Glycogen (Breakdown) and Glucose Homeostasis II
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
Glycogen Breakdown Requires _____ Enzyme Activities
Four
What are the 4 enzyme activities needed for glycogen breakdown
1) Glycogen Phosphorylase → phosphorolysis
2) debranching enzyme/ alpha-1,6-glucosidase
3) transferase
4)phosphoglucomutase
Phosphorylase a aka _______ is an active enzyme that initiates.......and leads to _____
Glycogen Phosphorylase; the breakdown of glycogen; phosphorolysis
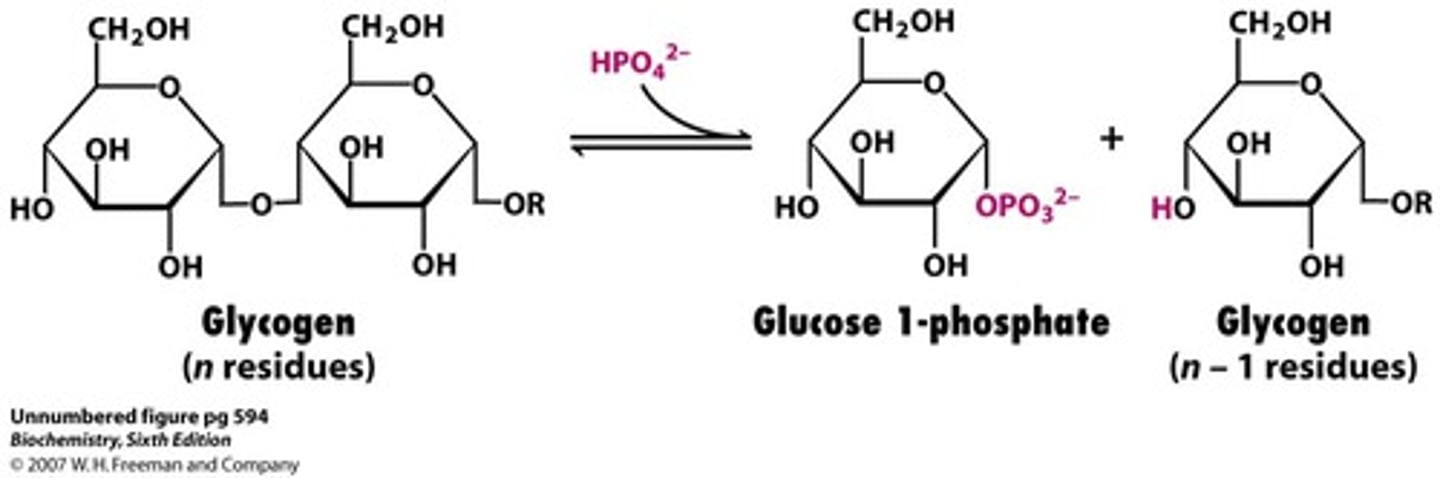
What is phosphorolysis?
Unusual non-hydrolytic cleavage requiring inorganic phosphate
What two enzymes are required to remodel glycogen to allow more breakdown to coutinue?
debranching enzyme/ alpha-1,6-glucosidase
& transferase
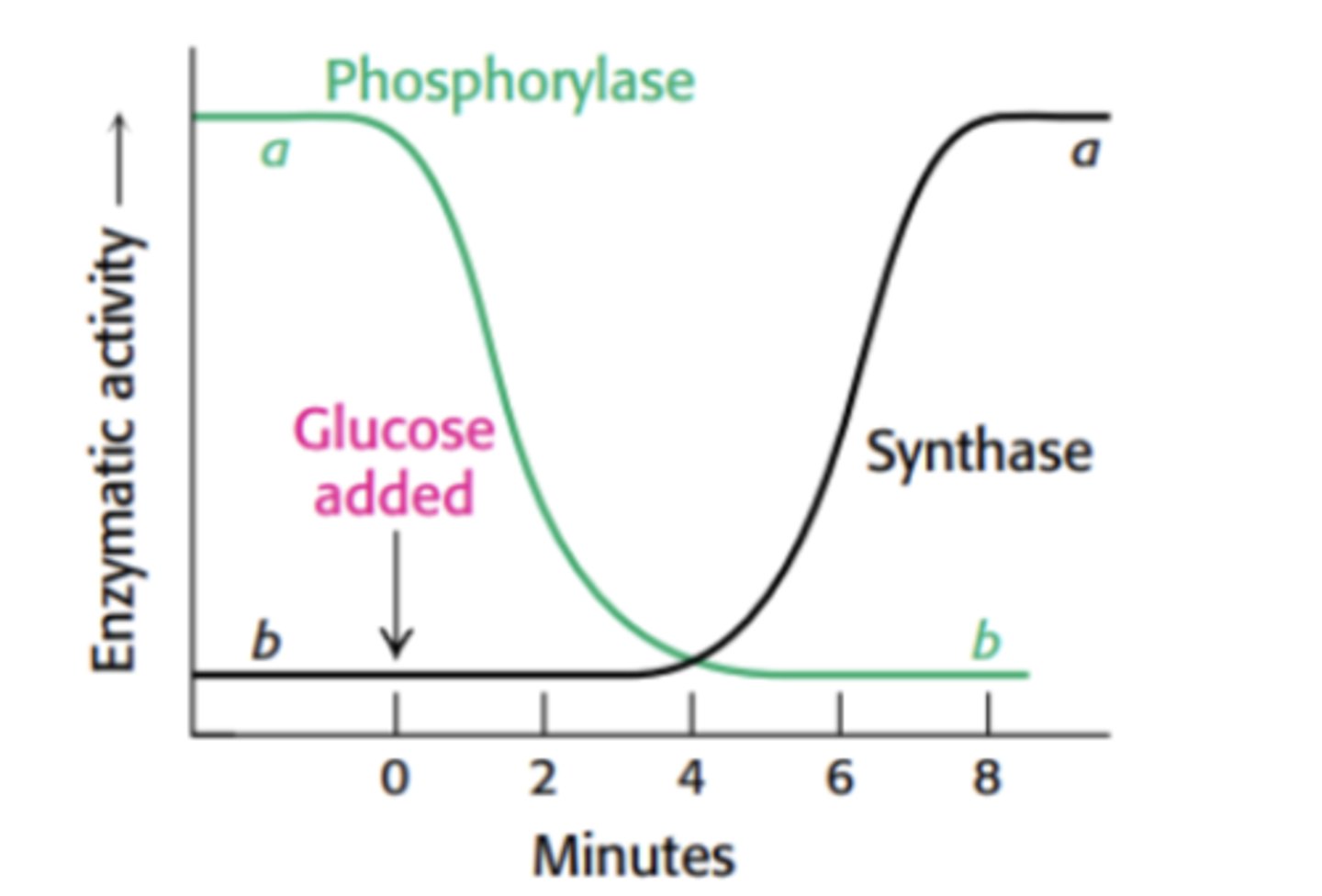
Glycogen Phosphorylase breaks.....
alpha-1,4 glycosidic bond
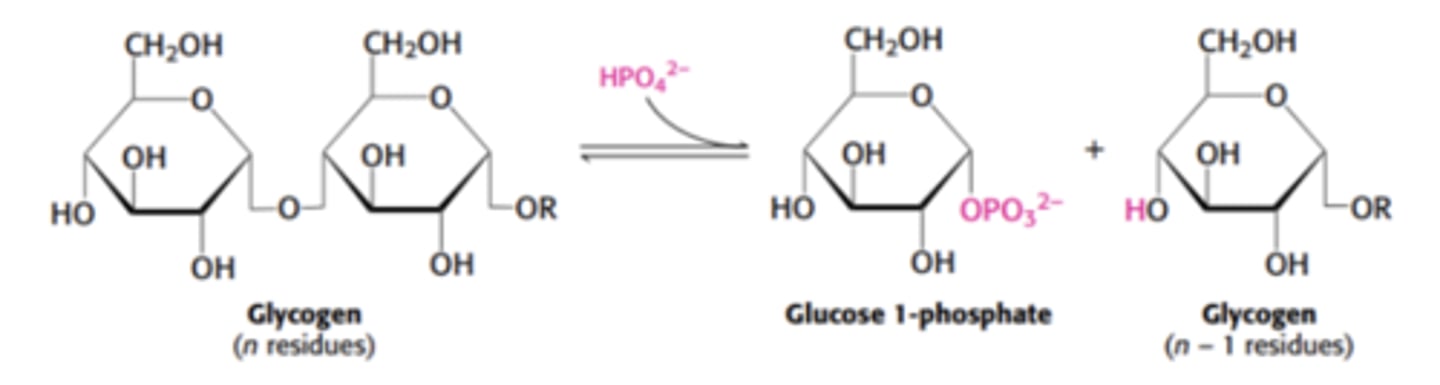
Debranching Enzyme (aka _______) breaks....through _____ cleavage
alpha-1,6-glucosidase; alpha-1,6 glycosidic bond; hydrolytic (uses h2o)
Explain the process of glycogenolysis
glycogen --> glycogen phosphorylase --> glucose-1-phosphate--> phosphoglucomutase --> glucose-6-phosphate

What is the fate of glucose 6-phosphate in muscle?
In muscle, glucose 6-phosphate is used as fuel for anaerobic or aerobic metabolism.
What is the role of glucose 6-phosphate in the liver?
In the liver, glucose 6-phosphate can be converted into free glucose and released into the blood.
What enzyme is involved in glycogen breakdown (glycogenolysis) to produce glucose 6-phosphate?
Glycogen phosphorylase and phosphoglucomutase are involved in converting glycogen to glucose 6-phosphate.
Why is glucose 6-phosphatase considered an "anti-hexokinase"?
Glucose 6-phosphatase allows the liver to secrete glucose derived from glycogenolysis, countering the effect of hexokinase, which traps glucose inside cells.
Is glucose 6-phosphatase expressed in muscle? Why or why not?
No, glucose 6-phosphatase is not expressed in muscle, as muscle does not release glucose into the blood.
What are the primary products of glycolysis in muscle and brain tissues?
In muscle and brain, glycolysis primarily produces pyruvate, lactate, CO₂, and H₂O.
What hormones are involved in co-regulating glycogen metabolism during exercise or fasting?
Glucagon (in the liver) and epinephrine (in muscle and liver).
What enzyme is activated by cyclic AMP (cAMP) in response to glucagon or epinephrine signaling?
Protein kinase A is activated by cAMP.
How is glycogen synthase regulated during exercise or fasting?
Glycogen synthase is deactivated by phosphorylation.
What is the role of phosphorylase kinase in glycogen metabolism?
Phosphorylase kinase activates phosphorylase by phosphorylating it, which promotes glycogen breakdown.
How does phosphorylation affect glycogen synthase and phosphorylase?
Phosphorylation deactivates glycogen synthase and activates phosphorylase.
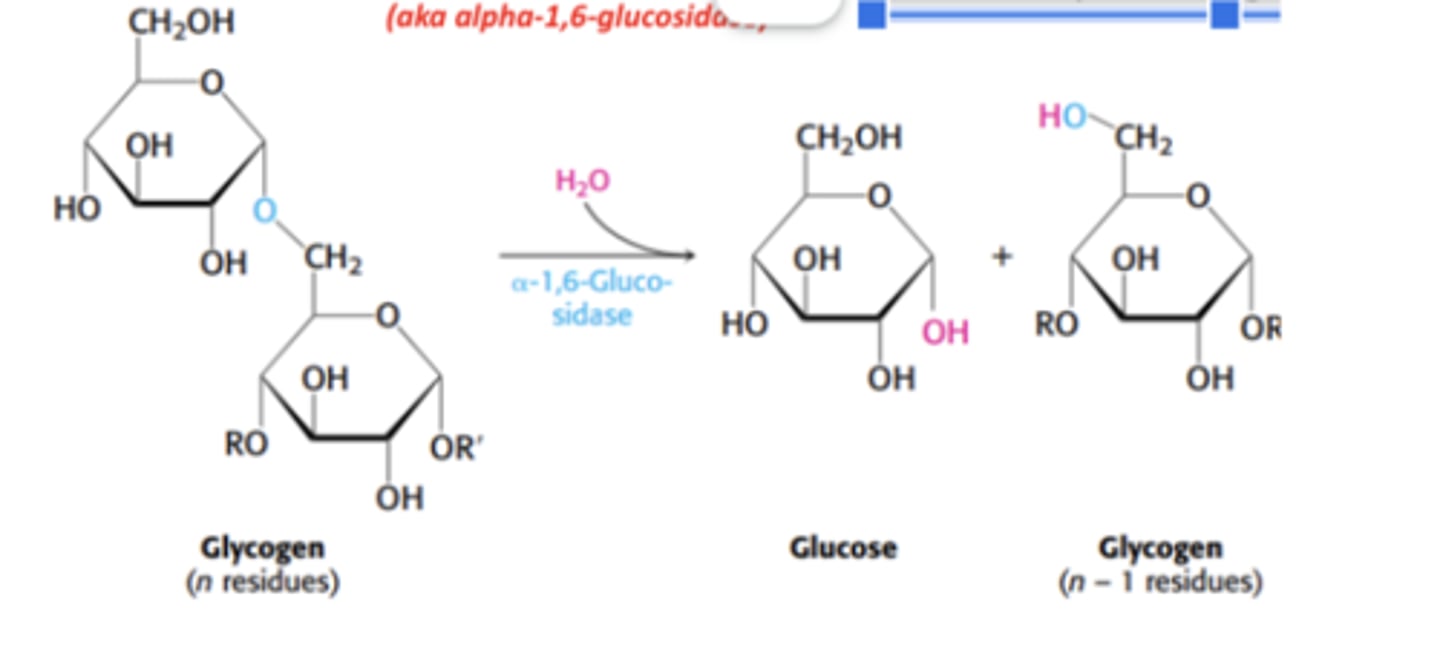
According to the enzymatic activity graph, what happens to phosphorylase activity when glucose is added?
Phosphorylase activity decreases after glucose is added.
What happens to glycogen synthase activity after glucose addition, according to the graph?
Glycogen synthase activity increases after glucose is added, reversing the effect within minutes.
What is the role of Protein Phosphatase 1 (PP1) in glycogen metabolism?
PP1 is responsible for rapid reversal of phosphorylation, turning glycogen phosphorylase OFF and glycogen synthase ON.
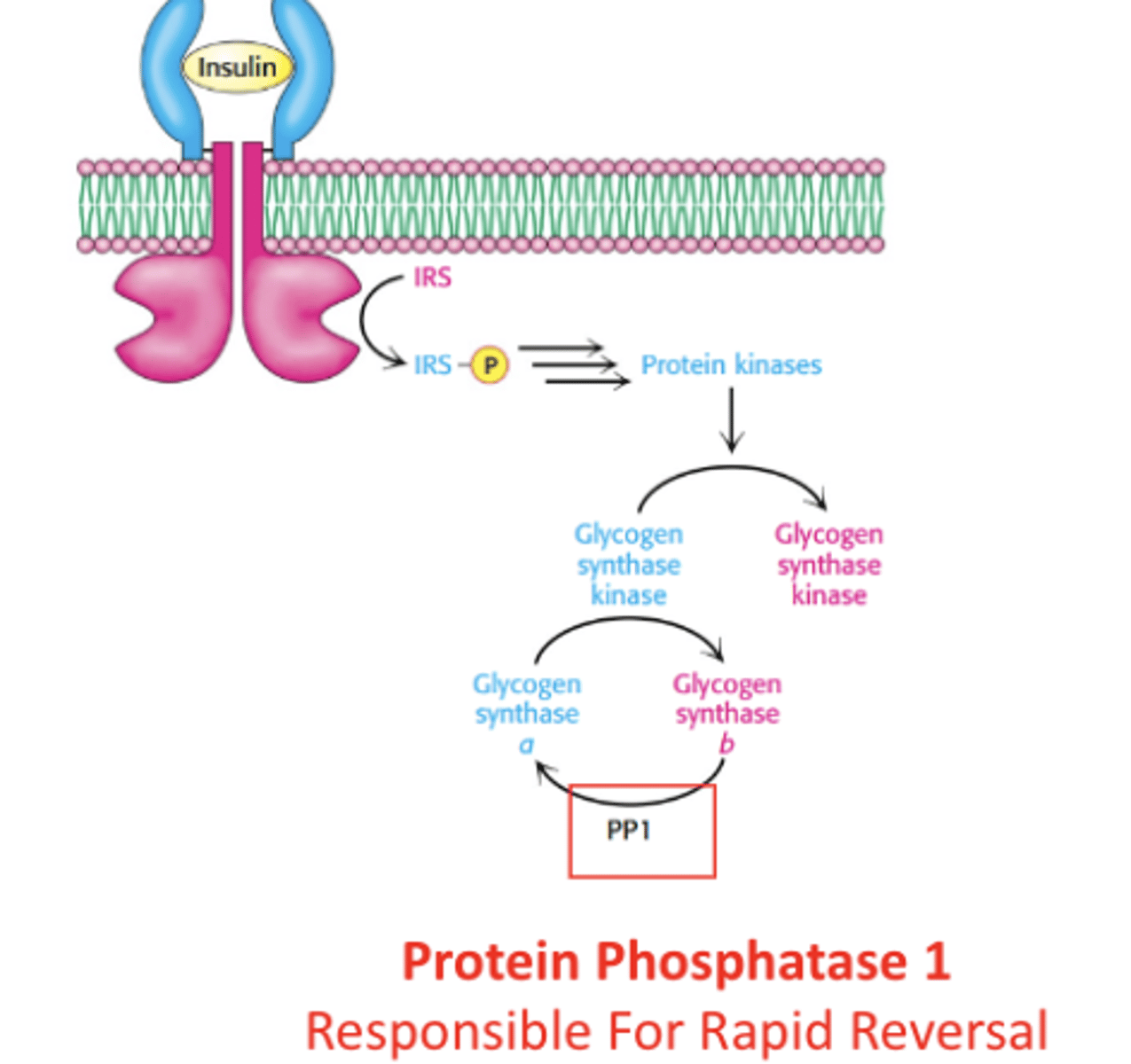
How does insulin influence glycogen metabolism after a meal or rest?
triggers the synthesis of glycogen
How do PP1 and Protein Kinase A (PKA) act in glycogen regulation?
PP1 and PKA push in opposite regulatory directions: PP1 promotes glycogen synthesis, while PKA promotes glycogen breakdown.
How quickly can the actions of PP1 and PKA be affected by hormones?
The actions of PP1 and PKA can be affected rapidly by hormones, leading to quick shifts in glycogen metabolism.
What happens to glycogen breakdown and synthesis after PP1 activation?
Glycogen breakdown is inhibited, and glycogen synthesis is stimulated after PP1 activation.
What is Glucagon-Like Peptide 1 (GLP-1) and where is it produced?
GLP-1 is a peptide with a similar amino-acid sequence to glucagon but different systemic effects.
It is produced and secreted by intestinal enteroendocrine L-cells and certain neurons in the nucleus of the solitary tract in the brainstem upon food consumption.
How does GLP-1 affect blood sugar?
GLP-1 decreases blood sugar levels independent of insulin.
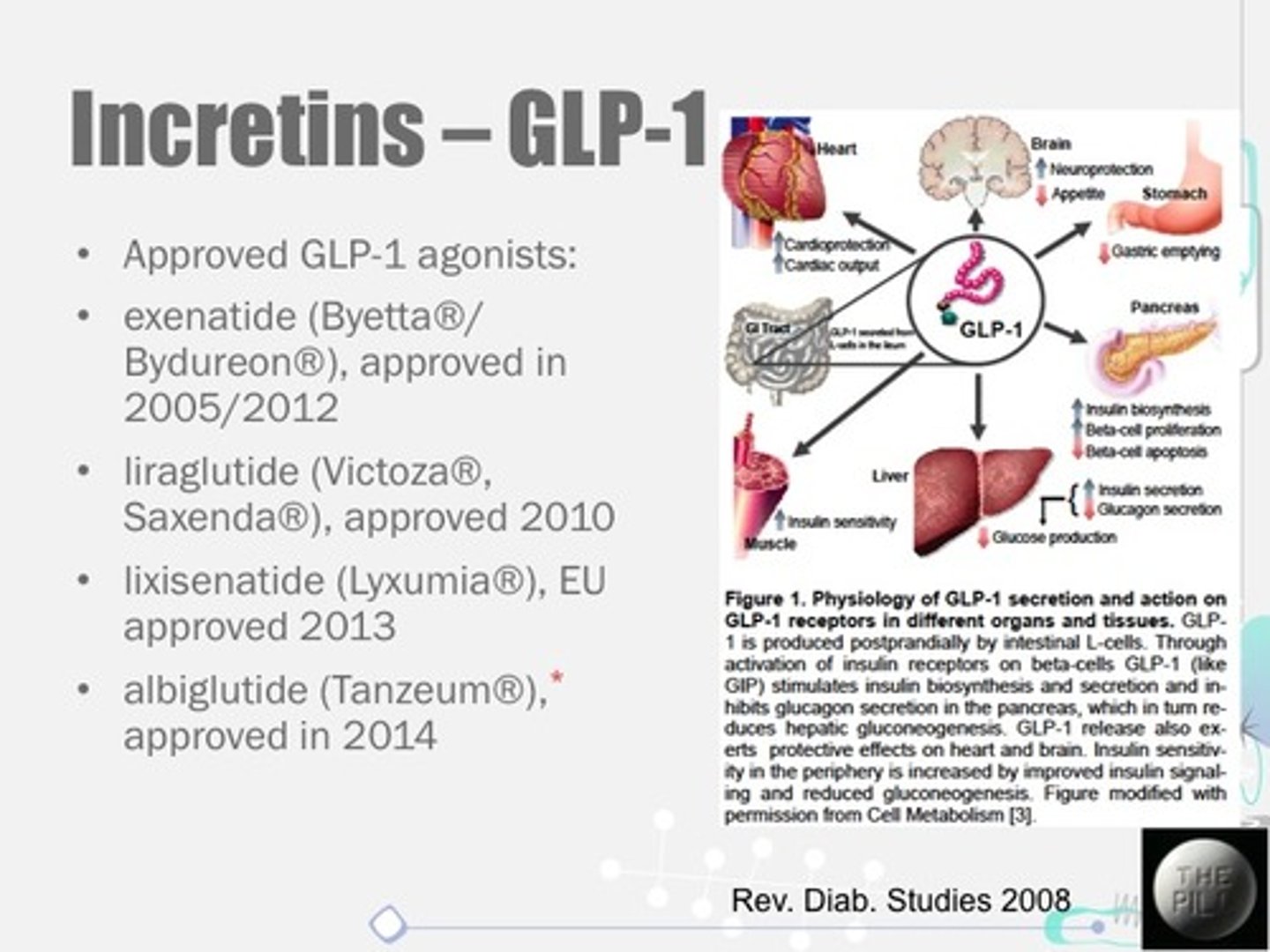
What are GLP-1 agonists, and how do they work?
GLP-1 agonists activate the GLP-1 receptor, slowing gastric emptying, inhibiting glucagon release, and stimulating insulin production.
What conditions are GLP-1 agonists used to treat?
Initially developed for type 2 diabetes control, GLP-1 agonists are now also used for obesity management.

What enzyme deficiency is associated with Von Gierke disease (Type I), and what organs are affected?
Von Gierke disease is due to a deficiency in glucose 6-phosphatase or a transport system, affecting the liver and kidneys.
What happens to glycogen structure in the affected organ in Von Gierke disease?
increased amount; normal structure
What are the clinical features of Von Gierke disease (Type I)?
Massive liver enlargement, failure to thrive, severe hypoglycemia, ketosis, hyperuricemia, and hyperlipemia.
What enzyme deficiency causes Pompe disease (Type II), and which organs are impacted?
Pompe disease is caused by a deficiency in α-1,4-glucosidase (lysosomal), affecting all organs.
What happens to glycogen structure in the affected organ in Pompe disease?
Massive increase in glycogen in all organs with normal structure;
What are the clinical features of Pompe disease (Type II)?
cardiorespiratory failure often leads to death, usually before age 2.
What enzyme deficiency is associated with Cori disease (Type III), and what is affected?
Cori disease is due to a deficiency in α-1,6-glucosidase (debranching enzyme), primarily affecting muscle and liver.
What happens to glycogen structure in the affected organ in cori disease?
Increased glycogen in muscle and liver with short outer branches
what are the clinical features of Cori disease (Type III)?
similar to Type I but with a milder course.
What enzyme deficiency causes McArdle disease (Type V)?
McArdle disease is caused by a deficiency in the enzyme phosphorylase in muscle tissue.
How does McArdle disease affect glycogen in muscle?
In McArdle disease, glycogen is moderately increased in muscle tissue but has a normal structure.
What are the main clinical features of McArdle disease?
Limited ability to perform strenuous exercise due to painful muscle cramps; otherwise, patients are generally normal and well-developed.