Optic Nerve & Visual Pathway
1/125
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
126 Terms
the ON is composed of:
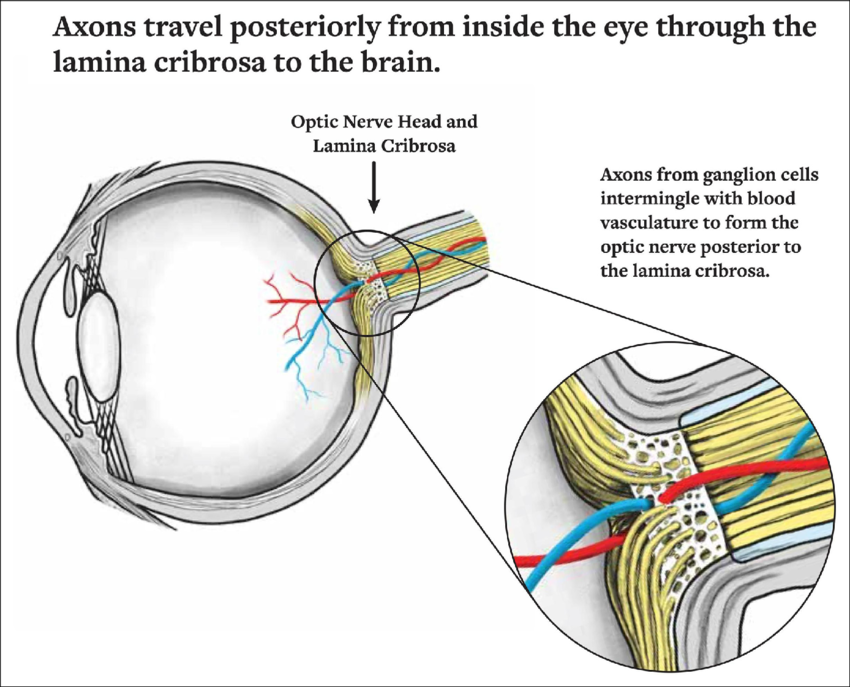
GC axons that make a 90 degree turn at the optic disc and make up the ON
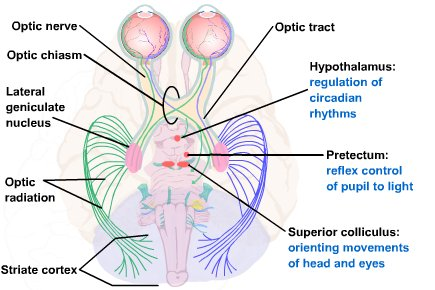
4 paths of GC
synapse in the LGN and travel to the primary visual cortex (V1)
superior colliculus to help with saccades
pretectal nucleus to help with pupil movement
hypothalamus to help with circadian rhythm
does the ON have regenerative abilities
no (little to none)
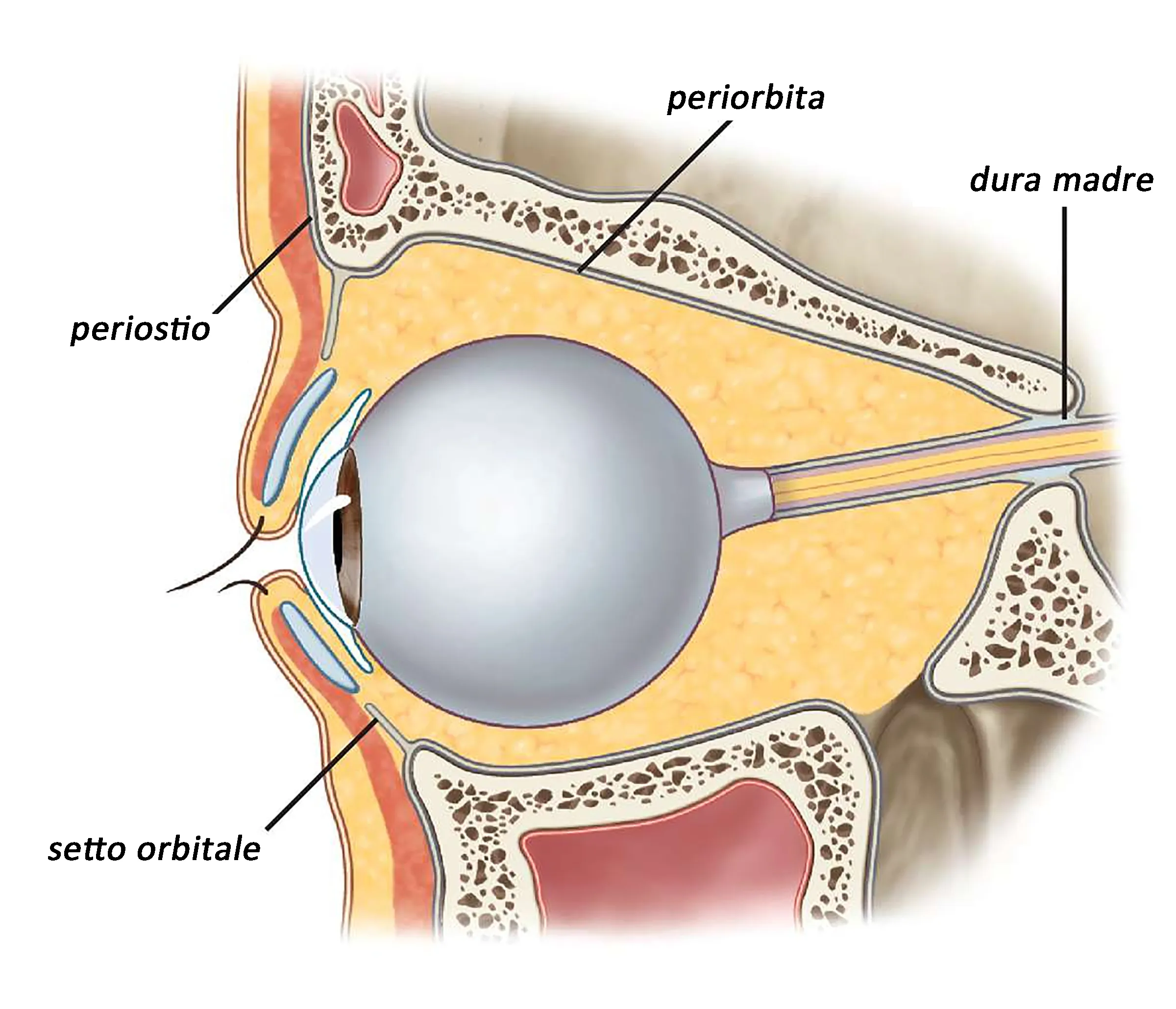
what surrounds the intraorbital (post-laminar) ON
pia, arachnoid, and dura membranes continuous with the meninges of the brain (inner to outer layers: PAD)

what is the subarachnoid space of the ON between and what does it contain
between the pia and arachnoid
contains CSF
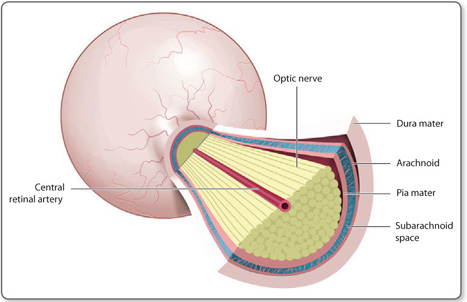
what 2 meningeal layers fuse together
dura and arachnoid
the dura and arachnoid fuse and become continuous with what ocular structures
sclera and periorbita
what meningeal layer continues with the intracranial portion of the ON
only the pia
the dura and arachnoid do not continue intracranially with the ON
why does papilledema cause blurred disc margins
an increase in ICP causes CSF from the subarachnoid space to leak over into the superficial optic disc
CSF spreads over the disc margins to the surrounding RNFL
what cells provide myelination to ON axons posterior to the lamina
oligodendrocytes
role of oligodendrocytes in the ON
myelinate the ON axons posterior to the lamina cribrosa
role of astrocytes in the ON
replace muller cells in the ILM of the ON
provide structural support to ON axons
schwann cells (do/do not) provide myelination for the ON
do not
schwann cells are not found within the ON
why do 90% of patients with optic neuritis report pain on eye movement
the ON sheath is attached to the sheaths that surround the SR and MR
blood supply of retinal NFL of ON
SPCAs and CRA
blood supply of intraocular ON (pre-lamina and lamina)
circle of zinn (anastomoses of SPCAs)
other SPCA branches
blood supply of intraorbital ON (post-lamina)
CRA branches
pial mater arterial plexus
blood supply of intracranial ON
ophthalmic, anterior, cerebral, anterior communication, and IC arteries
ON (is/is not) able to autoregulate its blood supply
is
like the retina
the choroid cannot autoregulate
optic disc location
most anterior portion of ON
nasal retina 15 degrees from fixation (fovea)
subtends angle of 5-7 degrees
the optic disc is larger (vertically/horizontally)
vertically
why does the ON act as a blind spot
the ON has no photoreceptors
only has RNFL and a glial membrane made of astrocytes
what layers is the ON composed of
RNFL
glial membrane made of astrocytes (ILM)
name of ILM made of astrocytes in the ON
ILM of Elschnig
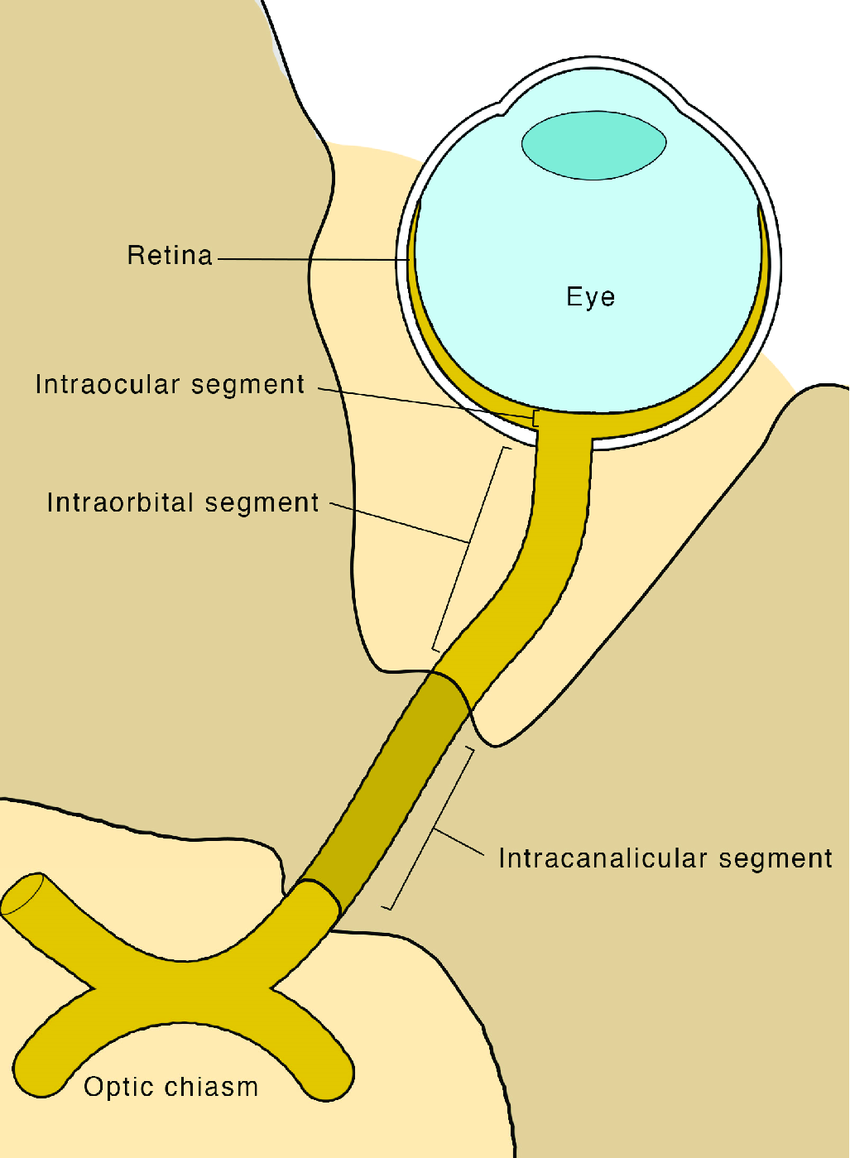
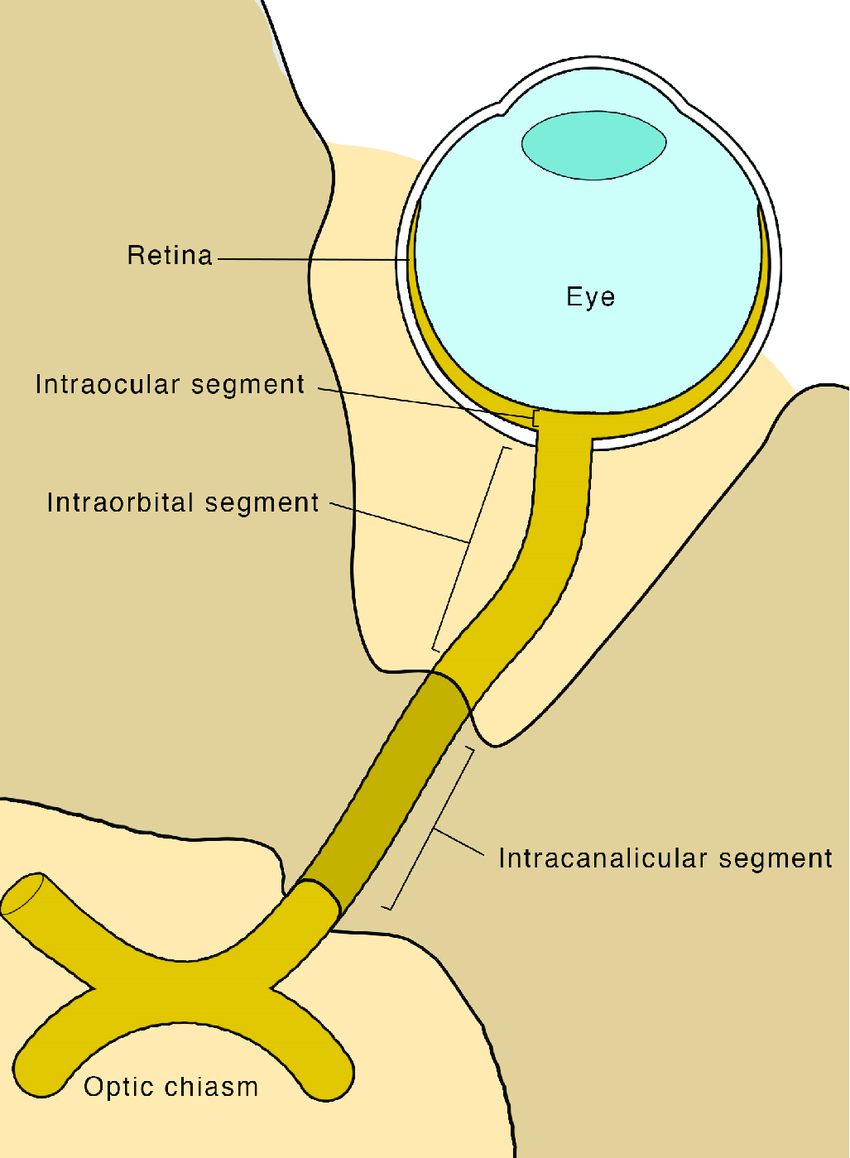
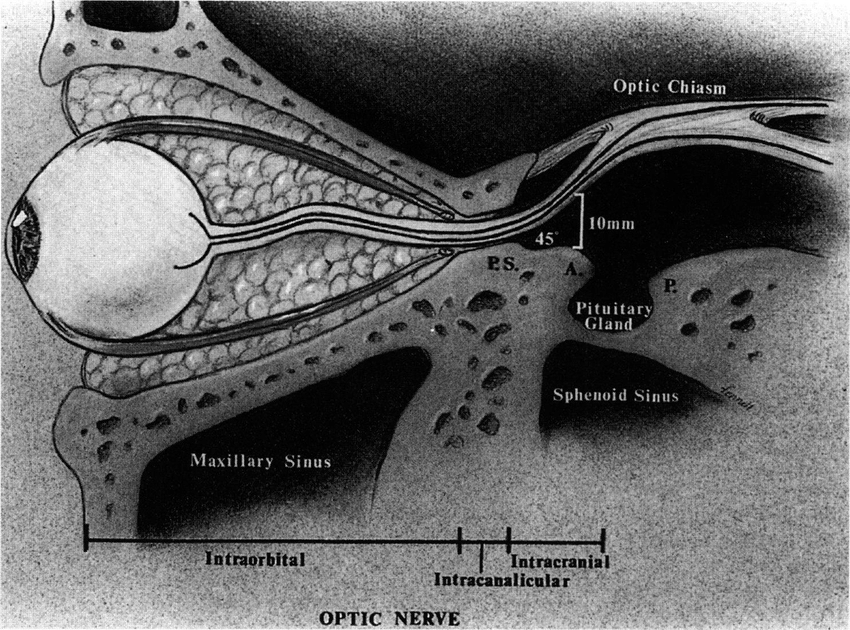
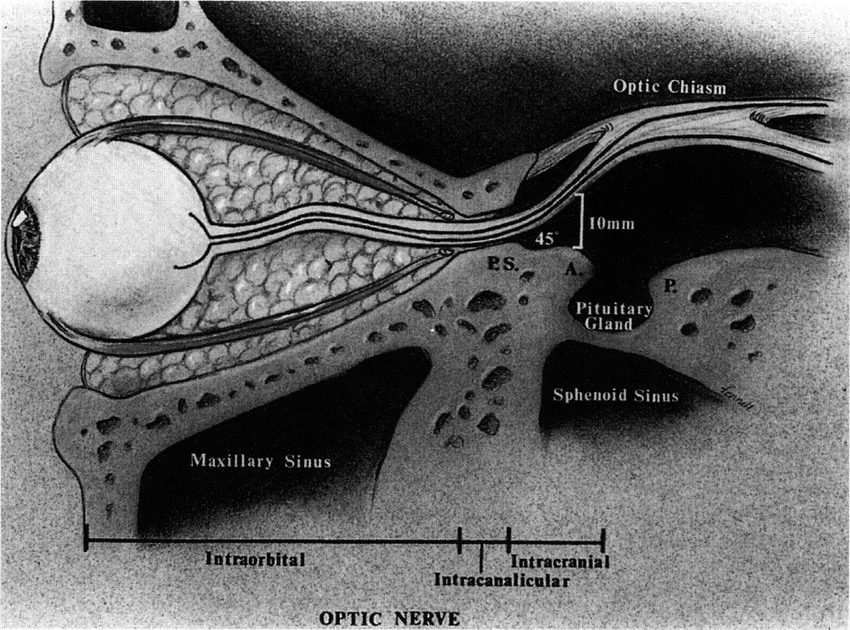
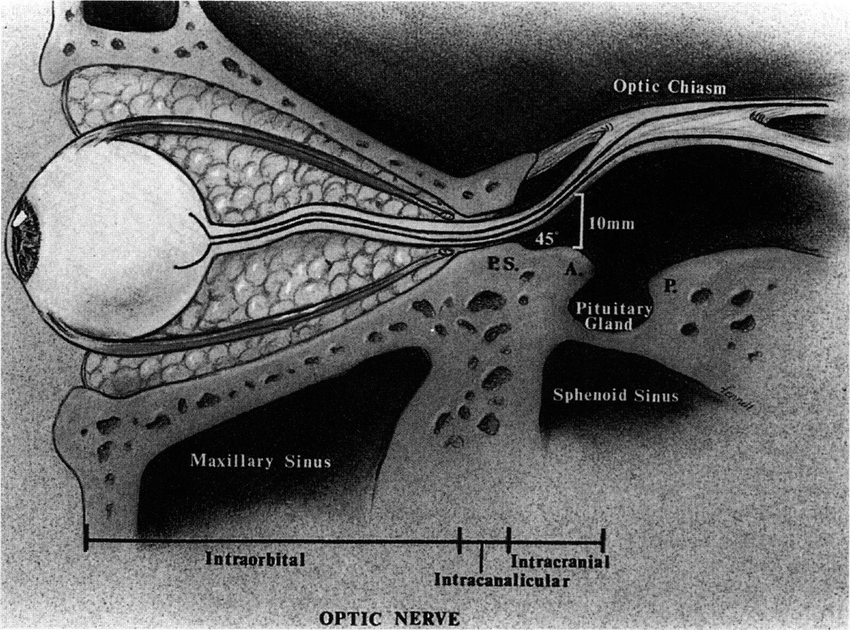
length and 4 sections of ON
50-60 meters long
intraocular, intraorbital, intracanalicular, intracranial
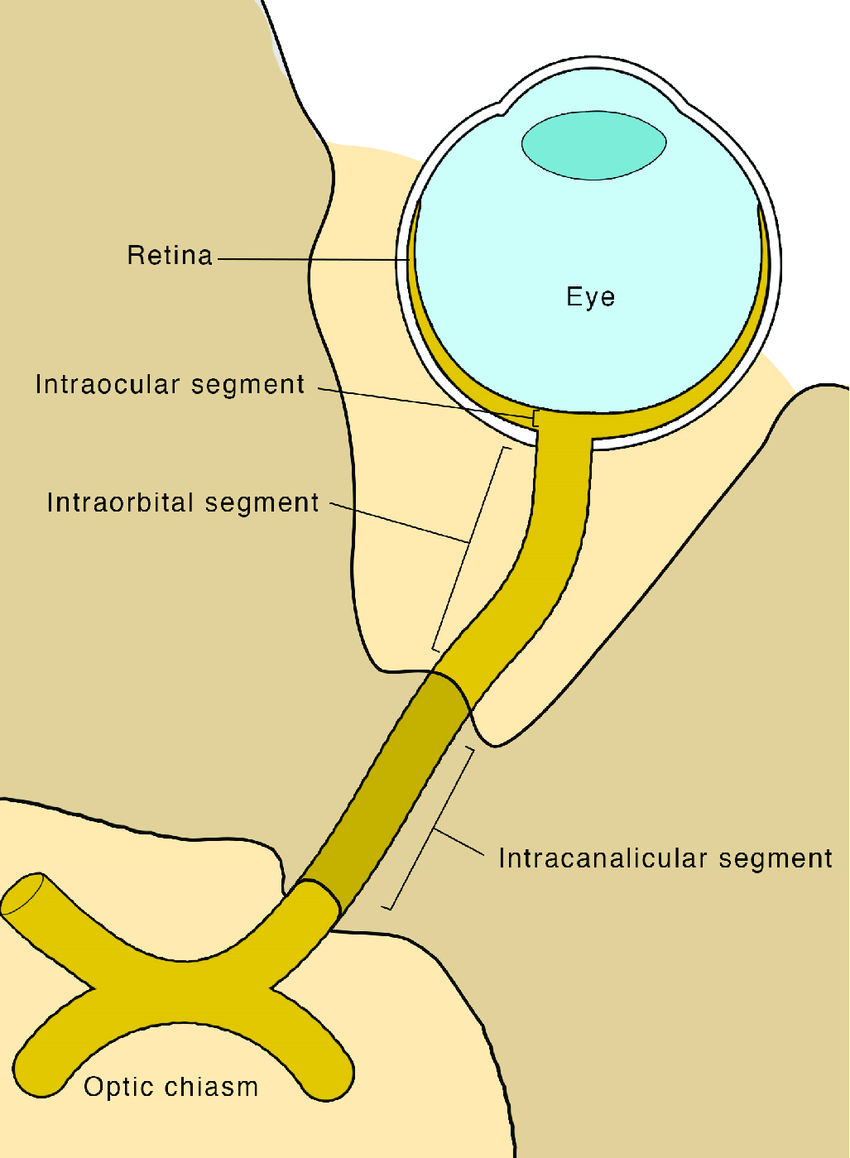
length and borders of intraocular ON
1 mm long
from the optic disc to the lamina cribrosa, made of the prelaminar ON and the laminar ON
composition of prelaminar ON
axons bundled in sheaths of astrocytes for structural support
the prelaminar ON (has/does not have) myelin
does not have
intermediary tissue of kuhnt
ring of glial tissue that separates ON fibers from the surrounding retinal tissue in the prelaminar ON
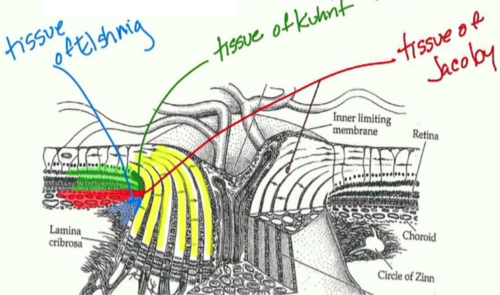
border tissue of jacoby
posterior continuation of glial tissue that makes up the tissue of kuhnt
separates ON fibers from choroid
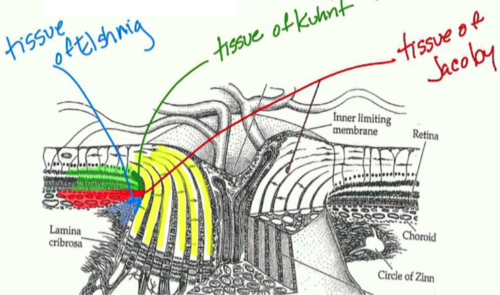
border tissue of elschnig
scleral collagen fibers that surround the glial fibers of the tissue of jacoby
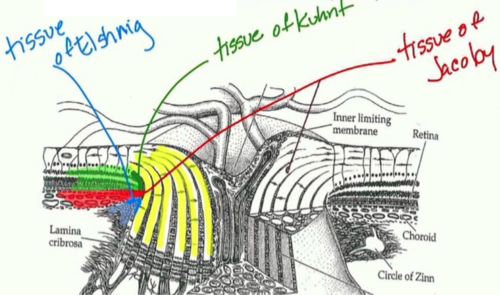
summarize border tissues of Kuhnt, Jacoby, and Elschnig
kuhnt: glial tissue separates ON from retina
jacoby: more posterior glial tissue separates ON from choroid
elschnig: scleral tissue that surrounds glial tissue of jacoby
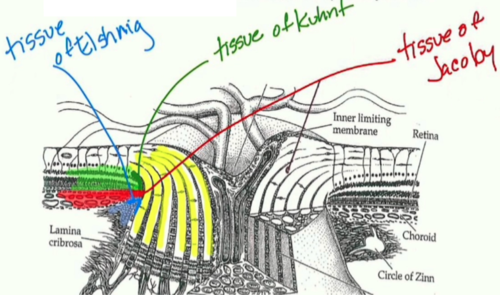
role of tight junctions within the glial tissue of the prelaminar ON
protects ON fibers from fluid leaking from fenestrated choroidal vessels
section of the ON that exits the globe
lamina cribrosa
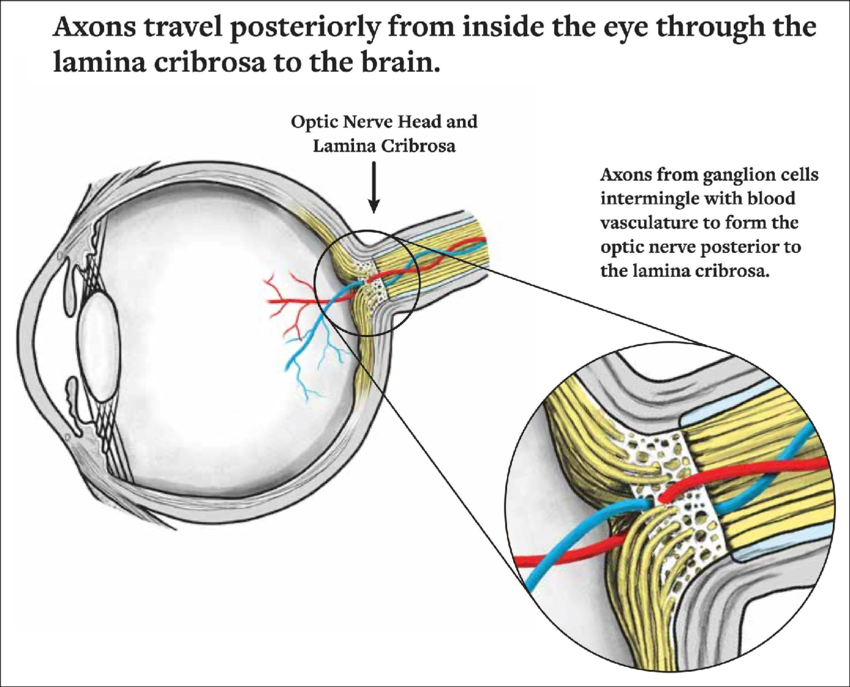
what does the lamina cribrosa consist of
network of collagen and elastic fibers that bridge across the posterior scleral foramen and support the ON
length and borders of intraorbital ON
posterior to the lamina until it exits the orbit via the optic canal
30 mm (longest portion)
what aspects of the ON anatomy allow for eye movements to happen without damaging the ON
the intraorbital ON is long and S-shaped
its axons are separated by CT septae that protect them from damage
role of CT septae in the intraorbital ON
allow the eye to move without damaging the ON
protect the ON axons
where does the intraorbital ON exit the orbit
optic canal of the lesser wing of the sphenoid
when do ON axons become myelinated, and what cells are they myelinated by
become myelinated posterior to the lamina cribrosa (in the intraorbital portion of the ON)
myelinated by oligodendrocytes
what surrounds the ON axons in the intraocular portion of the ON
CT septae, myelin, meninges that cover the rest of the brain
borders of intracanalicular ON
6-10 mm
part of ON running through the optic canal
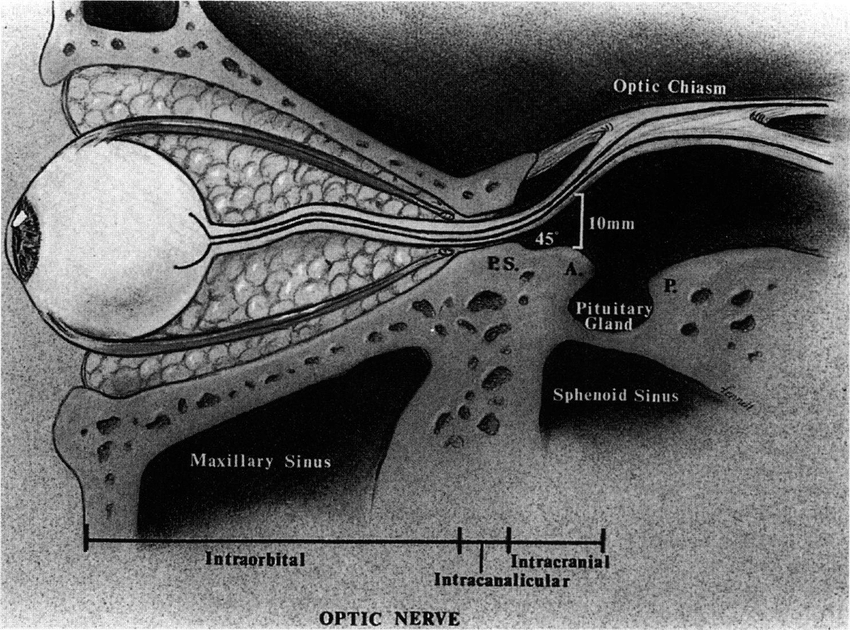
borders of the intracranial ON
10-16 mm
part of ON from optic canal to optic chiasm
what 2 things start at the lamina cribrosa
meninges & myelination
M&M
where is the CSF made
ventricles
what within the ventricles makes CSF
choroid plexus
where is the optic canal located
lesser wing of the sphenoid
the ON exits the orbit through which bone
lesser wing of the sphenoid
what nerve provides blood supply to the optic disc
SPCA
what is the longest section of the ON
intraorbital section (30 mm)
where do most optic nerve fibers go
90% go to synapse in the LGN and travel to the primary visual cortex (V1)
damage to what 2 things can cause a central scotoma
macula
papillomacular bundle via ON disease
path of papillomacular bundle fibers
go from the macula to the temporal optic disc
path of nasal ON fibers
go from RGCs nasal to the ON into the nasal ON
path of arcuate fibers
go from RGCs temporal to the fovea, arc over the papillomacular bundle, and insert into the inferior and superior ON
thickest to thinnest ON sections
ISNT
inferior, superior, nasal, temporal
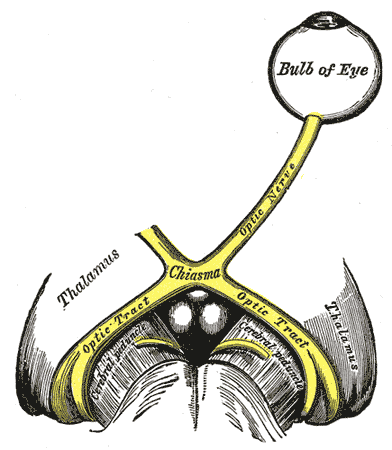
which fibers cross at the optic chiasm
superior and inferior nasal fibers that carry info from the temporal visual field
3 different paths nasal fibers can take when crossing the chiasm
anterior knees of wilbrand
posterior knees of wilbrand
optic chiasm
path of anterior knees of wilbrand
inferior nasal fibers cross at chiasm and loop anteriorly to the contralateral ON before entering the optic tract
the inferior fibers cross and then loop forward towards the opposite ON and then exit
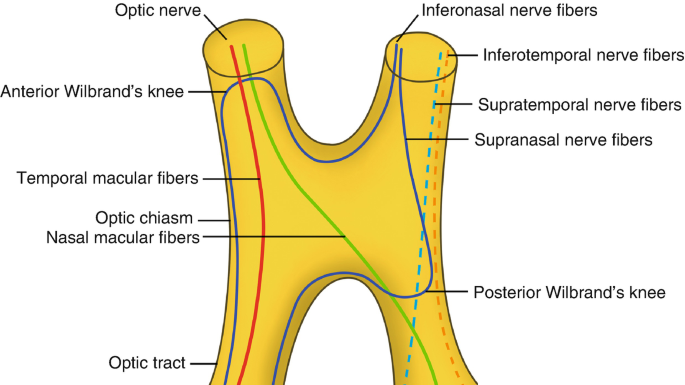
path of posterior knees of wilbrand
superior nasal fibers loop posteriorly into the ipsilateral ON before crossing the optic chiasm
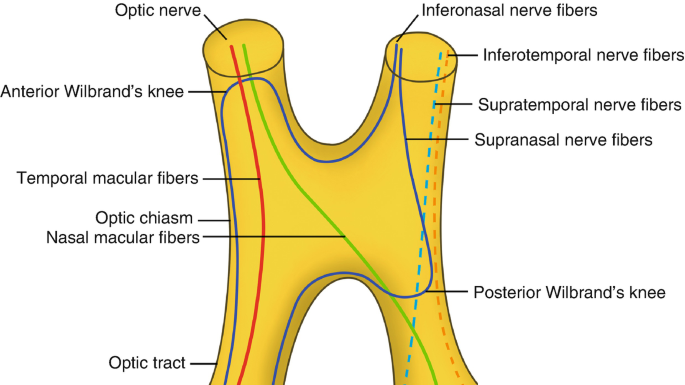
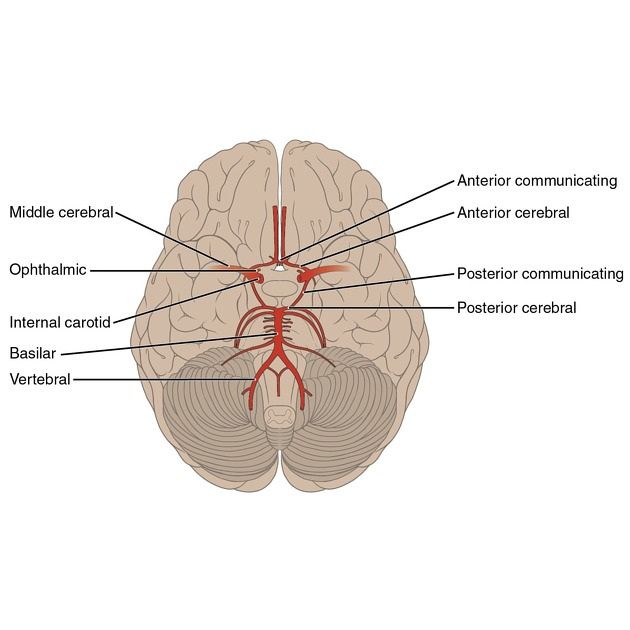
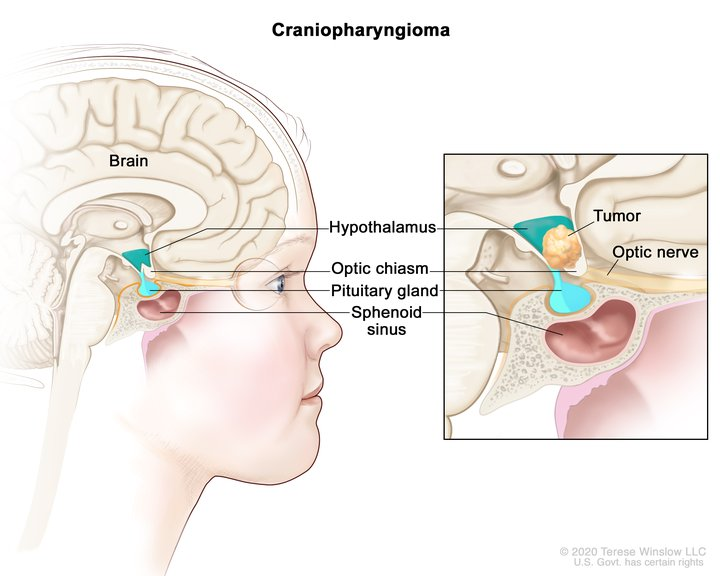
what is the optic chiasm located within
circle of willis
which fibers go into the anterior vs posterior knees of wilbrand and how does this affect fiber orientation in optic tract
inferior nasal fibers go to the anterior knees of wilbrand
superior nasal fibers go to the posterior knees of wilbrand
allows the inferior fibers to loop up and out to the temporal wall of the optic tract, while the superior fibers go down and in to the medial wall of the optic tract
in the optic tract, all superior fibers (contra temporal and ipsi nasal) are on the medial side, and all inferior fibers are on the temporal side
what is located inferior to the optic chiasm
pituitary gland
which arteries travel along the lateral edges of the optic chiasm
ICA and posterior communicating arteries
borders and contents of the optic tract
from the optic chiasm to the LGN
has crossed and uncrossed fibers from each eye (makes it so each eye sees its nasal field and the other eyes temporal field, translating to half a person’s visual field of either the right or left side in each eye)
the optic tract travels along the lateral surface of the:
cerebral peduncles
the optic tract is parallel to what artery
posterior cerebral artery
in the right optic tract, where are the superior, inferior, and macular fibers
superior fibers: nasal and temporal are on the medial side
superior nasal fibers of the left eye and superior temporal fibers of the right eye
inferior fibers: nasal and temporal are on the lateral side
inferior nasal fibers of the left eye and inferior temporal fibers of the right eye
macular fibers: middle of the tract
where do fibers within the optic tract synapse
lateral geniculate nucleus of the thalamus
layers of LGN
magnocellular layers: layers 1 & 2
parvocellular layers: layers 3-6
koniocellular layers: between the layers
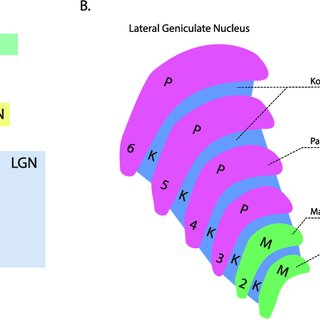
types of cells in each LGN layer
magno: large magno cells (1 & 2)
parvo: medium parvo cells (3-6)
konio: small cells
do the LGN layers go bottom up or top down
bottom up (layers 1 & 2 are located below layers 3-6)
which layers of the LGN do crossed and uncrossed fibers synapse in
U235
layers 2, 3, and 5 are uncrossed
layers 1, 4, and 6 are crossed
how are the optic tract fibers organized when they synapse in the LGN
maintain the same topography as the optic tract
remember: Lower are Lateral
superior fibers synapse in the medial LGN
inferior (lower) fibers synapse in the lateral LGN
macular fibers form a wedge of synapses at the dorsal LGN
where is the location of the first synapse within the post-ON visual pathway
LGN
how does the LGN fine-tune vision
gets fibers from subcortical areas and V1 that help fine-tune vision before it is again relayed to V1
optic radiations
fibers that leave the LGN and travel to the primary visual cortex (V1)
path of inferior optic radiations
inferior lateral fibers of the LGN travel through the temporal lobe
form Meyer’s loop by looping around the lateral ventricle into the parietal lobe
terminate in V1 in the occipital lobe
Lower (inferior) fibers travel Laterally in the optic tract and form meyer’s Loop before ending in the Lingual gyrus
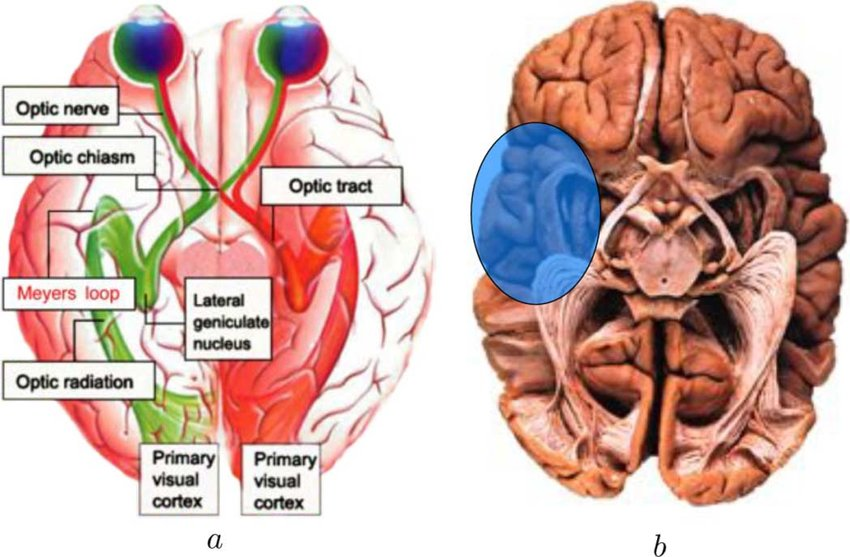
order of lobes of the brain that inferior optic radiations travel through
temporal lobe (LGN) > parietal lobe (Meyer’s loop) > occipital lobe (V1)
Meyer’s loop
loop formed by inferior optic radiations as they course around the lateral ventricle of the temporal lobe into the parietal lobe

path of superior optic radiations
superior medial fibers of the optic tract course posterior through the parietal lobe
terminate in the posterior portion of the occipital lobe of V1
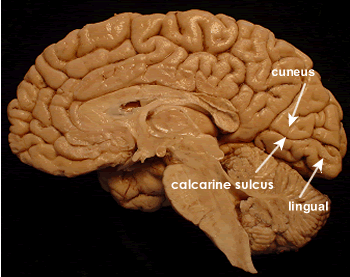
location of primary visual cortex (V1, Brodmann’s area 17, striate cortex)
medial surface of the occipital lobe (in the middle of the back of the brain)
calcarine fissure
divides the back of the occipital lobe/visual cortex into superior and inferior regions
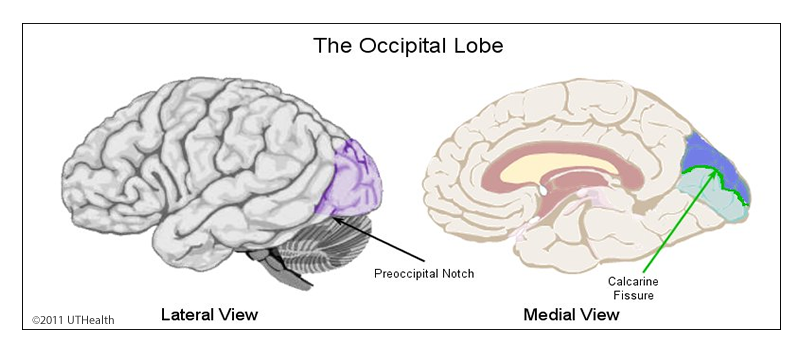
cuneus gyrus
superior part of V1 in the calcarine fissure division
superior retinal fibers terminate here
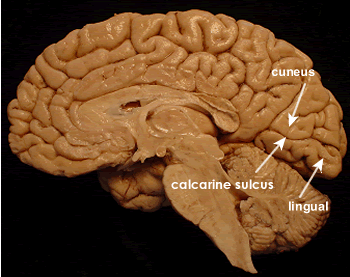
lingual gyrus
inferior part of V1 of the calcarine fissure division
inferior retinal fibers terminate here
Lower fibers travel Laterally, do a meyer’s Loop, and terminate in the Lingual gyrus
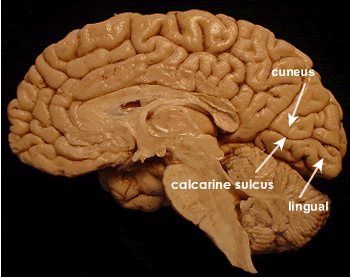
what gyri do the inferior and superior retinal fibers terminate in
superior: cuneus gyrus
inferior: lingual gyrus
what makes up 50% of V1 fibers
macular fibers
where do macular fibers project to and terminate in
project to outer surface of the apex of the occipital lobe
superior macular fibers terminate in the cuneus gyrus
inferior macular fibers terminate in the lingual gyrus
fibers of V1 are (myelinated/unmyelinated)
myelinated
fibers from what 3 places project to the primary visual cortex
LGN, superior colliculus, frontal eye fields
how is the primary visual cortex organized
6 horizontal layers and multiple vertical columns of neurons
in what V1 layer do the optic radiations synapse with the LGN cortex
layer 4
once optic radiations synapse in layer 4 of the LGN, where do they go
project to higher cortical areas of the visual cortex, V2-V5, for further processing of information
where does layer 5 send axons
the superior colliculus for control of saccadic EMs
what does layer 6 do in the visual cortex
sends feedback info to the LGN
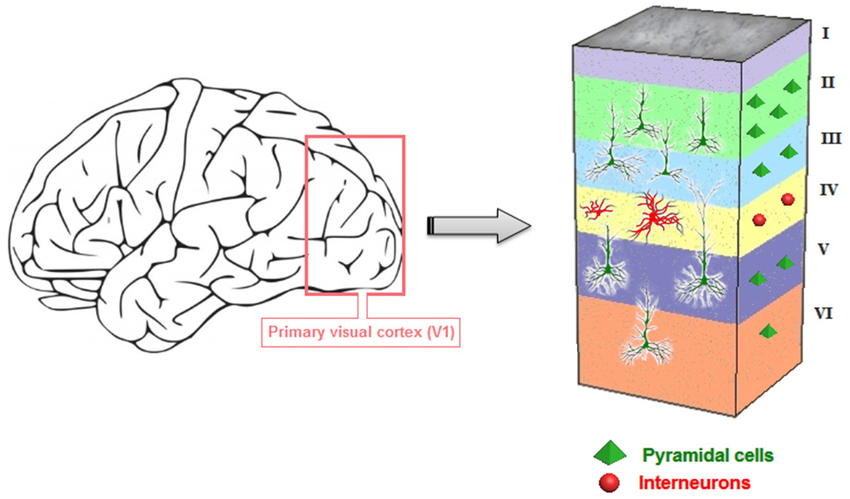
what are vertical columns in V1 called
ocular dominance columns
how are ocular dominance columns organized
each column contains fibers from only 1 eye
the columns are further organized by stimulus orientation (only respond to stimulus in front of a particular eye that is oriented in a particular way)
where does binocular visual processing begin
primary visual cortex
blood supply of the optic chiasm
circle of willis and ICA
blood supply of the optic tracts
anterior choroidal and middle cerebral artery