The High Risk Newborn
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
Who is at Risk?
Low socioeconomic status of the mother.
Limited access to healthcare or no prenatal care.
Drug use or exposure to toxic chemicals.
Pre-existing maternal medical conditions or pregnancy complications.
Newborn Classifications
Micro preemie: Born before 26 weeks or less than 0.8 kg
Preterm (preemie): 36 6/7 weeks (before 37 weeks)
Late preterm: 34 to 36 weeks 6/7 weeks
Term: 38 to 41 completed weeks
Post-term: Greater than 42 weeks
Birth Weight Variations
Large for gestational age (LGA): Above the 90th percentile growth curve or > 4.0 kg
Small for gestational age (SGA): Below the 10th percentile growth curve or < 2.5 kg
Very small for gestational age (VSGA): Below the 3rd percentile growth curve
Low birth weight (LBW): < 2500 g
Very low birth weight (VLBW): < 1500 g
Extremely low birth weight (ELBW): < 1000 g
Large for Gestational Age Infant (LGA)
Macrosomia:
Definition: Weight above 4 kg
Infant of a Diabetic Mother: Large body, normal head circumference (H/C)
Potential Problems:
Hypoglycemia and hyperinsulinemia
Birth trauma: Shoulder dystocia, CNS injury
Polycythemia
Hyperbilirubinemia
Poor feeding
Thermal instability
Infant of a Diabetic Mother (IDM)
Insulin does not cross the placenta.
Glucose does cross the placenta.
The fetus increases insulin production in response to the mother's high glucose levels.
Hypoglycemia may occur at birth.
Symptoms of Hypoglycemia (1 to 2 hours post-delivery):
Tremors/jitteriness
Cyanosis
Apnea
Temperature instability
Poor feeding
Hypotonia
Seizures
Interventions:
Control maternal glucose levels
Monitor for signs of hypoglycemia
Early feeding (oral or IV if unable to feed orally)
IV glucose: D10W if unable to PO
Glucose monitoring q30 to 60 minutes until stable, then q24h and before each feeding
Monitor electrolytes
Assess for congenital anomalies
Small for Gestational Age Infants (SGA)
Below the 10th percentile in weight or Intrauterine Growth Restriction (IUGR).
Can apply to Preterm, Term, or Post-Term infants.
Appearance:
Wasting
Decreased fat stores
Loose, dry skin
Poor muscle tone
Wide skull sutures
Potential Problems:
Increased respiratory effort
Hypoglycemia
Polycythemia
Cold stress
Term vs Preterm Neonate (picture)

Term >37 weeks
Successfully adapts to the extrauterine environment.
Pink at birth.
Strong muscle tone and reflexes.
Vigorous cry and respiratory effort.
Normal respiratory rate.
Normal cardiac rate and rhythm.
Preterm before 37 weeks
Immature central nervous system and other systems.
Thermoregulation problems.
Hypoglycemia.
Feeding problems.
Posture lacks flexion.
Decreased muscle tone (hypotonia).
Skin thin and transparent.
Lanugo (shed during the 7th to 8th month of gestation).
Respirations: rapid, periodic breathing.
Abdomen: soft, slightly rounded to scaphoid.
Eyes: fused until 25 ½ to 26 ½ weeks.
Ears: pinna flat without cartilage, folded.
Born after 42 weeks
Can be SGA or LGA.
Deep creases over soles of feet.
Thick ear cartilage.
No lanugo.
Increased risk for meconium aspiration.
Uteroplacental insufficiency.
Increased mortality risk.
Intraventricular Hemorrhage
Primarily related to prematurity.
90% occurs within the first 72 hours of life.
Can cause long-term developmental delay.
Clinical Manifestations:
Possibly none.
Hypotonia.
Increased heart rate (HR).
Low blood pressure (BP).
Hypoxic-Ischemic Encephalopathy
Possible Causes:
Intrauterine abruption.
Cord issues.
Resuscitation at birth.
Newborn Presentation:
Limp.
Cyanotic.
Bradycardic.
Apneic upon initial assessment.
Treatment:
Head and body cooling.
Outcome:
Outcome is variable and can lead to neurological impairment.
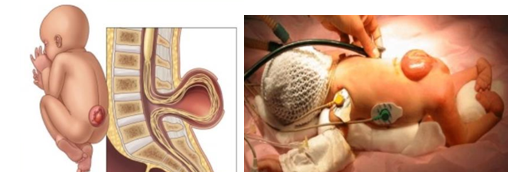
Meningocele/Myelomeningocele
Meningocele: Protrusion of a sac that contains meninges and spinal fluid.
Myelomeningocele: Sac-like cyst that contains meninges, spinal fluid, and a portion of the spinal cord and nerves.
Physical Assessment:
Sensory/motor function depends on the location.
Latex allergy.
Possible loss of movement/sensation in the lower extremities.
Neurogenic bladder/constant dribbling of stool.
Clubbed feet are common.
Repaired within 24 to 48 hours.
May develop hydrocephalus after surgical repair; monitor head circumference.
Hydrocephalus
Clinical Presentation:
Widened sutures
Full/fontanelles
Sunsetting eyes
Vomiting, lethargy, irritability
Visible scalp veins
IVH (Intraventricular hemorrhage) can cause post-hemorrhagic hydrocephalus
May occur after myelomeningocele closure
Treatment:
EVT (Endoscopic Third Ventriculostomy)
VAD (Ventricular Access Device)
VP Shunt (Ventriculoperitoneal Shunt)
Educate Families on Shunt Malfunctions and Infections:
Irritability, vomiting, increased head circumference, lethargy, change in feeding patterns.

Transient Tachypnea of the Newborn
Most common in LGA, post-term, and C-section infants.
Respiratory rate (RR) > 60, up to 80 to 100.
Shortly after birth: grunting, nasal flaring, retractions, cyanosis.
Improves within 12 to 72 hours.
Interventions:
Supportive treatment, including IV fluids and supplemental oxygen.
Meconium Aspiration Syndrome (MAS)
Risk Factors:
Post-term newborns
Long labor
Maternal smoking, diabetes, chronic cardiovascular disease, or hypertension
Intrauterine growth restriction (IUGR)
Clinical Presentation:
Tachypnea with rales
Grunting, flaring, retracting, low Apgar scores
Barrel-shaped chest
Meconium-stained skin, nails, and umbilical cord
Interventions:
If distressed:
Resuscitation with 100% oxygen
Direct tracheal suctioning (if decompensated)
Mechanical ventilation
High-frequency oscillation
Surfactant administration
Antibiotics for infection
Maintain pulmonary blood flow with volume expanders and vasopressors
Persistent pulmonary hypertension of the newborn (PPHN): nitric oxide, ECMO
Respiratory Distress Syndrome (RDS)
Surfactant deficiency and structural Immaturity.
Clinical Presentation:
Tachypnea, grunting, flaring, retractions
Poor lung compliance
Hypotension
Altered electrolytes
Interventions:
Monitoring:
Cardiac monitors (CR)
Pulse oximetry (POX)
CO2 monitoring
Correct acidemia and reduce hypoxemia
Antenatal corticosteroids
Supplemental oxygen and ventilation
Exogenous surfactant:
Administered intra-tracheally via endotracheal tube (ETT)
Monitor for pneumothorax and adjust ventilation as needed.
Involve and inform the family (mother may still be receiving medical care).
Giving Surfactant/Curosurf
The infant must be intubated; surfactant is given via endotracheal tube (ETT).
Position the infant flat and midline.
Pre-oxygenate and suction the infant.
The initial dose is given in two aliquots.
Rapidly administer half of the total dose (one aliquot).
Immediately manually bag the patient for 1 minute.
Repeat with the second aliquot.
Immediately manually bag the patient for 1 minute.
Do not rotate the patient from side to side; keep the infant flat and midline.
Do not suction the patient for at least 1 hour after the dose is given.
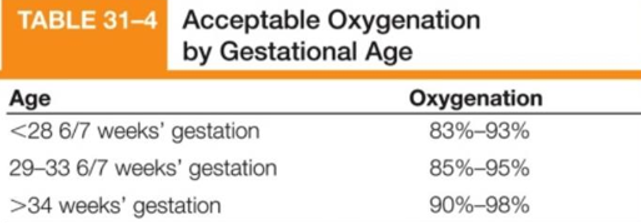
Acceptable Oxygenation by Gestational Age (picture)
Bronchopulmonary Dysplasia (BPD)
Definition: Chronic lung disease following neonatal lung injury.
Causes: Barotrauma, Respiratory Distress Syndrome (RDS), Persistent Pulmonary Hypertension of the Newborn (PPHN).
Physical Assessment:
Hypoxia
Hypercarbia
Growth failure
Pulmonary hypertension
Cor pulmonale and right-sided heart failure (HF)
Complications:
Increased mortality
Chronic respiratory infections
Home oxygen therapy
PPHN
Fractures and rickets
Neurodevelopmental sequelae
Management:
Prevent development of BPD discharge.
Prevent and manage hypoxia and hypercarbia.
Use the lowest oxygen and ventilator settings tolerated.
Administer corticosteroids
Administer bronchodilators
Provide chest physiotherapy (CPT), positioning, and suctioning.
Nutrition: Ensure increased caloric intake,
Address co-existing conditions like gastroesophageal reflux (GER), emesis, fatigue, and oral aversions.
Provide emotional support, home care, and respite care.
Persistent Pulmonary Hypertension (PPHN)
Persistent Fetal Circulation (PFC):
Definition: A right-to-left shunt away from the lungs and through the ductus arteriosus and patent foramen ovale (PFO), bypassing the lungs. This results in hypoxemia and acidosis, which stimulate pulmonary vasoconstriction and increase pulmonary vascular resistance (PVR).
Common Etiology:
Hypoxia
Asphyxia
Bacterial sepsis
Treatment:
Oxygenation
Ventilation
Nitric oxide (pulmonary vasodilator)
Volume expanders
Vasopressors
Afterload reducers
Hemodynamic support
Extracorporeal Membrane Oxygenation (ECMO)
UAC/UVC
UAC (Umbilical Artery Catheter):
Used to draw frequent blood samples and ABGs
Continuously monitor blood pressure
Monitor capillary refill in fingers, toes, and bottom
Alert the provider and prepare to pull the catheter if changes occur
UVC (Umbilical Venous Catheter):
Inserted into the vein of the umbilical cord
Used for IV fluids, nutrition, medications, and drips
Monitoring:
Monitor UAC/UVC for bleeding and proper placement!
Patent Ductus Arteriosus (PDA)
Definition: The fetal shunt between the left pulmonary artery and the descending aorta fails to close.
Common in premature infants.
Symptoms:
Unstable blood pressure
Widened pulse pressure
Bounding peripheral pulses
Murmurs
Increased oxygen requirement
Swinging SpO2
Metabolic acidosis
Interventions:
Fluid restriction
Diuretics
Respiratory support
Close the PDA
Prostaglandin Synthase Inhibitors:
Indomethacin or Ibuprofen (current practice varies)
Acetaminophen (Tylenol)
Surgical ligation
Feeding and Nutrition
Goal:
Steady weight gain
Nutrition:
High-calorie, high-protein formula supplemented with breast milk
Vitamin supplements (e.g., Poly-Vi-Sol)
Enteral vs. Parenteral Nutrition:
TPN/Lipids for parenteral nutrition
Feeding Methods:
Gavage feeding for infants who are unable to suck effectively
Bolus vs. intermittent feedings
Non-nutritive sucking to stimulate sucking reflex
Breastfeeding:
Breast milk is preferred
Early feeding is encouraged
Trophic feeds (small, stimulating feeds) or stimulus feeds for infants
Feeding Intolerance
Symptoms:
Emesis
Distension
Bowel loops
Decreased bowel sounds
Irritability/lethargy
Indications:
Necrotizing enterocolitis (NEC)
Sepsis
Acidosis
Necrotizing Enterocolitis (NEC)
Etiology:
Unknown
Research suggests 3 mechanisms:
Ischemia
Bacterial colonization of the bowel
Enteral feedings
Most common in infants <29 weeks gestation:
Hypoxia
Necrosis
90% of cases occur in preterm infants
Mortality rate of 22%, which increases to 50% if surgical intervention is needed.
Assessment: Signs & Symptoms:
Abdominal distension/shiny, discolored**
Bilious emesis**
Blood stools**
Decreased bowel sounds
Temperature instability
Poor perfusion
Metabolic acidosis/respiratory distress
Hypotension
Radiographic Changes:
Dilated bowel loops
Pneumatosis intestinalis
Interventions:
EMERGENCY!!
Stop feedings immediately
Decompress abdomen
Frequent CBC/CMP
Respiratory examination frequently
Septic workup and antibiotics (possible perforation)
Surgical resection or drain placement
Hyperbilirubinemia
Jaundice:
Elevation of serum bilirubin levels which result in jaundice.
Types of Jaundice:
Physiological Jaundice: Benign, caused by the breakdown of fetal red blood cells and an immature liver.
Pathologic Jaundice: Results from an underlying disease, appears before 24 hours, or persists beyond 14 days.
Acute Bilirubin Encephalopathy: Bilirubin deposits in the brain, potentially resulting in permanent damage.
Kernicterus: Irreversible bilirubin toxicity that leads to severe cognitive impairments, hypotonia, and quadriplegia.
Risk Factors:
Increased RBC production or breakdown
Rh or ABO incompatibility
Decreased liver function
Prematurity
Total serum bilirubin (TSB) at 12 hours <9.0
Assessments:
Yellow skin, sclera, and mucous membranes
Elevated bilirubin levels in labs
Hypoxia, hypothermia, and hypoglycemia
Interventions:
Monitor vital signs
Phototherapy: Maintain eye mask, keep infant undressed, avoid lotions
Monitor for Effects of Phototherapy: Dehydration, rash, bronze discoloration, elevated temperature
Maintain/monitor fluid status
Encourage parent bonding, explain phototherapy, and the reason for loose, greenish stools
Possible exchange transfusion
Retinopathy of Prematurity
Abnormal vascularization of the retina due to:
Too much oxygen causing damage, which leads to overgrowth or abnormal regrowth of blood vessels.
Risk Factors:
Generally affects low birth weight (LBW) preterm infants.
Outcomes:
Can lead to blindness if left untreated.
Prevention:
Cautious use of oxygen** to avoid excessive oxygen levels that may contribute to retinal damage.
Treatment:
Laser photocoagulation or Avastin (anti-VEGF treatment).
Apnea of Prematurity
Definition: Apnea in newborns <37 weeks gestation, characterized by:
20 seconds or longer or shorter periods if associated with cyanosis, pallor, or bradycardia.
Cause:
Due to an immature CNS (central nervous system).
Incidence:
Decreases with gestational age as the infant matures.
Interventions:
Assessment and close monitoring of the infant.
Prone positioning (if not contraindicated).
Gentle stimulation (back or foot) to encourage breathing.
Documentation:
Duration, heart rate (HR), and O2 saturation must be documented.
Nursing Care:
Medications like caffeine or theophylline may be used.
Respiratory support as needed.
Family support and community care for ongoing care needs.
Neonatal Sepsis (Birth to 28 days)
Characteristics:
Immature immune systems and inability to localize infections.
Poor inflammatory response and ineffective phagocytosis.
Lack of IgM immunoglobulin.
Assessment:
May rapidly deteriorate within the first 12 hours post-delivery.
Subtle behavioral changes:
Lethargy or irritability.
Color changes: pallor, dusky, cyanosis, mottling**.
Skin cool and clammy.
Temperature instability** (commonly hypothermia, rarely hyperthermia).
Tachycardia.
Later signs: apnea, bradycardia.
Feeding intolerance.
Vomiting, diarrhea, abdominal distension.
Poor suck or disinterest.
Hyperbilirubinemia.
Diagnostics:
Comprehensive workup:
Aerobic and anaerobic blood cultures.
CSF culture.
Urine culture (suprapubic or sterile catheter).
Tracheal aspirate (if intubated).
Cultures from wounds or tubes.
CBC with differential.
CRP (C-reactive protein).
Chest X-ray.
Interventions:
Broad-spectrum antibiotic therapy as soon as cultures are obtained:
Ampicillin.
Cefotaxime (Claforan).
Zosyn.
Meropenem.
Supportive care:
Respiratory support.
Hemodynamic support.
Nutritional support.
Metabolic management.
Prevention:
Strict handwashing.
Use of isolettes.
Visitation restriction to unnecessary personnel.
Clean equipment and incubators weekly.
Aseptic technique.
Supportive care:
Neutral thermal environment.
Respiratory support.
Cardiac care (monitor for anemia, hyperbilirubinemia, heart rate, blood pressure).
Nutrition.
Fluid and electrolyte balance.
Thermoregulation in Preterm Infants
Big issue with preterm infants.
High ratio of body surface area to body weight.
Thinner, more permeable skin.
Decreased ability to vasoconstrict.
Hyperthermia
Elevated temperature
Tachycardia
Ruddy skin color
Increased metabolism
Always check temperature before calling the provider!
Hypothermia/Cold Stress
Manifestations:
Color:
Pale
Acrocyanosis
Mottling
Respiratory distress:
Nasal flaring
Apnea and/or bradycardia
Behavior:
Lethargic/hypotonic
Feeble cry
Poor feeding
Interventions:
Neutral Thermal Environment (isolette):
Servo control skin probe**
Radiant warmer
Double-walled isolette
Humidity**
Other Interventions:
Use warm blankets/swaddling
Allow skin-to-skin care when possible
Keep the skin dry and cover the head with a cap
Cover the baby with plastic/polyethylene wrap**
Warm and humidify oxygen**
Use a skin probe to regulate temperature
Stress Cues
Hiccupping
Yawning
Sneezing
Frowning
Looking away
Squirming
Frantic, disorganized activity
Arms and legs pushing away
Arms and legs limp and floppy
Skin color changes
Ready to Interact
Normal skin color
Arms and legs flexed or tucked
Hands touching their face
Sucking
Looking at you
Smiling and appearing relaxed
Regular breathing rate
If the baby is on a monitor, a regular heartbeat
Developmental Care: Outcomes
Infant:
Stress is reduced, and sleep time is increased.
Promotes growth and development.
Decreases ventilator/supplemental oxygen time.
Results in more successful feeding.
Improves neurodevelopmental outcomes.
Reduces length and cost of stay.
Family/Caregiver:
The family becomes a collaborator in the infant's care.
Improves the family's emotional and social well-being.
Proper Positioning
Neutral head position (to prevent misshapen head/torticollis).
Rounded shoulders.
Hips and knees flexed.
Toes pointed straight.
Hands to mouth.
Boundaries provided appropriately.
Mimic the fetal position (which is often lacking in preterm infants).
Goal: Comfort and containment to promote development.
Family Centered Care
The infant is viewed as an integral part of the family group.
Care is directed at both the infant and the family.
Care is provided through a collaborative relationship with the family.
Encourage family presence, participation, and communication.
Open visitation hours and policies that encourage visitation.
Include the family in interdisciplinary conferences.
Encourage the mother to pump and explain the benefits of breast milk for the baby's health.
Skin-to-skin care.