gastrointestinal system minor conditions
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
55 Terms
GI anatomy?
mouth
pharynx
oesophagus - upper and lower sphincters
stomach
liver, gallbladder, pancreas
small intestine (duodenum, jejunum, ileum)
large intestine (ascending, transverse, descending, sigmoid)
rectum
anus
what does the GI system do in depth?
A muscular tube that transports food/fluids from the mouth to the stomach. Peristalsis propels food/fluids along the oesophagus. Starts at the cricoid cartilage, runs behind the heart and trachea down through the diaphragm (hiatus) to the stomach. The upper gastro-oesophageal sphincter prevents entry of air into the oesophagus. The lower gastro-oesophageal sphincter prevents gastric acid entering the oesophagus
what is pharmacy first?
NHS Pharmacy First Scotland is a service designed to make it easier for people to access healthcare for minor illnesses and common conditions directly through their local community pharmacy, without needing to see a GP.
what are symptoms arising from the upper GI tract which are typically present for four or more weeks?
upper abdominal pain/discomfort, heartburn, acid reflux, nausea and/or vomiting
(it may be caused by non-ulcer dyspepsia, GORD, PUD or a hiatus hernia
what are red flag/ alarm symptoms with dyspepsia?
age > 55yrs
unexplained weight loss
blood in vomit or stools
dysphagia
anaemia
potential cardiac cause - pain related to exercise, sweating, breathlessness, grey pallor
what are non- pharmacological management options for dyspepsia?
reduce weight if overweight or obese
avoid trigger foods e.g. coffee, chocolate, tomatoes, fatty or spicy foods
eat smaller meals and last meal 3-4 hours before bed
stop smoking
reduce alcohol use to recommended limits
reduce stress
(review medications: aspirin, bisphosphonates, calcium-channel blockers, corticosteroids, nitrates, NSAIDs, nicorandil, theophylline)
before recommending OTC dyspepsia treatments, it is important to ask patients about ?
the frequency of their symptoms, and whether they have already tried OTC antacids and/or alginates
when are antacids and alginates best taken?
when symptoms occur or are expected, usually between meals and at bedtime
(some medicines contain both alginate and antacid)
are liquid or tablet products more effective in dyspepsia treatment?
liquid products are more effective
what should i do if heartburn occurs at least twice a week for at least four weeks?
try an over-the-counter proton pump inhibitor (PPI) for 14 days to help reduce the production of stomach acid
what do antacids do and how do they work?
neutralise gastric acid, increasing gastric pH
typically contain magnesium salts or aluminium salts
-magnesium can cause diarrhoea
-aluminium can cause constipation
therefore combined formulations are used to balance side effects
examples of antacids?
rennies
tums
maalox/ maalox plus (contains simeticone, an antifoaming agent that helps relieve bloating)
what is the mechanism of action for alginate containing antacids?
increase viscosity and adherence of gastric mucus
form a ‘raft’ that floats on top of gastric contents
this barrier prevents reflux into the oesophagus
examples of alginate- containing antacids?
gaviscon Advance
peptac
take after meals and at bedtime
why must you consider electrolyte content when giving antacids and alginates to certain patients?
sodium/potassium content may affect patients with: hypertension, heart failure, renal impairment
why must you consider the effect on gastric pH when giving antacids and alginates to certain patients?
may alter absorption of other medications
why must you consider the chelation and interaction risks when giving antacids and alginates to certain patients?
antacids can bind to or reduce absorption of iron, levothyroxine, doxycycline, bisphosphonates, enteric-coated (EC) formulations, ACE inhibitors (less commonly affected but still worth noting)
how long should you space antacids treatment when taking other medications?
space antacids 2 hours apart from interacting medications to avoid reduced efficacy
what do proton pump inhibitors (ppi) do?
reduce stomach acid by blocking the H+/K+ ATPase enzyme in gastric parietal cells
what are PPIs used to treat?
frequent heartburn, acid reflux and dyspepsia
what are common OTC PPIs ?
nexium control 20mg GR tablet/capsule (18yrs+, 1 daily, max 14 days)
pyrocalm control 20mg GR tablet (Adults, 1 daily, max 14 days)
what are indications of PPIs?
frequent heartburn ( 2 days/ week)
mild to moderate GORD
short term relief of acid related symptoms
what safety and use advice should you give a patient when counselling PPIs?
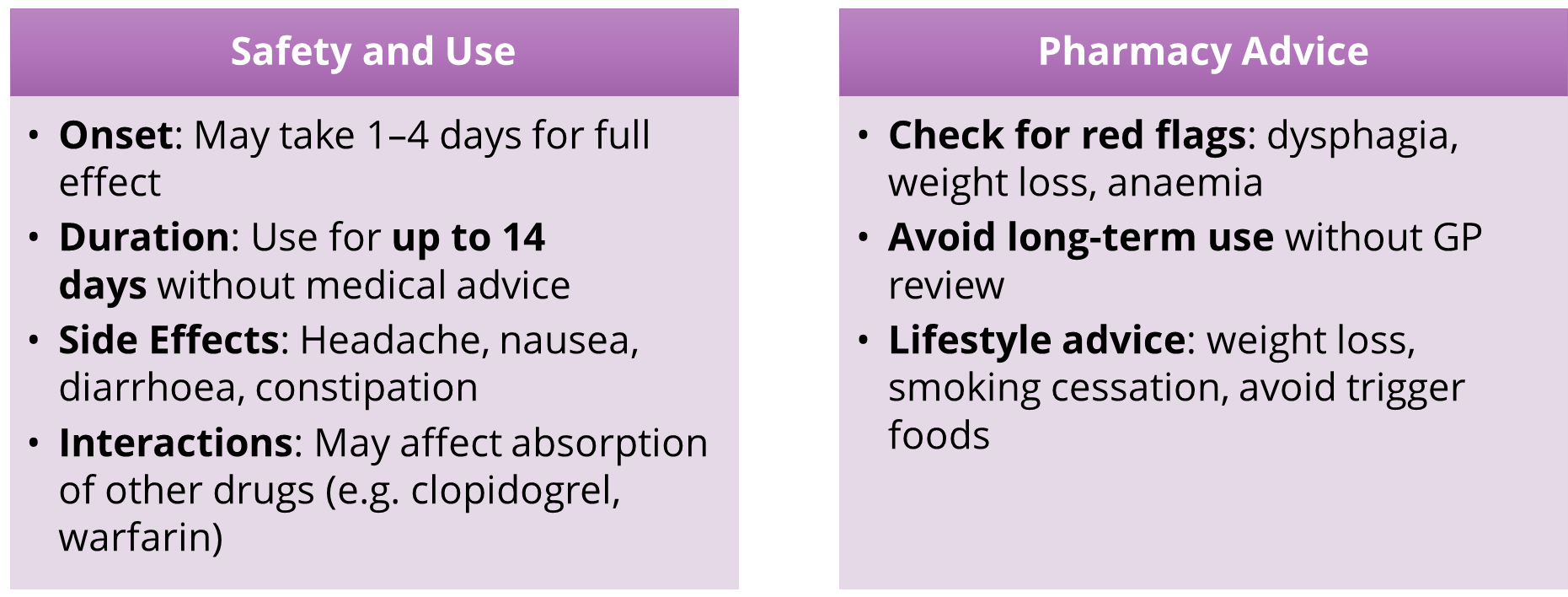
gastric parietal cell secretes H+ into the stomach using a?
H/K/ATPase pump (proton pump)
(stimulating factors: histamine, acetylcholine, gastrin)
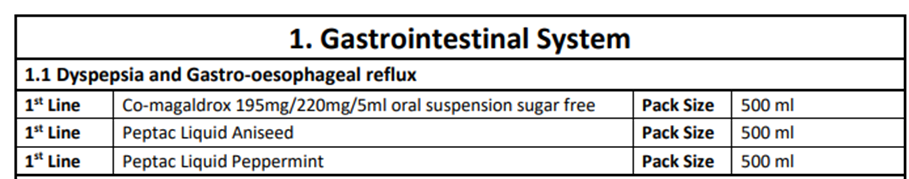
what are the medicines on gastrointestinal system (dyspepsia and gastro-oesophageal reflux) pharmacy first approved list?
what is dyspepsia ?
a medical condition that causes persistent pain or discomfort in the upper abdomen
what is GORD (gastro oesophageal reflux disease)?
is a medical condition that causes stomach contents to reflux up into the oesophagus towards the mouth
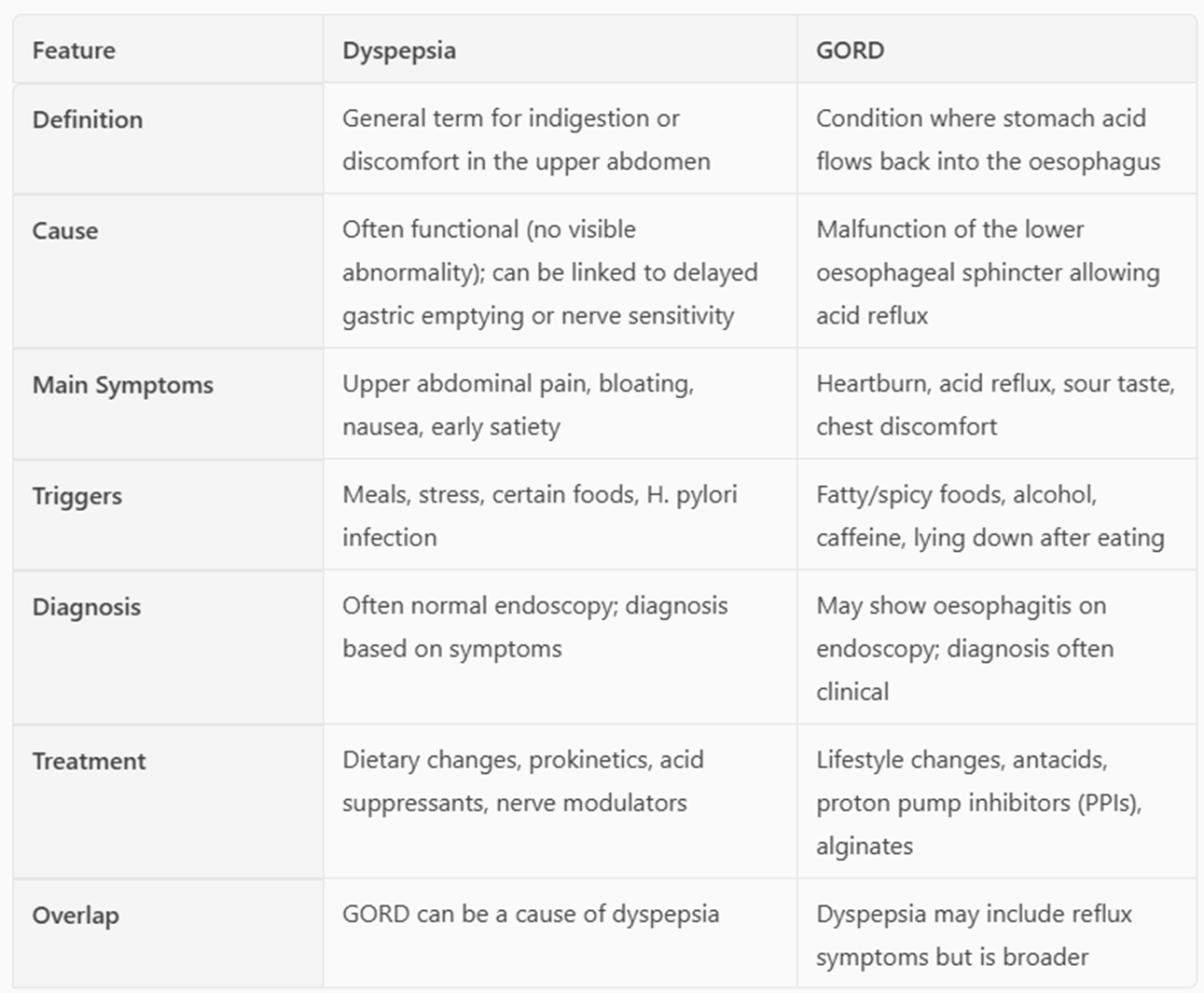
GORD vs dyspepsia?
GORD and dyspepsia are two common digestive conditions occurring in the GI tract
the term ‘dyspepsia’ indicates there is an underlying disease of the upper digestive tract rather than a specific diagnosis
underlying causes of dyspepsia include gastro-oesophageal reflux disease (GORD), peptic ulcer disease, Barrett’s oesophagus and upper gastrointestinal cancers
GORD vs dyspepsia table…
GORD is the chronic reflux of gastric contents (hydrochloric acid and pepsin) from the stomach into the oesophagus, this leads to?
oesophageal irritation and the symptoms of heartburn
GORD typical symptoms, atypical symptoms and alarm symptoms?
Typical symptoms:
•Heartburn/dyspepsia
•Epigastric/retrosternal burning sensation
•Regurgitation (water brash/acid brash/vomiting)
•Belching
•May be precipitated by bending over, eating too much or lying down
Atypical symptoms:
•Cough
•Laryngitis
•Severe chest pain – think cardiac!
Alarm symptoms
weight loss
difficulty swallowing
blood in vomit
abdominal mass
age 55 +
GORD
gastric acid exits the stomach entering the lower oesophagus causing?
irritation
inflammation
erosion of the oesophageal mucosa
GORD epidemiology?
prevalence increases with age
more common in women
20% of those with dyspepsia symptoms who have endoscopy will have GORD
Aetiology ( causes and origins) of GORD?
obesity- increased abdominal pressure
smoking
diet (coffee, mints dietary fat, onion, citrus fruit, tomatoes, alcohol
medication (calcium channel blockers theophylline nitrates, anticholinergics, bisphosphonates)
pregnancy (up to 50% of pregnant women will experience GORD)
structural: hiatus hernia, occurs in 30% of the population 50 years +
GORD treatment?
normally PPI for 4-8 weeks- this is prescribed as a POM
lifestyle advice
whwhat is diarrhoea ?
Diarrhoea is passing three or more loose or watery stools per day, affecting hydration and health
what are the different classifications of diarrhoea?
acute
persistent
chronic
based on symptom duration
what are infectious agents that commonly cause diarrhoea?
bacteria
viruses
parasites
e.g. stomach bug r food poisoning
what are non-infectious agents that commonly cause diarrhoea?
medications
IBS
malabsorption
inflammatory bowel disease
what to do/ lifestyle advice when dealing with diarrhoea?
stay at home and get plenty of rest
drink lots of fluids such as water or squash - take small sips if you feel sick
carry on breast or bottle feeding your baby - if they’re being sick, try giving them small feeds more often than usual
give babies on formula or solid foods small sips of water between feeds
eat when you feel able to - it may help to avoid foods that are fatty or spicy
take paracetamol for discomfort - (check the leaflet before giving it to a child)
what NOT to do/ lifestyle advice when dealing with diarrhoea?
do not have fruit juice or fizzy drinks - they can make diarrhoea worse
do not make baby formula weaker - use it at its normal strength
do not give children under 12 medicine to stop diarrhoea
do not give aspirin to children under 16
how to counsel for diarrhoea?
in adults and children:
-diarrhoea usually stops within 5 -7 days
-vomiting usually stops in 1 or 2 days
stay off school or work until you have not been sick or had diarrhoea for at least 2 days
hygiene measure are very important to stop spread
alarm symptoms: severe and frequent vomiting, diarrhoea > 7 days or vomiting > 2 days, dehydration signs in child younger than 5, bleeding from rectal area, coloured vomit, sudden and severe headache/ stomachache
diarrhoea pharmacy first approve list treatment?
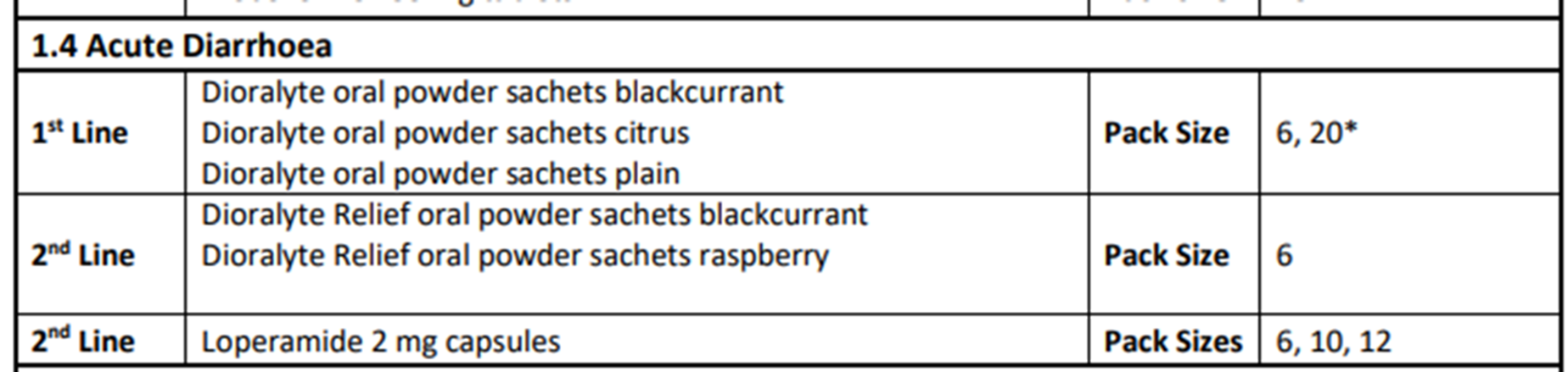
diarrhoea treatment ?
•Rehydration sachets e.g. DioralyteÒ
•Powder form, typically in sachets. Mix the contents with water to create a drink that helps replenish fluids and electrolytes lost during diarrhoea.
•Improves absorption of water and salts in the intestines thanks to the glucose and rice starch content
•Each sachet contains:
•Sodium chloride, Potassium chloride, Disodium hydrogen citrate, Glucose
•Some versions (like Dioralyte Relief) also include rice starch, which helps firm up stool
rehydration sachets?
•Adults and children over 3 months can safely use rehydration sachets.
•For infants under 1 year, medical advice is recommended before use.
•It's suitable for use during travel, illness, or after exercise when dehydration is a risk
•Mix one sachet with 200 ml of fresh drinking water (boiled and cooled for infants).Take after each loose stool.
•Use immediately after mixing. If refrigerated, it can be stored for up to 24 hours.
•Not a cure for diarrhoea – manages dehydration
diarrhoea treatment - loperamide (antimotility agent)?
opiate receptor agonist that stimulates opiate receptors in the GI tract
Reduction of motility. More water is absorbed from faeces
Does not cross the blood-brain barrier (at normal doses)
Extensive first pass metabolism
Licensed OTC dose is up to a max of 6 capsules in 24 hours
Licensed POM dose is higher
Brand names e.g. Imodium
constipation symptoms?
You have fewer than three bowel movements per week
Your stools are hard, dry, lumpy, or unusually large/small
You experience straining, pain, or a feeling of incomplete emptying
You feel bloated, nauseous, or have stomach aches
common causes of constipation?
Low fibre intake (not enough fruits, vegetables, or whole grains)
Dehydration (not drinking enough fluids)
Lack of physical activity
Ignoring the urge to go to the toilet
Changes in routine, diet, or travel
Side effects of medications (e.g. opioids, iron supplements, antidepressants)
Stress, anxiety, or depression
Pregnancy or ageing
Medical conditions like IBS, Parkinson’s disease, or diabetes
when to consult a GP if experiencing constipation?
Constipation lasts more than 2 weeks
You notice rectal bleeding
You experience unexplained weight loss or fatigue
You have persistent abdominal pain
You suspect a medication is causing the issue
lifestyle treatment and prevention of constipation?
diet
eat high fibre foods: whole grains, fruits (especially apples, apricots, grapes) vegetables, nuts and seed
drink 1.5-2 litres of fluid daily
avoid excessive caffeine and alcohol
toilet habits
respond promptly to the urge to go
sit with knees above hips (use a footstool if needed)
physical activity
regular movement like walking or light exercise helps stimulate bowel function
medication treatment and prevention?
If lifestyle changes don’t help, laxatives may be recommended by a pharmacist. These include:
-Bulk-forming laxatives (e.g. ispaghula husk)
-Osmotic laxatives (e.g. lactulose)
-Stimulant laxatives (e.g. senna)
-Softening laxatives (e.g. docusate)
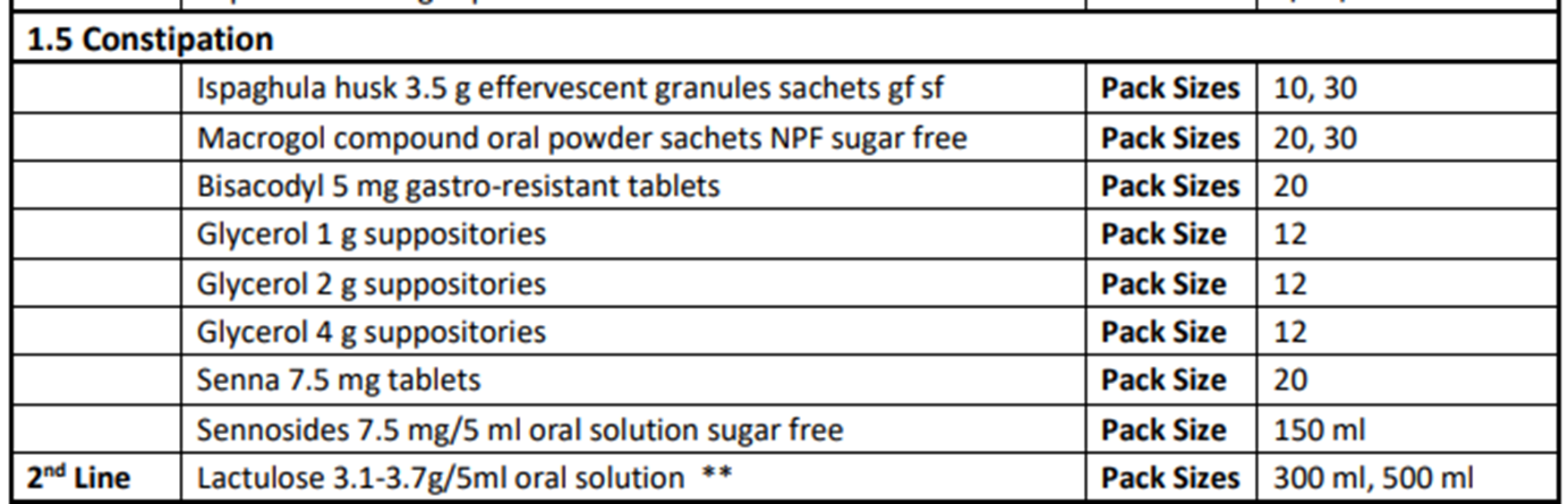
bulk forming laxatives?
•Bulk forming laxatives
Contains soluble fibre ispaghula husk – Retains fluid in the faeces
Important to have good fluid intake, otherwise can be constipating
Not recommended in persons taking constipating medication – risk of further constipation
Takes 2 or 3 days to have an effect
(fybogel, ispaghula husk orange)
osmotic laxatives?
•Draws water into the faeces due to osmosis – must be alongside a good fluid intake!
•Glycerol suppositories, also has a mild irritant effect on the bowel promoting peristalsis
•Can be used if there is an inadequate response to bulk forming laxatives
•Orally can takes 1 or 2 days to have an effect, glycerol suppositories have a rapid onset of action within 15 - 30 minutes
(laxido, movicol, glycerol suppositories, lactulose)
stimulant laxatives?
•Cause direct stimulation of the bowel leading to increased colonic motility
•Can cause cramping abdominal pain so potentially limited value in IBS
•Can be used in conjunction if inadequate response to bulk forming/osmotic laxatives or if constipation exacerbated by medication (e.g. opiates)
•Orally they can take 6 - 12 hours to have an effect, bisacodyl suppositories will take 10 to 45 minutes to have an effect.
(senna , bisacodyl, dulcolax)
softening laxatives?
•Docusate has a lubricating/stool softening action in addition to being a stimulant
•Docusate is a wetting agent lowering the surface tension and allowing water and salt to penetrate accumulated hard dry faeces in the bowel
•Orally docusate can take 1-3 days to have an effect.
( docusate sodium)