Hormonal Control of Calcium Homeostasis
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
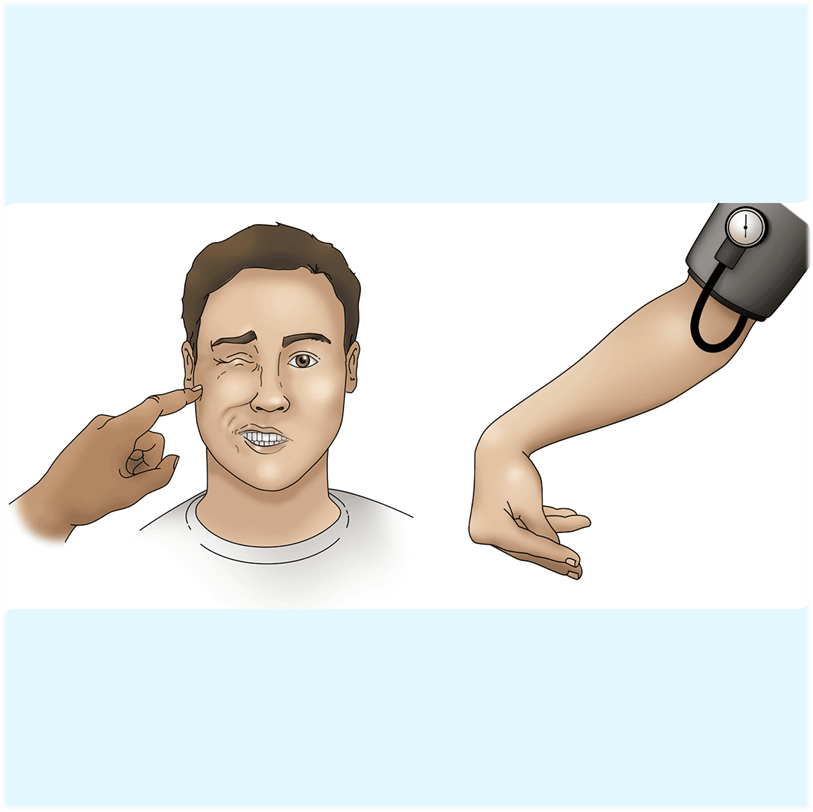
What are Chvostek’s and Trousseau’s Signs of Tetany and how are they related to calcium levels?
Hypocalcemia is associated with increased nerve excitability whereas hypercalcemia is associated with decreased nerve excitability
1) Hypocalcemia causes tetany due to its affect on increasing nerve excitability, which causes a positive Chvostek’s and Trousseau’s sign
→ Trousseau’s sign - placing a blood pressure cuff and pumping it up on a patient will cause hand spasms
→ Chvostek’s sign - tapping the facial nerve will cause facial spasms
2) This is because hypocalcemia allows for sodium channels to open leading to increase in membrane potential
→ this is why our body has basically an equal level of excretion and consumption of calcium daily in order to prevent tetany
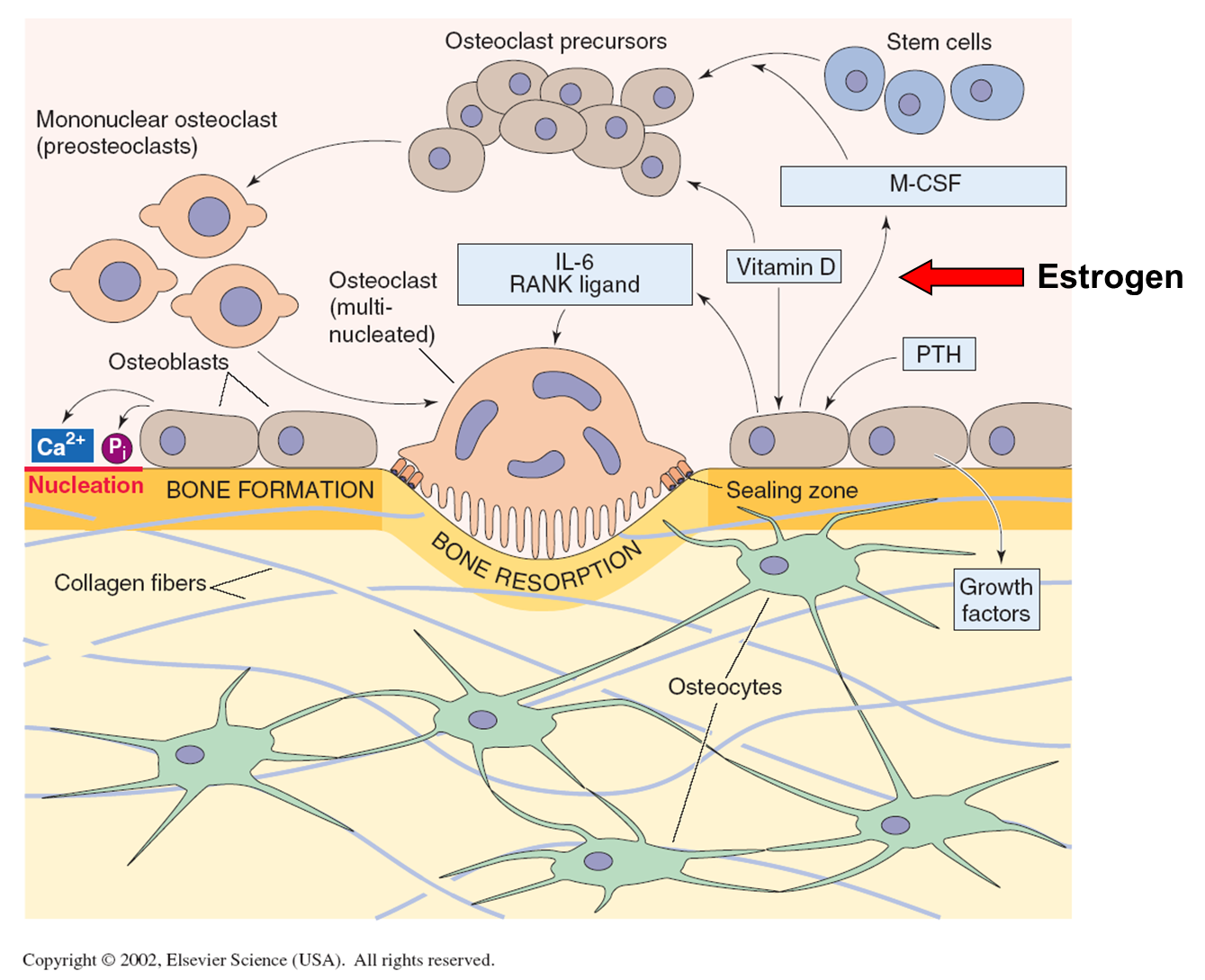
What cells are involved in bone turnover and what receptors do each of them carry?
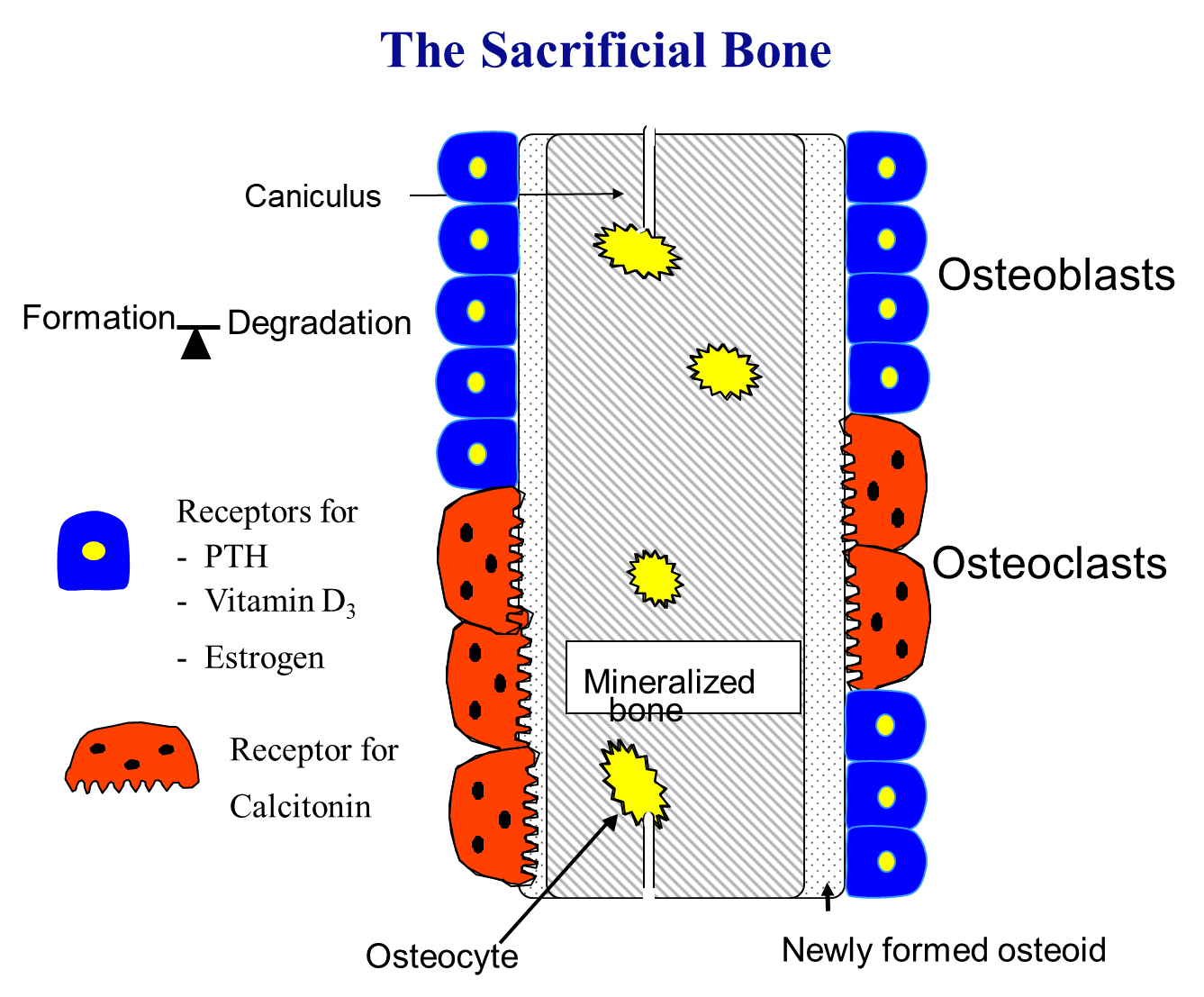
Bone Turnover is the process of building and breaking down bone, with the entire process of replacing the whole skeleton taking 7 years
1) Osteoclasts break down bone and are monocyte lineage
→ osteoclasts carry receptors for calcitonin
2) Osteoblasts build bone and carry three major receptors for three hormones
→ parathyroid hormone
→ vitamin D3
→ estrogen
How is Vitamin D produced?
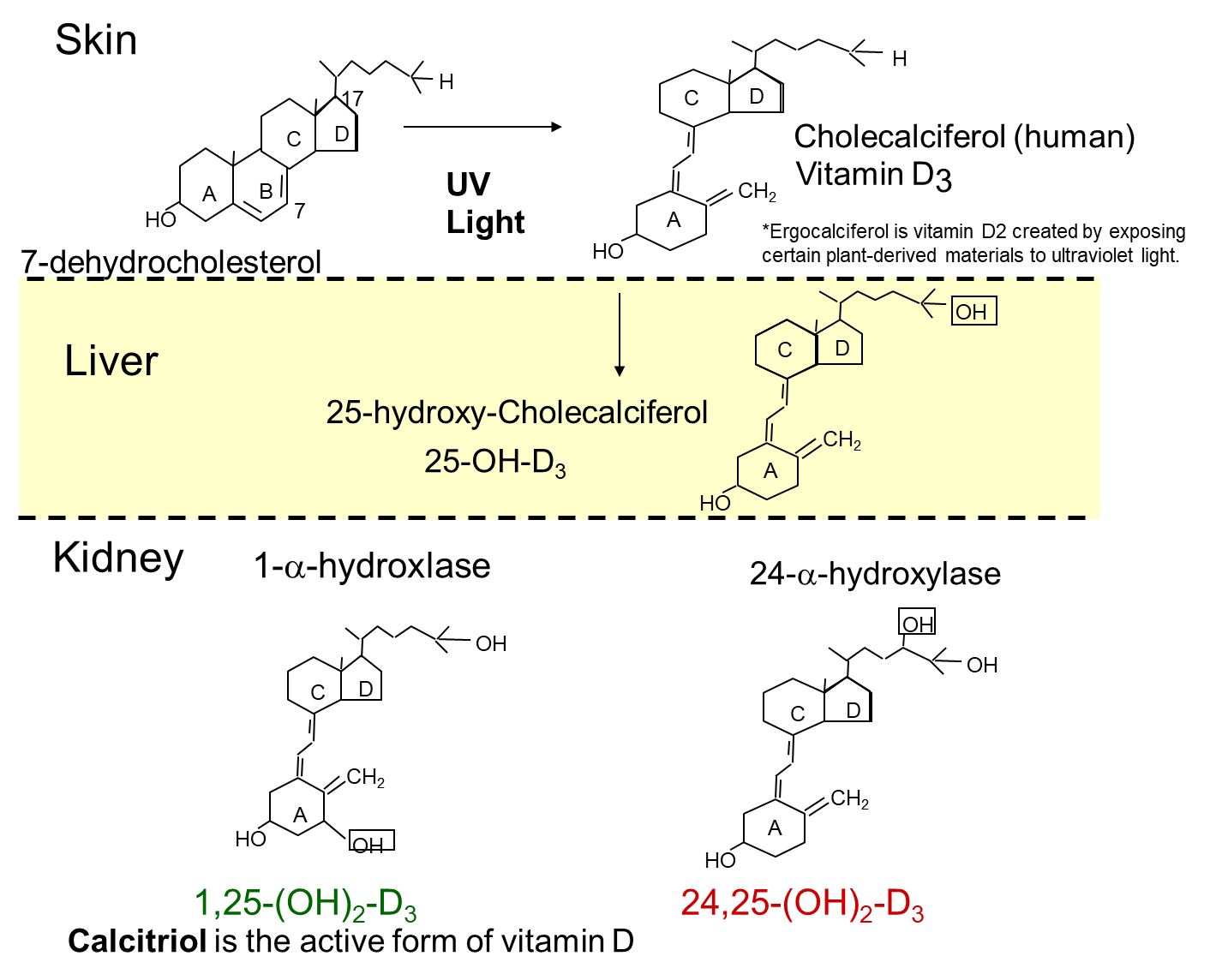
Humans can get Vitamin D is considered a hormone that we gain through exposure to UV-radiation and through our diet
1) When our skin is exposed to sun 7-dehydrocholesterol is converted to cholecalciferol or Vitamin D3
→ cholecalciferol is also found in our diet in the form of dairy products
2) Cholecalciferol is converted in the liver via hydroxylation at the 25th position, converting it into 25-hydroxycholecalciferol or calcifediol
3) 25-OH cholecalciferol then travels to the kidneys where it is hydrolyzed again into 1,25-dihydroxyvitamin D3 (calcitriol) which is the active form, converted via 1-alpha hydroxylase
→ 25-alpha hydroxylase can also activate in periods of high calcium or high phosphate, leading to the inactive form which is 24,25-dihydroxyvitamin D3
What does Vitamin D3 do?
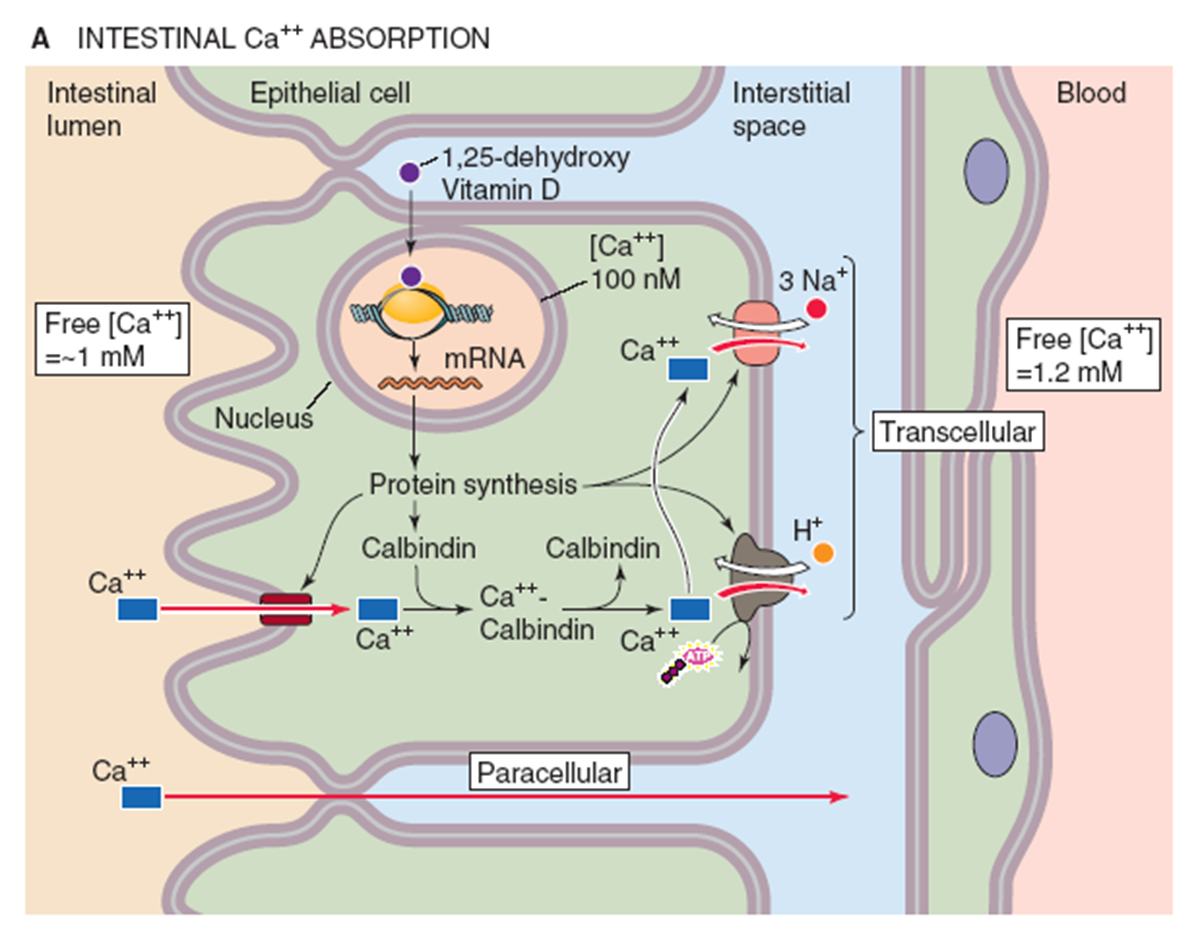
Vitamin D3 in its active form as 1,25 dihydroxyvitamin D3 (calcitriol) will bind to the GI epithelium in order to increase calcium and phosphate absorption in our diet
Binds to an intracellular receptor promoting 3 major changes
1) Expression of calcium channels on the apical surface that move calcium from the lumen into the cell
2) Expression of calbindin that moves calcium across the cell
→ stops calcium from being involved in intracellular processes in the GI lumen
3) Expression of active transport on the basolateral membrane to move calcium into the blood
Why is soda bad for growing kids?
Sodas have high levels of phosphates which can decrease expression of 1-alpha hydroxylase in the kidney
→ this leads to decreased levels of 1,25-dihydroxyvitamin D or calcitriol which can impede absorption of calcium in the GI lumen
→ may cause kids to be short
How does our body regulate parathyroid hormone production?
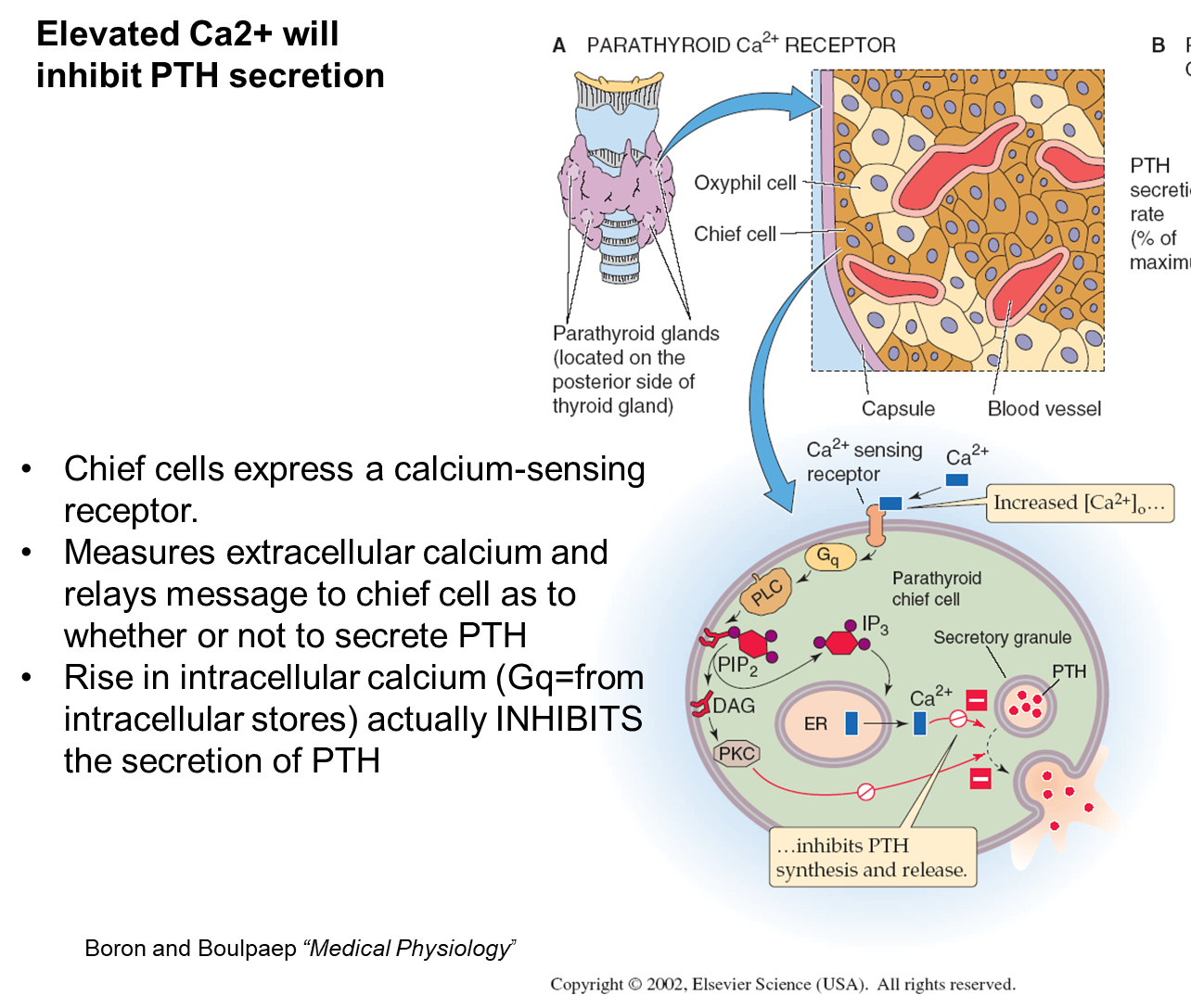
Chief Cells/Principial Cells of the parathyroid gland is the main cell involved in production of parathyroid hormone
1) There is a calcium sensing receptor (Gq) on the surface of chief cells that measures extracellular calcium levels
→ when you have high calcium it will stimulate the receptor leading to an increase in Protein Kinase C and leads to a rise in intracellular calcium
2) this rise in intracellular calcium acts differently compared to other hormones, resulting in a INHIBITION of secretion of parathyroid hormone
Where does Parathyroid Hormone act?
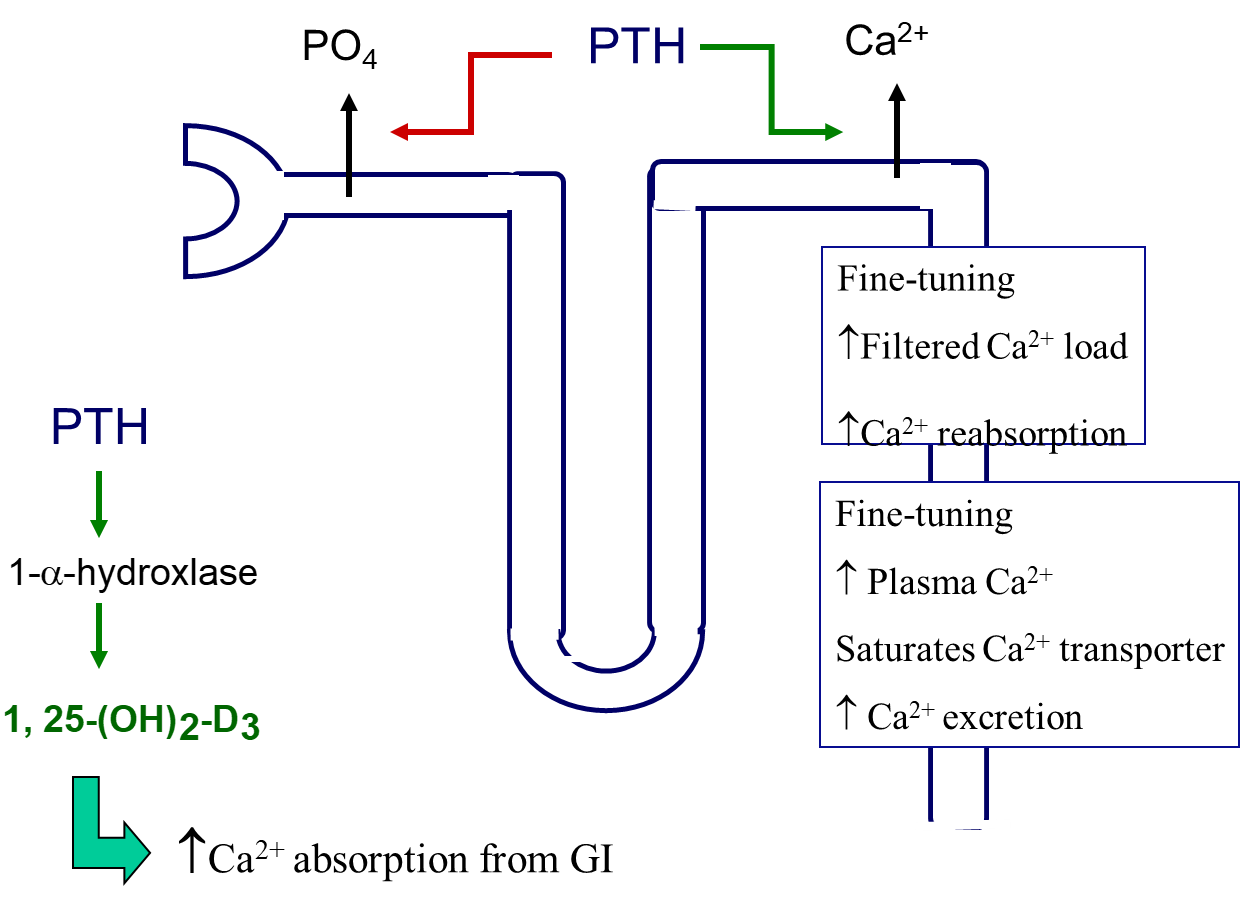
Kidney
1) Parathyroid Hormone binding will cause an increase in calcium reabsorption and phosphate excretion
→ this is the ONLY site where the levels of calcium and phosphate move in opposite directions in order to prevent Ca/PO4 salt accumulation in the nephron (stop kidney stone formation)
Bone
1) PTH will increase bone resorption by changing ligand expression on osteoblasts
→ PTH will upregulate levels of RANK-L while decreasing levels of osteoprotegerin on osteoblasts
What is Hypercalcemia of Malignancy?
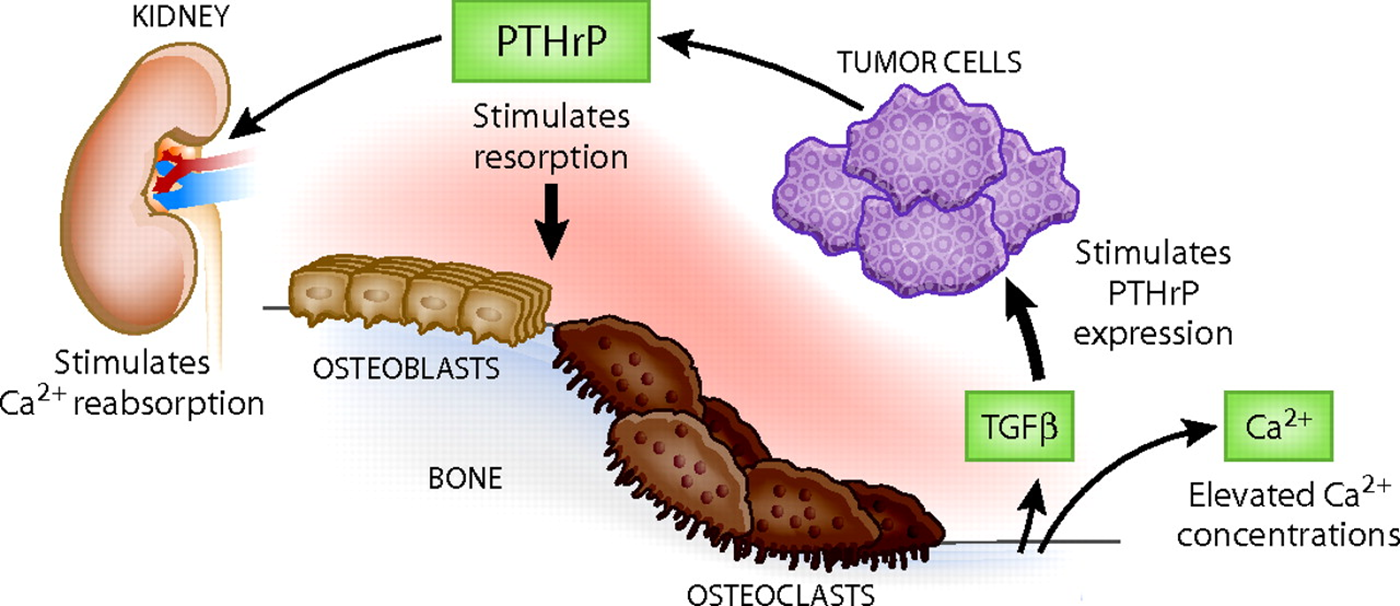
Small Cell Carcinoma can produce PTHrP or parathyroid hormone related peptide, that functions the same way as parathyroid hormone
1) this leads to a stimulation of osteoclast breakdown of bone, which can release TGF-beta
→ TGF-beta release can stimulate tumor growth
2) This disease is always seen in patients with hypercalcemia and is a smoker
What is Calcitonin?
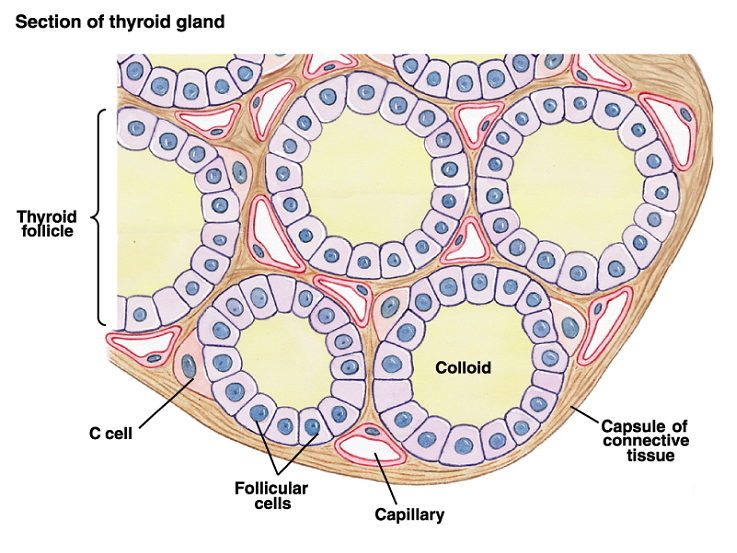
Calcitonin is a non-essential thyroid hormone produced by C-cells/Parafollicular Cells
1) Receptors on the osteoclasts can bind to calcitonin and stop bone resorption
→ often used therapeutically to treat osteoporosis
What is the role of estrogen and glucocorticoids in Osteoporosis?
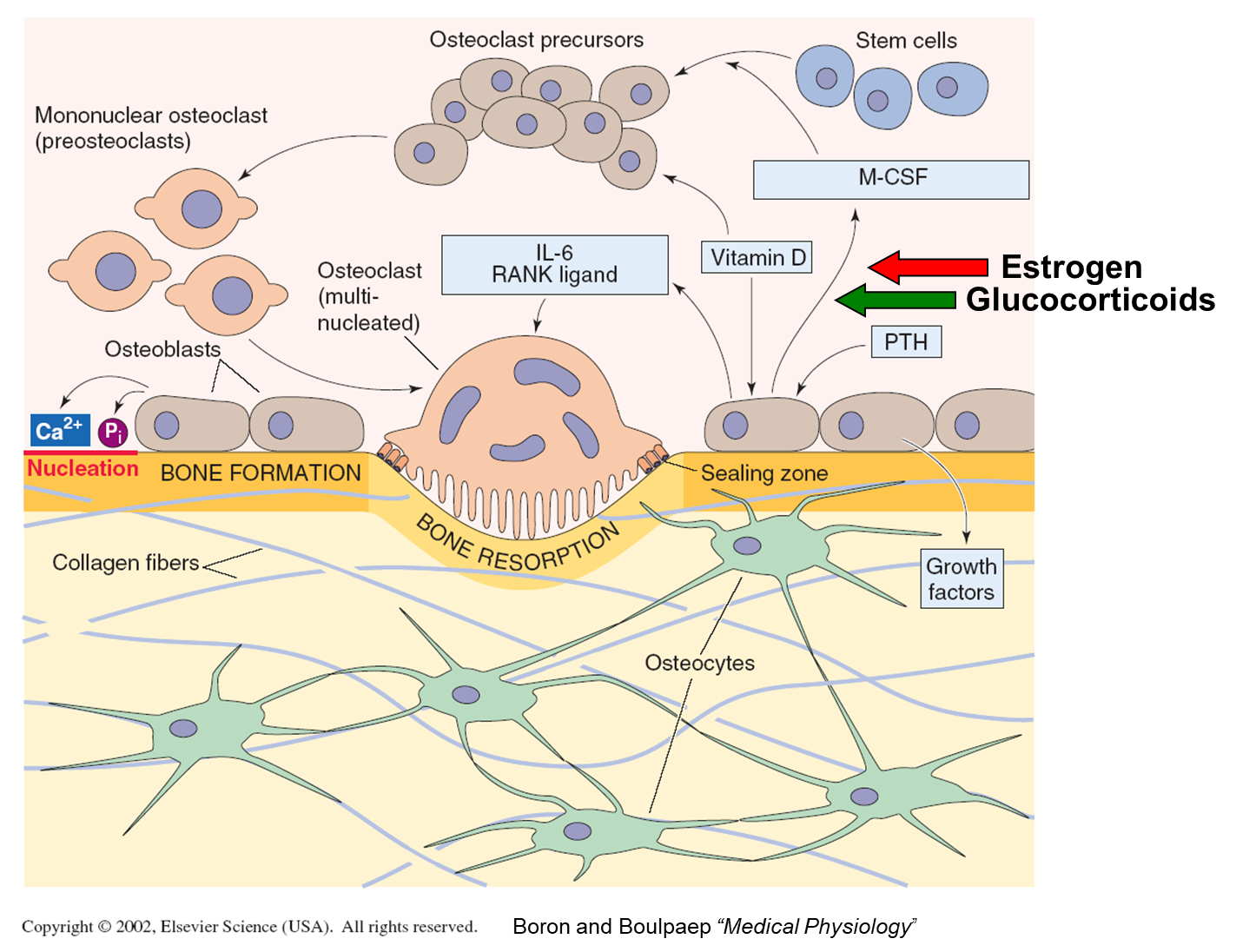
1) Estrogen will prevent overstimulation of bone resorption in this process, so women on menopause will be susceptible to osteoporosis,
→ classically presenting with a dorsal kyphosis
2) Glucocorticoids can stimulate osteoclasts leading to increased bone turnover, furthering osteoporosis
What is Primary Hyperparathyroidism?

Excess parathyroid hormone is produced due to hyperplasia/tumor at the parathyroid gland leading to a loss of bone tissue
1) Patients will have elevated PTH despite high levels of calcium and low levels of phosphate
→ patients will often be lethargic and weak with constipation
→ they are often susceptible to breaking their bones and may present with easy fractures
2) There can also be the formation of kidney stones due to an eventual increase in calcium in the urine
3) Treated with calcitonin and bisphosphonates
What is Secondary Hyperparathyroidism?
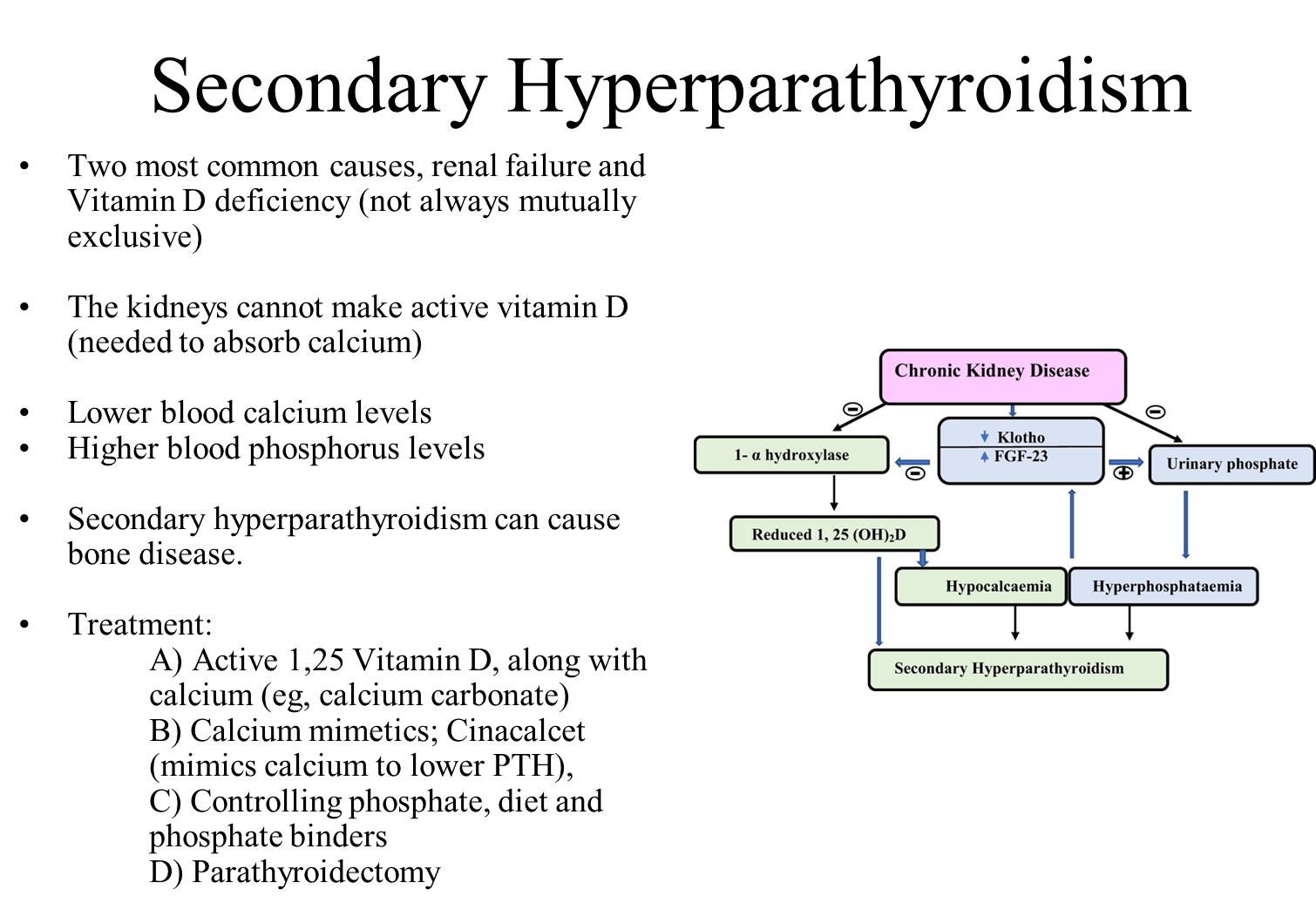
Secondary Hyperparathyroidism is a condition where a disease outside of the parathyroid glands causes the parathyroid glands to become enlarged and hyperactive
→ seen secondarily to renal failure or vitamin D deficiency
1) Kidney Failure
→ kidney is unable to make Vitamin D or remove phosphorus leading to low calcium levels
→ leads to stimulation of the parathyroid glands
2) Low Vitamin D levels can lead to low calcium absorption chronically
→ leads to increased stimulation of the parathyroid gland
3) Treated in three ways
→ Vitamin D and Calcium
→ Calcium Mimetics
→ Controlling dietary phosphate levels
→ Parathyroidectomy