week 23 reproductive health
menstrual blood flow
= shedding of the endometrium → inner lining of the uterus passes through the small opening in the cervix → out of the body through the vagina
usually there is also some retrograde blood flow through the fallopian tubes into the ==abdominal cavity==
normal menstrual cycles can range from 21-35 days in adults (less = oligomenorrhoea, more = poly)
menstrual cycles are slightly irregular during the first 2-4 years
- 55% are anovulatory
- the blood shed is caused more by ==imbalanced oestrogenic endometrial stimulation==
towards the end of the reproductive lifespan (perimenopause), the interval between cycles decrease and menstrual cycles become irregular just before the final menstruation (menopause)
hormonal regulation of the menstrual cycle
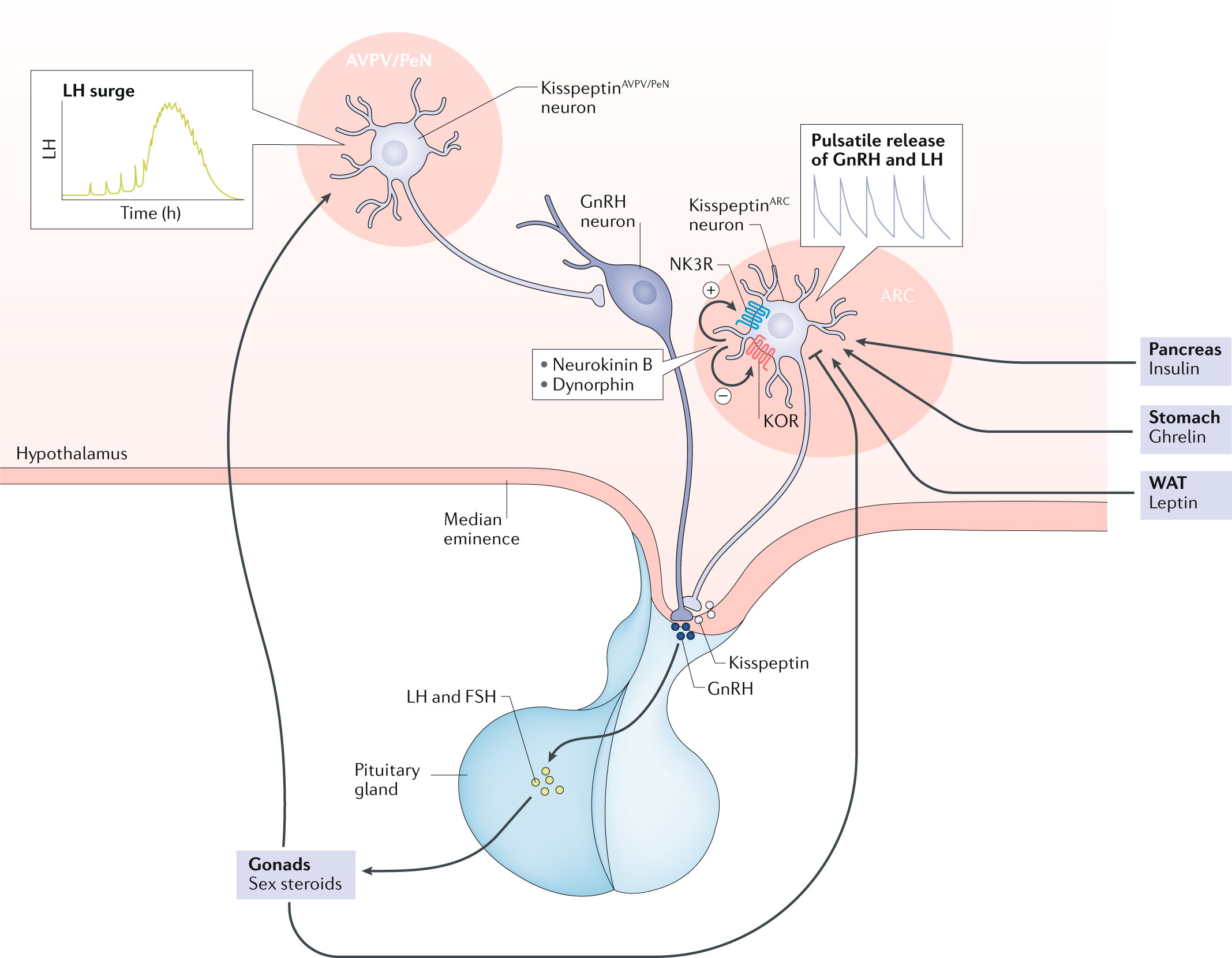
controlled by the HPG axis
GnRH secretion is a pulsatile from the hypothalamus (^^base of the 3rd ventricle just behind the optic chiasm^^) → regulates the secretion of LH and FSH from the AP → control the steroidogenic production of sex steroids for the ovaries
- kisspeptin neurons in the preoptic area and infundibular nucleus → co-express neurokinin B and dynorphin → directly signal GnRH neurons
- under negative control of the sex steroid hormones, opioids such as endorphins and ghrelin
- stimulated by leptin (???)
LH and FSH levels in prepubertal girls are extremely low
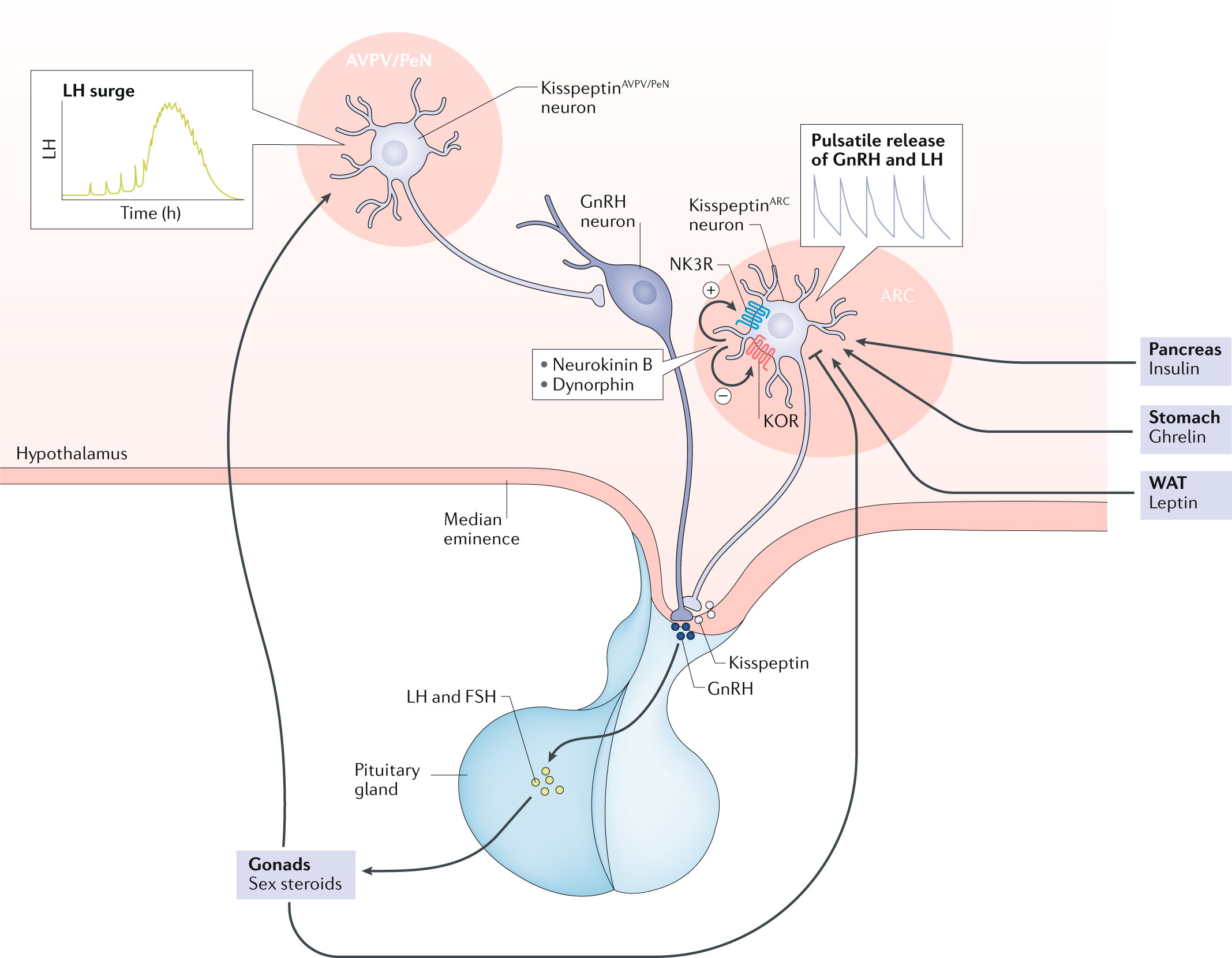
just prior to a menstrual period, oestrogen, progesterone and inhibin A levels are decreased → increase in FSH → ovarian follicle recruitment → induces growth and aromatase activity → ==granulosa cells in these follicles produce oestrogens and inhibin B (inhibin B will eventually inhibit FSH release)==
LH induces the production of androgens in theca cells
- ==theca cells== = cells on the outer part of the follicle separated from the granulosa cells by a basal lamina
- progesterone is produced in low quantities in the follicular phase under the influence of LH in theca cells
oestrogens provide negative feedback to the hypothalamus and pituitary
==Moreover, rising levels of oestradiol, the most prominent oestrogen, is associated with an increase in the pulse frequency of GnRH release from the hypothalamus???????????????? CONTRADICTION???==
when FSH decreases, only the largest of the growing follicles is rescued (and become dormant? → growth further and produce increasing quantities of oestradiol), the rest become atretic and disappear
higher levels of oestradiol → proliferation and growth of the endometrium???
ovulation completes successful follicle development = release of the oocyte granulosa cumulus cells from the follicle
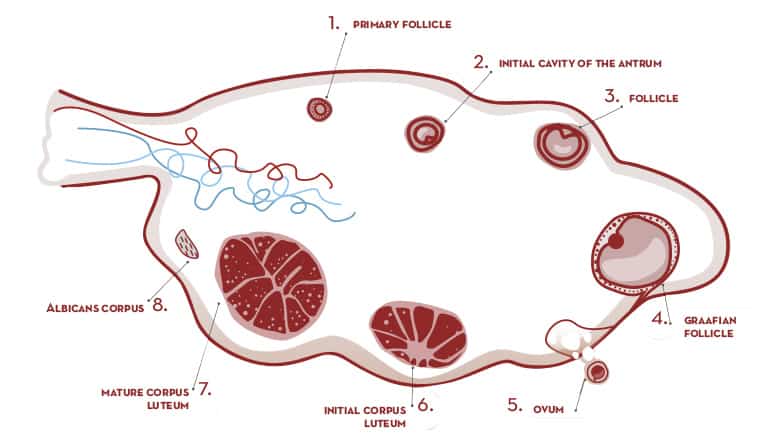
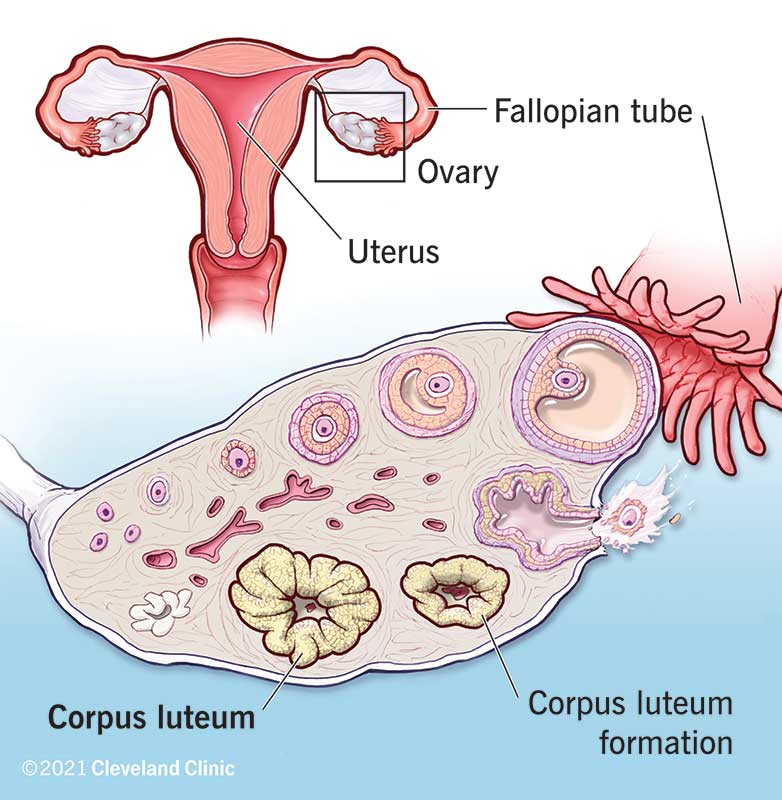
the granulosa cells (antral and mural) and theca cells left behind will luteinize and form the corpus luteum
1/69
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
menstrual blood flow
= shedding of the endometrium → inner lining of the uterus passes through the small opening in the cervix → out of the body through the vagina
usually there is also some retrograde blood flow through the fallopian tubes into the ==abdominal cavity==
normal menstrual cycles can range from 21-35 days in adults (less = oligomenorrhoea, more = poly)
menstrual cycles are slightly irregular during the first 2-4 years
- 55% are anovulatory
- the blood shed is caused more by ==imbalanced oestrogenic endometrial stimulation==
towards the end of the reproductive lifespan (perimenopause), the interval between cycles decrease and menstrual cycles become irregular just before the final menstruation (menopause)
hormonal regulation of the menstrual cycle
controlled by the HPG axis
GnRH secretion is a pulsatile from the hypothalamus (^^base of the 3rd ventricle just behind the optic chiasm^^) → regulates the secretion of LH and FSH from the AP → control the steroidogenic production of sex steroids for the ovaries
- kisspeptin neurons in the preoptic area and infundibular nucleus → co-express neurokinin B and dynorphin → directly signal GnRH neurons
- under negative control of the sex steroid hormones, opioids such as endorphins and ghrelin
- stimulated by leptin (???)
LH and FSH levels in prepubertal girls are extremely low
just prior to a menstrual period, oestrogen, progesterone and inhibin A levels are decreased → increase in FSH → ovarian follicle recruitment → induces growth and aromatase activity → ==granulosa cells in these follicles produce oestrogens and inhibin B (inhibin B will eventually inhibit FSH release)==
LH induces the production of androgens in theca cells
- ==theca cells== = cells on the outer part of the follicle separated from the granulosa cells by a basal lamina
- progesterone is produced in low quantities in the follicular phase under the influence of LH in theca cells
oestrogens provide negative feedback to the hypothalamus and pituitary
==Moreover, rising levels of oestradiol, the most prominent oestrogen, is associated with an increase in the pulse frequency of GnRH release from the hypothalamus???????????????? CONTRADICTION???==
when FSH decreases, only the largest of the growing follicles is rescued (and become dormant? → growth further and produce increasing quantities of oestradiol), the rest become atretic and disappear
higher levels of oestradiol → proliferation and growth of the endometrium???
ovulation completes successful follicle development = release of the oocyte granulosa cumulus cells from the follicle
the granulosa cells (antral and mural) and theca cells left behind will luteinize and form the corpus luteum
==Factors and processes leading to the LH surge are not completely understood. While oestrogen and progesterone levels have an inhibitory effect on LH secretion, the increase in oestrogens and a subtle end-follicular phase progesterone increase enormously enhance pituitary sensitivity of GnRH resulting in the LH surge==
the key feature of the timing of the mid cycle LH surge is…
the progressive increase of pituitary sensitivity to GnRH triggered by positive feedback signals from the ovary that the follicle has reached ovulatory status
is accompanied by an FSH surge for unknown reasons
what hormone causes ovulation
LH
corpus luteum
after ovulation → remaining follicle collapses → corpus rubrum → corpus luteum (vascularised) → will continue to produce oestrogens
vascularisation of the complete corpus luteum enables the luteal granulosa cells to produce progesterone + inhibin A → decrease in FSH and LH
eventually, the decrease in LH will cause the stimulation of the corpus luteum to decrease → decrease in progesterone, oestradiol and inhibin A → corpus luteum ‘dissolves’ → endometrium lining the uterus will also become less vascularized and will therefore shed from its basal lamina resulting in ==menstrual blood flow==
→ feedback of oestradiol, progesterone and inhibin A on the hypothalamus and pituitary → increase in FSH again to recruit follicles for the next menstrual cycle
==how could there be a further increase in oestradiol if inhibin B inhibits the secretion of FSH?????==
why do FSH levels continue to decrease towards the end of the early follicular phase of the cycle
due to progressive negative inhibin B feedback
the most prominent oestrogen is…
oestradiol
androgens provide the substrate for…
oestrogen production which is facilitated through aromatase induction in granulosa cells as a result of FSH stimulation
what occurs immediately after LH surge
progesterone strongly increases due to enzymatic system of theca cells
LH surge increases StAR
GnRH after birth
Immediately after birth an active GnRH system is already triggering pulsatile pituitary LH and FSH secretion. The system is completely active. This pulsatile LH and FSH secretion lasts longer in girls than in boys. But after some time GnRH secretion decreases and the period of prepubertal silence follows
inhibin A,B and LH + FSH*******
mini puberty
high concentrations of leptin and kisspeptin and furthermore oestradiol and oestriol originating from the placenta are found of which the rapid post-delivery decline unleashes its negative feedback
associated with a transient increase in anti-Müllerian hormone (AMH), inhibin B and oestrogen concentrations
the onset of puberty is…
==independent== of the gonads and originates from the brain by kisspeptin reactivation and the return of pulsatile GnRH release by the hypothalamus → nocturnal LH pulse release and secretion of FSH followed by increased oestrogen concentrations in the early morning (==then how is it independent of gonads????==)
leptin signalling is a co-factor
menstrual fluid
- about half of it is blood, the rest is cervical mucus, vaginal secretions, and endometrial tissue
- blood contains sodium, calcium, phosphate, iron, and chloride (iron is relatively small)
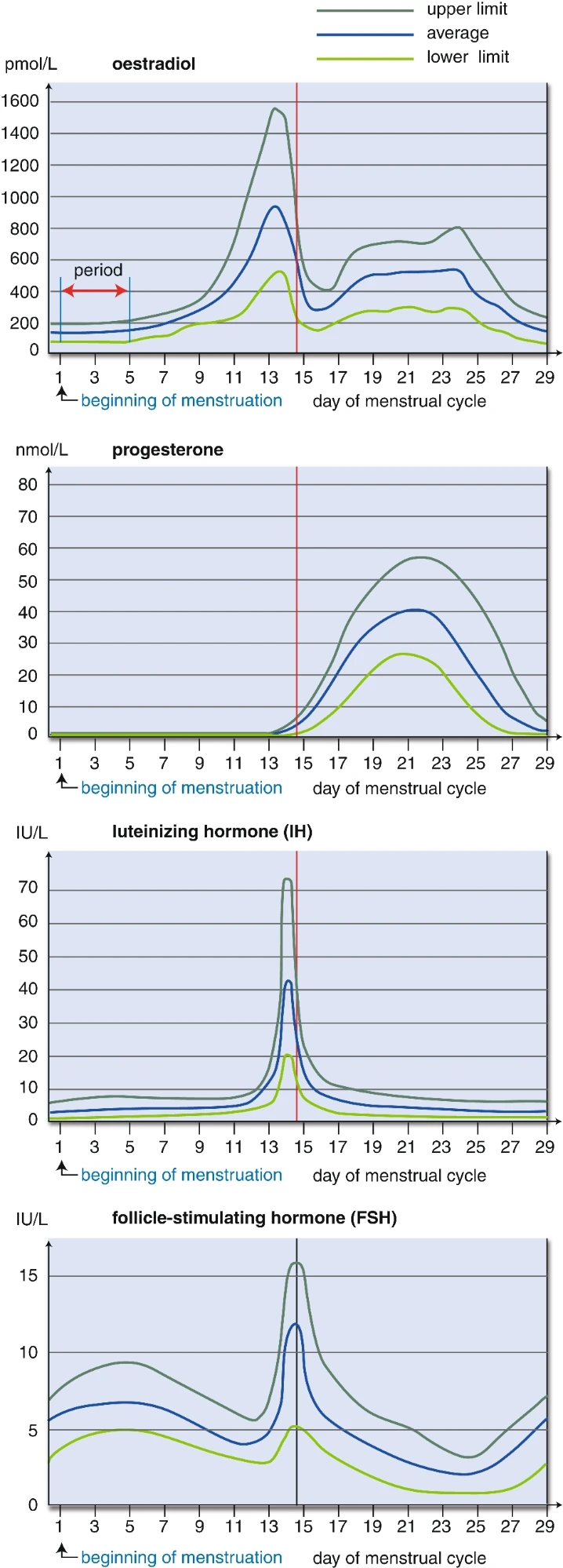
hormone levels during the normal menstrual cycle (photo)
dysmenorrhoea
painful cramps due to ischaemia and muscle contractions
ischaemia is due to constriction of spiral arteries in the secretory endometrium → allows the uterine lining to sough off
contractions of the myometrium are mediated by…
prostaglandins
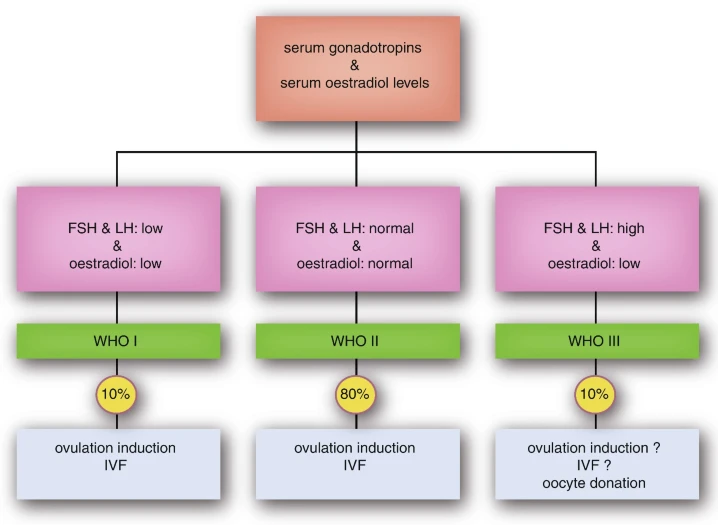
classification of menstrual cycle disturbances
classified based on the assessment of both gonadotropins (LH and FSH) and serum oestradiol levels
low/normal LH+FSH and low oestradiol → suspect a ^^central^^ defect, usually leads to ==hypogonadotropic hypogonadism== = WHO I anovulation = 10% of cases
normal LH, FSH (usually LH>FSH) and oestradiol levels → suspect a combined ^^central^^ and ^^peripheral^^ cause → ==normogonadotropic normo-oestrogenic== anovulation = WHO II = 80%
a few may also be diagnosed with PCOS (?)
this might be due to reduced hypothalamic feedback response to circulating sex steroids, especially ^^progesterone^^ → increased LH → increased stimulation of theca cells → may cause follicular arrest and cause the accumulation of antral follicles → polycystic anatomy
high LH+FSH (usually FSH>LH due to the lack of inhibin feedback) but low oestradiol → suspect an ^^ovarian defect^^ → ==hypergonadotropic hypogonadism (==^^= primary hypogonadism^^==)== or ==primary ovarian insufficiency== (POI) = WHO III (10%)
may be caused by toxic causes (eg. CT or RT), ovarian surgery or genetic causes (most of them are linked to X chromosomal abnormalities, usually Turner. other = FMR1 gene)
so,,,
central (hypothalamus or pituitary), peripheral (gonadal)
WHO I (central defect), WHO II or PCOS (combined defects) and WHO III or POI (gonadal defect)
pathophysiology of irregular menstrual cycles
hypogonadism may occur if the HPG axis is interrupted at any level
failure of the hypothalamic GnRH pulse generator (eg from stress and nutritional problems, chronic diseases, iron overload etc) may cause: ^^hypogonadotropic hypogonadism^^ or ^^functional hypothalamic amenorrhoea (1st causes the 2nd)^^
= supra-pituitary problems
true pituitary problems are less common
what medicines can cause hypogonadotropic hypogonadism
high doses or long term use of opioid medicine (mimics the effects of endorphins)
kallmann syndrome is caused by…
migration of the GnRH neurons → fail to establish contact with the pituitary
the affected genes (KAL 1, 2 or 3) also cause the migration of neurons into the bulbus olfactorius so it’s associated with a loss of the sense of smell generally referred to as anosmia
hyperprolactinaemia can cause…
hypogonadotropic hypogonadal amenorrhoea (often accompanied by galactorrhoea)
(dopamine prevents the release of prolactin so obstructive processes (for example) can prevent dopamine from reaching the anterior pituitary)
oligomenorrhoea is often due to…
anovulation
women with PCOS typically report more regular cycles as…
they get older
WHO I hypogonadotropic hypooestrogenic
- low/normal LH+FSH and low oestradiol → central cause
- clinical presentation depends on whether it is congenital or acquired, the severity of the defect and the presence of associated conditions
- acquired → usually in their 20s with delayed pubertal onset, absent or poorly developed secondary sexual characteristics, primary amenorrhoea, eunuchoid proportions, or infertility
- presence of anosmia is suggestive of Kallmann syndrome
- adult onset is characterised by secondary amenorrhoea, decreased libido, infertility, and osteoporosis → do a brain MRI to rule out pathology at that level
- always check AP gland function to rule out a more complex endocrine disorder with multiple hormone deficiencies
- renal US is usually recommended if they have syndromic FHA eg. in Kallmann syndrome
- related to profound impairment of reproductive functions including anovulation and infertility
- may affect the skeletal system, cardiovascular system + cause mental problems → osteopenia and osteoporosis are the main long term complications
how is the pituitary adrenal axis assessed
checking morning cortisol levels
how to distinguish between hypothalamic and pituitary gonadotropin deficiency
pituitary capacity test, this is based on the fact that a normal pituitary will release enormous amounts of LH and FSH if it is exposed to pulsatile GnRH after being devoid of pulsatile GnRH for some days
WHO II normogonadotropic normo-oestrogenic anovulation (PCOS)
- 80% of anovulatory patients present with normal serum FSH and oestradiol levels
- diagnosis of PCOS is made if 2 out of 3 are met: androgen excess, ovulatory dysfunction, or polycystic ovarian morphology (PCOM)
- clinical hyperandrogenism may include hirsutism, acne or androgenic alopecia
- clinical hyperandrogenism = elevated serum androgen level
- PCOM = 12 or more follicles 2-9mm in diameter and/or an ovarian volume >10ml (without a cyst or dominant follicle) in either ovary
- non-classic congenital adrenal hyperplasia (primarily 21-hydroxylase deficiency) should be excluded since it mimics PCOS
- they must be screened for abnormal TSH levels, hyperprolactinaemia as well as elevated levels of 17-hydroxy progesterone
- women with PCOS are more likely to have upper body fat distribution (clinical presentation may overlap with cushings disease → overnight dexamethasone suppression test)
- prevalent findings → insulin resistance (should be monitored), impaired glucose tolerance, gestational diabetes and type II diabetes (in particular with obesity)
- increased metabolic syndromes and dyslipidaemia
- 2-3x increased risk of endometrial cancer (most endometrial cancers are well differentiated and have a good prognosis) but not ovarian cancer and breast cancer
- at risk for psychological and behavioural disorders and reduced quality of life
- may have hyperandrogenic features
- miscarriage rates are not higher but their pregnancie are more often complicated by pregnancy-induced hypertension, preeclampsia, gestational diabetes and premature delivery
- offspring of women with PCOS seem to be at risk for developing reproductive as well as metabolic features early on in life
WHO III anovulation or POI***
monotropic rise in FSH + low levels of oestradiol (+ low AMH and inhibin B levels) → premature or primary ovarian insufficiency
commonly leads to premature menopause
typically present with primary or secondary amenorrhoea + increasing symptoms of oestrogen deficiency
others → shortening or increase in the intermenstrual cycle interval, menstrual irregularities, dysfunctional uterine bleeding, or amenorrhoea, hot flushes, mood and sleep disturbances
atrophic vaginitis may give rise to dyspateunia
may experience long term consequences of hypo-oestrogenism → osteoporosis, accelerated cardiovascular aging and neurocognitive disorders
exclude secondary causes of amenorrhoea → focus of a family history of early menopause, previous ovarian/pelvic surgery, as well as chemotherapy or radiation therapy, which may identify a cause
also check for (history of/or in them) Turner, FMR1 gene, antibodies against adrenal, thyroid and TSH receptors and ovarian tissue
If a Y chromosome is identified, the patient should be counselled regarding gonadal removal because these individuals have an increased potential for malignancy
check for reduced antral follicle count or even absent follicles in both ovaries through transabdominal (if a virgin) or transvaginal US
early menopause has been associated with increased CVD
miscarriage rates and congenital anomalies of their offspring are high (probably due to increased DNA damage in their remaining oocytes due to an accelerated aging process)
what seems to precede the phenotype of PCOS in some women
weight gain
in all women with PCOS, weight gain is associated with a deterioration of the phenotype
what is mandatory in treating PCOS
restoring normal menstrual cycles through the use of oral contraceptive pills to prevent the occurrence of endometrial cancer
OCP → suppress LH secretion → decrease in ovarian androgen production
some progestin in the pill can compete for ==5α-reductase at the level of the androgen receptor==
The oestrogenic component increases the levels of sex hormone-binding globulin, which, in turn, results in a decrease in circulating free testosterone levels==??????==
hypogonadotropic hypogonadism might result from…
defective GnRH production or from impaired gonadotropin excretion
treatment of subfertility
- start of with reaching a normal BMI (weight gain or loss) to restore a normal anabolic status
- in case of hypogonadotropic hypogonadism:
- if due to defective GnRH pulse generation → administer GnRH through a pump which delivers pulses subcutaneously every 60-90 minutes
- if due to impaired gonadotropin excretion → supply preparations that contain FSH and LH
- in case of hyperprolactinaemia → give dopaminergic drugs (eg. cabergoline, bromocriptine and quinagolide)
- if due to macroprolactinoma, the tumour volume should be reduced first before a patient can be allowed to conceive
- in case of PCOS, lifestyle correction is the 1st line treatment and then clomiphene citrate (oral anti-oestrogen) or letrozole (aromatase inhibitor)
- second line is parenteral gonadotropin therapy or laparoscopic ovarian diathermy (destruction of ovarian tissue using electro-cauterisation)
- in some cases, metformin may be used
- in vitro fertilisation may be required for women with anovulatory PCOS who do not become pregnant with ovulation induction or if there are additional fertility factors, for example tubal damage or male subfertility
- in case of POI, treatment is subpar, they show poor response to ovarian hyperstimulation protocols
- due to their dramatically diminished ovarian reserve the ovary does not respond to increasing levels of FSH because their endogenous levels have already been elevated for prolonged periods of time
- hormone replacement therapy should be initiated as soon as they develop complaints such as flushes and night sweats
treatment of irregular menstrual cycles
- \
the ultimate goal in WHO I patients is…
restoring menstrual cycles and thereby endogenous levels of oestrogens and progestogens
abnormal uterine bleeding
- = a collective name for all vaginal bleeding problems (or lack of bleeding)
- AUB and especially HMB (heavy menstrual bleeding) can be caused by abnormal blood clotting, disruption of normal hormonal regulation or uterine pathology (e.g., fibroids, polyps, adenomyosis)
- standard gynaecological examination → speculum (medical tool) and vaginal examination
- speculum examination is particularly important for dysfunctional blood loss (eg. irregular bleeding) or intermenstrual bleeding to visualise the cervix
- during examination a cervical smear and triple swabs can be obtained
- pathophysiology of AUB and especially HMB can be divided in anatomical anomalies or essential HMB
PALM-COEIN
= classification system for AUB
polyp; adenomyosis; leiomyoma/fibriods; malignancy and hyperplasia; coagulopathy; ovulatory dysfunction; endometrial; iatrogenic; and not yet classified
postmenopausal menstrual bleeding (PMB)
vaginal bleeding more than 1 year after the last menstruation
FIGO???***
how is menstrual blood loss measured
golden standard = alkaline haematin extraction but it is very time consuming and stressful (women need to collect all of their menstruation blood including all used pads or tampons)
other method → the pictorial blood assessment chart → counting the number of pads and tampons per month and then divide them by level of soiling → specificity and sensitivity of 80-90%
PBAC score of 150 points most accurately correlates with menstrual blood loss of 80ml
polyps as the cause of AUB
polyp = endometrial tissue that bulges from the endometrial layer
can cause AUB but is rarely associated with HMB
in the postmenopausal period, AUB is often caused by a polyp
adenomyosis as the cause of AUB
= when the tissue that normally lines the uterus (endometrial tissue) grows into the muscular wall of the uterus → proliferation of endometrial glands and stroma within the myometrium
the displaced tissue continues to act normally (thickening, breaking down and bleeding) during each menstrual cycle
TRANSlesional flow as opposed to the circumferential flow of fibroids
characteristic on MRI → ==thickening of the junctional zone of the uterus to more than 12 mm, either diffusely or focally==
most likely to affect adult women
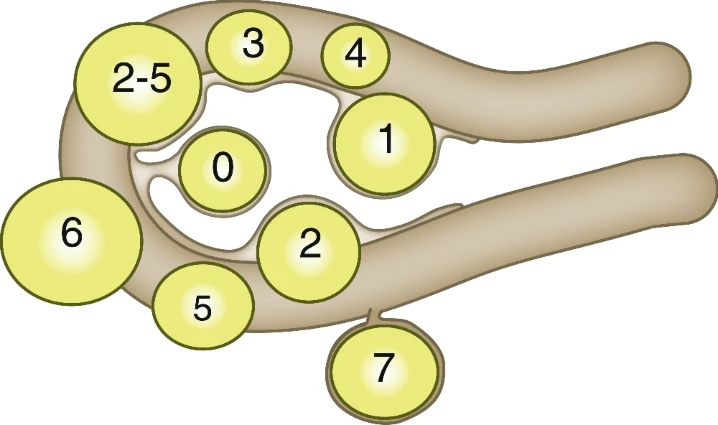
leiomyoma/fibroids as the cause of AUB
= benign muscle tumours
well defined
fibroids can be situated in an intrauterine, submucosal intramural (which means in the muscle of the uterus) or subserosal position
classified with PALM-COEIN with numbers 0-7 (FIGO classification for fibroids)
circumferential flow
type 0-2 to 5 (intracavitary or partly intracavitary fibroids) can cause AUB and HMB while 5-7 (located on the serosal side) often give bulk symptoms
there are 2 explanations as to why myomas may cause HMB
fibroids → insufficient compression of the vessels → lack of effective contraction of the uterus muscle
==WOULDNT THIS CAUSE LESS BLEEDING OUT? WONT IT STAY IN THE UTERUS IF ITS NOT CONTRACTING????????????==
fibroids → increasing intrauterine surface → more endometrial tissue → HMB
characteristic on MRI →
characteristic of leiomyosarcomas on MRI
a single large infiltrating myometrial mass with irregular and ill-defined margins
malignancy (endometrial carcinoma) as the cause of AUB
it will often cause AUB
noticed especially by postmenopausal who start having blood loss again → may have endometrial cancer or atypical hyperplasia
so postmenopausal bleeding should always be investigated
why should postmenopausal bleeding always be investigated
may be endometrial cancer or atypical hyperplasia
on the other hand, due to lack of oestrogen stimulation, endometrial tissue can be atrophic → vulnerable vessels → blood loss
iatrogenic causes of AUB
- asherman’s syndrome:
- = intrauterine adhesions or synechiae
- 2 entities → traumatic intrauterine adhesions and stenosis of the internal cervical bone (==???==)
- usually caused by global endometrial ablation, surgical hysteroscopy with resection or destruction of endometrium on purpose or unintendedly and infections such as genital tuberculosis
- adhesions → infertility, menstrual irregularities (including amenorrhea, hypomenorrhoea, or dysmenorrhoea), recurrent pregnancy losses and a history related to abnormal placentation including praevia (placenta is near the exit of the uterus) and accreta (placenta grows too deeply into the uterine wall)
- dysmenorrhoea not related to menstruation may be caused by myometrial contractions that try to evacuate blood trapped in the uterine cavity but only if the intrauterine adhesions lead to ==haematometra== (when the uterine cavity is filled with blood due to obliteration of the cervix)
- however, haematometra and dysmenorrhoea are uncommon
- niche:
- = a small defect at the site of the caesarean scar in the uterine or cervical wall
- seen on an US as a triangular anechoic area
- seen in around 60% of women after a C section
- may cause postmenstrual spotting, dyspareunia, pelvic pain and dysmenorrhoea
incarcerated gravid uterus
= a pregnant uterus that is trapped between the sacral promontory and pubic symphysis
menorrhagia des vierges
irregular heavy menstrual women in young women just after their menarche due to anovulatory cycles
due to immature hypothalamus-hypophysis-ovarian axis which causes anovulatory menstruation with sometimes very long, heavy menstrual bleeding due to ==oestrogen only stimulation of the endometrium (as opposed to what?)==
if the bleeding continues, a clotting disorder may be the underlying cause
perimenopausal phase starts with…
irregular menstruation
a history of … is 2x as common among women with symptoms of dysmenorrhoea, HMB, and sexual dysfunction as compared with women without such complaints
sexual assault
imaging for AUB
- transvaginal US
- saline/gel infusion sonography
- hysteroscopy
- MRI
transvaginal US
- transabdominal if a virgin
- must be performed carefully in elderly women (= postmenopausal) due to their hypo-oestrogenic state which can result in vulnerable atrophic vaginal epithelium
- the size of the uterus usually enlarges after pregnancy and stays that way, other reasons for an enlarged uterus may be focal or diffuse myometrial pathology such as fibroids or adenomyosis
myometrium
the muscular layer of the wall of the uterus and consists of smooth muscles which run horizontally, vertically, and diagonally
made of 2 layers:
- the inner part = junctional zone
- outer part
endometrium
consists of a functional layer and a basal layer
the functional layer undergoes cyclic regeneration influenced by hormones during the fertile period
it should not proliferate in postmenopausal women
has a typical 3 layer appearance with a central hyperechoic line surrounded by 2 hypoechoic layers during the ==periovulatory phase==
==how is it a 3 layer appearance if its 2 layered???==
a thickened endometrium can represent a highly proliferative endometrium but can also mask the presence of an endometrial polyp
fibroids and leiomyosarcomas may be hard to differentiate, what points away from a fibroid
a large ( ≥ 8 cm), solitary, oval-shaped, highly vascularized and irregular, heterogeneous myometrial tumour with central necrosis/degenerative cystic changes and absence of calcifications must raise the suspicion of a leiomyosarcoma
ill defined myometrial pathology is suspicious for…
adenomyosis
saline/gel infusion sonography
- = when the uterine cavity is infused with saline or gel during US
- may cause some cramping or bleeding
- highly sensitive so if no suspicious intracavitary structures are seen, more invasive diagnostic procedures dont need to be done
hysteroscopy
- provides direct visualisation of the uterine cavity by endoscopy with access through the cervix
- inserted transvaginally through the cervix into the uterus
- saline (NaCl) or a sugar solution (sorbitol) is used to distend the uterus and obtain visualisation of the uterine cavity
treatment of abnormal menstrual bleeding
non hormonal therapy:
- mainly suitable for HMB
- tranexamic acid:
- an antifibrinolytic drug → binds to plasminogen or plasmin → stops plasmin from binding to and degrading fibrin
- used on the heavy bleeding days for max 4–5 days
- very effective, 50% reduction in blood loss
- NSAIDs:
- reduces blood flow by 30%
- also treats dysmenorrhoea which is often present with HMB
hormonal therapy:
- combined oral contraceptives:
- can reduce blood loss by 35%
- contain synthetic oestrogens (ethinylestradiol) with levonorgestrel
- least chance of venous thrombosis
- intermittent use with a 4-7 days
- progesterone-only contraceptives:
- levonorgestrel releasing intra uterine device:
- diminishes blood loss by 70%
- can be left in situ for up to 5 years
- gonadotropin releasing hormone agonist:
- initially stimulates the pituitary gland to release LH and FSH = flare effect → eventually decrease due to receptor downregulation
- monthly, 3 times, injections
- stop menstrual bleeding (completely) in 90%
- uterine fibroids shrink typically by 40 % and adenomyosis decreases in volume
- symptoms recur after stopping treatment
- due to the hypo-oestrogenic state, the risk of heart disease and osteoporosis is increased
- ulipristal acetate:
- pre-treatment before surgery for uterine fibroids
- once daily for 12 weeks
- stops menstrual blood loss in most cases
- less side effects than ^ because oestrogen levels are maintained at mid follicular levels + more uterine volume reduction
- combined oral contraceptives:
surgical therapy
surgical therapy of AUB in a normal uterus
- endometrium ablation techniques:
- = destruction of the endometrium (by heat? or radiofrequency?) including the basal endometrial lining → no new endometrium is formed → absence of menstrual blood loss
- 1st gen = retroscopic, was hysteroscopic assisted, 2nd gen is performed without hysteroscopy
- 2nd gen has better results (amenorrhoea rates of 40% compared to 30%)
- successful in at least 75-85%
- hysterectomy:
- most effective treatment for AUB since no uterus means no bleeding by definition but it is not usually first line (?)
- performed vaginally (advantage → no visible scars), laparoscopically or by laparotomy
- intra-abdominal adhesions, an enlarged uterus or insufficient descent of the uterus are contraindications for a vaginal approach
- laparoscopic and laparotomic hysterectomies can be performed with and without removal of the cervix
what is the best treatment for AUB
hysterectomy
surgical therapy for uterine fibroids
fibroids may cause HMB, dysmenorrhoea and pressure on surrounding organs
- hysteroscopic removal:
- usually for submucosal fibroids (types 0, 1 and 2)
- NaCl is used as distention fluid, ==somehow causes a risk of NaCl fluid loss???==
- abdominal myomectomy (laparoscopy/tomy):
- usually for intramural or subserosal fibroids
- laparotomy is for bigger lesions
- if the fibroids are located transmurally (types 2-5) → caesarean section (?)
- uterine artery embolisation:
- catheter is inserted through the femoral artery towards the uterine artery → small particles are injected until the vessels supplying the fibroids are blocked → necrosis
- 75% dont require another procedure after 5 years
- there is some evidence that ovarian damage can occur after so it is not recommended for women who still want to conceive → myomectomy is done instead
- hysterectomy
surgical therapy for adenomyosis
since adenomyosis does not have an anatomical cleavage plane (the endometrial islands invade the myometrium instead of forming a capsule as with fibroids) surgical removal is very difficult and with a high chance of complications
- hysterectomy (when conservative treatment fails)
- uterine artery embolisation
- minimally invasive alternative to hysterectomy
adenomyosis may be associated with
endometriosis
surgical therapy for uterine niches
- hysteroscopic removal if >2.5mm
- laparoscopic removal if <2.5mm
surgical therapy for endometrial polyps
mostly hysteroscopy
surgical therapy for Asherman’s syndrome
hysteroscopy is the method of choice for diagnosis and treatment