Neuro Block 2
5.0(1)
5.0(1)
Card Sorting
1/211
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
212 Terms
1
New cards
stimulus detector
level of sensory processing that converts environmental stimulus to neural signal
2
New cards
initial receiving center
level of sensory processing in CNS that receives input from stimulus detector
3
New cards
integration center
level of sensory processing where information is filtered/processed/integrated from groups of initial receiving centers
4
New cards
primary sensory cortex
level of sensory processing involving perception
5
New cards
stimulus detector units
specialized receptors depolarized directly by environmental stimuli
6
New cards
sensory transduction
conversion of stimulus energy into electrical energy
7
New cards
limbic system
region of brain where smell is integrated through
8
New cards
thalamus
region of brain where all senses except smell are integrated through
9
New cards
occipital lobe
location of primary visual cortex
10
New cards
temporal lobe
location of primary auditory cortex and taste + olfaction limbic cortex
11
New cards
parietal lobe
location of primary somatosensory cortex (touch)
12
New cards
association cortex
located near primary sensory areas, involved in perception, integrating sensory modalities
13
New cards
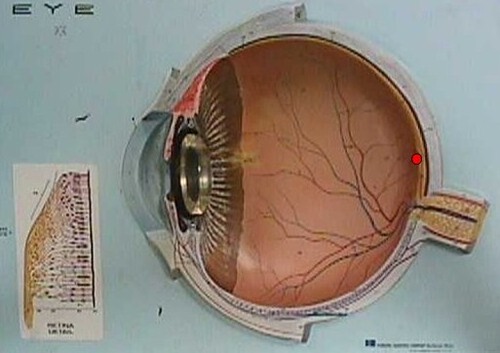
retina
part of CNS where vision stimulus detector units and initial receiving centers are located; where light energy is turned into neural activity
14
New cards
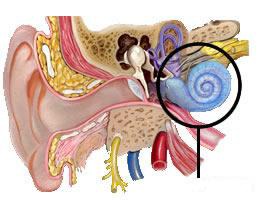
cochlea
part of inner ear where auditory stimulus detector units are located; energy from pressure waves is transduced into neural signals; hollow structure, filled with lymphatic fluid
15
New cards
medulla
initial receiving center for audition, somatosensation (in addition to spinal cord), gustation, and equilibrium
16
New cards
skin, muscle, joints
where somatosensory stimulus detector units are located
17
New cards
tongue, throat
where gustatory stimulus detector units are located
18
New cards
nose, throat
where olfactory stimulus detector units are located
19
New cards
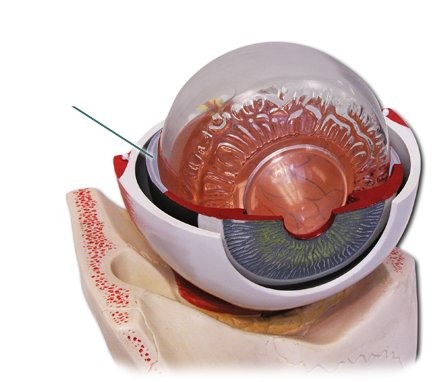
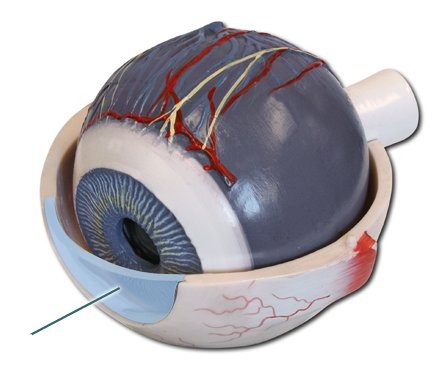
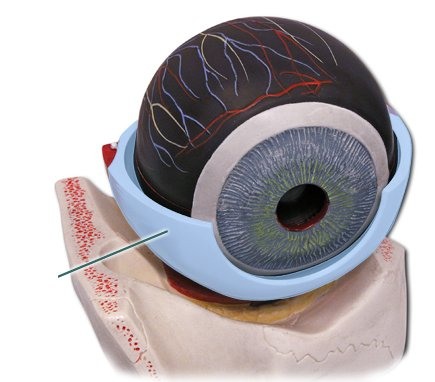
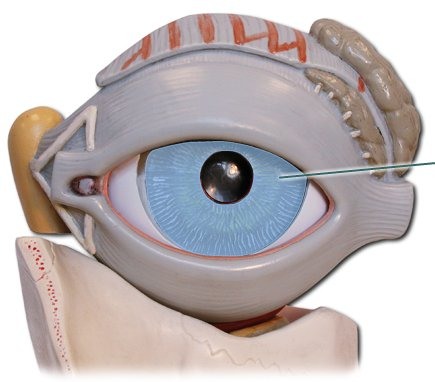
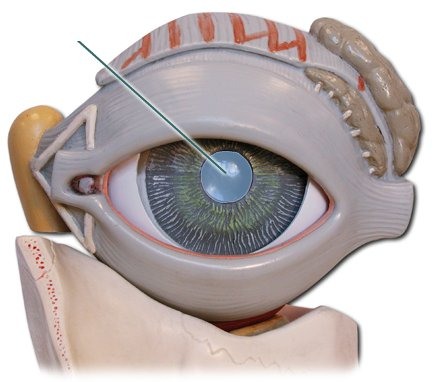
olfactory bulbs
initial receiving centers for olfaction
20
New cards
vestibular organ
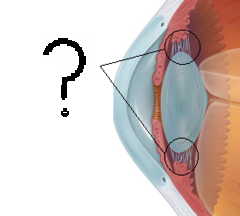
part of inner ear that contains stimulus detector units for equilibrium
21
New cards
somatosensory system
encodes and processes sensory information (touch, pressure, vibration, limb position, heat, cold, pain, itch, etc) from the skin, muscles, and viscera
22
New cards
proprioception
kinesthesia; position of limbs in space
23
New cards
pseudo-unipolar neuron
one single axon with two branches
24
New cards
peripheral branch
part of pseudo-unipolar neuron that extends from the periphery to the cell body
25
New cards
central branch
part of pseudo-unipolar neuron that extends from the cell body to the CNS
26
New cards
somatosensory receptive field
location on the body where a stimulus will affect the activity of a given somatosensory neuron
27
New cards
two point discrimination
the minimum interstimulus distance required to perceive two simultaneously applied stimuli as distinct (higher receptor density = greater discrimination)
28
New cards
dermatome
area of the skin innervated by a single spinal segment
29
New cards
slowly adapting receptors
afferent neurons whose firing rate decreases after stimulus onset, but the decrease is gradual and firing lasts as long as the stimulus is present; conveys static qualities of a stimulus, such as information about the size and shape of a stimulus
30
New cards
rapidly adapting receptors
afferent neurons whose firing rate decreases rapidly after stimulus onset and
can stop entirely before the stimulus has ended; signals start of a stimulus, but not continued presence; conveys dynamic qualities of the stimulus such as information about ongoing stimulation (movement)
can stop entirely before the stimulus has ended; signals start of a stimulus, but not continued presence; conveys dynamic qualities of the stimulus such as information about ongoing stimulation (movement)
31
New cards
A-beta-fibers
touch fibers; light touch, pressure, vibration, >22 micrometers, highly myelinated fibers, fast conducting
32
New cards
type I A-delta-fibers
nociceptive fibers for gross touch, fast pain, high heat (>53C), capsaicin-insensitive, 12-22 micrometers, little myelination
33
New cards
type II A-delta-fibers
nociceptive fibers for gross touch, fast pain, low heat (>43C), capsaicin-sensitive, 12-22 micrometers, little myelination
34
New cards
C-fibers
nociceptive fibers for slow pain, low pH, heat, capsaicin-sensitive,
35
New cards
somatosensory pathway 1
mechanosensory; fine tactile (touch), pressure, vibration
36
New cards
somatosensory pathway 2
pain, temperature, itch
37
New cards
encapsulated nerve endings (corpuscles)
mechanoreceptors; tip of sensory axon embedded in specialized connective tissue; sense touch, including fine tactile, vibration, and pressure; proprioceptive; in non-hairy skin
38
New cards
Piezo2
channels that convert mechanical signals to electrical signals
39
New cards
Meissner's corpuscles
encapsulated nerve endings closest to skin surface; sense light touch, vibrations of textured objects against skin, and slippage between skin and object (grip)
40
New cards
Merkel cells
encapsulated nerve endings enriched in fingertips and lying in tips of primary epidermal ridges (fingerprints); sensory axons in close contact with a connective tissue capsule within the skin; highest spatial resolution (0.5mm); fine touch
41
New cards
Ruffini's corpuscles
encapsulated nerve endings that sense stretching of skin by deforming sensory axon when skin stretched; sensory axons run through bundles of collagen fibers deep in the skin
42
New cards
Pacinian corpuscles
encapsulated nerve endings with large sensory axons embedded in fluid-filled layers of special connective tissue cells located deep in the skin; sensitive with large receptive fields; respond mainly to high frequency vibration (grasping, picking up, putting down)
43
New cards
muscle spindles
intrafusal fibers stretch and activate (depolarize) afferent sensory neurons, which signal length of muscle and rate of stretch
44
New cards
stretch reflex
muscles contract in response to stretching; sensory afferents signal stretch to spinal cord, where they synapse directly onto motor neurons
45
New cards
Golgi tendon organs
consist of a capsule attached to a tendon on one end and a muscle on the other; single afferent neuron innervates when tension is applied, signaling muscle contraction
46
New cards
dorsal column pathway
carries afferent mechanosensory input (tactile, proprioception) from spine to brain; first synapse at secondary sensory neurons in medulla; decussation level at medulla
47
New cards
decussation
crossing over of neural fibers
48
New cards
somatopy
topical organization of the body's surface sensations within each division of the primary somatosensory cortex (post central gyrus)
49
New cards
cortical plasticity
functional remapping of brain based on experience, "use it or lose it"
50
New cards
pain
unpleasant sensory and emotional experience associated with actual or potential tissue damage (subjective component)
51
New cards
nociception
encoding and processing of noxious stimuli by the CNS and PNS (relative objective component)
52
New cards
analgesia
relief from pain
53
New cards
noxious stimuli
stimuli that are actually or potentially damaging to tissue, including mechanical, thermal, or chemical stimuli; lead to release of a variety of substances that act on nociceptors
54
New cards
free nerve endings
receptor ending of somatosensory neuron that senses noxious stimuli (pain, temperature, itch, etc); tip of sensory axon in cutaneous tissue without anything surrounding it
55
New cards
high-threshold mechanoreceptors
nociceptors that respond to intense mechanical stimulation
56
New cards
chemosensitive nociceptors
nociceptors that respond to chemicals released in response to tissue damage and inflammation and some noxious chemicals that come into contact with skin
57
New cards
thermal nociceptors
nociceptors that respond to extreme heat or cold
58
New cards
transient receptor potential (TRP) channels
ion channels that activate in response to mechanical, thermal, and chemical (in addition to GPCRs) stimuli; influx of calcium and/or sodium causes depolarization
59
New cards
phasic receptors
receptors that produce an initial burst of activity firing but reduce if stimulus maintained
60
New cards
tonic receptors
receptors that produce constant rate of firing for length of the stimulus; most nociceptors
61
New cards
first pain
sharp pain usually in a specific location; short duration; carried by lightly myelinated, small-diameter axons (A delta fibers)
62
New cards
second pain
diffuse pain (dull aching); longer-lasting; carried by unmyelinated, very small-diameter axons (C-fibers)
63
New cards
spinothalamic pathway
carries afferent pain and temperature input from spine to brain; first synapse at neurons in dorsal horn; decussation level where afferent nerve enters spinal cord
64
New cards
referred pain
pain experienced as coming from one location when it is actually coming from a different source; pain caused in an internal organ can be confused by neurons in the spinal cord for pain from a peripheral location on the skin
65
New cards
central sensitization
activity-dependent increase in excitability of neurons in the dorsal horn of the spinal cord following high levels of activity in peripheral afferents
66
New cards
hyperalgesia
a normally painful stimulus is now perceived as significantly more painful
67
New cards
allodynia
a normally innocuous stimulus is now perceived as painful
68
New cards
gate theory
input from large, myelinated touch afferents synapse onto spinal interneurons, which can in turn block input from small, unmyelinated pain afferents
69
New cards
supraspinal mechanism
periaqueductal gray matter can inhibit spinal pain input
70
New cards
massage
high pressure causes large myelinated touch and pressure receptors (A-beta-fibers) to activate spinal inhibitory neurons that "drown out" pain signals from nociceptors
71
New cards
acupuncture
needles move to create steady stream of non-pain impulses by stimulating specific points which affect A-beta-fibers
72
New cards
acute pain
protective; occurs in presence of stimulus or tissue repair following injury
73
New cards
chronic pain
deleterious; occurs without an obvious stimulus or injury; >3mo; migraines, arthritis, fibromyalgia, low back pain, diabetic neuropathy
74
New cards
Mu opioid receptor
targeted by opioids to reduce firing of action potential at primary and secondary afferent and decrease pain signal transmission
75
New cards
optogenics
using light to control a limited population of neurons
76
New cards
Arch
inhibits neurotransmission in the presence of yellow light; could be used to treat pain
77
New cards
photoreceptors
retinal cells that convert light energy into neural activity; rods and cones; graded membrane potential, release Glu, hyperpolarized by light, only one type
78
New cards
lateral geniculate nucleus
part of thalamus that is first synaptic relay in primary visual pathway
79
New cards
light
electromagnetic radiation
80
New cards
high energy waves
gamma and cool colors
81
New cards
low energy waves
radio waves and hot colors
82
New cards
optics
study of light rays and their interactions
83
New cards
reflection
bouncing of light rays off a surface
84
New cards
absorption
transfer of light energy to a particle or surface
85
New cards
refraction
bending of light rays from one medium to another
86
New cards
cornea
transparent outer layer that allows light into eye
87
New cards
sclera
white of eye, opaque; tough protective cover
88
New cards
iris
colored part of eye; involuntary (smooth) muscle forms a ring that contracts and relaxes to control the amount of light that enters the eye
89
New cards
pupil
circular opening in iris where light comes through
90
New cards
lens
bends light as it comes into eye to focus it onto retina

91
New cards
ciliary muscle
smooth muscle that contracts and relaxes to control lens shape
92
New cards
accommodation
contraction of ciliary muscles causes lens to change shape, which focuses an image on retina
93
New cards
myopia
nearsighted; focus is in front of retina; eyeballs too elongated and lens too curved
94
New cards
hyperopia
farsighted; focus is behind retina; eyeball too short and lens too flat
95
New cards
horizontal cells
retinal cells involved in lateral control and mediation of bipolar cells and ganglion cells
96
New cards
bipolar cells
retinal cells that form middle layer of neurons that process visual info; graded membrane potential, release Glu, ON or OFF center cells; perform sign conserving/inverting operation
97
New cards
amacrine cells
retinal cells involved in lateral control and mediation of bipolar cells and ganglion cells
98
New cards
ganglion cells
retinal cells that receive visual input from bipolar cells; axons form optic nerve; generate action potentials, ON or OFF center
99
New cards
fovea
center of retina specialized for high acuity vision; contains more cones
100
New cards
blind spot
location on retina where axons of retinal ganglion cells come together and form the optic nerve; blood vessels enter and exit eyes