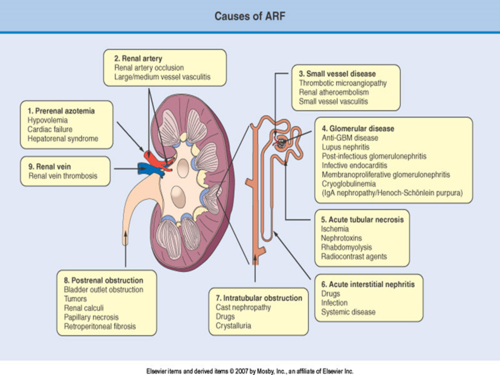
What causes a postrenal AKI?
-urinary tract *obstruction* affecting both kidneys causing back pressure to bowman's space- afferent arteriole can dilate to compensate but will fail --> under perfused areas of the renal cortex and decrease of GFR
•Ureteric: caliculi, blood clots, papillary necrosis, cancer, external compression
•Bladder: neurogenic bladder, BPH, caliculi, blood clots, cancer
•Intratubular crystallization: uric acid, Ca oxalate, acyclovir, sulfonamide, methotrexate
•Ureteric: caliculi, blood clots, papillary necrosis, cancer, external compression
•Bladder: neurogenic bladder, BPH, caliculi, blood clots, cancer
•Intratubular crystallization: uric acid, Ca oxalate, acyclovir, sulfonamide, methotrexate
87
New cards
What causes a prerenal AKI?
-*most common AKI*
-renal hypoperfusion with intact parenchyma- caused by impaired renal blood flow- normal compensatory mechanism is release of ATII --> afferent arteriole vasodilation and constriction of efferent arterioles to maintain GFR but this will fail if prolonged
•Hypovolemia: hemorrhage, GI fluid loss, renal fluid loss, extravascular sequestration (burns, pancreatitis, renal artery stenosis, severe hyperalbuminemia), decreased intake
•Low cardiac output
•systemic vasodilation: sepsis, anti hypertensives, anaphylaxis
•renal vasoconstriction: hypercalcemia, catecholamines, amphotericin B
•Impairment of renal autoregulatory responses: NSAIDS, ACEI, ARBs
-renal hypoperfusion with intact parenchyma- caused by impaired renal blood flow- normal compensatory mechanism is release of ATII --> afferent arteriole vasodilation and constriction of efferent arterioles to maintain GFR but this will fail if prolonged
•Hypovolemia: hemorrhage, GI fluid loss, renal fluid loss, extravascular sequestration (burns, pancreatitis, renal artery stenosis, severe hyperalbuminemia), decreased intake
•Low cardiac output
•systemic vasodilation: sepsis, anti hypertensives, anaphylaxis
•renal vasoconstriction: hypercalcemia, catecholamines, amphotericin B
•Impairment of renal autoregulatory responses: NSAIDS, ACEI, ARBs
88
New cards
What causes an intrinsic AKI?
-Parenchymal renal disease: *acute tubular necrosis* (most common- often after vascular surgery), cortical necrosis, acute glomerulonephritis, microvascular disease, allograft rejections, or interstitial disease
•aminoglycosides (neomycin, gentamycin, tobramycin)
•*radiocontrast media*
•chemotherapy - Cisplatin
•aminoglycosides (neomycin, gentamycin, tobramycin)
•*radiocontrast media*
•chemotherapy - Cisplatin
89
New cards
What are the 4 categories of intrinsic AKI?
-Vascular- vasculitis, malignant HTN, TTP/HUS, emboli/thromboemboli vein or artery
-Glomerular- glomerulonephritis
-Tubular- ischemia, infection/sepsis, toxins (exogenous: radiocontrast, chemo or endogenous: rhabdomylysis, hemolysis)
-Interstitial-allergic/drug rxns, infiltration (lymphoma, sarcoidosis), inflammatory/ nonvascular (Sjogrens), intratubular obstruction (enodgenous or exogenous)
-Glomerular- glomerulonephritis
-Tubular- ischemia, infection/sepsis, toxins (exogenous: radiocontrast, chemo or endogenous: rhabdomylysis, hemolysis)
-Interstitial-allergic/drug rxns, infiltration (lymphoma, sarcoidosis), inflammatory/ nonvascular (Sjogrens), intratubular obstruction (enodgenous or exogenous)
90
New cards
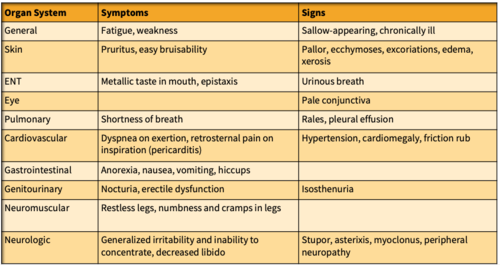
What are signs/symptoms of uremia?
91
New cards
What diagnostic studies are helpful to differentiate what kind of AKI?
-UA then 24 hour urine collection- to monitor fluid balance
-Electrolytes in serum and urine - look for *hyperkalemia*
-ABG for *metabolic acidosis*
-CBC for *infection or anemia*
-biopsy if needed
-EKG due to electrolyte imbalances
-US to visualize the kidney
-IV Urography : to evaluate urinary tract- IVP requires contrast
-CT scan: to evaluate solid or cystic lesions
-MRI: for glomerulonephritis, hydronephritis, and renal vascular occlusion
-Arteriography and venography
-Electrolytes in serum and urine - look for *hyperkalemia*
-ABG for *metabolic acidosis*
-CBC for *infection or anemia*
-biopsy if needed
-EKG due to electrolyte imbalances
-US to visualize the kidney
-IV Urography : to evaluate urinary tract- IVP requires contrast
-CT scan: to evaluate solid or cystic lesions
-MRI: for glomerulonephritis, hydronephritis, and renal vascular occlusion
-Arteriography and venography
92
New cards
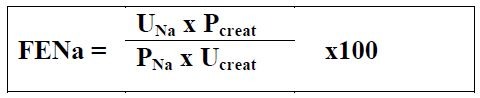
What is FENa and how is it calculated?
- Fraction Excretion of Sodium
- FENa = (urine Na+ x serum Cr)/ (serum Na+ x urine Cr)
- FENa = (urine Na+ x serum Cr)/ (serum Na+ x urine Cr)
93
New cards
What does >20:1 BUN:Cr ratio indicate for AKI?
prerenal, post renal or acute glomerulonephritis
94
New cards
What does
intrarenal (ATN or acute interstitial nephritis)
95
New cards
Which AKI's have high urine Na+?
Acute tubular necrosis
96
New cards
Which AKI's have low urine Na+?
prerenal or acute glomerularnephritis
97
New cards
What indicates significant irreversible renal disease?
98
New cards
Why is Gadolinium contraindicated in stage 4-5 CKD, AKI, or a kidney transplant?
risk of nephrogenic systemic fibrosis
99
New cards
What is the gold standard for diagnosis of renal vein thrombosis?
venography
100
New cards
How is AKI treated?
depends on cause
-manage BP, treat infections, kidney rest
-consider drugs and metabolites not excreted
-low protein, high carb diet
-*primary goal is to maintain the individuals life until recovery*
-dialysis
-manage BP, treat infections, kidney rest
-consider drugs and metabolites not excreted
-low protein, high carb diet
-*primary goal is to maintain the individuals life until recovery*
-dialysis