Vesiculoerosive & Ulcerative lesions
1/144
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
145 Terms

What is a traumatic ulcer?
Non-specific ulcer (acute or chronic trauma) that can cause surface ulcerations

Where are the most common injuries for a traumatic/nonspecific ulcer?
Lips
Tongue
Buccal mucosa

What does a traumatic ulcer look like?
A rolled white border of hyperkeratosis can develop immediately adjacent to the ulceration

What is the management of a traumatic ulcer?
Incisional biopsy if > 2 weeks
Determine cause of trauma
Remove sharp edges, construct a night guard, follow up

What is the healing like for a traumatic ulcer compared to TUGSE?
Quicker for traumatic ulcer

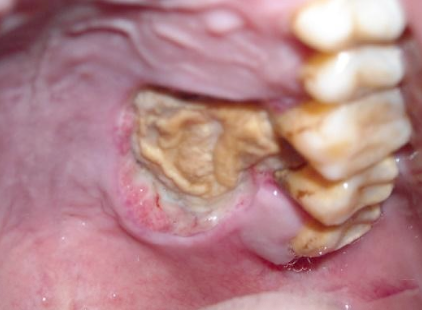
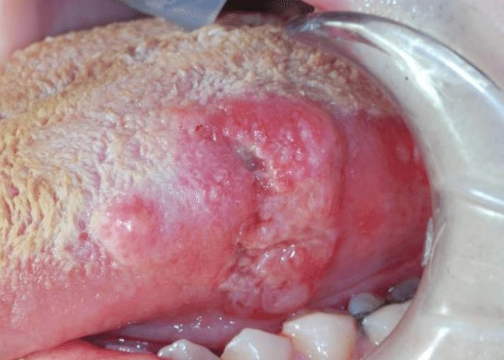
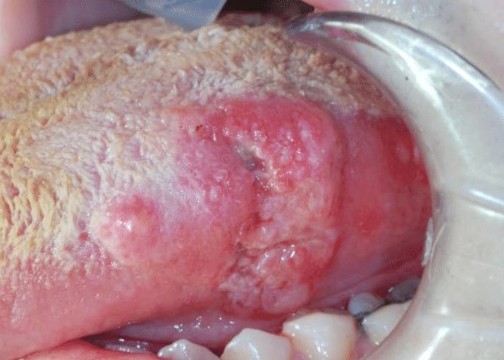
What is Traumatic Ulcerative Granuloma with Stromal Eosinophilia (TUGSE)
Deep chronic ulceration with eosinophils due to damaged muscle; due to trauma

Where would you find Traumatic Ulcerative Granuloma with Stromal Eosinophilia (TUGSE)
Can occur anywhere but tongue most common location
What is the management of Traumatic Ulcerative Granuloma with Stromal Eosinophilia (TUGSE)?
It is very slow to resolve—> up to a month
Biopsy for any ulcer that is >2 weeks
Intralesional steroid injection
Surgical removal

What does Traumatic Ulcerative Granuloma with Stromal Eosinophilia (TUGSE) look similar to?
Squamous Cell Carcinoma

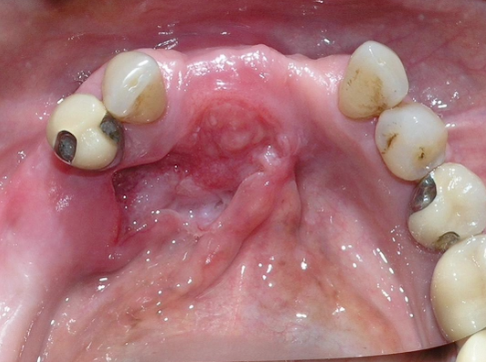
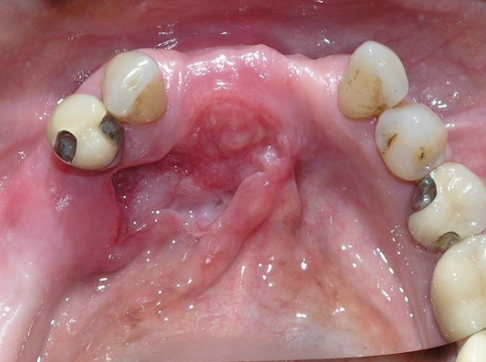
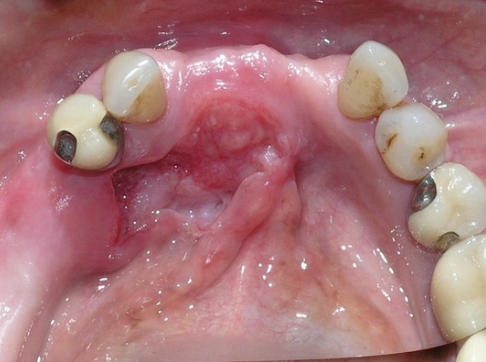
What is Necrotizing Sialometaplasia?
An uncommon, locally destructive inflammatory condition of the salivary glands

What is Necrotizing Sialometaplasia caused by?
Ischemia that leads to infarction of salivary glands
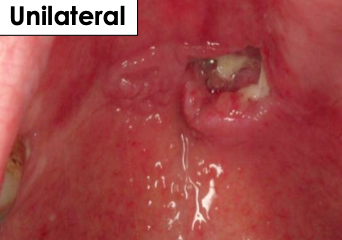
Where would find Necrotizing Sialometaplasia?
Hard palate
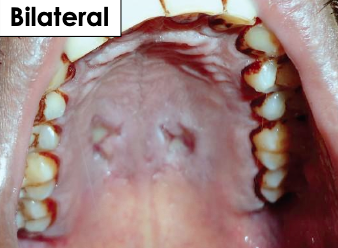
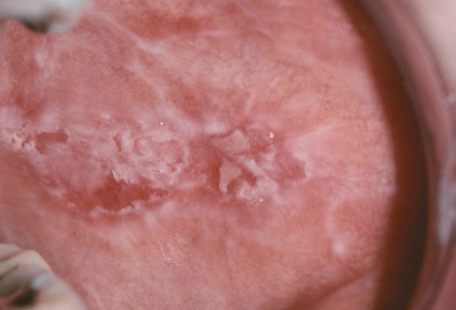
What is the clinical manifestation of Necrotizing Sialometaplasia?
Begins as a painful, non-ulcerated swelling
In 2-3 weeks, leaves a non-painful ulcer (mimics malignancy)

What is the management of Necrotizing Sialometaplasia?
Incisional biopsy —> no tx necessary once diagnosis is established

How long does Necrotizing Sialometaplasia take to resolve?
Lesion resolves within 6-10 weeks
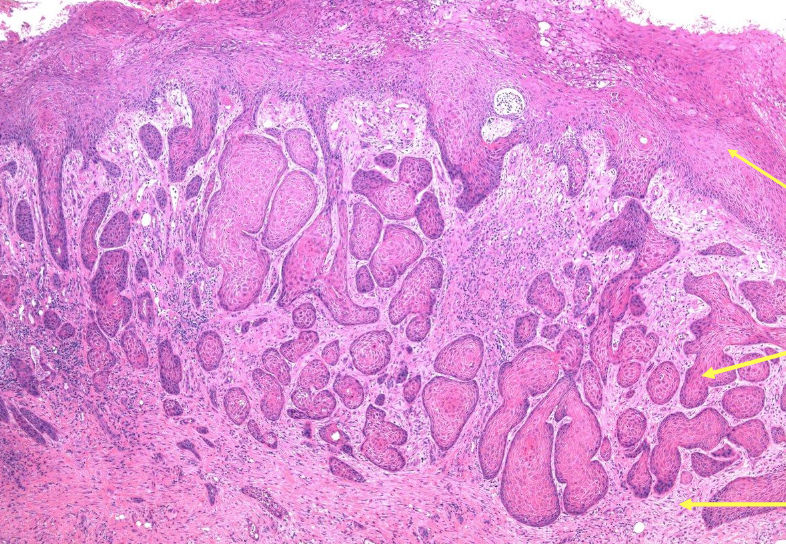
In which two conditions do you see Pseudoepithelial Hyperplasia (PEH)?
Granular cell tumor (myoblastoma)
Necrotizing Sialometaplasia

What is anesthetic necrosis?
Uncommon, locally destructive inflammatory condition of the salivary glands; necrosis of tissue due to ischemia

WHere would you find anesthetic necrosis?
More common in palate; similar to Necrotizing Sialometaplasia
What is the management of anesthetic necrosis?
Heal on its own
Antibiotics
NSAIDs
Surgical debridement
Wound care
Grafting

What is the cause of an aphthous ulcer?
Cause unknown, maybe due to stress, hormones, ALWAYS on movable mucosa, young age, pain, recurs

What is the size and healing time of a minor aphthous ulcer (stomatitis)?
3-10 mm (small), 7-14 days with no scarring, 1-5 lesions, less recurrences

What is the size and healing time of a major aphthous ulcer (stomatitis)?
1-3cm (large), 2-6 weeks with biopsy to rule out cancer with scarring present, 1-10 lesions, and long duration

What is the size and healing time of herpetiform (least common) aphthous ulcer (stomatitis)?
1-3mm (small), 7-10 days with no scarring, up to 100 lesions present with most recurrences

What is the management for aphthous ulcer (stomatitis)?
OTC topical anesthetic
Topical steroid
Avoid spicy food
What is the most common type of oral cancer that can have various clinical patterns?
Squamous Cell Carcinoma (SCC)
What are some high risk sites of Squamous Cell Carcinoma (SCC)?
Floor of mouth
Lateral ventral tongue
Lower lip
Soft palate
How does early-stage SCC usually feel?
Often non-painful (check with TNM staging)
What neurologic sign can appear in later-stage SCC?
Numb chin syndrome

What oral finding should raise concern for SCC?
A persistent, non-healing ulcer
When should a suspicious oral ulcer be biopsied (SCC)?
If it lasts more than 2 weeks
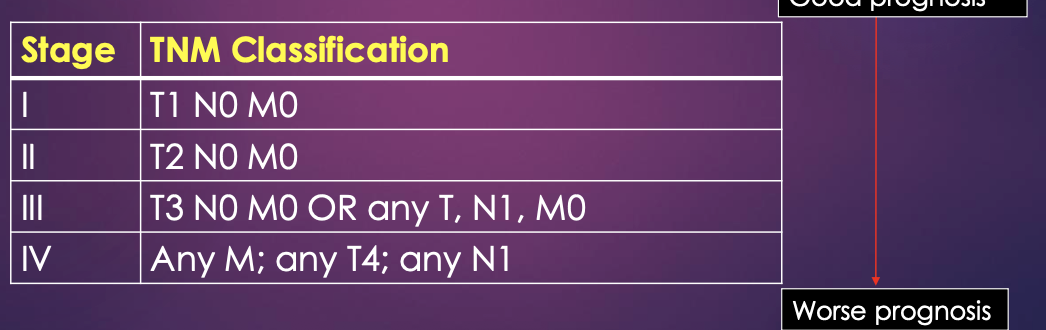
What does TNM staging indicate?
Dictates treatment and best indicator of patient prognosis.
T = size of primary local tumor in cm
N = Involvement of local lymph nodes
M = Distant metastasis

What is the first-line medication for Squamous Cell Carcinoma?
Methotrexate —> immunosuppressive medication that treats cancer and autoimmune conditions such as rheumatoid arthritis

What is the management of Methotrexate?
Over 2 weeks might need incisional biopsy
Change dose and medication
Folic acid

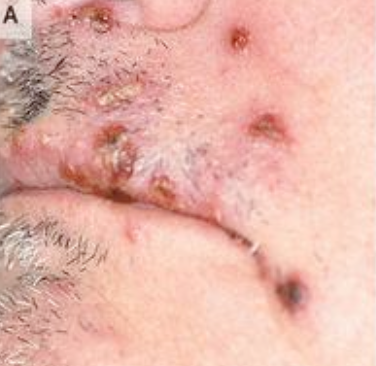
What is primary herpetic gingivostomatitis?
Herpes Simplex-1 (HSV-1/HHV-1) that affects children between the ages of 6 months and 6 years

What is the clinical presentation of primary herpetic gingivostomatitis? Intraoral?
Systemic symptoms such as fever, malaise, and cervical lymphadenopathy; Intraoral presentation is painful, erythematous and swollen gingivae and multiple tiny vesicles on the perioral skin, vermillion border of the lips and oral mucosa

What is the management of primary herpetic gingivostomatitis?
Antiviral —> subsides around 7-14 days

Where does Recurrent Herpes (HSV-1 / HHV-1) persist in the body?
In a latent state within nerve tissue

What are prodromal signs in herpes infection?
Tingling, burning, or itching that occurs a few days before the lesion appears

What is herpes labialis?
Recurrent herpes on the lips; may be single or multiple lesions

What is herpetic whitlow?
Recurrent herpes infection on the finger

Where do intra-oral recurrent herpes lesions occur?
On keratinized mucosa (attached to bone, like hard palate, attached gingiva)

How do recurrent herpes lesions typically resolve?
They are self-limited and heal spontaneously in 1–2 weeks

How is recurrent herpes diagnosed?
Clinically or with a swab

What is Varicella-Zoster Shingles (VZV/HHV3)?
Unilateral, painful eruption of vesicles along the distribution of the trigeminal nerve in older patients

What can Varicella-Zoster Shingles (VZV/HHV3) be associated with?
Immunocompromised or immunodeficiency or certain malignancies like Hodgkin disease and leukemia

Which age group does Varicella-Zoster Shingles (VZV/HHV3) commonly occur in?
Older adults
What is the management for Varicella-Zoster Shingles (VZV/HHV3)?
Antiviral
What is the management for viral lesions?
Herpetic lesions: Antiviral like acyclovir suspension or tablets
Valacyclovir —> 1mg 3x/day for 7 days
Famciclovir
Medication is effective during prodromal signs and first 72 hours of symptoms
Herpangina and HFM disease: self limiting, subsides in 7-10 days, NSAIDs
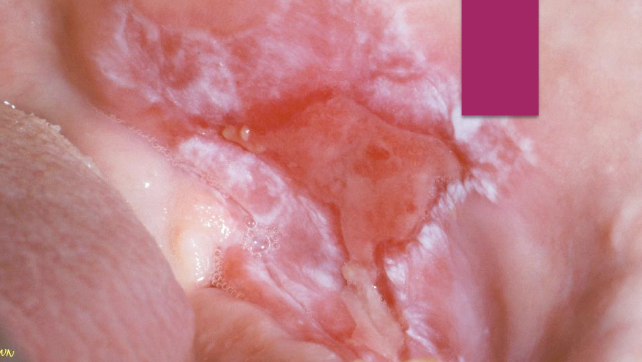
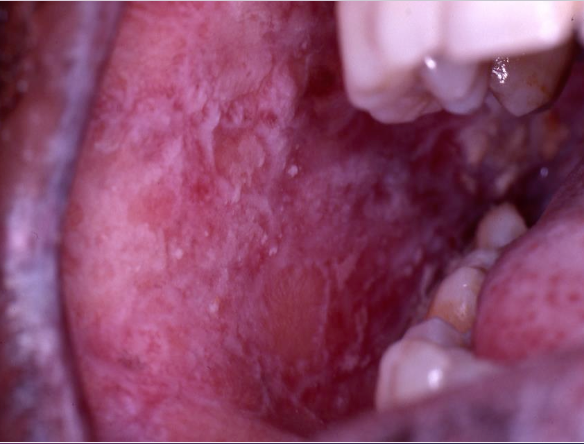
What are the hallmark symptoms of erosive lichen planus?
Pain and erythema with white striations

How do patients with erosive lichen planus often describe eating?
Painful- especially sensitive to spicy foods
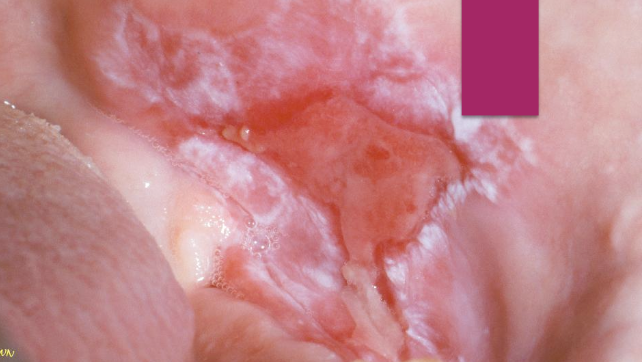
Does erosive lichen planus have a uniform presentation?
No, severity varies from mild discomfort to severe erosions

What oral sites are commonly affected by erosive lichen planus?
Buccal mucosa and gingiva, anywhere intraorally, lips, and skin
Erosive vs. Reticular Lichen Planus

What is the underlying cause of Pemphigus Vulgaris and Mucous Membrane Pemphigoid (MMP)?
Autoimmune disease (more common in older females)
Where do lesions often begin in PV and MMP?
On the mucosa- oral lesions are often the first sign (~50% of cases)

Which condition more commonly involves the eyes?
Mucous Membrane Pemphigoid (MMP)
What skin findings are seen in PV and MMP?
Vesicles, bullae, and scarring
What clinical sign is positive in both PV and MMP?
Nikolsky sign
What is the gold standard for diagnosis of PV and MMP?
Biopsy for H&E + Direct Immunofluorescence (DIF)
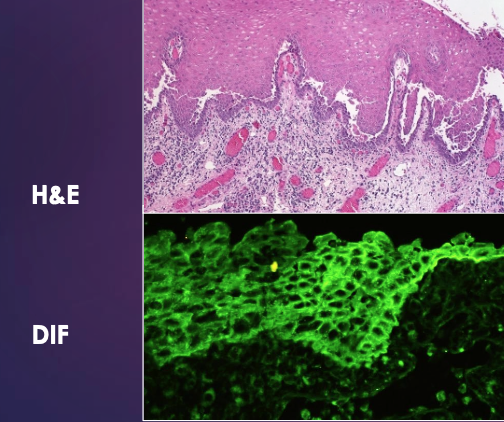
What type of epithelial separation is seen in Pemphigus Vulgaris?
Intra-epithelial separation - chicken wire epithelium
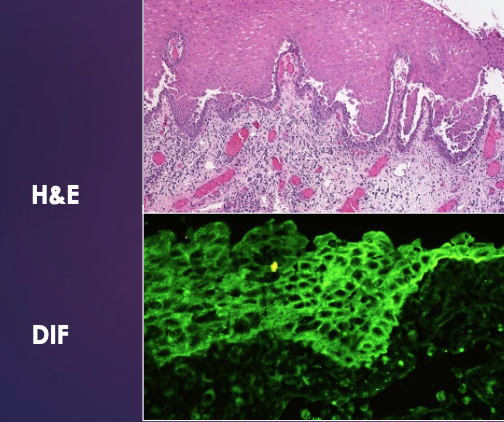
What is acantholysis?
Loss of cohesion between epithelial cells
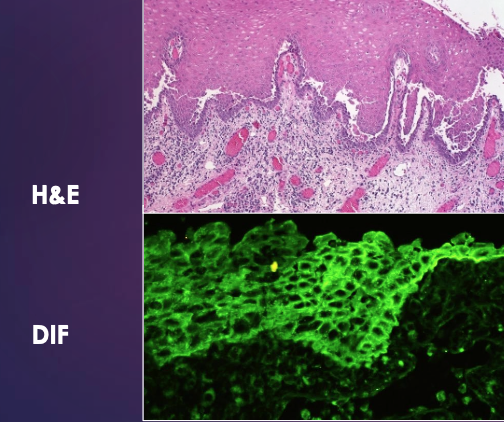
What are Tzanck cells?
Detached epithelial cells seen in Pemphigus Vulgaris
What type of epithelial separation is seen in MMP?
Sub-epithelial separation
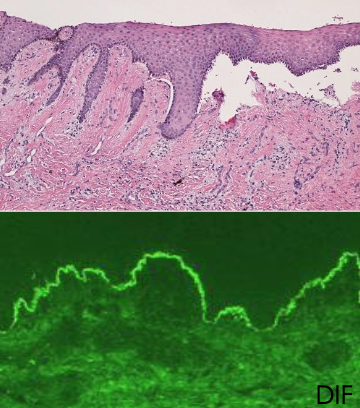
What does DIF show in MMP?
Linear fluorescence along the basement membrane
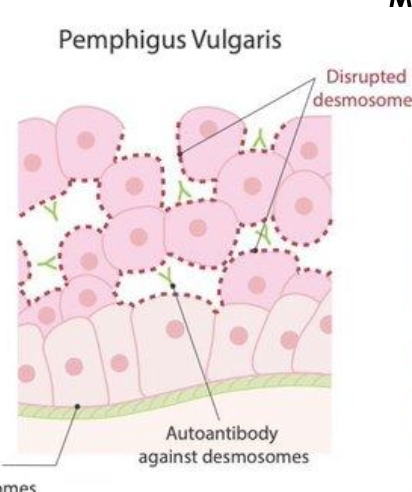
What structure is targeted in pemphigus?
Desmosomes (cell-to-cell attachments within epithelium)
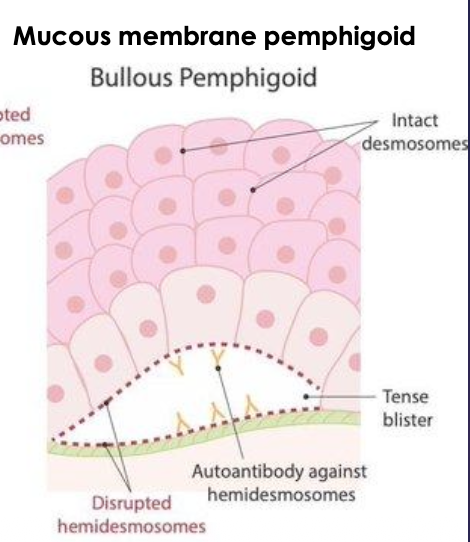
What structure is targeted in pemphigoid?
Hemidesmosomes (epithelium-to-basement membrane attachments)

What type of disease is Pemphigus Vulgaris?
An autoimmune blistering disorder
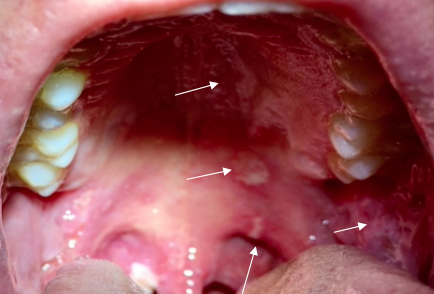
What oral findings are common in Pemphigus Vulgaris?
Painful erosions and ulcers of the oral mucosa (often widespread)

How is gingival involvement in PV compared to LP and MMP?
Gingiva is less affected than in lichen planus (LP) and mucous membrane pemphigoid (MMP)

What is a key FDA-approved treatment for Pemphigus Vulgaris?
Rituximab (immunotherapy)
Why is Rituximab used in PV?
It targets the autoimmune process driving blister formation

What is Symblepharon?
An eye condition where the eyelid becomes abnormally attached to the eyeball due to scarring —> seen in MMP

What does MMP mainly affect?
Gingiva
What are the different types of management of autoimmune conditions?
Steroid
Topical
Systemic
Antifungal
Lozenges
Mouth rinse
Systemic
What is the first-line therapy for many immune-mediated oral lesions?
Topical corticosteroids
Name common topical steroid options for oral lesions.
Diprolene gel
Decadron (dexamethasone) elixir
Lidex (fluocinonide) gel
Temovate (clobetasol) gen
What is a key side effect of dexamethasone elixir?
Burning (especially if it contains alcohol)
What alternative avoids alcohol-related burning?
Dexamethasone oral solution (without alcohol) at the same dose
When are systemic steroids used?
For severe or widespread disease (like prednisone taper)
Why are antifungals often needed with steroid therapy?
Steroids can predispose to oral candidiasis
First-line antifungal mouth rinses for candidiasis?
Nystatin oral suspension (swish & swallow or expectorate)
Itraconazole oral solution
What are common antifungal lozenges/tablets to treat candidiasis?
Clotrimazole troches (dissolve in mouth 5×/day)
Fluconazole tablets (systemic)
What topical treatment can be used for angular cheilitis presentations?
Dermazene (iodoquinol and hydrocortisone cream)
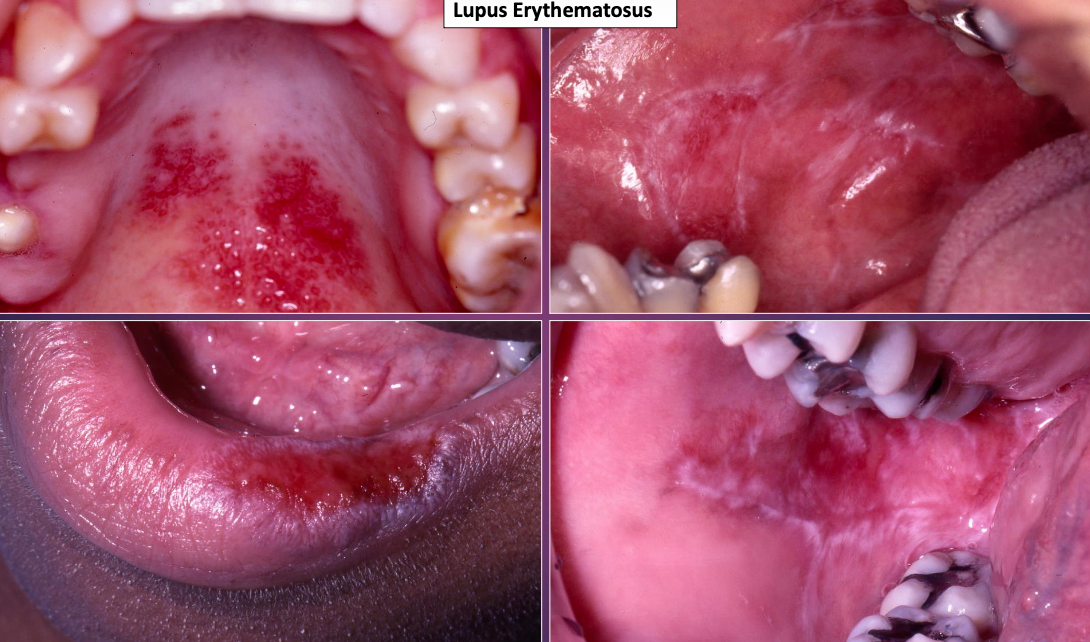
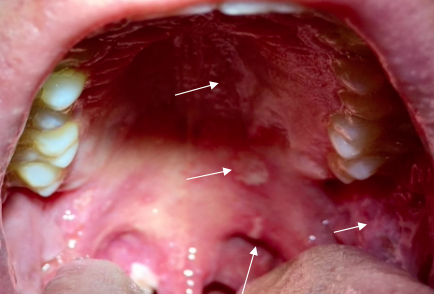
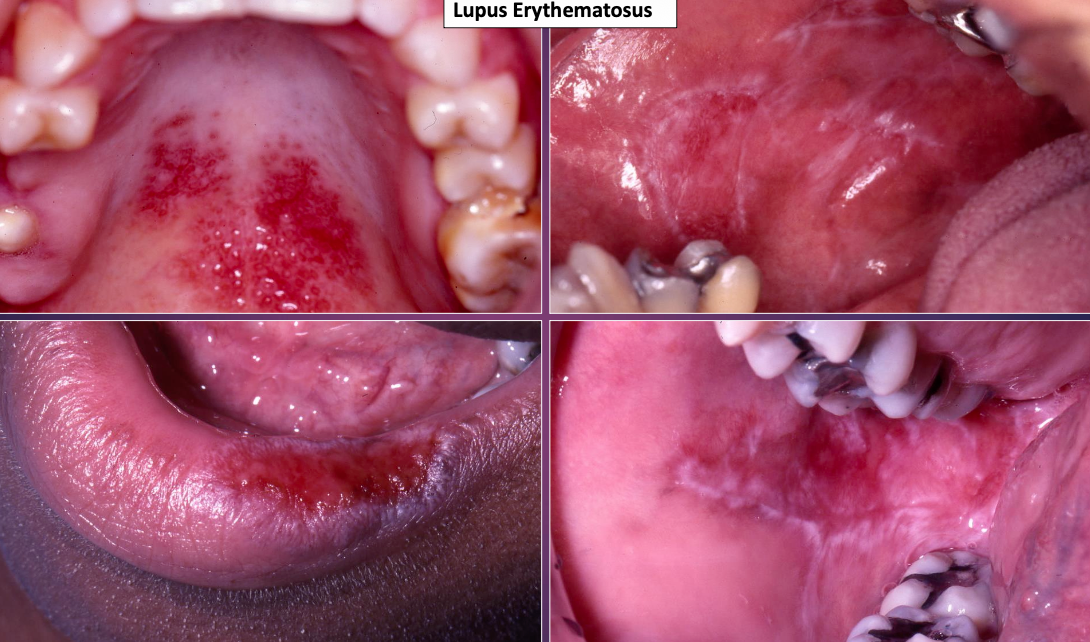
What is Systemic Lupus Erythematosus?
An acute and chronic inflammatory autoimmune disease of unknown cause
In which gender does Systemic Lupus Erythematosus primarily show up in? What age?
Female » Male (8:1); childbearing age (avg. 31)
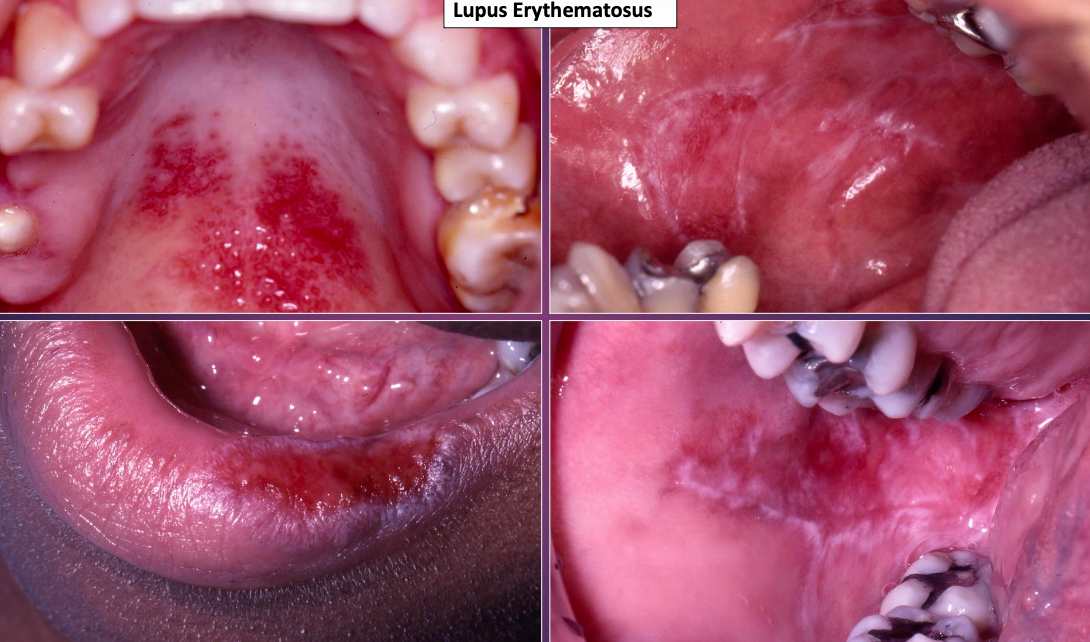
Where would you mostly see Systemic Lupus Erythematosus?
Skin, kidney, heart, lungs; intra-orally (5-25%): may appear lichenoid or non-specific

What is a common feature of Systemic Lupus Erythematosus?
50% have a butterfly rash over malar area of nose sparing the nasolabial fold
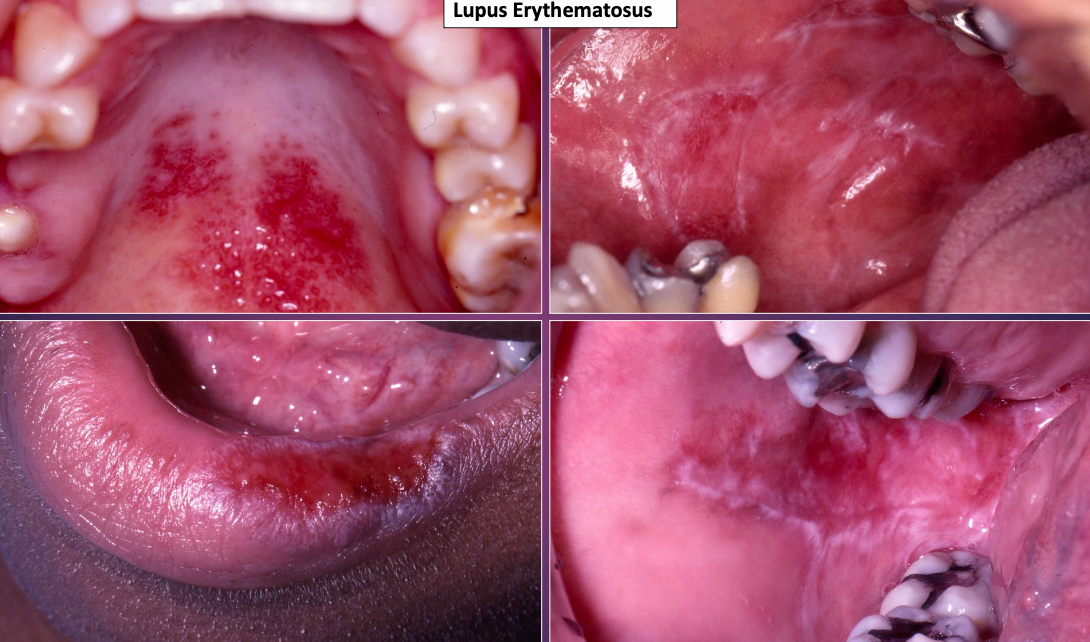
How would you treat Systemic Lupus Erythematosus?
Follow up
NSAIDs
Anti-malaria drug therapy (hydroxychloroquine)
Systemic steroids (prednisone)
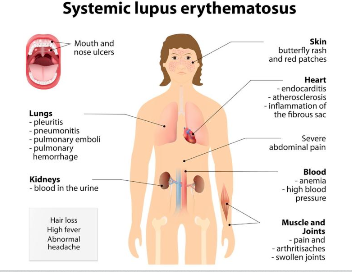
What are some common conditions faced with Systemic Lupus Erythematosus?
Weight loss
Fever
Arthritis
Fatigue/malaise
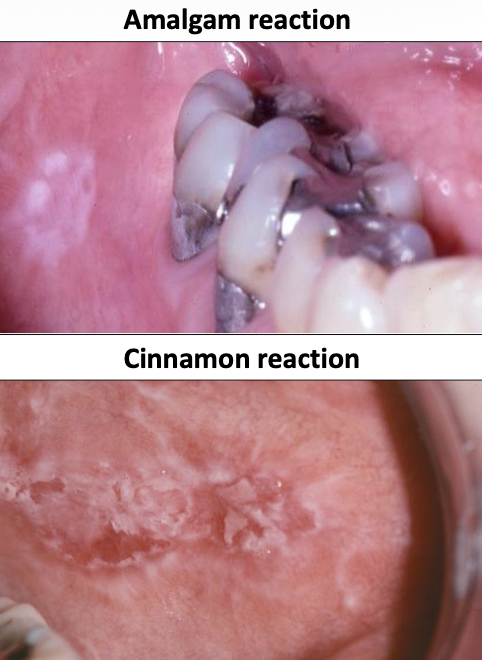
What is Lichenoid Mucositis?
An allergic (hypersensitivity) reaction of the oral mucosa that mimics oral lichen planus
What conditions can mimic oral lichen planus?
Lichenoid drug reaction
Graft-versus-host disease (GVHD)
Contact mucositis (amalgam, cinnamon)

What is a lichenoid amalgam reaction?
A localized lichenoid lesion adjacent to an amalgam restoration

What is an oral mucosal cinnamon reaction?
A contact hypersensitivity reaction to cinnamon-containing products
How is lichenoid mucositis managed?
Discontinue the offending agent —> lesions resolve within a few weeks
What is contact mucositis?
A hypersensitivity reaction from prolonged or frequent contact with an agent
Candy —> localized
Chewing gum —> localized
Toothpaste —> diffuse
Medication
Graft v Host Disease
Lichenoid mucositis


What is Erythema Multiforme (EM)?
A blistering ulcerative mucocutaneous condition that has a spectrum of hypersensitivity reaction

What is the cause of Erythema Multiforme (EM)?
Herpes virus (HSV)
Mycoplasma pneumoniae
Medications

What is the main demographic that you see Erythema Multiforme in?
Young M > F

How long has Erythema Multiforme last?
2-6 weeks (self-limiting); 20% have recurrent episodes