8. Uronic acid pathway of glucose and other hexoses/glucuronic acid pathway
1/54
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
Define the glucuronic acid pathway.
An alternative oxidative pathway for glucose
Deals with the synthesis of glucuronic acid, pentoses, and vitamins
Does glucuronic acid pathway lead to the generation of ATP?
No
Where does the glucuronic acid pathway take place?
Cytoplasm of liver cells
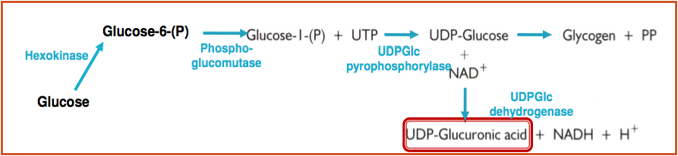
What is the first step of glucuronic acid pathway?
Glucose is isomerized to glucose-6-phosphate and then glucose-1-phosphate
Enzymes used are hexokinase and phosphoglucomutase, respectively
What is the second step of the glucuronic acid pathway?
Glucose-1-phosphate reacts with UTP to form uridine diphosphate glucose (UDPGlc)
Enzyme used is UDPGlc pyrophosphorylase
What is the third step of the glucuronic acid pathway?
UDPGlc is oxidized at carbon 6 to yield UDP-glucuronate/UDP-Glucuronic acid
Enzyme used is NAD-dependent UDPGlc dehydrogenase
UDP glucuronic acid is the ______ form of glucuronic acid.
active
What is the importance of glucuronic acid pathway?
Provides UDP Glucuronic acid, which is used for:
Conjugation of less polar compounds etc bilirubin, steroids and some drugs, making them more water soluble (detoxicated)
Synthesis of glycosaminoglycans (mucopolysaccharides) e.g. heparin and hyaluronic acid
Precursor of L-ascorbic acid in some plants and animals
What are the effects of drugs on the uronic acid pathway?
Barbiturates, antipyrine, and aminopyrine will increase uronic acid pathway
Leads to availability of more glucuronate for conjugation
Why can’t ascorbic acid be synthesized in humans, primates, guinea pigs, and bats?
Due to absence of L-gulunolactone oxidase
(So, Vitamin C essential in diet)
Describe essential pentosuria.
Inborn error of metabolism
1 in 2,500 births
In pathway, L-xylulose is converted to D-xylitol by NADP-dependent enzyme xylulose reductase
Deficiency in enzyme leads to L-xylulose excreted in urine, leads to pentosuria
Detected by Benedict’s test
Not harmful condition
Differentiated from diabetes mellitus by HbA1c, fasting blood sugar test for DM
Describe the polyol pathway of glucose/sorbitol pathway.
Directly related to glucose conc. and higher in uncontrolled DM
AKA sorbitol-aldose reductase pathway
Polyol pathway appears to be involved in diabetic complications, esp. microvascular damage to retina, kidney, and nerves
Sorbitol poorly absorbed from intestine, cannot cross cell membranes, cannot diffuse out of cells easily and gets trapped in them
When accumulates produces osmotic stress on cells by drawing water into insulin-dependent tissues
What are the reactions of polyol pathway/sorbitol pathway?
Glucose reduced to sorbitol using aldose reductase
Sorbitol oxidized into fructose using sorbitol dehydrogenase
Where is sorbitol present normally?
Lens of eyes
In DM, glucose level increases, which increases sorbitol content. What does this lead to?
Osmotic damage of tissues and developement of cataracts
How does sorbitol pathway play a role in diabetic renal complications?
Aldose reductase metabolizes excess glucose to toxic metabolites which induce hyperfiltration and glomerular dysfunction
Sorbitol pathway produces fructose which is present in a large quantity in _____ and also found in ___.
semen
CSF (cerebrospinal fluid)
Where is the polyol pathway active?
Brain
Where is the polyol pathway inactive?
Liver
_______ is found in corn syrups and honey in high concentrations.
Fructose
Entry of fructose into cells is not _______-_________.
insulin-dependent
Fructose does not promote the secretion of _______.
insulin
Fructose is metabolized by the ______.
liver
The pathway of ___________ of fructose differs in ______ and ______.
utilization
muscle
liver
What is the first step in fructose metabolism?
Fructose phosphorylated into fructose-1-phosphate
Enzyme used is fructokinase
ATP converted into ADP
What is the second step in fructose metabolism?
Fructose-1-phosphate split into glyceraldehyde and DHAP (dihydroxyacetone phosphate)
Enzyme used is fructose-1-phosphate aldolase
What happens to glyceraldehyde?
Glyceraldehyde phosphorylated to glyceraldehyde-3-phosphate
Enzyme used is triose kinase
ATP is converted into ADP
What happens to DHAP?
DHAP converted into glyceraldehyde-3-phosphate
Enzyme used is TIM (triphosphate isomerase)
Muscles that contain only __________ can phosphorylate fructose into ___ which is a direct glycolytic ____________.
hexokinase
F6P
intermediate
Why is fructose metabolism in the muscle not a significant pathway for fructose metabolism?
Hexokinase has a very low affinity to fructose compared to glucose unless it is present at high conc. in the blood
Free fructose is seen in large amounts in _______ ______.
seminal plasma
Fructose is secreted by _______ ________.
seminal vesicles
Fructose provides energy for mobility of ___________.
spermatozoa
What is seen in people who have blocked seminal ducts?
Azoospermia
Deficiency of fructose correlates with
male infertility
What are 2 hereditary defects of fructose metabolism?
Fructosuria
Hereditary Fructose Intolerance (HFI)
Describe fructosuria.
Benign metabolic defect
Caused by deficiency in fructokinase
Excess accumulated fructose lost in urine
Urine gives positive benedicts and seliwanoff’s test
1 in 130,000 births
Describe Hereditary Fructose Intolerance (HFI).
Autosomal recessive inborn error of metabolism
1 in 20,000 births
Caused by deficiency in aldolase B
Leads to accumulation of F1P
Seen when sucrose introduced into diet of infant usually 6 months of age
Accumulation of F1P inhibits glycogen phosphorylase, leading to accumulation of glycogen in liver and associated with hypoglycemia
What are the symptoms and treatment of HIF.
Vomiting
Loss of appetite
Infants fail to thrive
Hepatomegaly and jaundice
Death, if damage of liver progresses
Treatment is to withdraw fructose from diet
Will immediately relieve symptoms
What is the major source of galactose?
Dairy products
How does galactose enter glycolysis?
By its conversion to glucose-1-phosphate which occurs through series of steps
Where is galactose metabolized?
Liver
What test is done to asses functional capacity of liver?
Galactose tolerance test
What is the first step of galactose metabolism?
Galactose is phosphorylated into galactose-1-phosphate
Enzyme used is galactokinase
ATP is converted into ADP
What is the second step of galactose metabolism?
Galactose-1-phosphate is converted into glucose-1-phosphate
Enzyme used is Galactose-1-phosphate uridylyltransferase
Cofactor is UDP glucose
Where does the UDP glucose come from?
Glucose-1-phosphate is converted into UDP glucose
Enzyme used is UDP-glucose pyrophosphorylase
UDP-glucose is converted into UDP-galactose
UDP-galactose is converted back to UDP-glucose using UDP-galactose epimerase
UDP-glucose used as cofactor again
What is the third step of galactose metabolism?
Glucose-1-phosphate is converted into glucose-6-phosphate
Enzyme used is phosphoglucomutase
Describe galactosemia.
Increasing blood galactose conc. due to inability to metabolize galactose
Inborn error of metabolism
1 in 35,000 births
Caused by inherited defects in uridyl transferase (most common) or 4-epimerase
Accumulation of galactose-1-p in liver will inhibit galactose kinase and glycogen phosphorylase resulting in hypoglycemia
What are the effects of galactosemia?
Galactose reduced in eye by aldose reductase to form dulcitol which accumulates and causes cataracts (characteristic feature of galactosemia)
Enlargement of liver, jaundice, severe mental retardation
Describe galactosuria.
Excretion of galactose in urine
Treatment: lactose-free diet
Won’t improve mental retardation so early detection is important