Infectious Disease (Module 7)
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
* prions
* viruses
* bacteria
* protozoa
* fungi
* macro-parasites.
* can convert normal proteins into abnormal ones and multiply through physical contact.
* Creutzfeldt-Jakob Disease (CJD)
* Kuru
* cannot replicate or survive on its own and must use a host cell.
* Influenza
* COVID-19.
* Tuberculosis (TB).
* Giardia
* Tinea
* Roundworms
**Hypothesis**: distilled water will not contain microbes, however the tap and pond water will
\
**Method**:
1. Collect water from different water sources (tap, distilled, pond)
2. Sterilise inoculating loops by placing them into the blue flame of bunsens burner (around 15 seconds)
3. Allow to cool
4. Place loop in water sample
5. Open agar plate and spread water sample in zig zag motion
6. Seal agar plate completely
7. Label
8. Place in incubator (repeat \[1-8\] for each water source)
9. Leave for around a week, observe bacterial and fungal growth, note colour, amount and size
\n **Result:** most microbial growth in the pond water, followed by tap and there was no microbial growth in distilled water
* An acute diarrheal disease which can kill within hours
* mode of transmission: faecal-oral transmission
* Goes from the faeces directly or indirectly into the mouth of a new host
* Food and water may look clean → bacteria is microscopic
* caused by bacteria
* prevention: wash hands, not shaking hands, wash chopping boards and utensils, eating food hot → heat kills cholera,
* control: isolation/quarantine of infected people
* direct
Infectious agents are transmitted to new hosts through intermediates such as air, food, water and substances in the environment or other animals
* droplet transmission
* dried secretions suspended in the air
* food
* poor hygiene and careless handling
* water
* Can carry diseases if not purified
* vectorborne
* organisms like mosquitoes transmitting diseases
* vehicleborne/contaminated
* non-living substances or objects contaminated by infectious agents
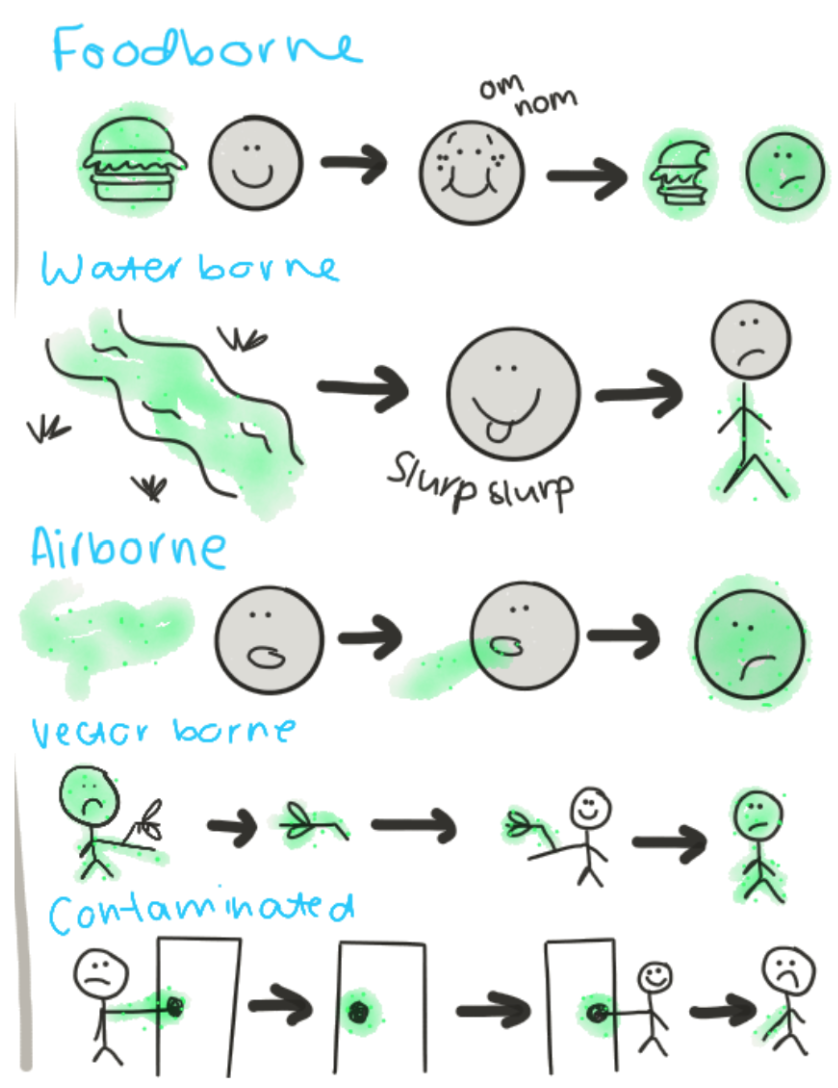
* Person to person (touching, kissing, coughing, sneezing on someone)
* Animal to person (handling, bites, scratches
* vertical
* contact between offspring and parent
* transplacental, vaginal birth, or breastfeeding

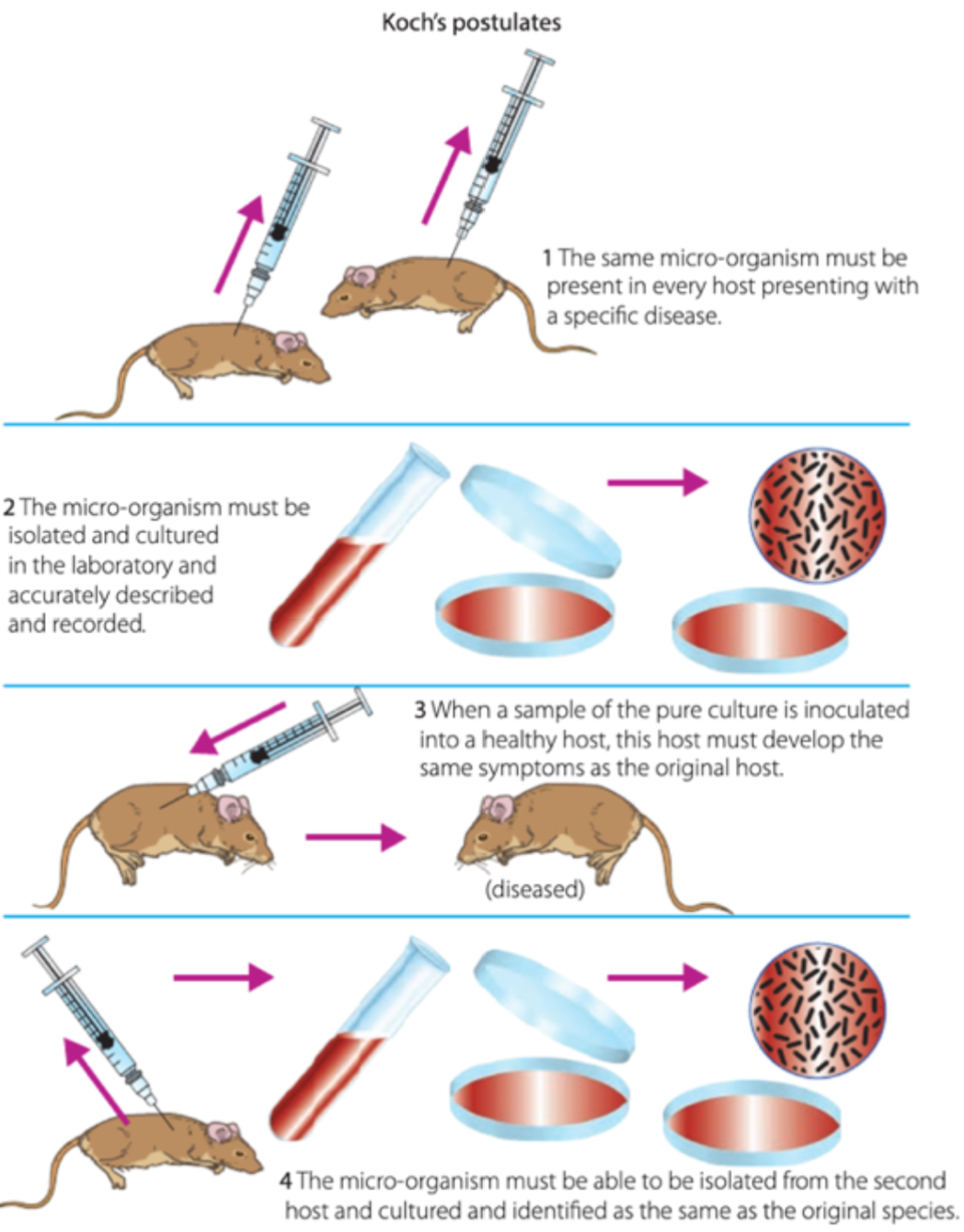
postulates include:
1) the pathogen must be associated with the disease
2) the pathogen must be isolated and grown in pure culture
3) the cultured pathogen must cause the same disease when introduced into a healthy host
4) the pathogen must be re-isolated and shown to be the same as the original pathogen.
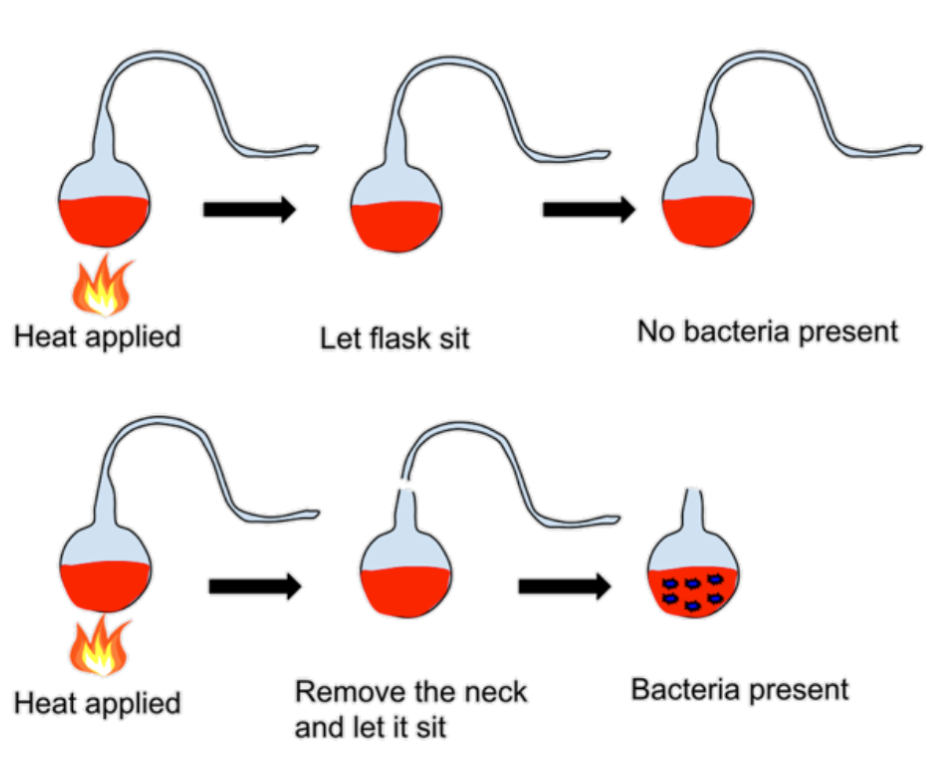
* He demonstrated that microorganisms are present in the air and that most infectious diseases are caused by microorganisms.
the experiment:
1. Take flask with bent swan necks. Particles in the air cannot travel through these necks without getting stuck. Fill with broth
2. Apply heat to both flasks, bring to boil. (this sterilises the contents of the flask)
3. Break the neck of one of the flasks
4. Observe growth of microorganisms in broth
* Flask with broken neck = microbe growth
* Flask without broken neck = no growth
\
* in plant diseases, various pathogens including bacteria, fungi, viruses, protozoa, and micro-parasites can lower the productivity of plants and impact agricultural yield.
* In animal diseases, they can cause economic losses, suffering, and death for animals, affecting food security, farmers' livelihoods, and potentially posing health risks to humans.
* caused by various pathogens, including bacteria, fungi, viruses, protozoa, and micro-parasites
* caused by a highly contagious fungus called Fusarium oxysporum.
* The disease results in yellow wilting leaves and splitting stems, damaging the conducting tissues and causing water and nutrient deprivation.
* Diseases in animals cause major production and economic loss, as well as suffering and death for the animals
* cause: Number of pathogens including bacteria, viruses, protozoa and macro-parasites
* **Food security:** animal disease may severely impact agriculture which has significant impacts upon at-risk populations facing poverty or malnutrition
* **Health risks:** Animal diseases have potential to infect humans hosts as well. May affect farmer handlers and those who chose to consume
* It is caused by a virus (aphthovirus) and infects cattle, sheep, and goats.
* The disease is highly contagious and causes rash/blisters on the hands, feet, and in or around the mouth.
* Reduces herd fertility → less efficient herd production
* Reduced milk yield → impacts farmers economically and raises prices
* **Entry points:** Pathogens can enter the host through the skin, lungs, gastrointestinal system, or genitourinary tract.
* **Adhesion:** They possess adhesins that allow them to adhere to the host's cells or tissues.
* **Invasion:** Pathogens invade the host with the help of invasins, which facilitate their entry into cells or tissues.
* **Hiding:** Pathogens can evade detection from the immune system by living inside cells or using other strategies.
* **Exit:** Once inside the host, pathogens replicate, and their offspring spread out and exit the host.
* **Transmission:** These pathogens can transmit themselves to other hosts.
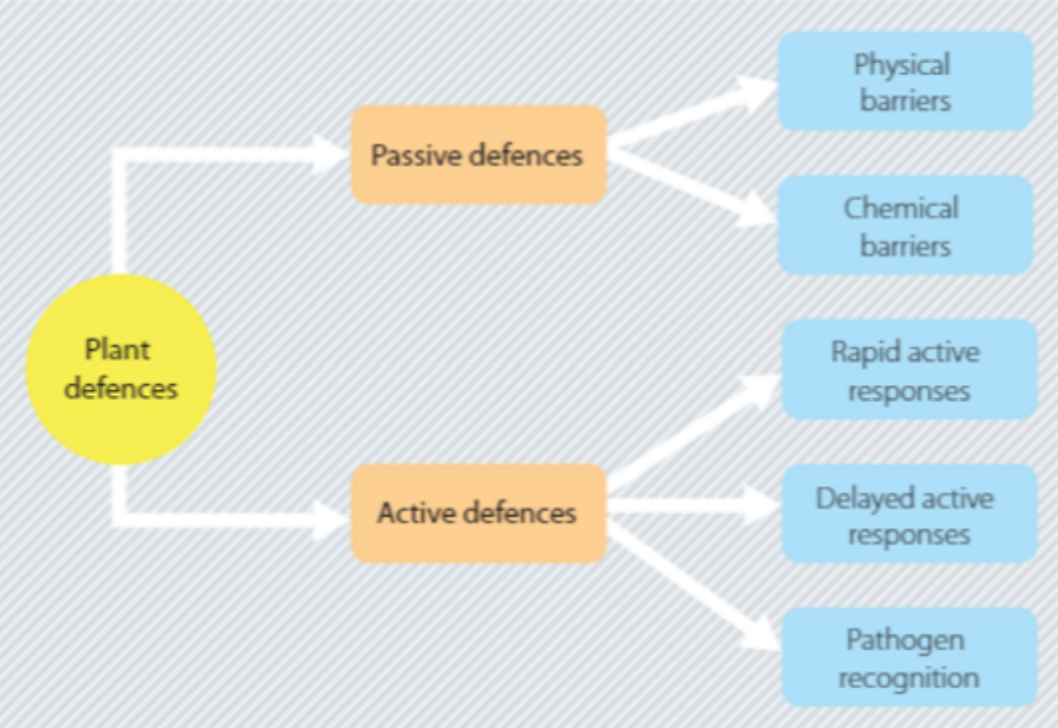
* physical barriers
* Thick cuticle or bark
* Cell wales
* Small stomata
* chemical barriers
* Compounds and enzymes that reduce fungal or viral growth
* **active defence**
* Recognition of pathogen: Plants detect physical and chemical signals.
* Rapid active response: Release of hydrogen peroxide, reinforcement of cell walls, apoptosis.
* Delayed active response: Limit the spread of the pathogen, repair damaged bark, release of lysozyme-like chemicals, "memory" of pathogen through salicylic acid.
* primarily affects leaves, stems, and flowers of the eucalyptus tree, causing deformed leaves, stunted growth, reduced fertility, and inhibiting photosynthesis.
* Cell walls become reinforced by additional structural proteins at the site of infection.
* Secretory cells and glands transport defensive substances
* Accumulation of harmful metabolites (e.g., oxygen species, salicylic acid) at the site of infection.
* Upregulation of pathogenesis-related proteins with antifungal activity.
* Skin
* Mucous membrane
* Cilia
physical changes: apoptosis and inflammation
What are some physical changes that reduce infection?
apoptosis
inflammation
* controlled process of programmed cell death that eliminates infected and/or damaged cells.
* involves specific morphological changes in infected cells, effectively removing them from tissue and limiting pathogen replication.
* biological response triggered by the presence of pathogens or tissue injury.
* causes redness, swelling, and other changes in the affected area. Inflammation helps eliminate infection by increasing blood flow, removing pathogens and toxins, and promoting the recruitment of immune cells to the site of infection.
* Acidic conditions in stomach
* Alkaline conditions in intestines
* Body secretions - urine, lysozymes, saliva
chemical changes: cytokines, interferons, chemokines
What are chemical changes that reduce infection?
cytokines
interferons
chemokines
* signaling molecules released by cells in the immune system.
* bind to specific receptors on target cells, triggering various cellular responses.
* attract immune cells to the site of infection, stimulate inflammation, and activate the adaptive immune response.
* substances produced by infected cells to help the immune system fight infection.
* when cell is infected by a virus, it produces interferons, which are released into the surrounding extracellular fluid.
* bind to receptors on neighboring uninfected cells, triggering cellular responses that stimulate an antiviral state, activate the adaptive immune response, and reduce viral load.
* small proteins produced by cells in response to infection.
* act as signaling molecules, attracting immune cells to the site of infection and enhancing phagocytosis, the process of engulfing and eliminating pathogens by immune cells.
* play a role in immune cell recruitment and the overall defense against pathogens.
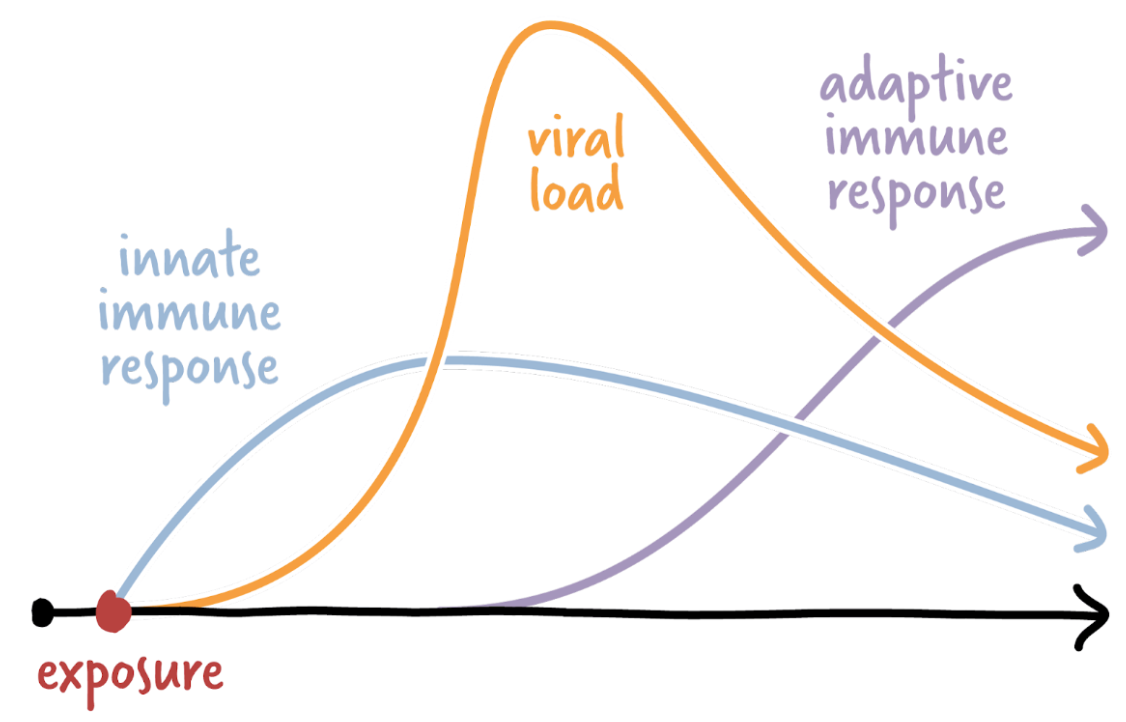
* includes physical barriers, body fluids, non-specific cellular response (e.g., phagocytosis), and non-specific biochemical processes.
* first and second line of defence
* activated when the innate immune response fails
* third line of defense.
What is the first line of defense?
body's initial defense against a pathogen attack.
aims to prevent pathogens from entering the body
includes physical and chemical barriers, as well as microbiological barriers.
NON-SPECIFIC
* Physically block pathogens
* skin
* mucous membrane → line digestive, respiratory, reproductive and urinary tracts
* cilia → hair-like structures that beat and sweep mucus out of body through nostrils
* other flushing mechanisms - urine
* Substances such as stomach acid, alkali conditions in the small intestine, and enzymes in the mouth – all act to kill pathogens
* Makes the surface inhospitable
* Pathogens entering the body in food and drink are usually destroyed by the acidity of the stomach or the alkalinity of the small intestine (bile produced by the liver is alkaline) able for potential pathogens
* recognizes antigens and produces an immune response, including inflammation, phagocytosis and the lymph system.
What is inflammation?
damaging of the body tissue causes the blood vessels around the area to be supplied with extra blood. body tissue damaged = area red, hot, swollen and painful
accumulation of fluid, plasma proteins, and white blood cells that occurs when tissue is damaged or infected.
involves increased blood circulation, blood vessel dilation, and release of chemicals like histamine and prostaglandins.
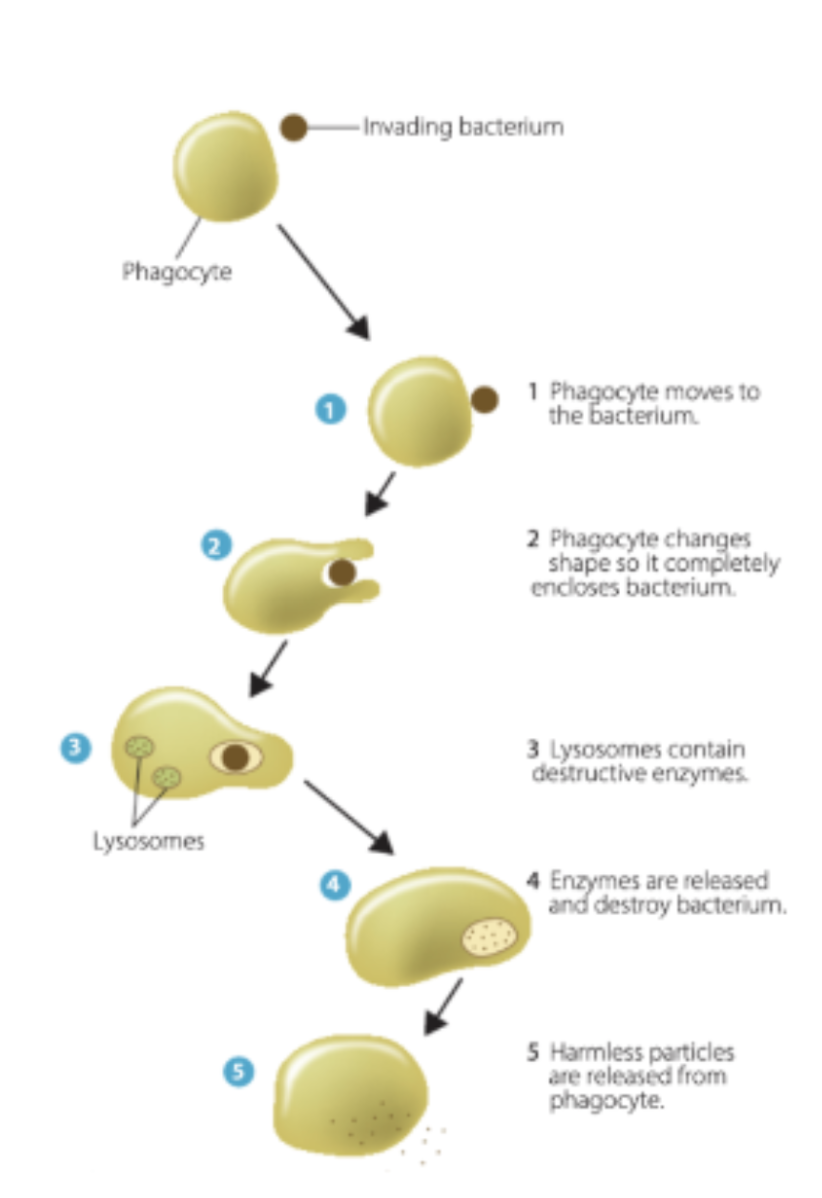
What is phagocytosis?
process by which phagocytes engulf and destroy foreign or unwanted material, such as bacteria or viruses.
Virus and cell must come into contact with one another
Virus binds to cell surface receptors on the macrophage
Macrophage surrounds virus and engulfs into the cell
Surrounded virus becomes completely enclosed in a bubble-like structure, called a ‘phagosome’, within the cytoplasm
Lysosome breaks down virus by lowering pH of its internal environment → kills/neutralises so cannot infect cell
What is a macrophage?
specialised cell involved in detection, phagocytosis and destruction of bacteria and other harmful organisms
* Pathogens are drained to lymph nodes via lymph fluid, where they are killed or neutralized by immune cells.
What is cell death to seal off pathogens?
aka apoptosis
Occurs when body is unable to neautralise an antigen
Process: macrophages and lymphocytes completely surround a pathogen so it is enclosed in a cyst
Cells die - pathogen is isolated from food supply and also dies
Present in tuberculosis and leprosy
What is the third line of defense in the immune system?
Acquired/specific immunity - not present at birth but is developed over time due to exposure to infection
antibody-mediated and cell-mediated immunity
What are t-cells?
type of white blood cell
What is cell-mediated immunity?
third line of defence
involves T-cells, a type of white blood cell.
control the specific immune response inside cells and are responsible for targeting pathogen
bacteria, virus in cells, protozoans, fungi, flatworms, roundworms, cancer, transplanted organs
Activated due to receptor proteins on the surface that recognised specific antigens → differentiated into 4 different cell types
Helper T cells
Cytotoxic (killer) T cells
Memory T cells
Suppressor T cells
1. Produced in bone marrow
2. Released into the blood and mature in thymus gland
3. Once matured, they are released into the blood again where they circulate in an inactive state
4. If T-cell comes into contact with its specific antigen, the receptors on its surface allows it to bind it and the cell becomes activated
**Killer T cells**
* Responsible for removing pathogens and infected host cells
* Do this by binding with the cell and secrete/object toxic chemicals into the target cell
* Also sometimes kill the body’s own cells
* Produced in respnse to helper T cells or free antigens
* Help promote the activities of other immune responses
* Secrete cytokines
* Produce chemicals that stimulate the production of multiple copies of B and cytotoxic T cells in response to the detection of an antigen
* They also stimulate macrophages and other phagocytes to engulf antigens
* Help promote inflammation
* Produced during time of infection
* Remain in the body and recognise later infections by the same antigen → they reactivate quickly when this occurs
* They persist after an infection, to enable a larger and faster response upon reinfection with the same pathogen
* If body is exposed to same antigen, the memory T cells will recognise it and divides into cytotoxic an d helper T lymphocytes
What are B-cells?
type of white blood cell
What is antibody-mediated immunity?
involves B-cells, a type of white blood cell.
mature and develop in bone marrow
control humoral response in which B cells present in the blood and lymph are activated by the presence of antigens
B-cells produce antibodies that combine with antigens, forming antigen-antibody complexes.
This activation leads to the destruction of bacteria and is part of the humoral immune response.
differentiate into:
plasma cells
memory b cells
1. Produced and mature in bone marrow
2. Once matured they are released into the blood
3. They accumulate in the lymohoid tissues
4. When B-cell comes into contact with a specific antigen it becomes activated
5. Once triggered by an antigen, it begins to proliferate to form millions of clones
What are plasma cells?
Produce antibodies that attach to pathogen on the outside of the body cell
Proteins which bind to specific antigens
They secrete antigen-specific antibodies that then move via the blood and lymph to infected areas
* If animal is exposed to same antigen again, memory cells recognise it and divided to produce anti-body producing plasma cells
* Remain in the body
What are the two types of immunity?
active
passive
\
* A person's resistance to strep throat due to a previous infection or a person's immunity to polio due to the polio vaccine
\
* Passive immunity occurs when a baby receives a mother's antibodies through the placenta or breast milk.
What are some interrelated factors involved in limiting the spread of infectious diseases at the local level?
neighbourhood, village, city, town
Personal hygiene practices, such as washing hands and cleaning surfaces
Safe health practices, including protection against sexually transmitted infections and staying home when sick
Provision of public information to raise awareness and knowledge
Neighbourhood or community-based initiatives
What are some interrelated factors involved in limiting the spread of infectious diseases at the regional level?
region/country
Climate, which influences the distribution of disease vectors
Sanitation facilities and practices, including water supply and anticontamination measures
Surveillance systems for disease recognition, diagnosis, and effective response
Access to clean water and adequate food storage and preservation
What are some interrelated factors involved in limiting the spread of infectious diseases at the global level?
international
Communication between countries and global health organizations, such as the World Health Organization (WHO)
Quarantine measures, including travel bans and monitoring the movement of potentially affected individuals
Limiting travel between countries
Collaborative efforts and information sharing among nations
Case Study: Cholera
acute diarrhoeal infection caused by ingestion of food or water contaminated with the bacterium Vibrio cholerae.
local
not shaking hands
wash utensils
wash hands with soap
cover food (prevent vector of fly)
isolate infected individuals (quarantine)
regional
water supply: access to clean water
sanitation facilities: inadequate disposal facilities may lead to contamination of water supplies, poor hygiene, and living conditions
food: contamination or poor preservation may lead to a spread of food-borne infections
global
Limiting travel between countries
Communicating between countries with the global health organisations is essential
Implementation of quarantine measures – involving travel bans into or out of countries significantly affected by disease outbreaks
* quarantine
* vaccination
* public health campaigns
* use of pesticides
* genetic engineering
What are personal hygiene practices?
washing hands → Prevents the spread of pathogens that cause symptoms such as diarrhoea (e.g. cholera)
cough/sneeze into elbow → Prevents airborne droplets from spreading to others
What are community hygiene practices?
sterilisation and disinfection of equipment → dentists, doctors, reduces the risk of the spread of pathogens from one person to another
social distancing → reduces the risk of transmission of diseases throughout the population – very important in controlling disease (covid)
food/water cleanliness → cook enough, cover, clean water source. e.g. salmonella – chicken must be cooked to at least 71°C (when bacteria is killed)
* involves isolating potentially infected individuals or items to prevent the spread of disease.
What is vaccination?
the introduction of a vaccine into the body to stimulate an immune response and provide immunity against a specific disease.
Response produces memory cells for the antigen and gives the body immunity = secondary response occurs to avoid worst symptom if antibody enters host again
Vaccination primes the immune system to deal with a pathogen it has never been in contact with
* Vaccines contain cultures of microorganisms, either living but attenuated or dead, which stimulate the immune response.
What is passive acquired immunity?
involves the introduction of antibodies (immunoglobulins) into the body to prevent a disease from developing.
These antibodies are obtained from another organism that has previously had the disease.
no memory cells produced → will only last a couple of months
* focus on management and prevention, leading to healthier choices in the community and preventing the spread of disease.
* ‘Slip, slop, slap’
* Skin cancer and sun protection prevention campaign
* Memorable catch phrase → helped educate a wide variety of people
* reduces the occurrence of disease and controls its spread through the population.
* pesticides include insecticides, fungicides, and herbicides.
* Genes can be inserted into plants and animals to confer resistance to specific diseases.
What is an example of genetic engineering?
BT cotton = disease resistant crop grown in Australia
Plants genetically modified so that they produce a poison/protein which kills the cotton pest helicoverpa caterpillar
Gene taken from soil bacterium known as Bacillus thuringinesis (BT for short)
Which pathogen is targeted by antibiotics?
bacteria
e.g. penicillin
Which pathogen is targeted by antivirals?
virus
e.g. antiretro → AIDS
Which pathogen is targeted by antifungals?
fungi
e.g. fluconazole
Which pathogen is targeted by antiprotozoals?
protozoa
e.g. doxycycline
Define antivirals.
a class of antimicrobial used to treat viral infections, by inhibiting the development of pathogen inside the host cell (NOT killing the virus)
they don’t cure the disease but slow down its progress, allowing the body’s natural defences to take over – if taken early in course of disease, symptoms will be milder and of shorter duration
examples of diseases antivirals are used for
HIV
Influenza A
Herpes
Hepatitis B and C
Define antibiotics.
a class of antimicrobials used to treat bacterial infections, May be achieved either by killing the infective bacteria, or inhibiting its growth.
Stop growth or kill bacteria by…
Interference with cell membrane permeability
Interference with nucleic acid synthesis
Interference with protein synthesis
Interference with cell wall synthesis
What is antibiotic resistance, and why is it a growing concern?
when bacteria develop mechanisms to avoid or deactivate antibiotics.
It's a concern due to the misuse and overuse of antibiotics, leading to the evolution of antibiotic-resistant bacterial strains.
Explain the process of antibiotic resistance development.
Within a bacterial population, a few bacteria are naturally antibiotic-resistant.
When antibiotics are used, most bacteria are killed, but resistant ones survive and reproduce, passing on their resistance genes.
Additionally, bacteria can transfer resistance genes to each other using plasmids, speeding up resistance evolution.
What is ebola?
severe infectious and contagious caused by the Ebola virus
Easily preventable: spread when people have close direct contact with body fluids and mucous membranes (as well as items contaminated by these) from infected individuals, including sexual transmission
Large outbreak west Africa 2014-2016
What are some methods to control ebola?
control of epidemic in clinical setting
quarantine
cleaning
environmental