Apex: Cardiovascular Anatomy & Physiology
1/170
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
171 Terms
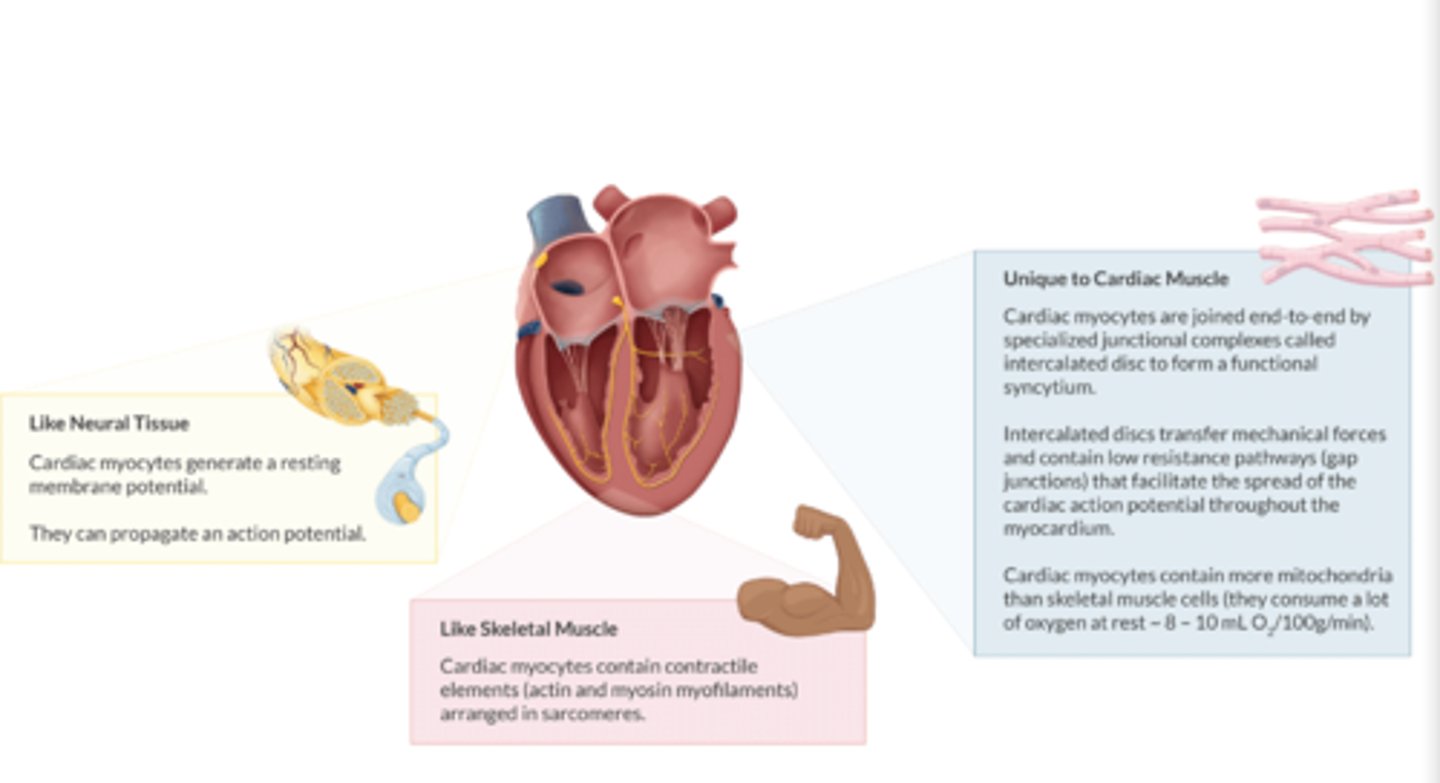
What is unique about cardiac myocytes:
1. How are they joined together?
2. do cardiac myocytes contain more or less mitochondria vs skeletal muscle cells?
3. How much O2 do cardiac myocytes consume at rest?
1. Joined by INTERCALATED DISCS & contain gap junctions to spread action potentials
2. More mitochondria than skeletal muscle cells.
3 O2 consumption at rest: 8-10 mL O2/100g/min.
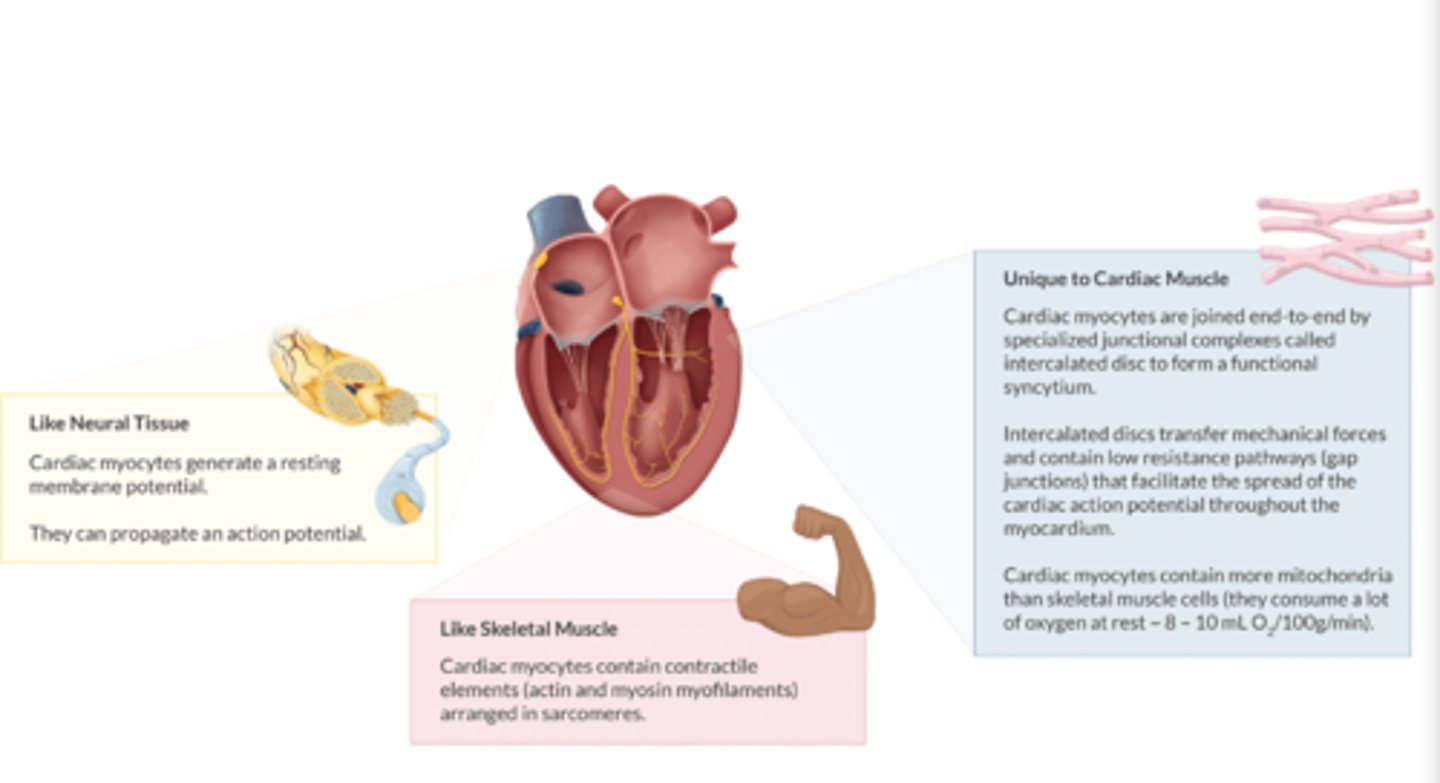
How are cardiac myocytes like neural tissue/myocytes? (2)
Both generate a resting membrane potential & propagate an action potential
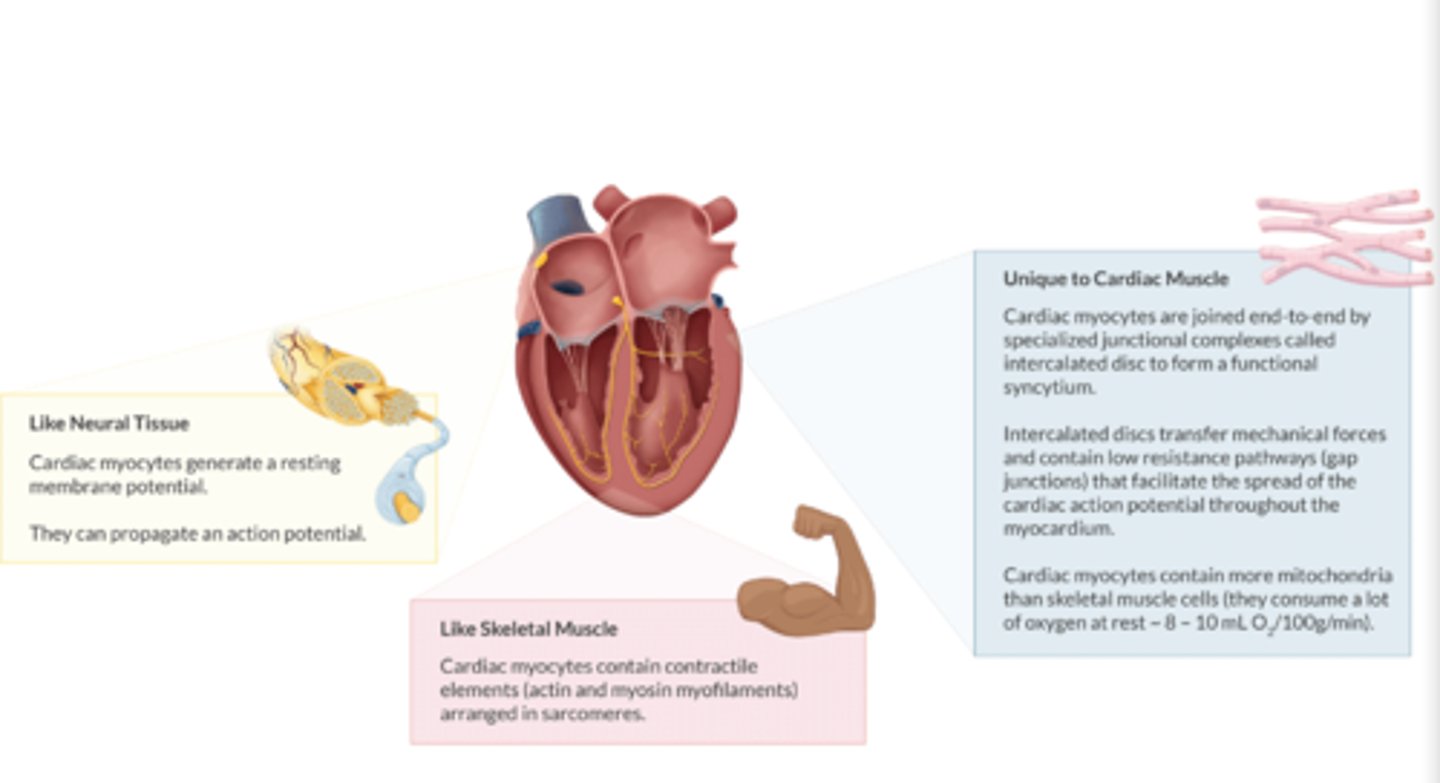
How are cardiac myocytes like skeletal tissue/myocytes? (2)
1. Both contain actin and myosin myofilaments (contractile elements)
2. arranged in sarcomeres
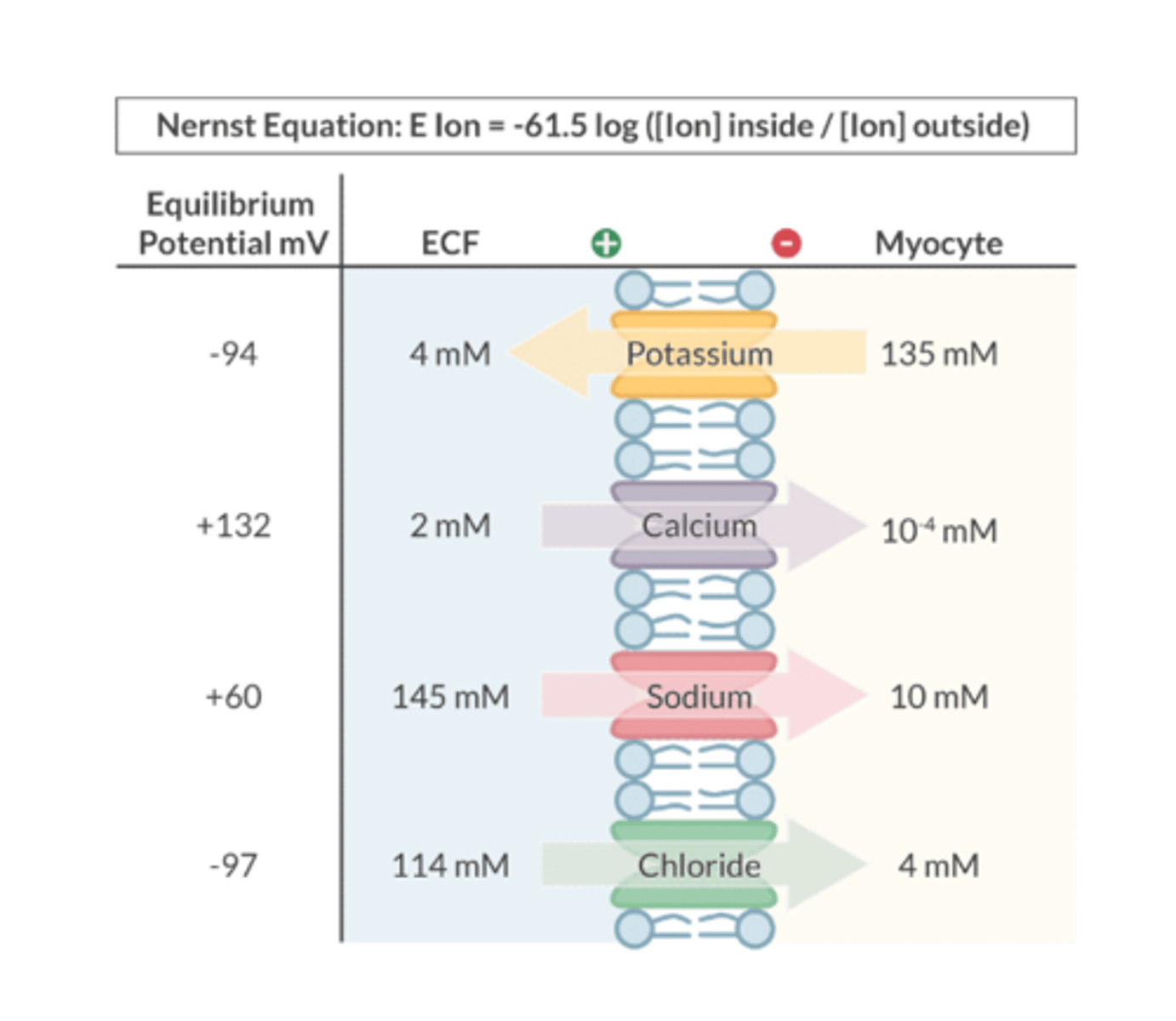
What is Equilibrium Potential?
Describes the situation where there is NO NET MOVEMENT of an ion across a cell membrane
-charge inside balances the charge on the outside
What can be used to predict an ion's equilibrium potential?
Nernst equation
Automaticity is the ability to:
Ability for the heart to generate an action potential spontaneously (via the SA node- sets the heart rate)
Excitability is the ability
- Heart responds to electrical stimulus
- Depolarizes & fires action potential
Conductance is the ability to transmit:
the ability to transmit electrical current
-Because ions are charged, they do no freely pass through cell membranes. Instead, an ion requires an open channel to cross from one side of the membrane to the other
-An open ion channel INCREASES the conductance of that ion
-A closed ion channel REDUCES the conductance of that ion
Define Inotropy
the force of myocardial contraction during systole
Define Chronotropy
heart rate
Define Dromotropy
conduction velocity through the heart
(velocity= distance/time)
Define Lusitropy
relaxation during diastole
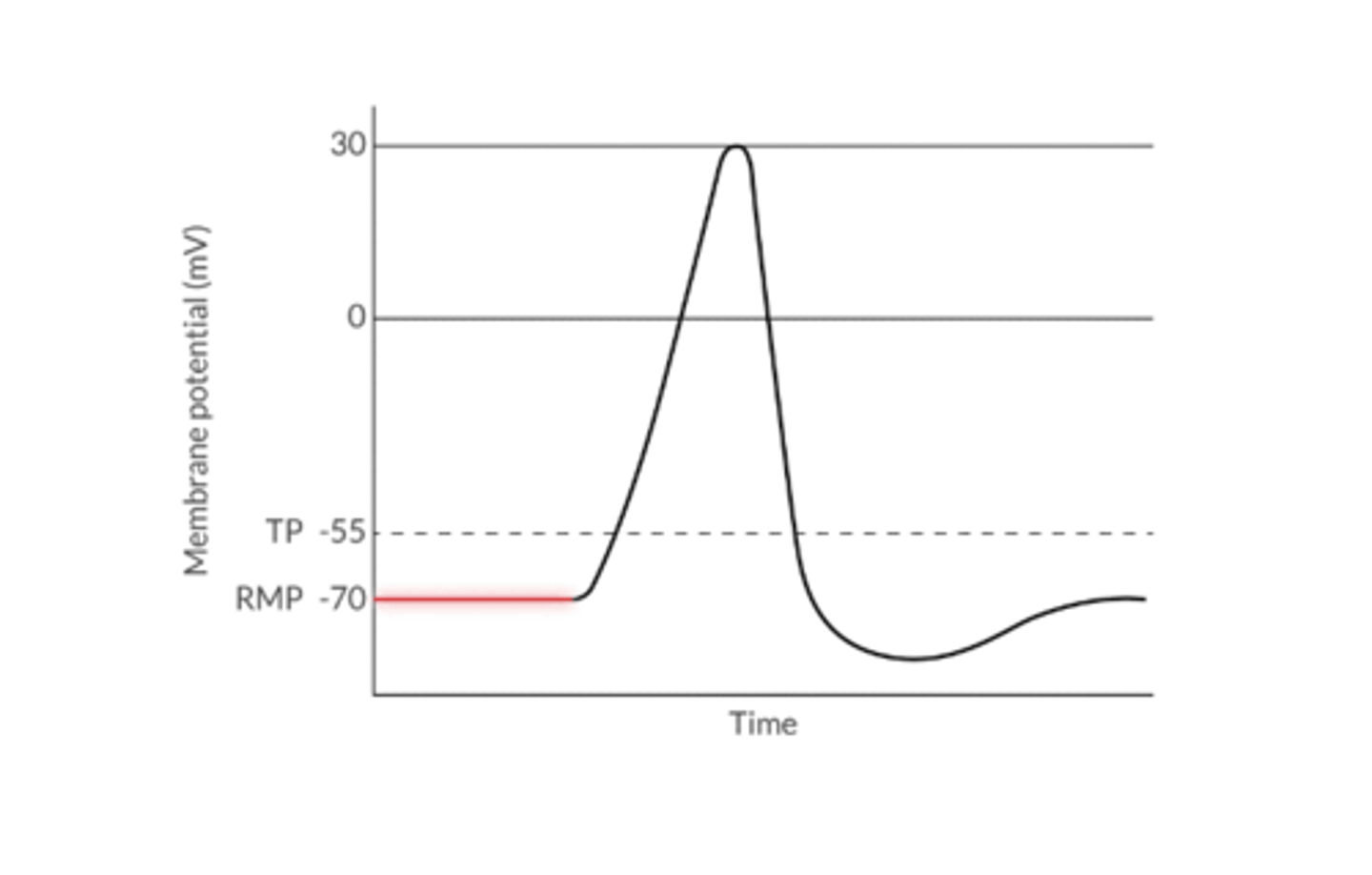
What is the Resting Membrane Potential of a Cardiac Myocyte?
The electrical potential across a cell membrane at rest (-70mV in cardiac myocyte)
What 3 things determine the RMP?
1. Chemical force (concentration gradient)
2. Electrostatic counterforce
3. Sodium/potassium ATPase
What is the primary determinant of RMP?
SERUM K***
At rest the nerve cell continuously leaks ________
K+ (loses its positive charge)
DECREASED serum K+ --> RMP becomes more _________
NEGATIVE
INCREASED serum K+ --> RMP becomes more _________
POSITIVE
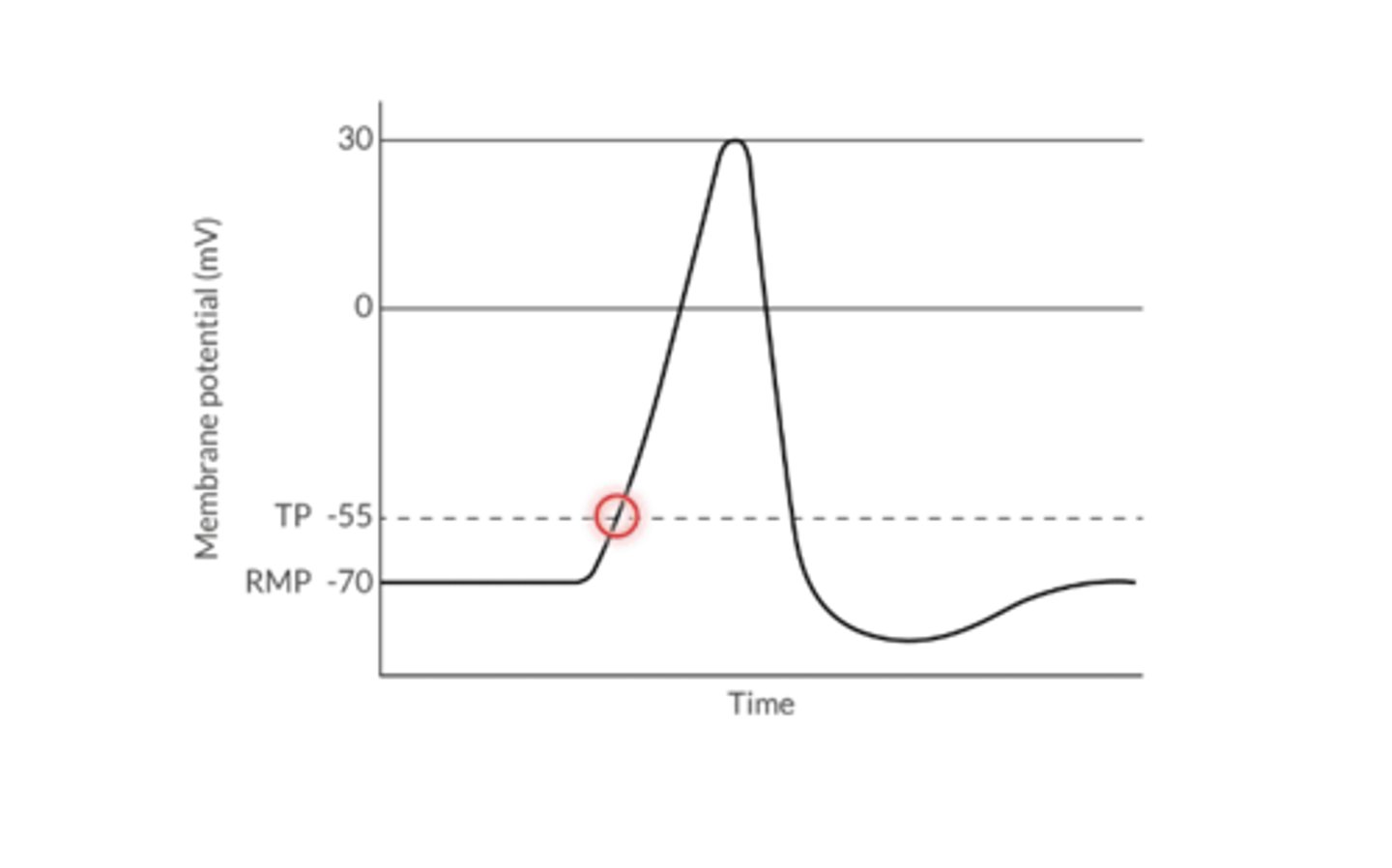
What is the Threshold Potential?
the voltage change that must occur to initiate depolarization (-55mv)
What is the primary determinant of threshold potential?
SERUM Ca+!!!
DECREASED serum Ca+--> TP becomes more ________
NEGATIVE
1. Depolarization describes:
2. What type of phenomenon
1. the movement of cell's membrane potential to a more positive value (less of a charge difference between inside and outside the cell)
Na+ or Ca+ enters the cell
2. All or nothing phenomenon
Results in an AP as long as the TP is achieved
What determines the ability of a cell to depolarize?
The difference between RMP and TP
When RMP is CLOSER to TP, the cell is ___________ to depolarize
EASIER
When RMP is FURTHER from TP, the cell is ___________ to depolarize
HARDER
1. What is Repolarization?
2. Ion movement during this time?
3. resistant to what during this time?
1. The return of a cell's membrane potential towards a more negative value after depolarization
2. K+ leaves the cell of Cl- enters the cell
3. The cell is resistant to subsequent depolarization during the refractory period
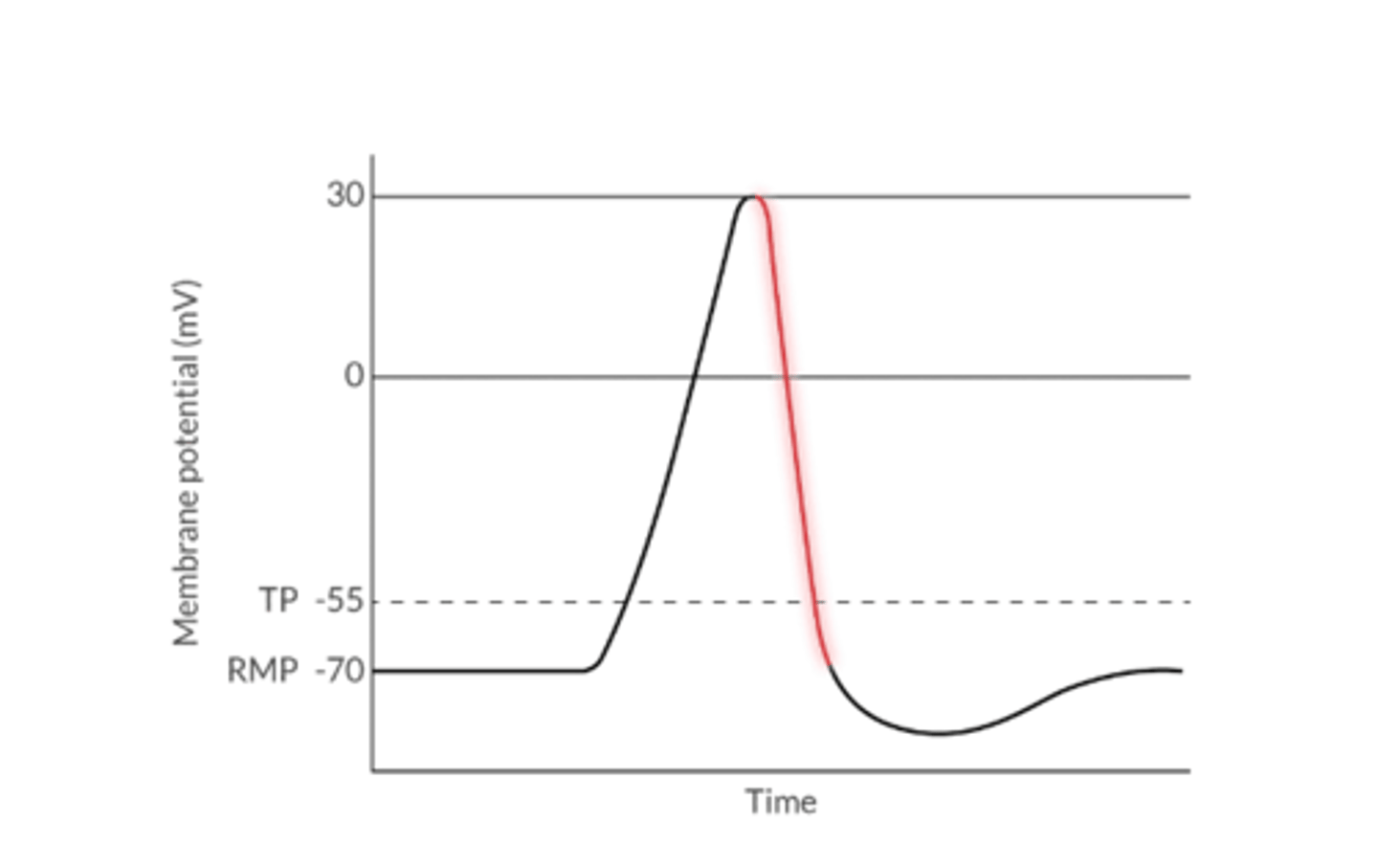
Hyperpolarization describes what?
The movement of a cell's membrane potential to a more negative value beyond the RMP
Typically happens after repolarizations for a very short time
Because RMP is further from TP, it's more difficult to depolarize a cell that's hyperpolarized
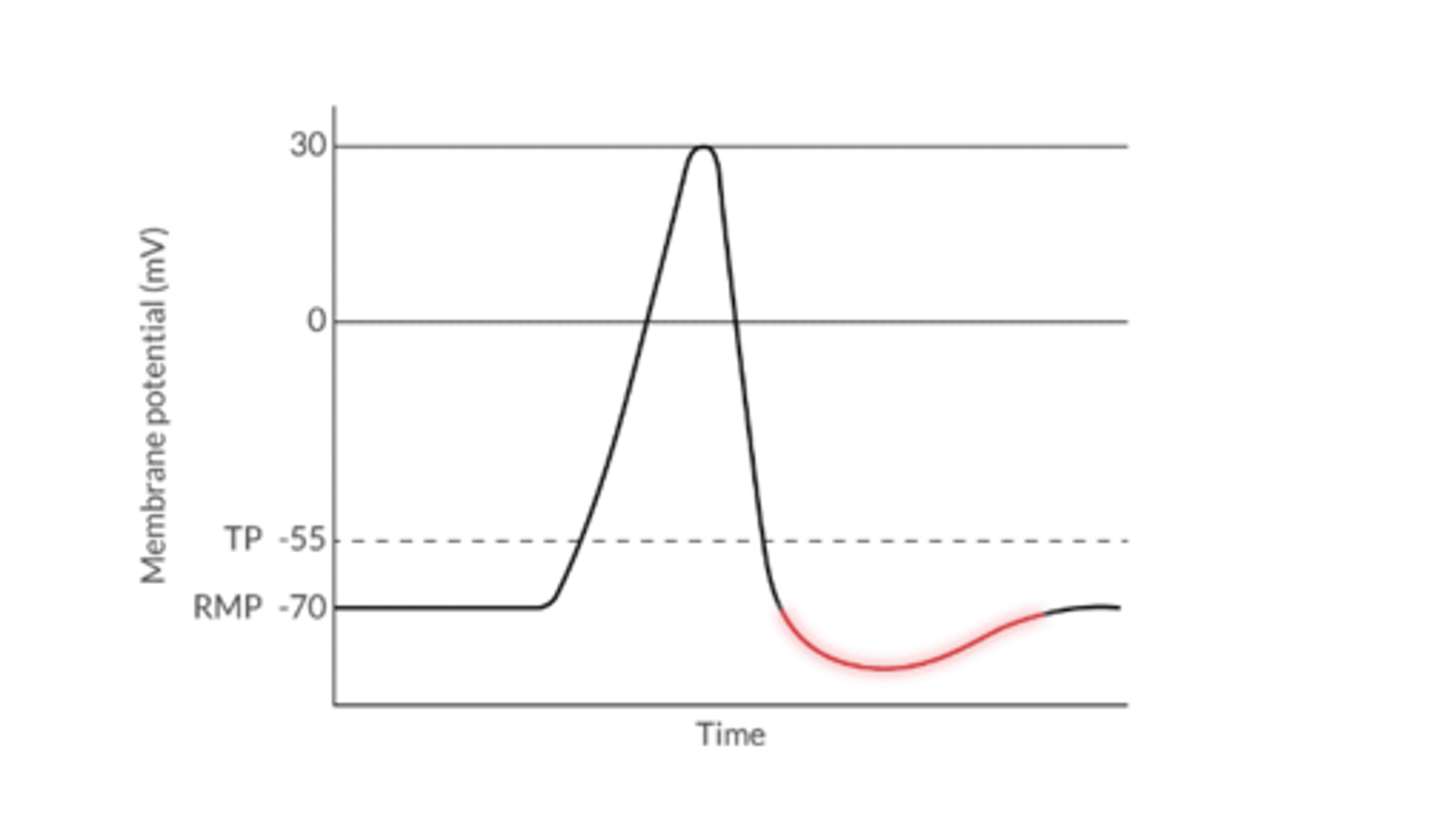
What restores the ionic balance towards RMP in excitable tissue?
Sodium-potassium ATPase pump
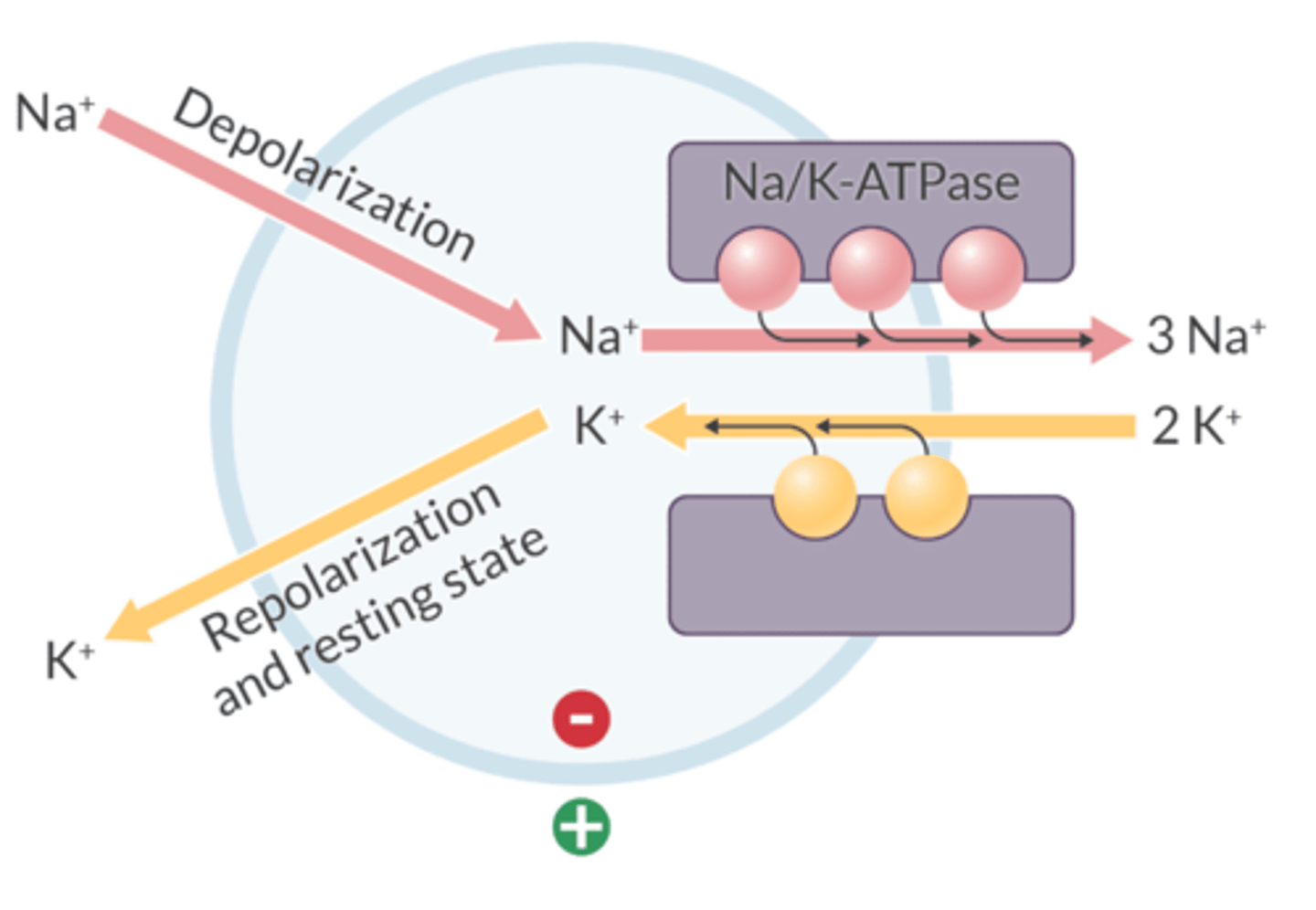
Sodium-potassium ATPase pump:
1. Ion movement with this pump?
2. Passive or active?
1. Removes 3 Na+ that enters the cell during depolarization
2. Returns 2 K+ that has left the cell during repolarization
1. For every 3 Na+ ions it removes, it brings 2 K+ into the cell
Always on
2. An ACTIVE TRANSPORT mechanism that requires ATP
What drug inhibits the Na/K-ATPase?
Digoxin
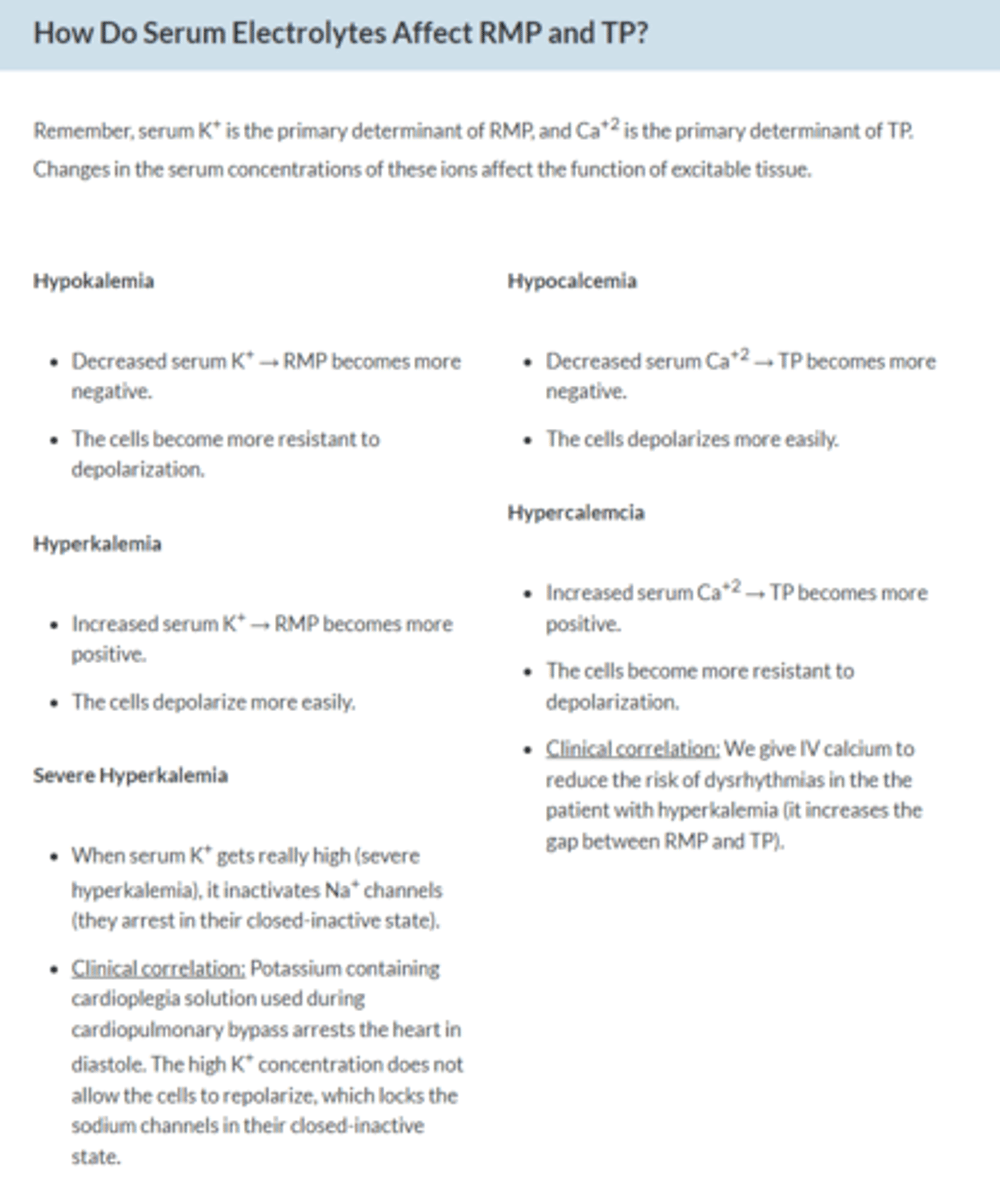
How do serum electrolytes affect RMP and TP?
1. Hypokalemia
2. Hyperkalemia
3. Hypocalcemia
4. Hypercalcemia
1. RMP more negative--> Cell resistant to depolarization
2. RMP more positive--> depolarize more easily
3. TP more negative--> depolarize more easily
4. TP more positive--> more resistant to depolarization
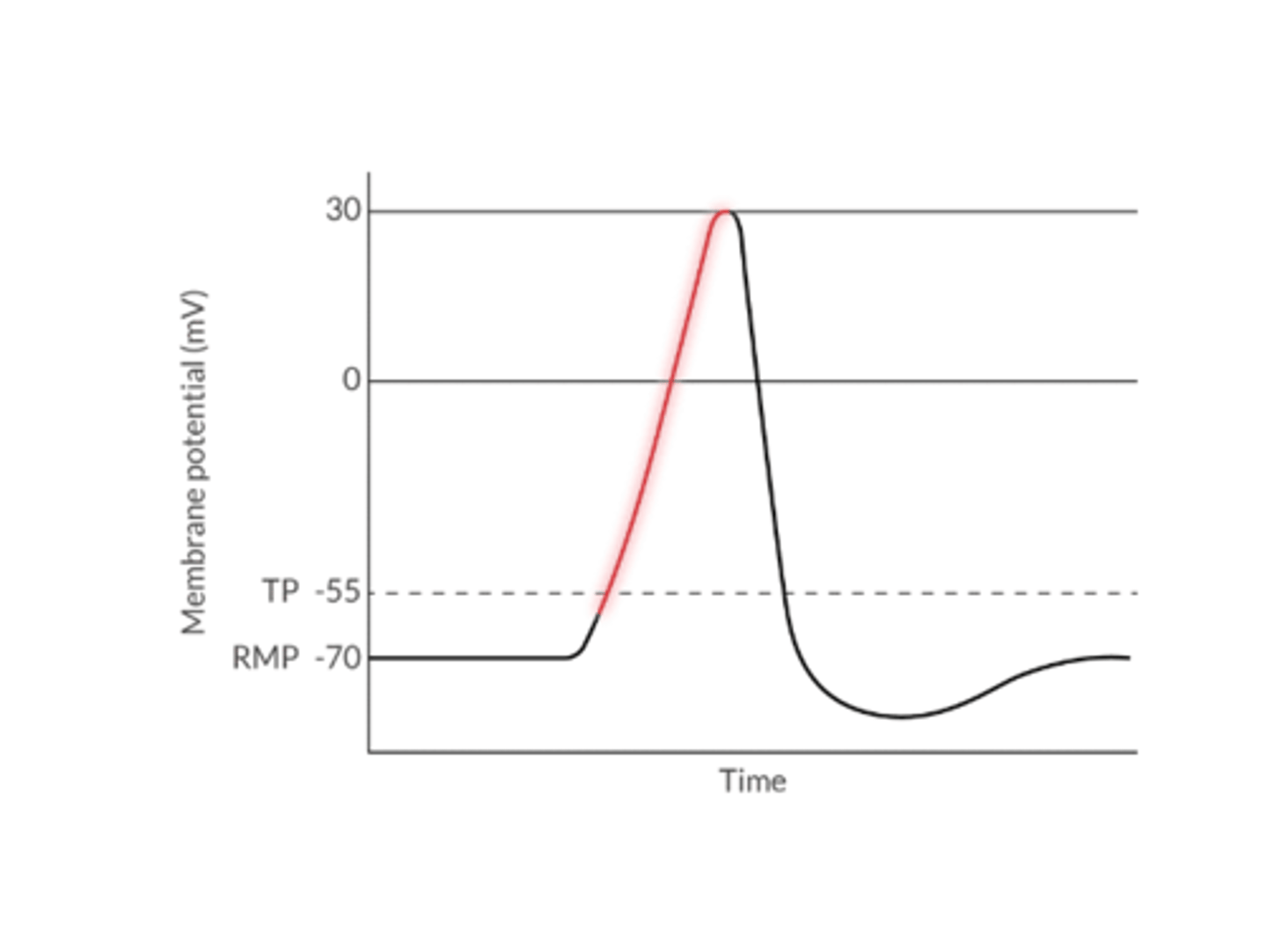
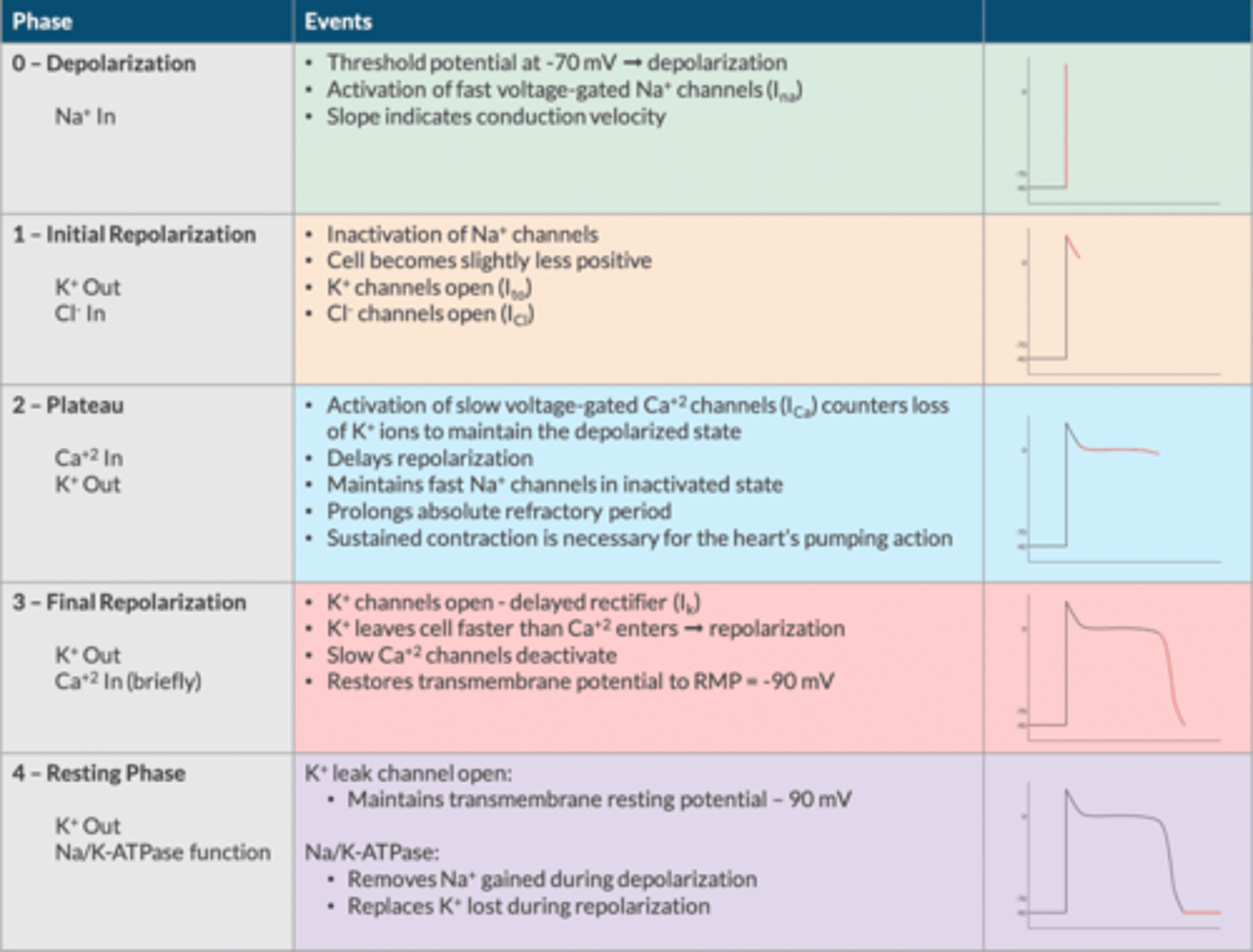
Myocyte Action Potential (The Bare Minimum):
What are the phases (5)?
Describe ion movement during each phase:
Phase 0= Depolarization: Na+ IN
Phase 1= Initial Repolarization: Cl- IN and K+ OUT
Phase 2= Plateua: Ca+ IN and K+ OUT
Phase 3= Repolarization: K+ OUT
Phase 4= Maintenance of TMP: K+ OUT and Na/K-ATPase function
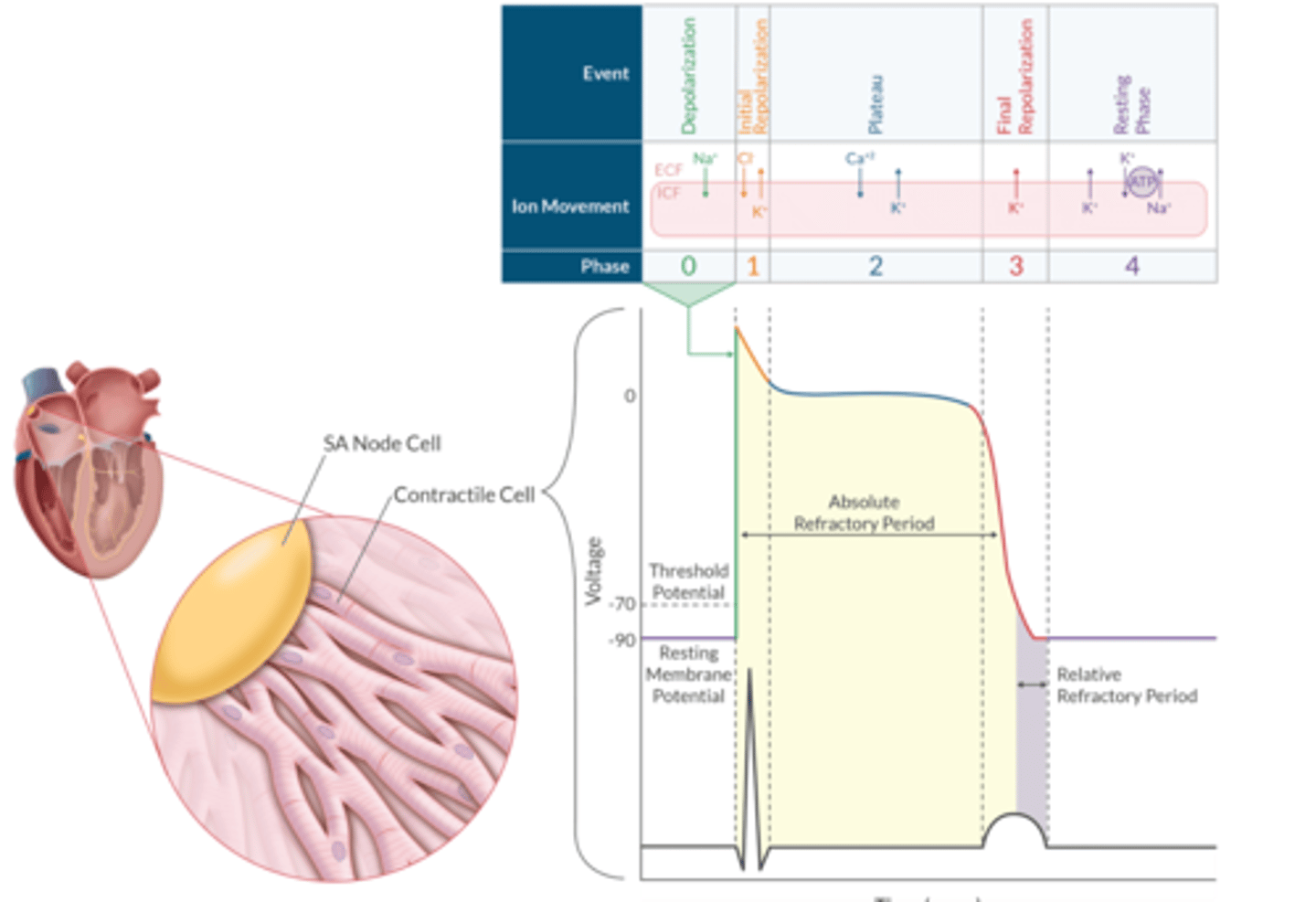
Myocyte Action Potential (Apex Chart)
Describe the Conduction Tissue AP Pathway through the Heart
SA Node--> Internodal Tracts --> AV node --> Bundle of His --> Left and Right BB --> Purkinje Fibers
SA Node Action Potential contains how many phases?
3 ( Phase 4, 0, 3)
What is the RMP for the SA node AP?
-60 mV (HIGHER!!)
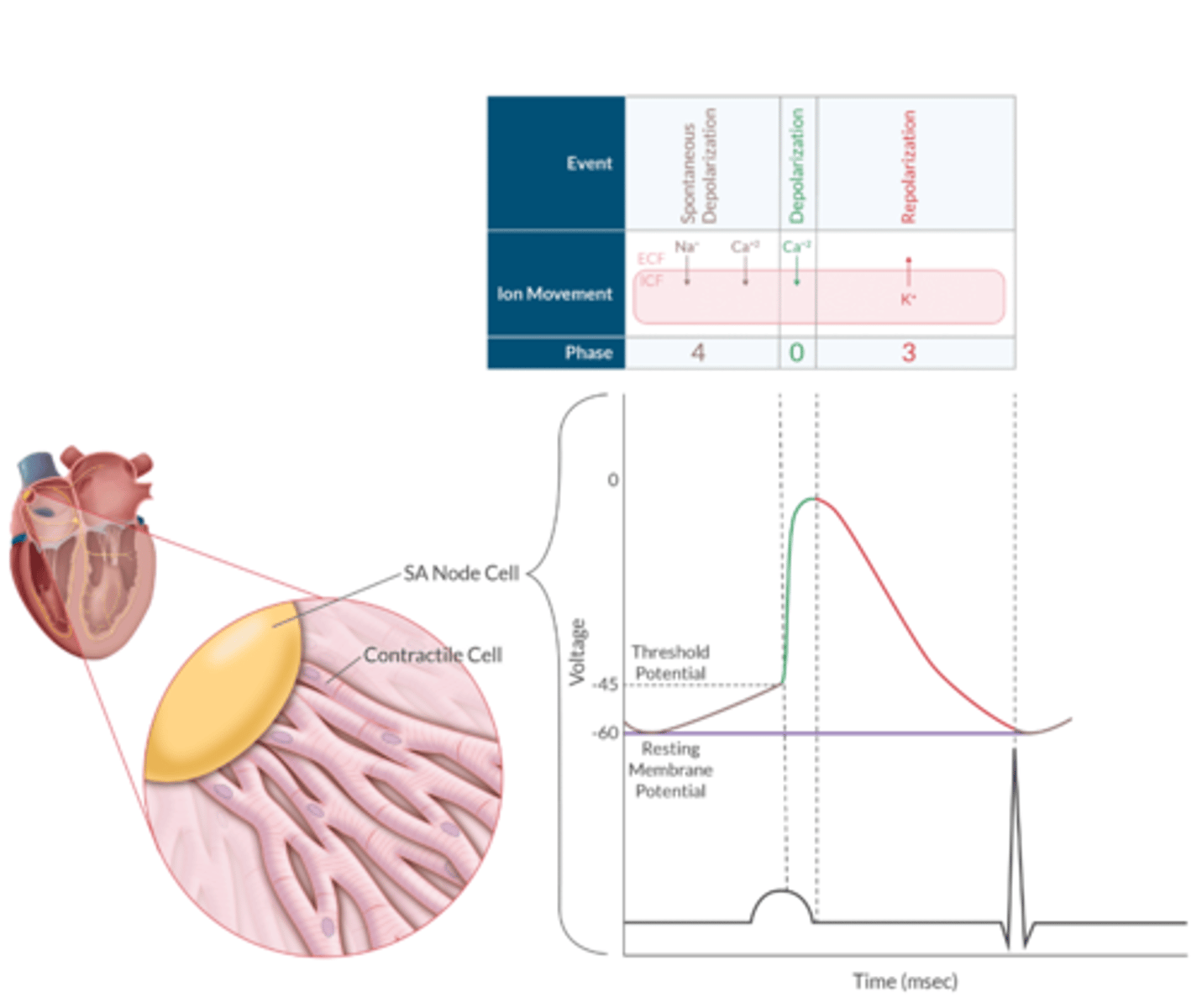
SA Node AP Apex Chart
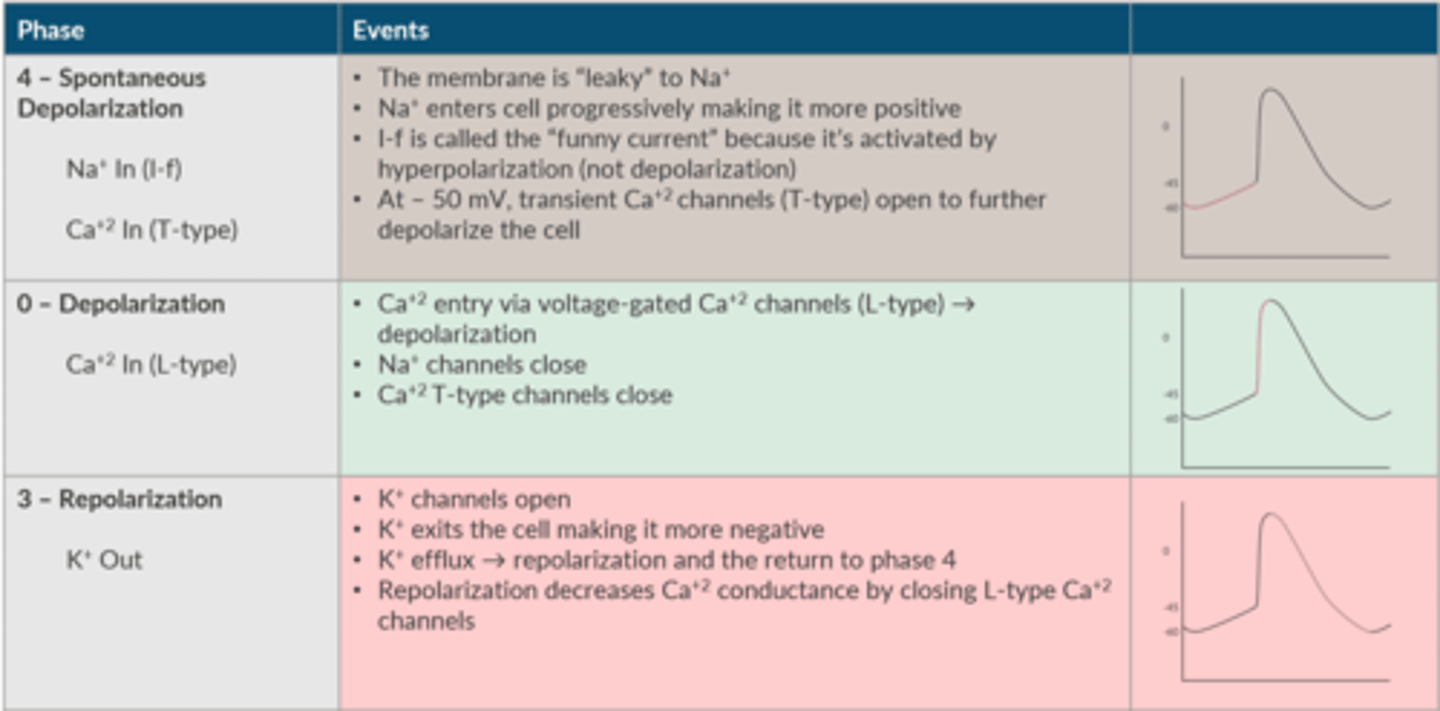
Phase 4 of SA AP is termed what?
Ion movement during this phase?
Spontaneous Depolarization ( Na+ in (I-f), Ca+ In (T-type))
- the membrane is "leaky" to Na+
-Na+ enters cell progressively making it more positive
-I-f is called the "funny current" because it's activated by hyperpolarization (NOT depolarization)
-At -50mV, transient Ca+2 channels (T-type) open to further depolarize the cell
Phase 0 of SA AP?
Ion movement?
Depolarization- Ca+ In (L- type)
-Ca+2 entry via VG- Ca+2 channels (L-type)--> DEPOLARIZATION
-Na+ channels close
-Ca+2 T-type channels close
Phase 3 of SA AP
ion movement
Repolarization
-K+ channels open
-K+ exits the cell making ti more negative
-K+ efflux --> repolarization and the return to phase 4
-Repolarization decreases Ca+2 conductance by closing L-type Ca_2 channels
What helps re-establish the SA node AP gradient after repolarization?
NA/K-ATPase pump
What determines the heart rate? (2)
1. Intrinsic firing rate of the dominant pacemaker (usually the SA node)
2. Autonomic tone (At rest, PNS exceed SNS tone)
Where does the SA node reside?
in the right atrium
What is another name for the SA node?
Keith-Flack node
The rate of ___________________________ of the SA node determines the intrinsic HR
spontaneous PHASE 4 DEPOLARIZATION
What happens if disease or hypoxia of the SA node impairs it's ability to fire?
The cell with the next highest rate of spontaneous phase 4 depolarization will assume the pacemaker responsibility.
This explains why a junctional rhythm is slow and does not have a P wave. Volatile anesthetics depress SA node automaticity, which explains why these agents can cause a junctional rhythm
What innervates the SA node?
RIGHT vagus (CN 10)
What innervates the AV node?
LEFT vagus nerve
What are the cardiac accelerator fibers for SNS tone?
T1-T4
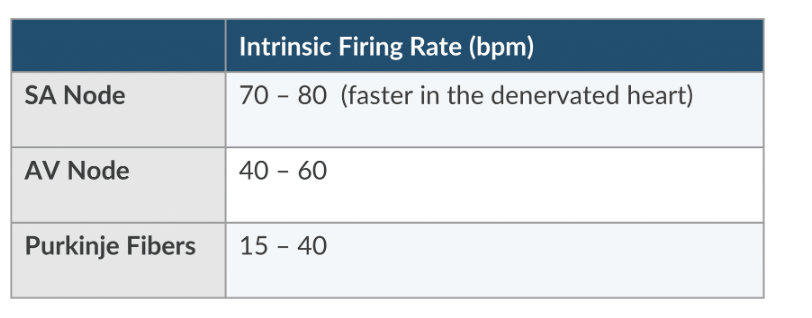
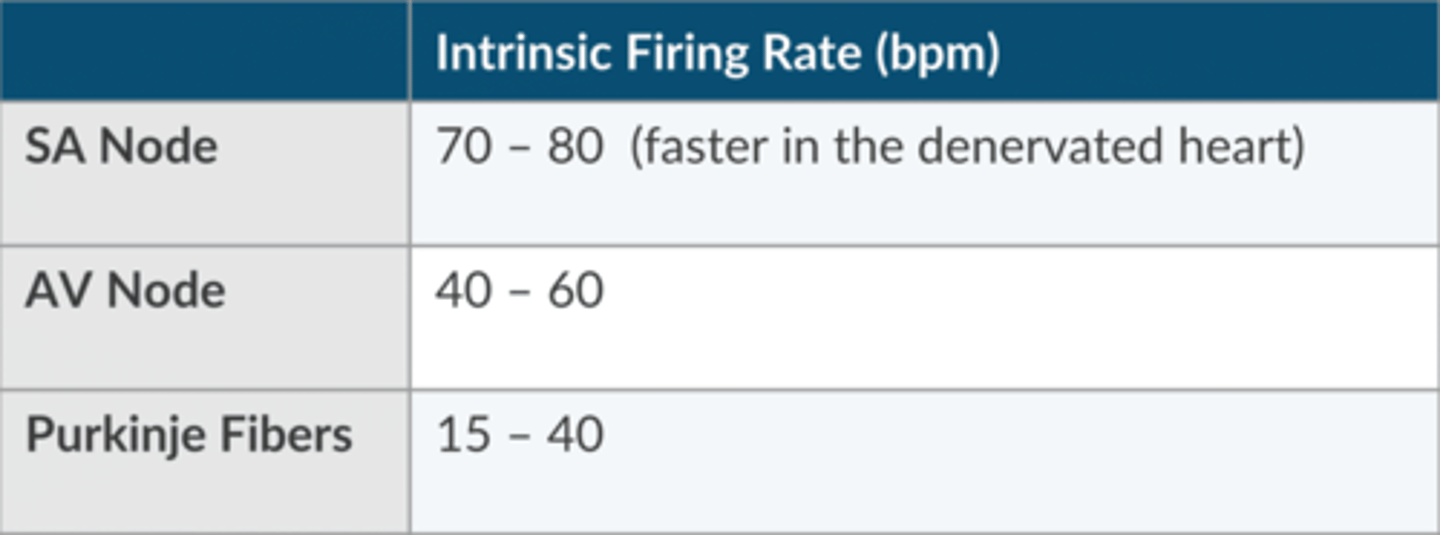
What is the normal intrinsic firing rate of the SA node?
70-80 (faster in the denervated heart) bpm
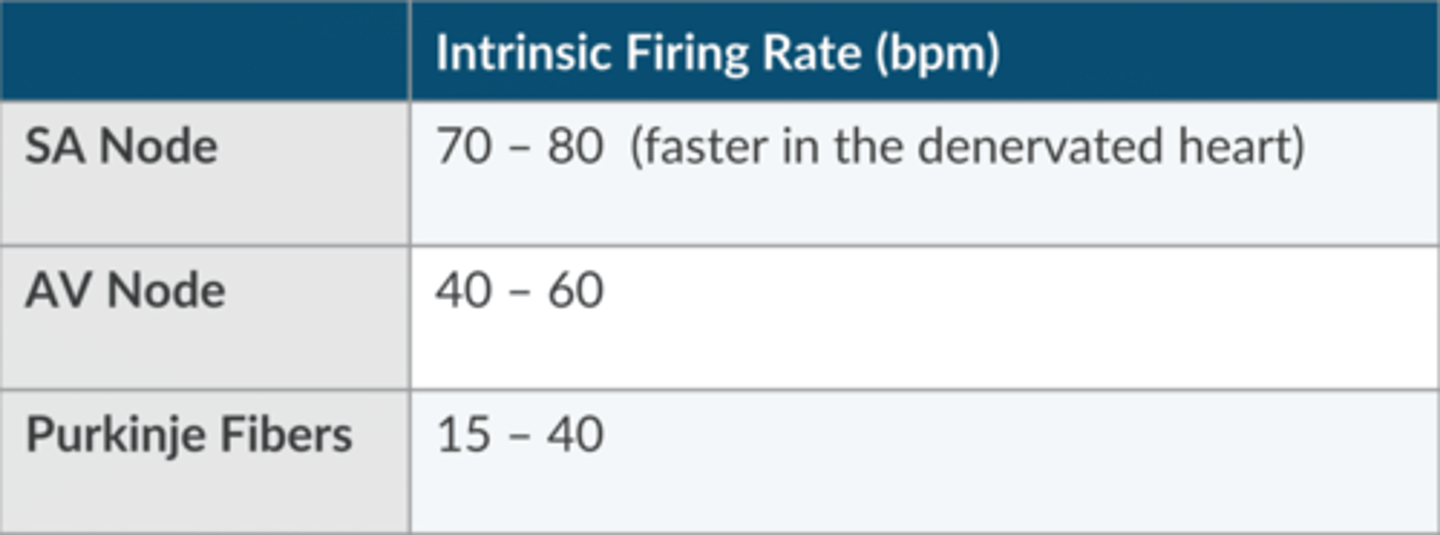
What is the normal intrinsic firing rate of the AV node?
40- 60 bpm
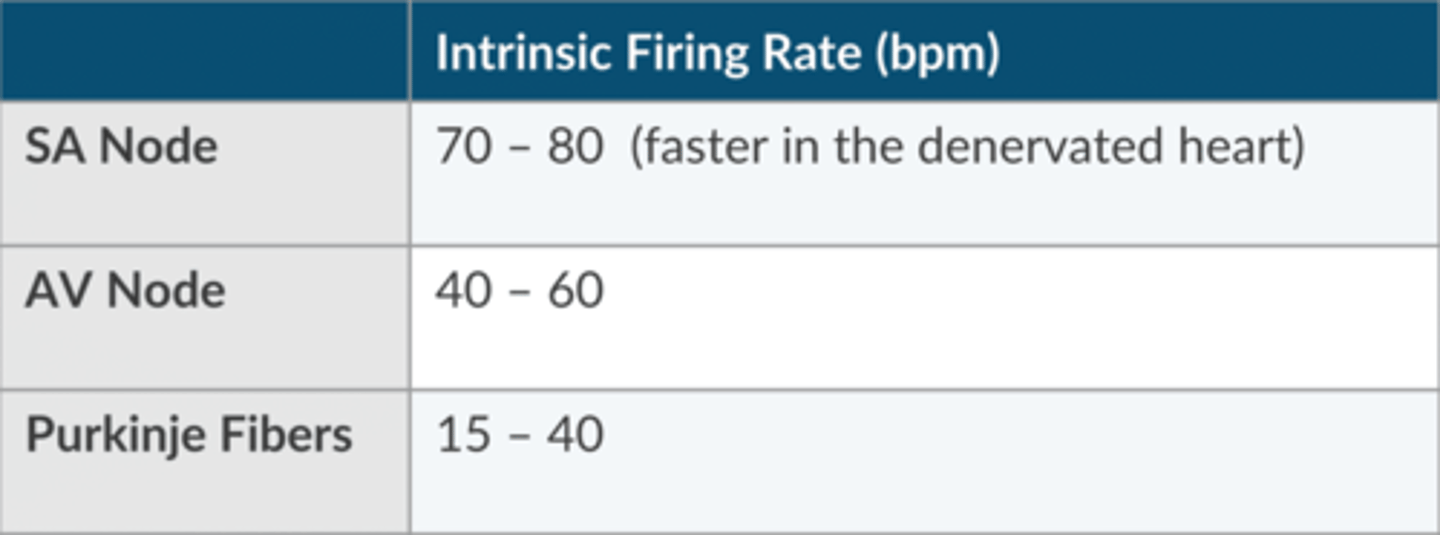
What is the normal intrinsic firing rate of the Purkinje Fibers?
15-40 bpm
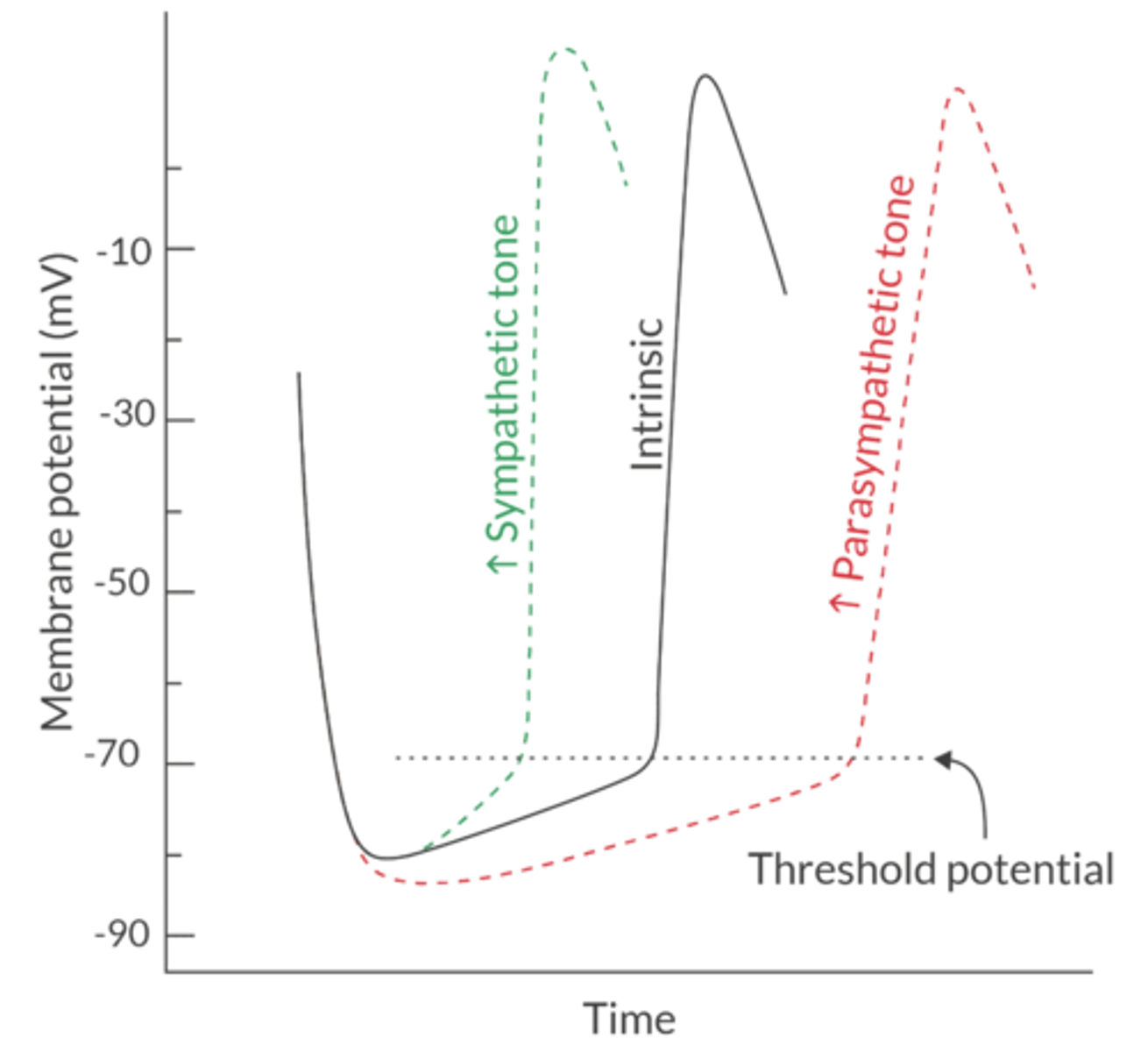
What 3 variables can be manipulated to change the sinus node rate?
1. the rate of spontaneous phase 4 depolarization
2. Threshold potential
3. RMP
How does SNS autonomic tone affect HR?
NOREPINEPHRINE stimulates beta-1, which INCREASES NA+ and Ca+ conductance
This increases the slope of spontaneous phase 4 depolarization
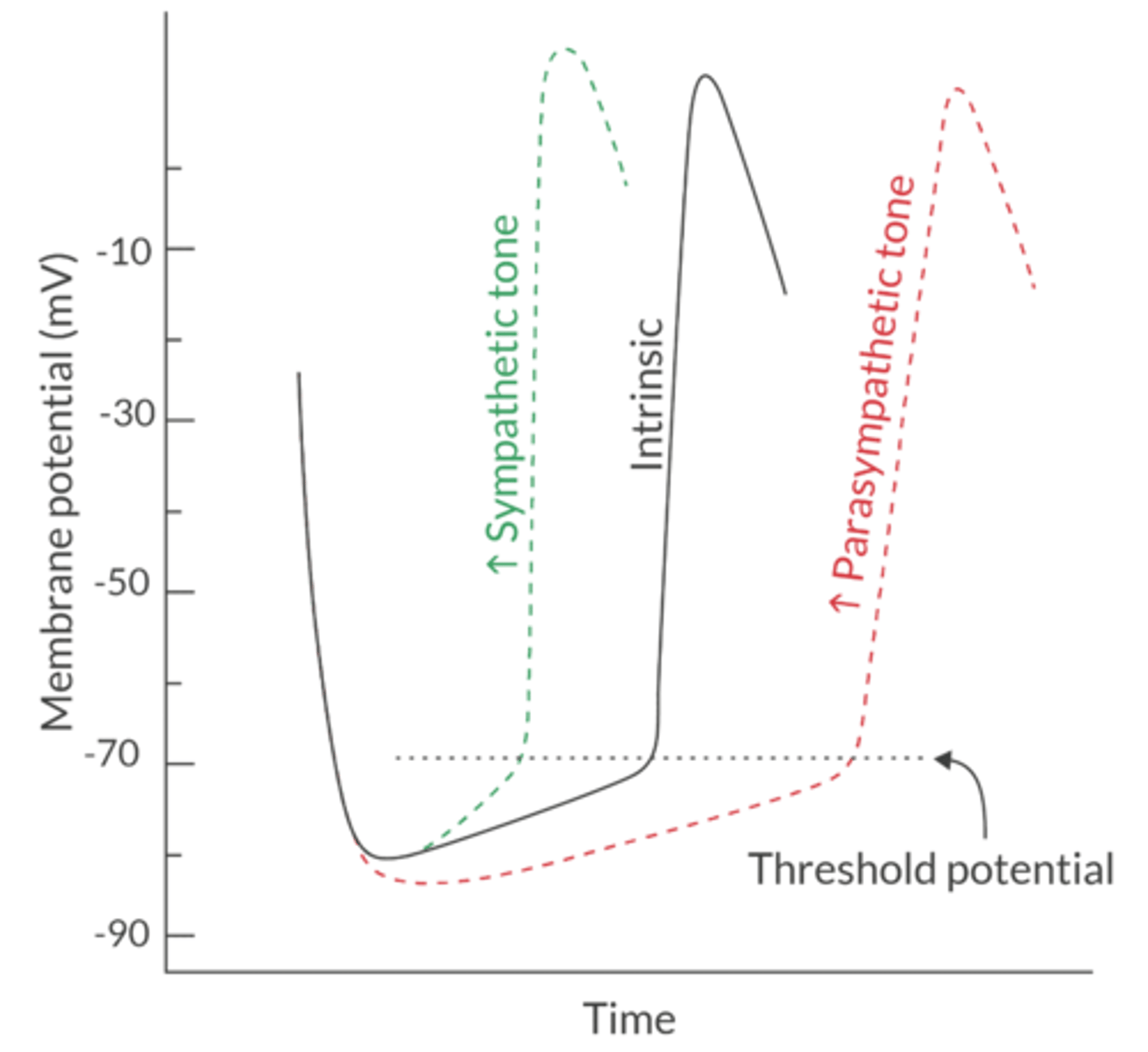
How does PNS autonomic tone affect HR?
Acetylcholine stimulates the muscarinic-2 receptor, which slows the HR by increasing K+ conductance and hyperpolarizing the SA node
This decreases the RMP and reduces the slope of spontaneous phase 4 depolarization (notice the less steep curve in the picture)
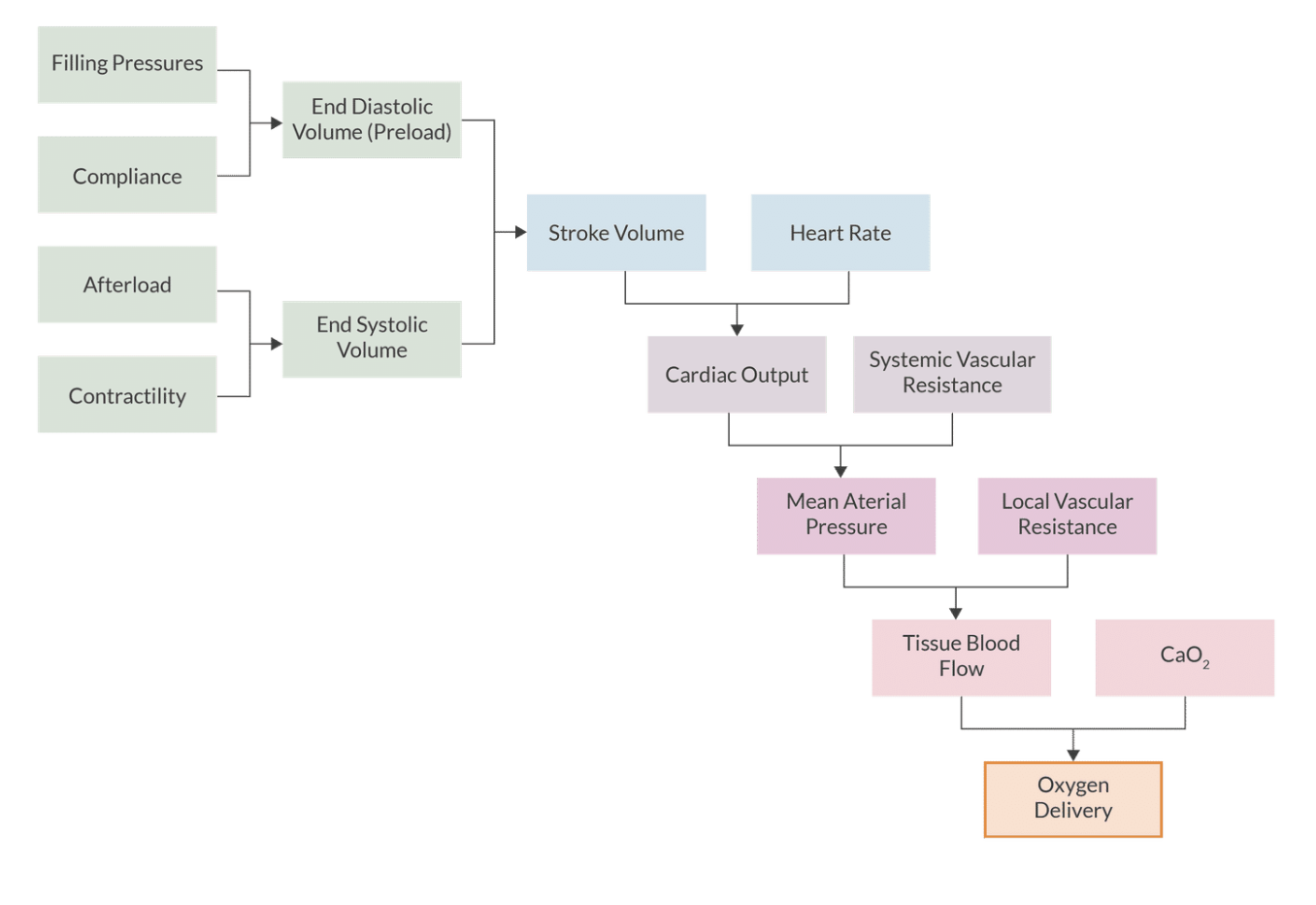
What does CaO2 tell us?
O2 carrying capactiy- tells us how many grams of O2 are contained in a deciliter of arterial blood
What is the DO2 Equation?
CO x (CaO2 x 10)
Normal CaO2 value
20 mL/dL
DO2 describes what?
delivery of O2 to the tissues
what is the CaO2 Equation?
Oxygen carrying capacity
(Hbg x SaO2 x 1.34) + (PaO2 x 0.003)
What is a Normal DO2
DO2= CO x CaO2 x 10
1000 mL/min
What is EO2?
Oxygen extraction ratio
how much oxygen is the body using
EO2 Equation
CaO2- CvO2. = EO2
CaO2
25% (whole-body)
VO2 describes the bodies?
Oxygen Consumption
What is the VO2 normal value
250 mL/min or 3.5 mL/kg/min
CVO2 is the?
Venous Oxygen Content
CvO2 equation
(Hb x 1.34 x SvO2) + (PvO2 x 0.003)
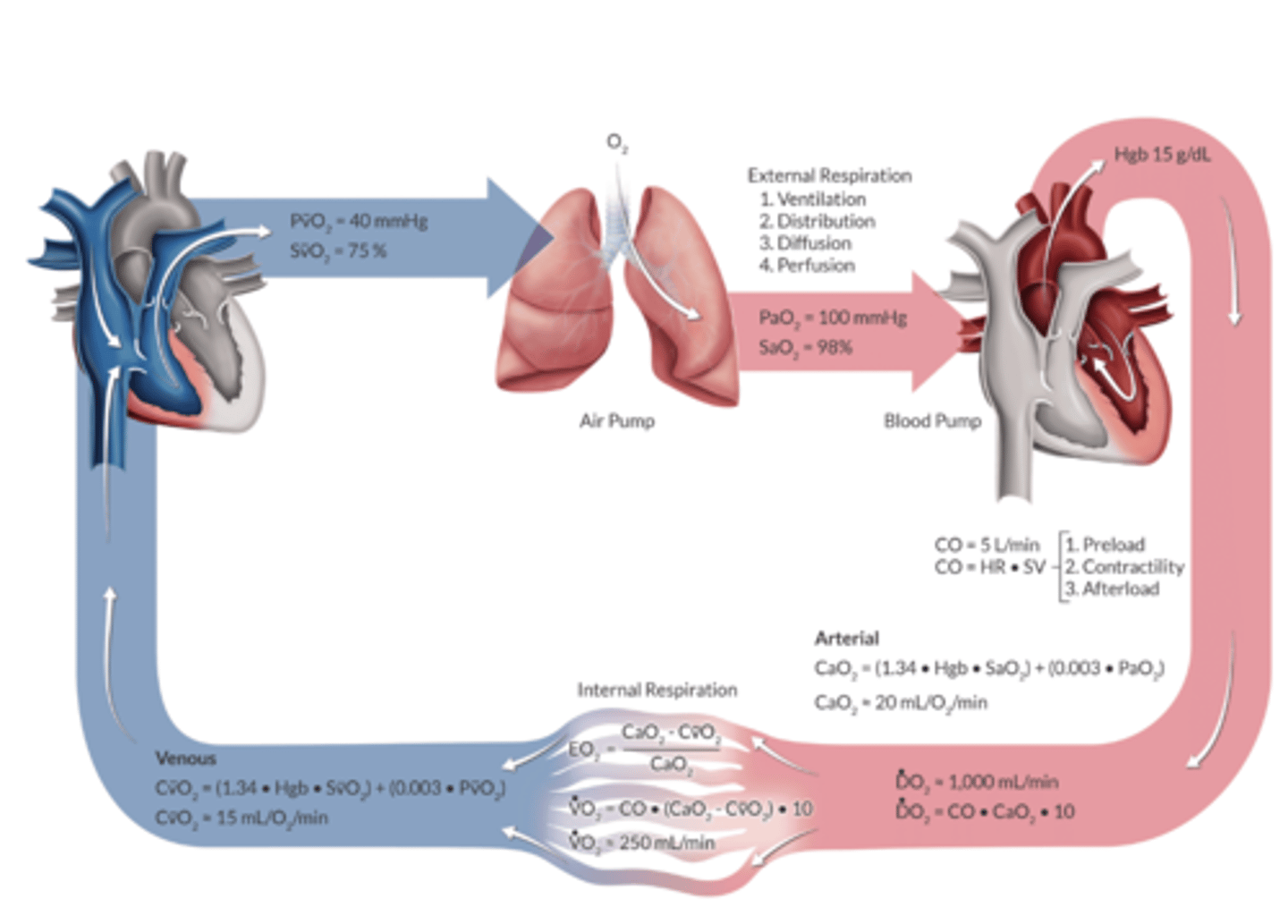
Venous Oxygen Content Normal Value
15 mL/dL
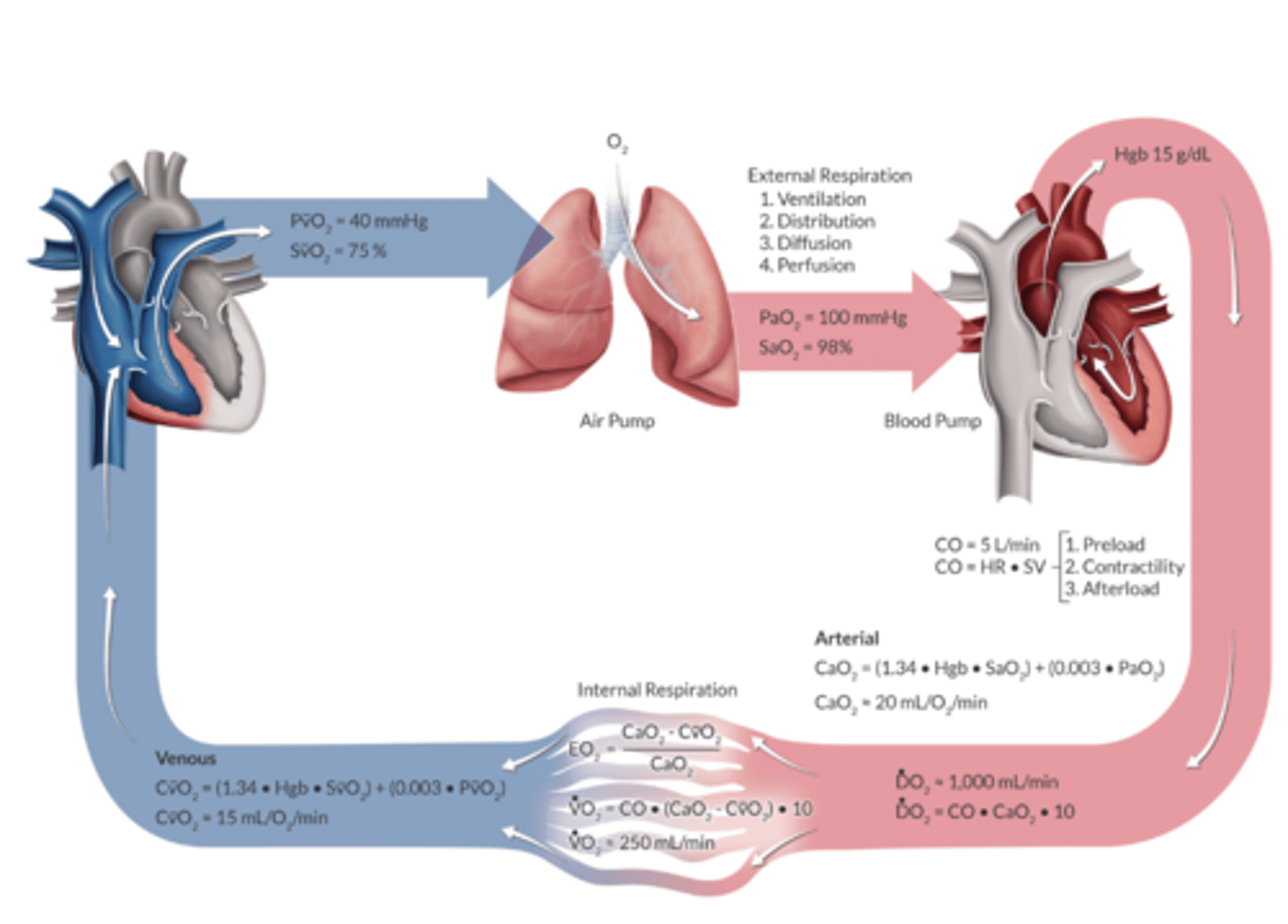
PaO2 is the?
The amount of oxygen dissolved in blood
PaO2 follows what law?
Henry's
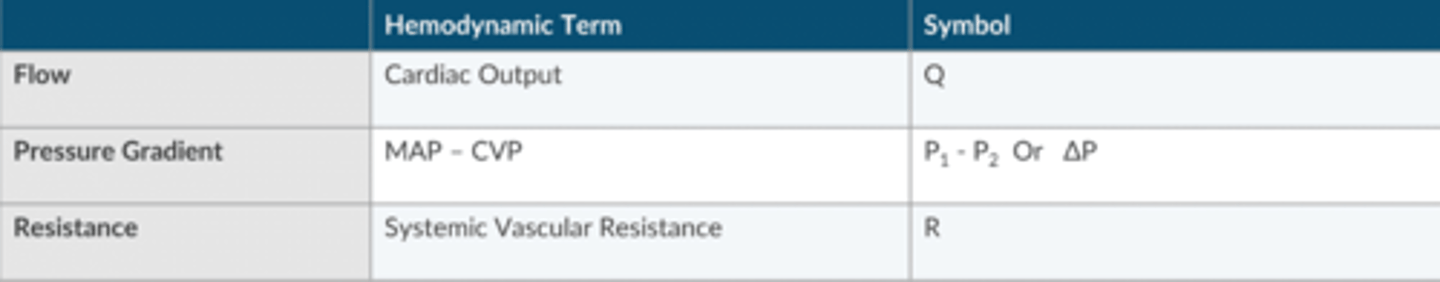
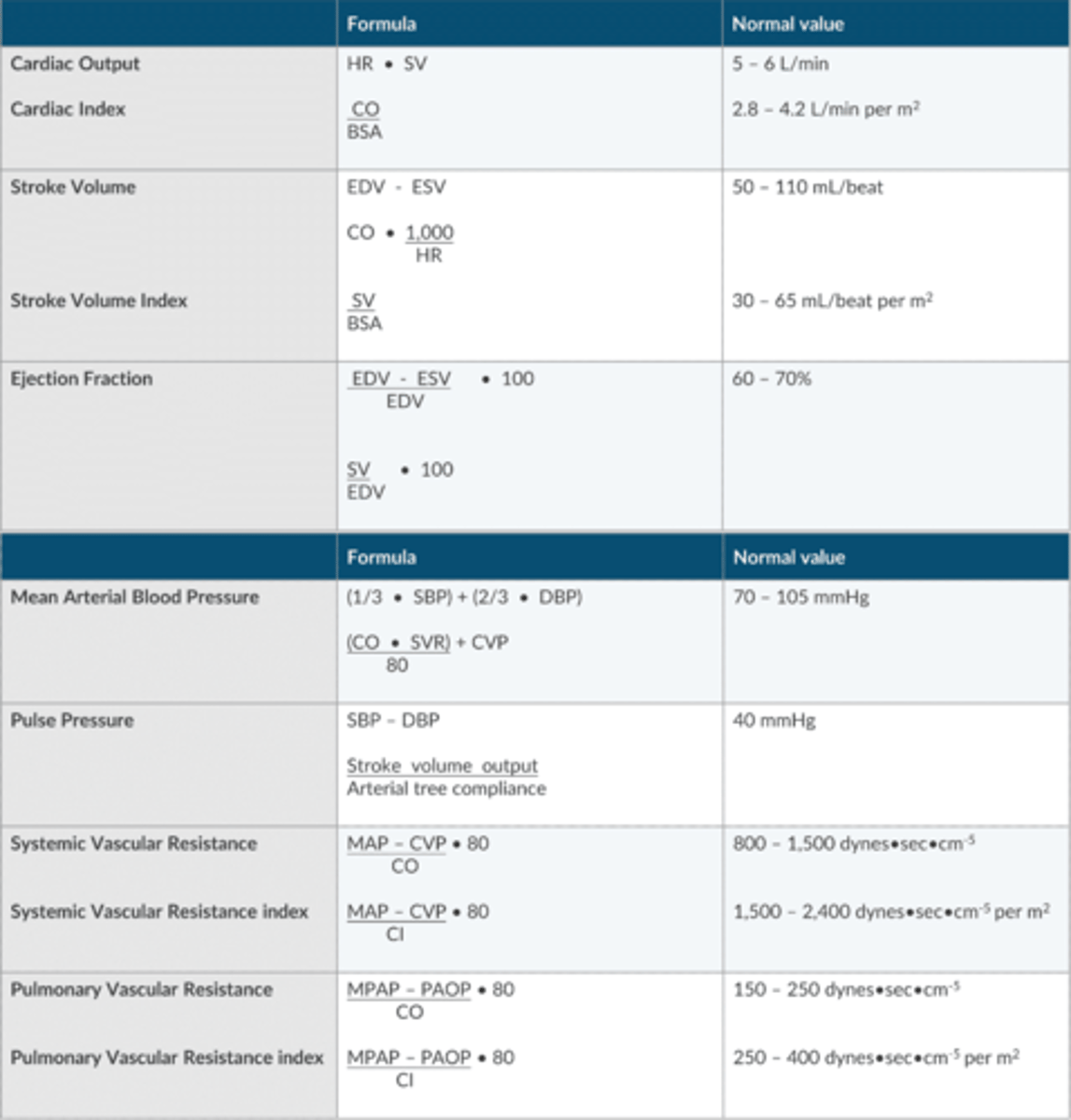
Ohm's Law
Current= Voltage Difference/ Resistance
OR
Flow=Pressure Gradient/Resistance
Apex Table for Ohm's Law Variables
MAP Equation using SVR
(CO x SVR)/ 80 + CVP
What is Poiseuille's Law?
flow rate = ΔP(πr^4 / 8Lη)
Q = dP/R
flow rate depends on pressure difference, and radius, length, and viscosity of liquid
increased resistance can be caused by increased length, increased viscosity, or decreased radius
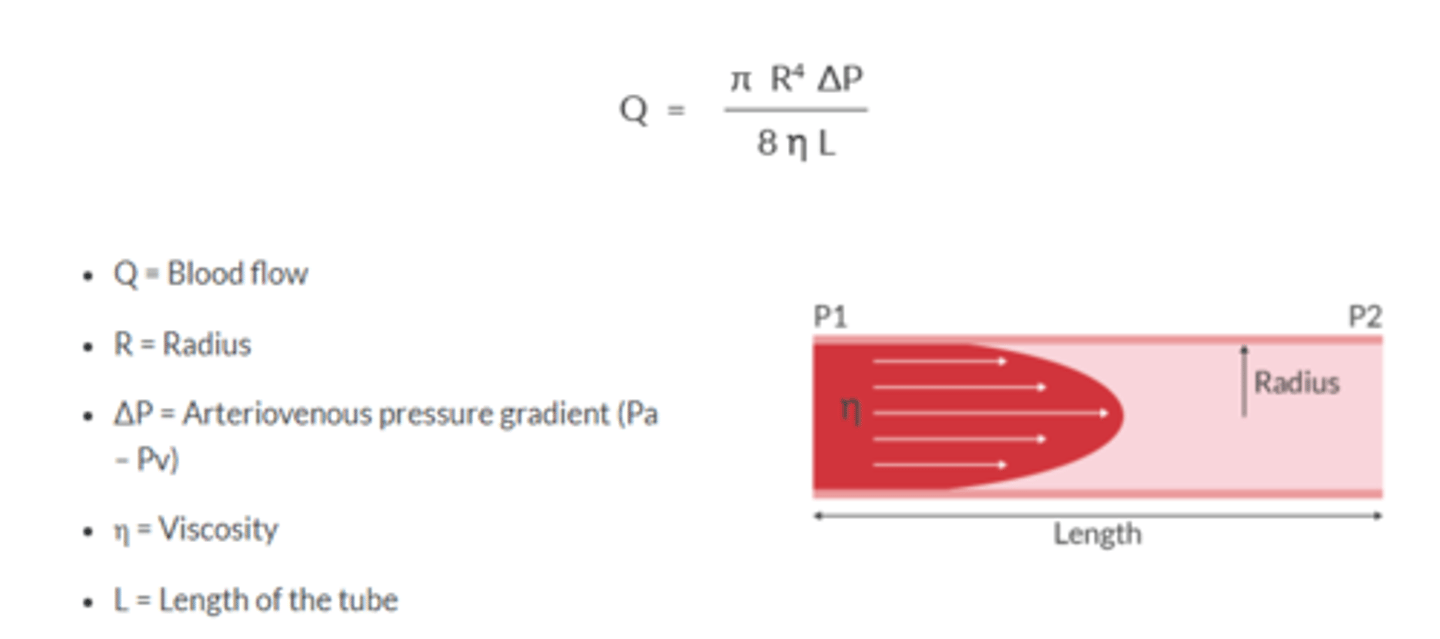
Vascular resistance is determined by ___ of artierioles
Radius
DOubling radius —> flow increases 16 fold
Tripling the radius—> flow increases 81 fold
Quadrupling the radius—> flow increases 256 fold
Laminar Flow
molecules travel in a parallel path through the tube
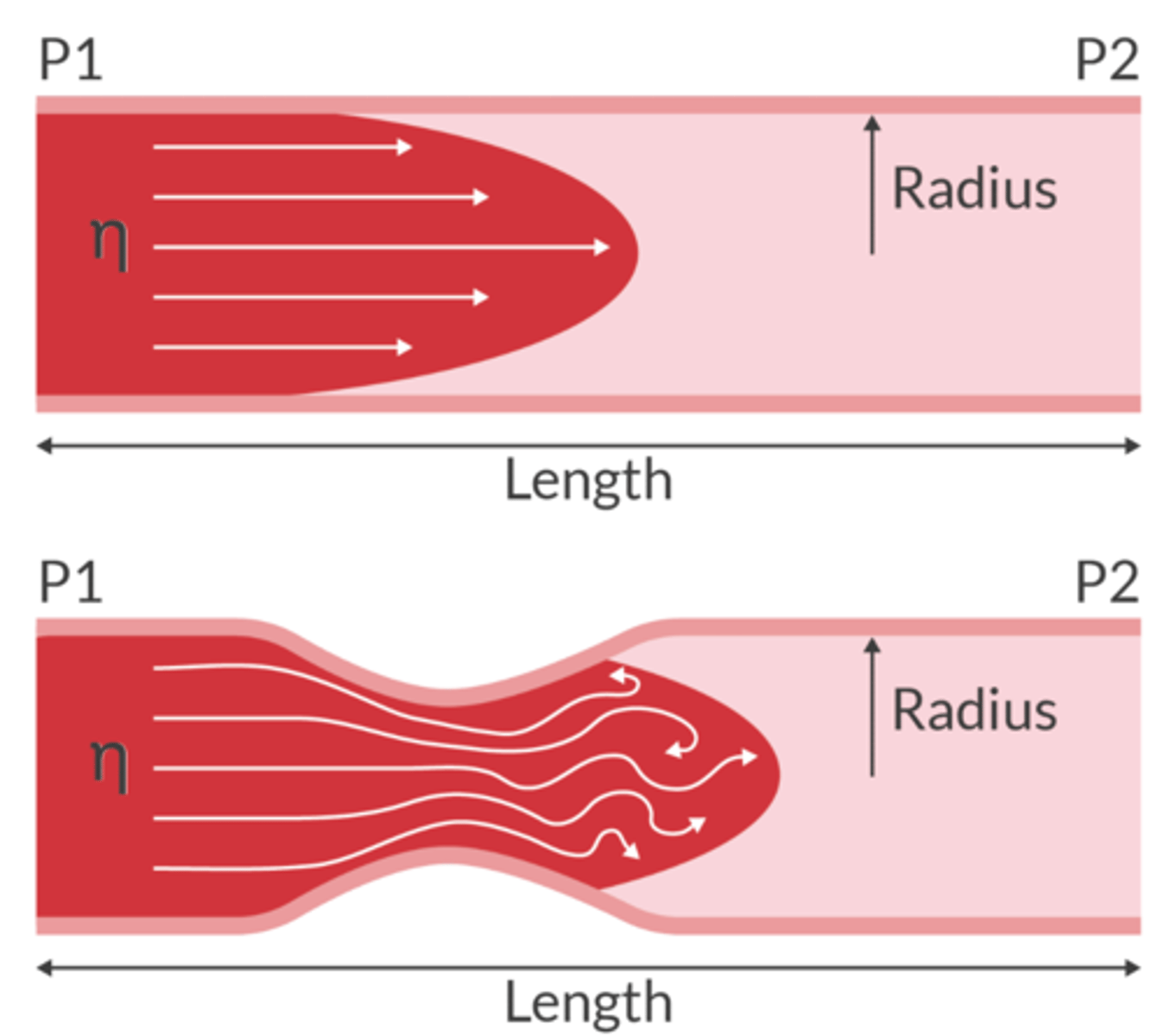
Turbulent Flow
molecules travel in a non-linear path and will create eddies
When flow is turbulent, lots of neergy is lost to heat and virbrations. (can produce a mumur)
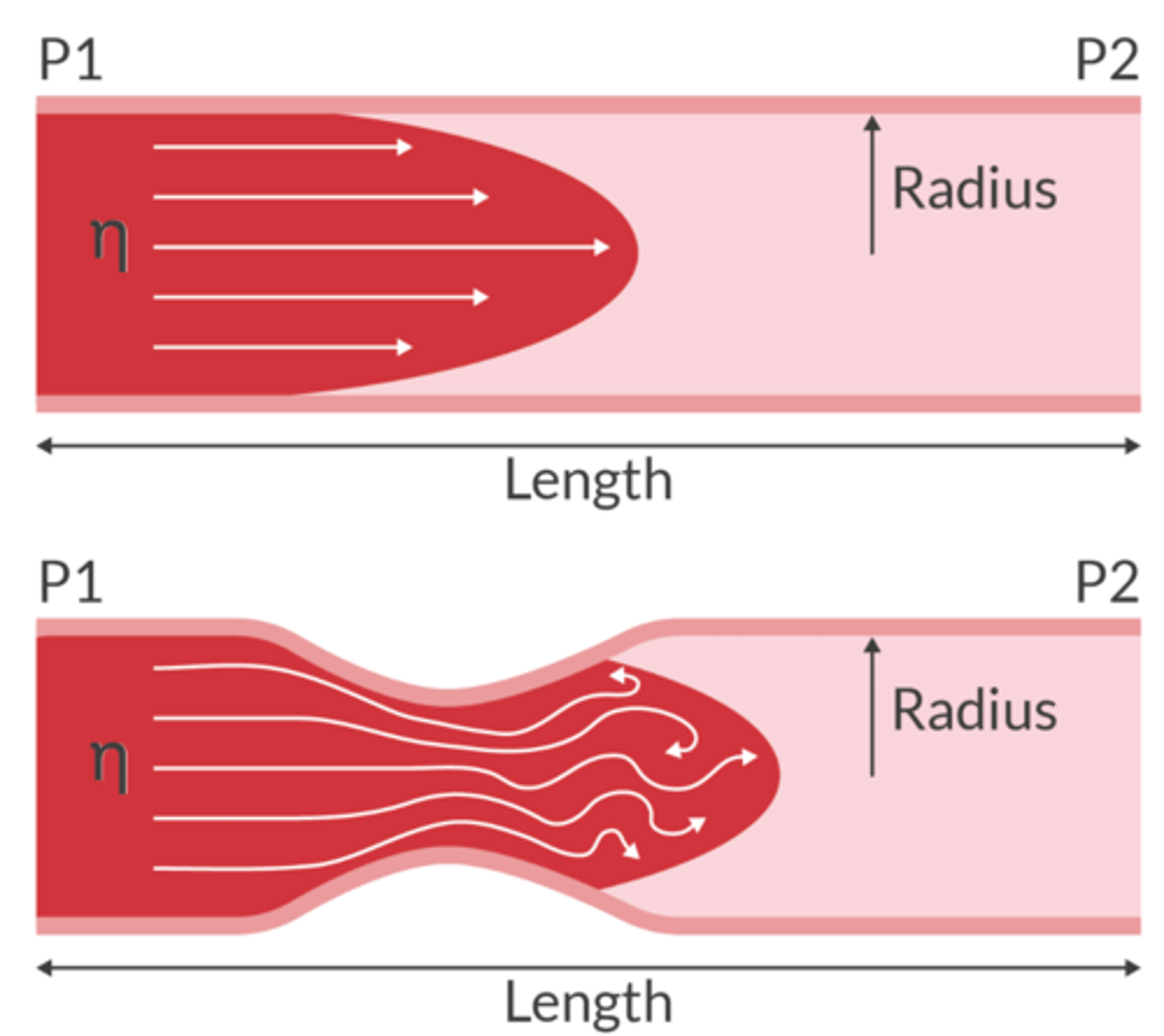
Transitional Flow
Laminar flow along the vessel walls with turbulent flow in the center
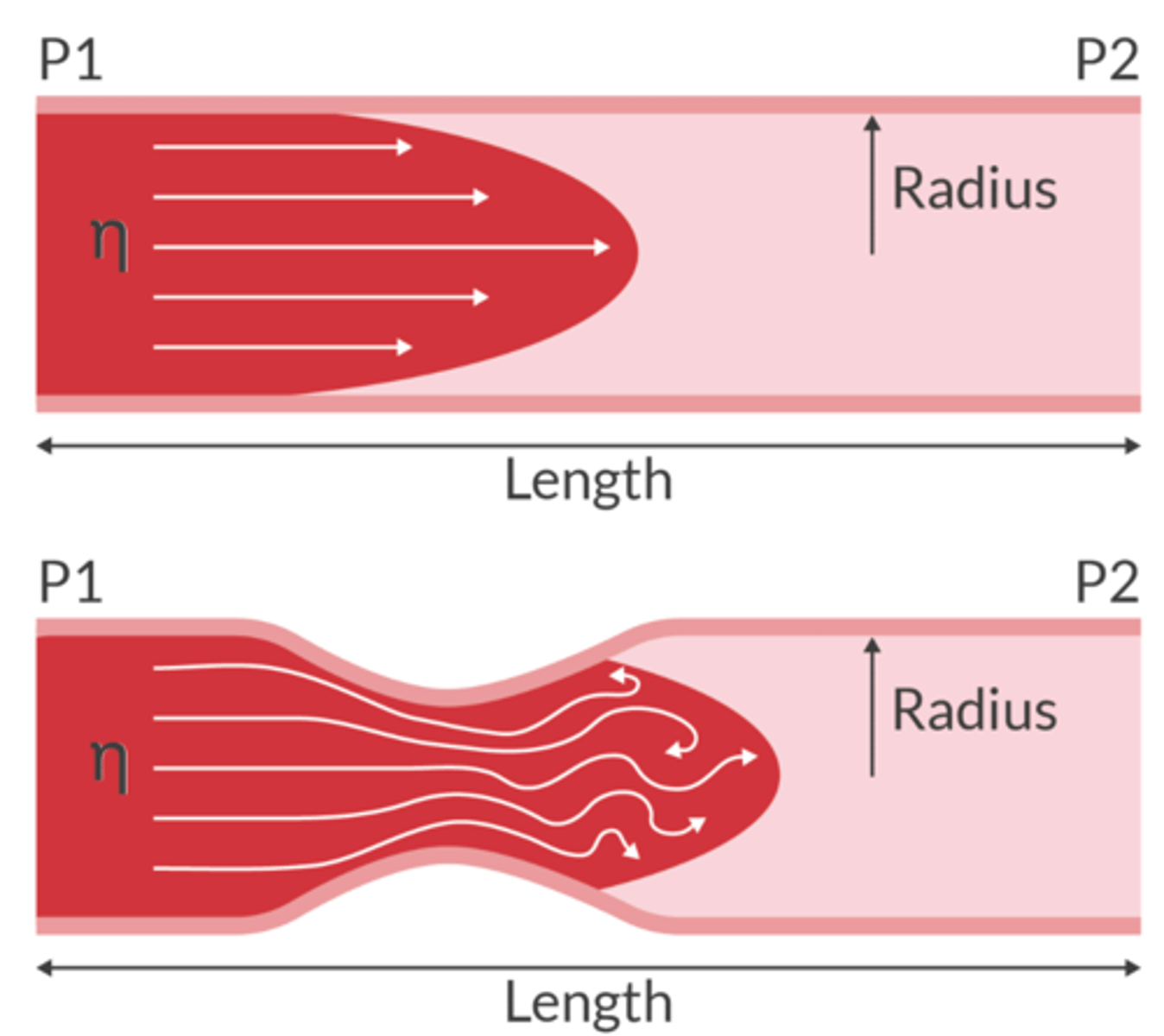
Reynold's Number tells us what about flow?
used to predict if the flow will be laminar or turbulent
-Re <2000 = flow will be mostly laminar
-Re >2000 = flow will be mostly turbulent
- Re = 2,000-4,000 suggests transitional flow
The result of friction from the intermolecular forces as a fluid passes through a tube
Viscosity
What is blood viscosity determined by in the human body?
hematocrit and body temperature
Viscosity of blood is ________________ proportionate to temperature
INVERSELY PROPORTIONATE
Apex table for Hemodynamic Formulas/Variables
Interrelationship between hemodynamic variables
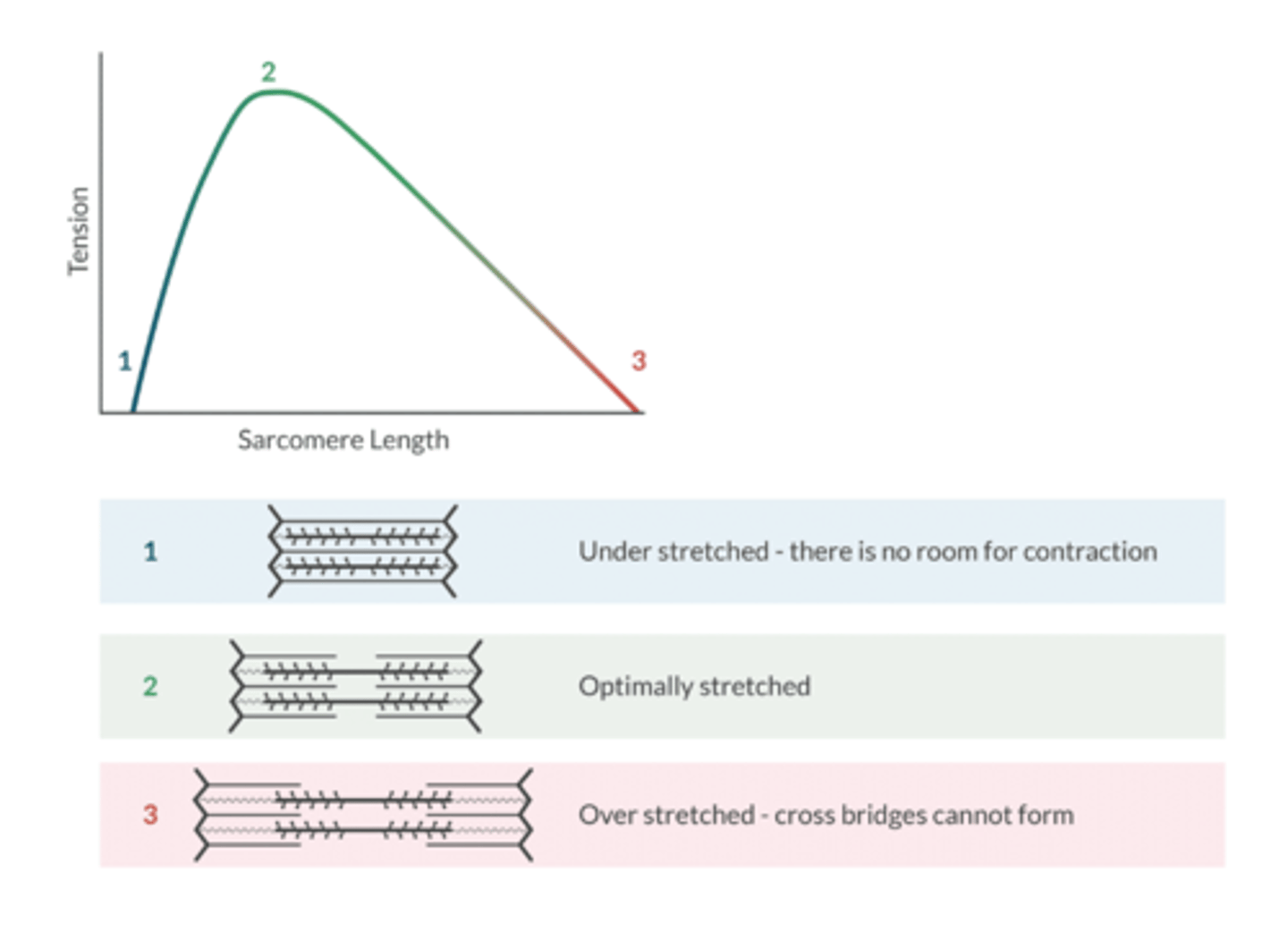
What is the functional unit of the contractile tissue in the heart?
sarcomere
Factors that influence preload: (7)
Blood volume- hypovolemia reduces preload
Atrial kick- atrial fib reduces preload
Venous tone- sympathectomy reduces preload
Intrapericardial pressure- pericardial tamponade reduces preload
Intrathoracic pressure- dynamic hyperinflation reduces preload
Body position- reverse Trendelenburg reduces preload
Valvular Regurgitation- aortic or mitral insufficiency INCREASES preload
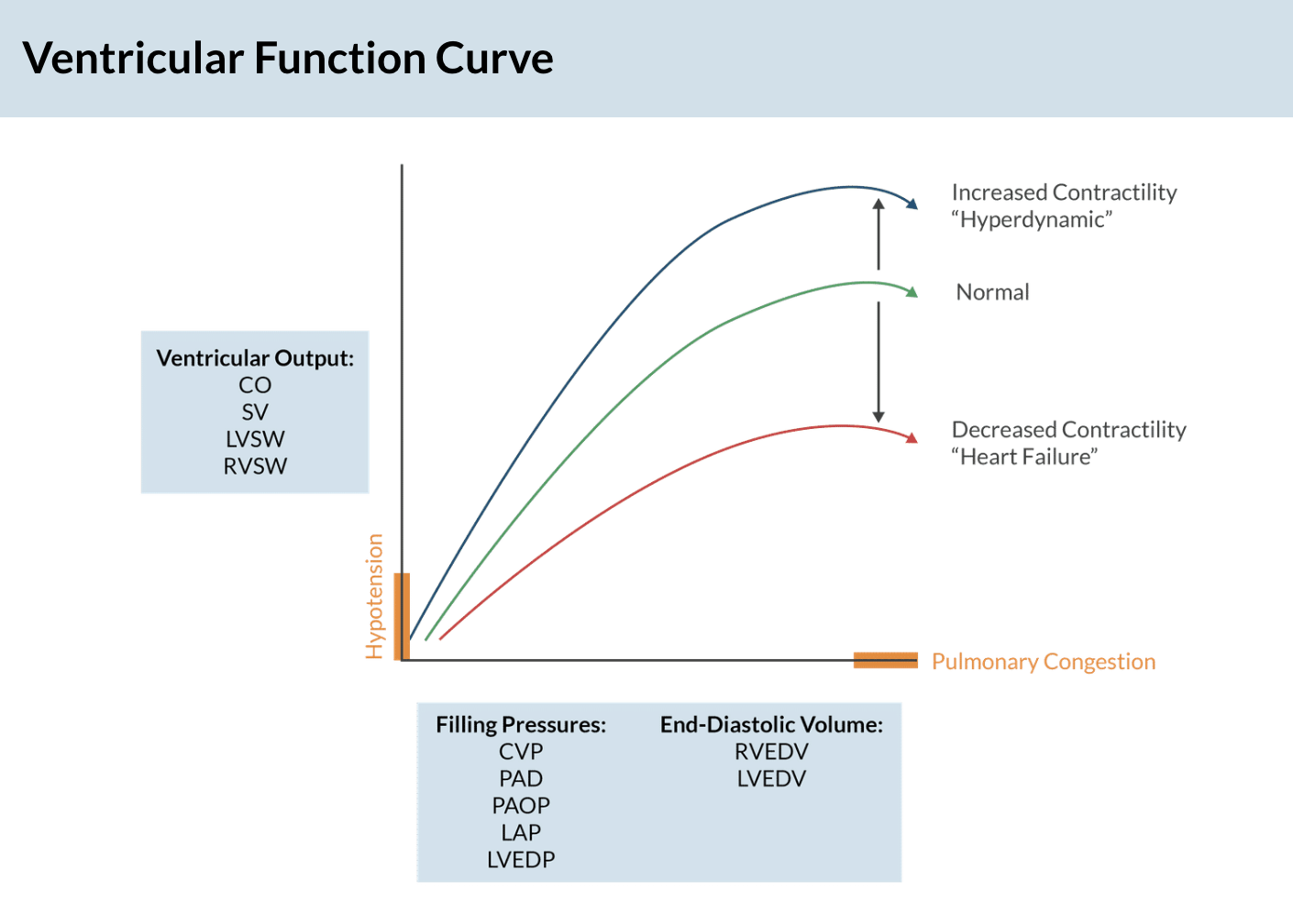
Ventricular Function Curve (apex )
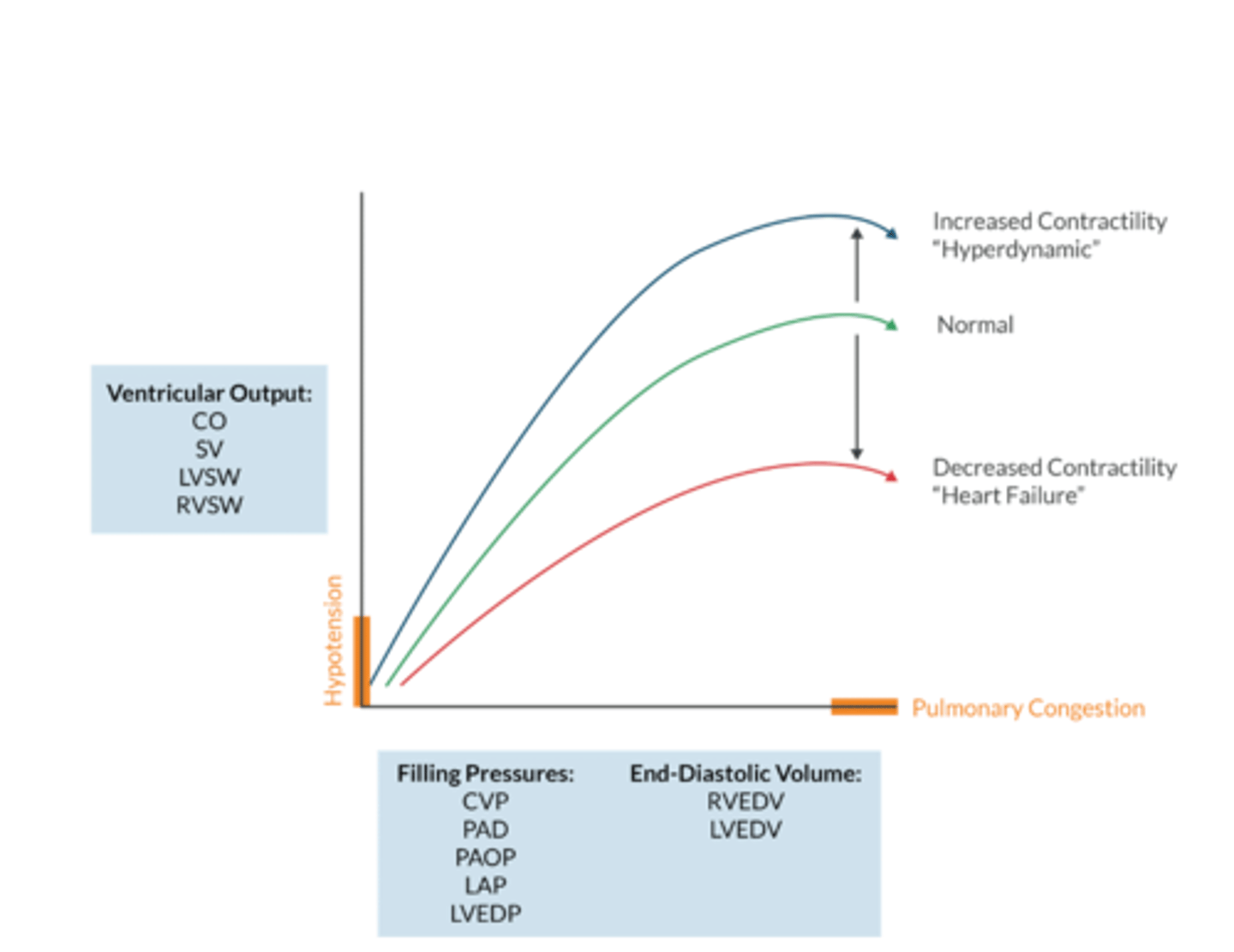
What does the ventricular function curve represent?
The Frank-Starling Mechanism- an increased ventricular volume produces a larger Cardiac output (to a point)
Contractility is _________________ of preload and afterload
INDEPENDENT
- an increase preload increases the force of contraction (Starlings Law) but this is NOT the same as contractility
Whats on the Y axis of the ventricular function curve? (4)
Ventricular output:
CO
SV
LVSW
RVSW
what's on the x axis of the ventricular function curve? (2)
Filling Pressures:
-CVP
-PAD
-PAOP
-LAP
-LVEDP
End Diastolic Volume:
-RVEDV
- LVEDV
What % does atrial kick contribute to LVEDV (aka CO by extention)
20-30%
W/ a-fib, CO declines as a result
Conditions associated with reduced myocardial compliance include...(4)
1. hypertrophy
2. HF with preserved EF (diastolic failure)
3. fibrosis
4. aging
-these pts are more likely to experience a reduction in CO with cardiac rhythm disturbances, such as a-fib and junctional
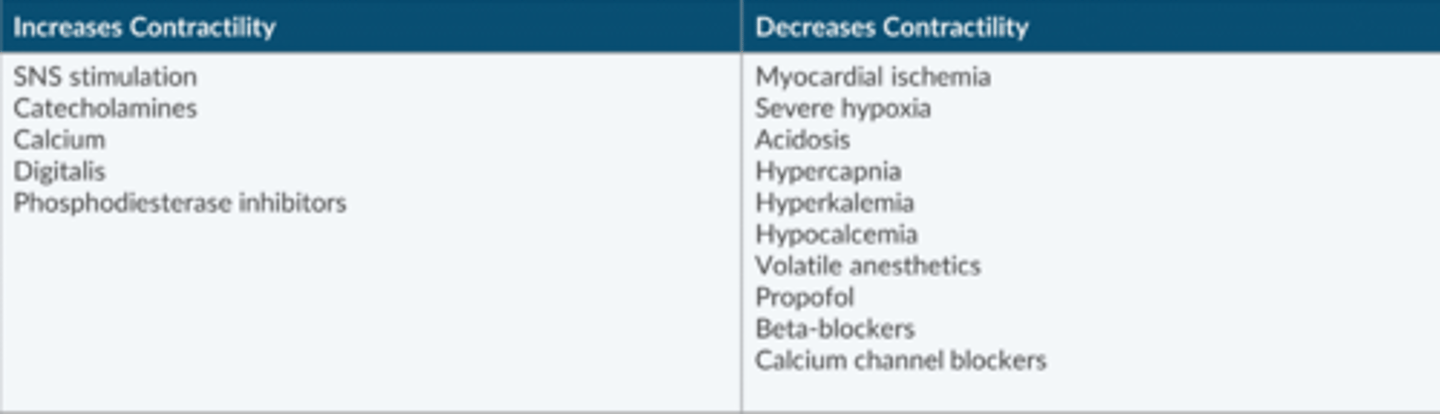
Factors that Influence Contractility:
INCREASES: (5)
Decreases: (10)
**Chemicals affect Contractility- particularly Calcium**
Increases Contractility:
-SNS stimulation
-catecholamines
-Calcium
-Digitalis
-Phosphodiesterase Inhibitors
Decreases Contractility:
-MI
-Severe hypoxia
-Acidosis
-Hypercapnia
-Hyperkalemia
-Hypocalcemia
-Volatile anesthetics
-Propofol
-Beta-blockers
-Calcium channel blockers
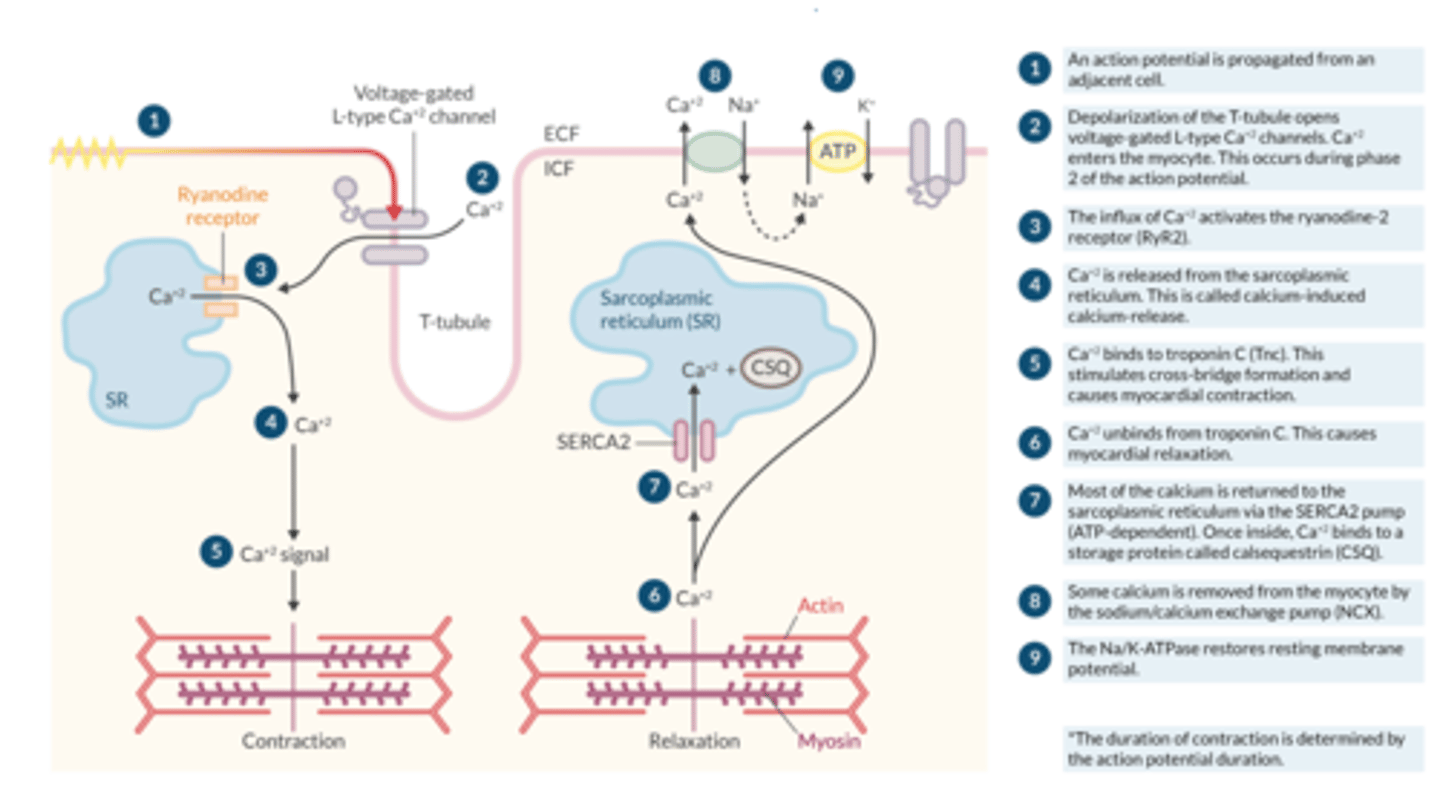
Excitation-contraction Coupling (Apex Picture Step by Step)
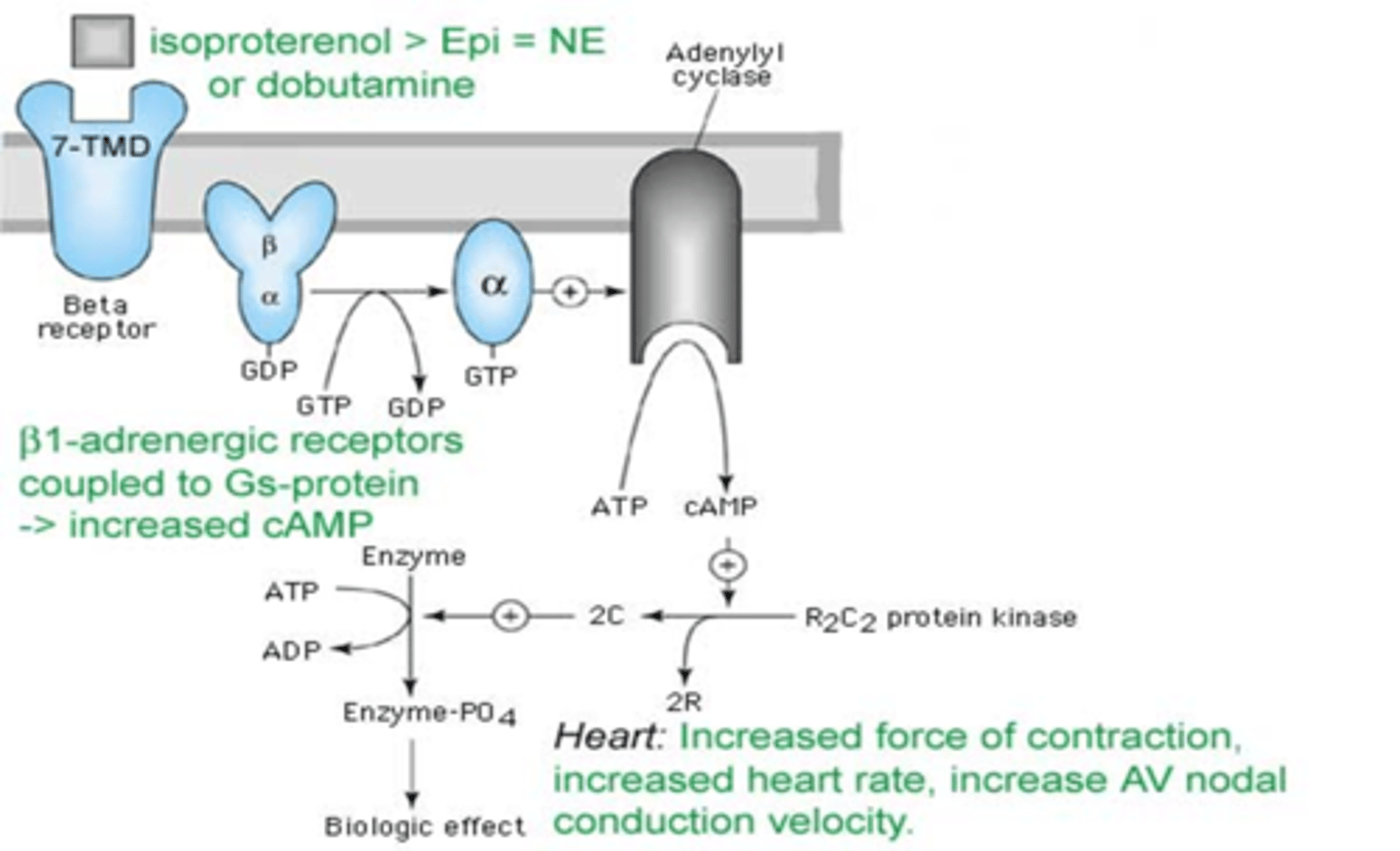
How does beta-1 stimulation increase contractility
(Gs aka cAMP pathway)
By activating adenylate cyclase, which converts ATP to cAMP.
cAMP increases the activation of protein kinase A (PKA). Activated PKA phosphorylates proteins and accomplished 3 tasks:
1. Activation of more L-type Ca+2 channels (more Ca+2 enters the cell)
2. Stimulation of the ryanodine-2 receptor to release more calcium (more calcium is made available to TnC)
3. Stimulation of the SERCA2 pump to increase Ca+2 uptake (faster rate of Ca+2 uptake in the SR) with subsequent enhanced Ca+2 release
a. Phospholamban (PLN) normally inhibits SERCA2 activity
b. Phosphorylated PLN relieves inhibition of SERCA2--> enhanced Ca+2 uptake
Net effect=more forceful contraction over a shorter period of time
What is Afterload?
The force the ventricle must overcome to eject its stroke volume
What two physiologic diseases set the afterload PROXIMAL to the systemic circulation?
aortic stenosis
Coarctation of the aorta
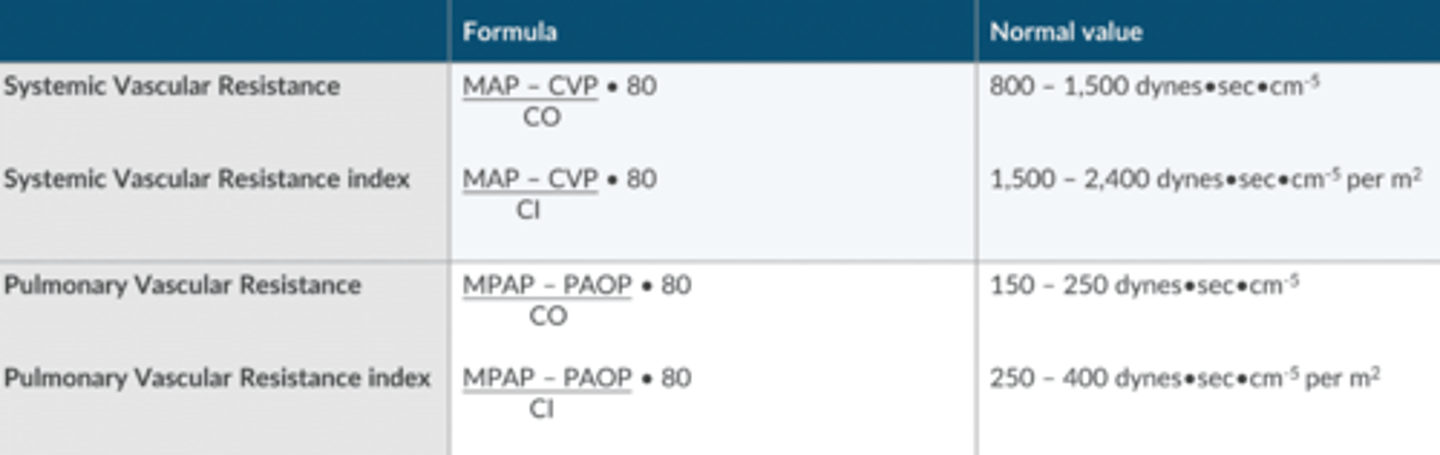
SVR, SVRI and PVR,PVRI Calculations (Apex Chart)
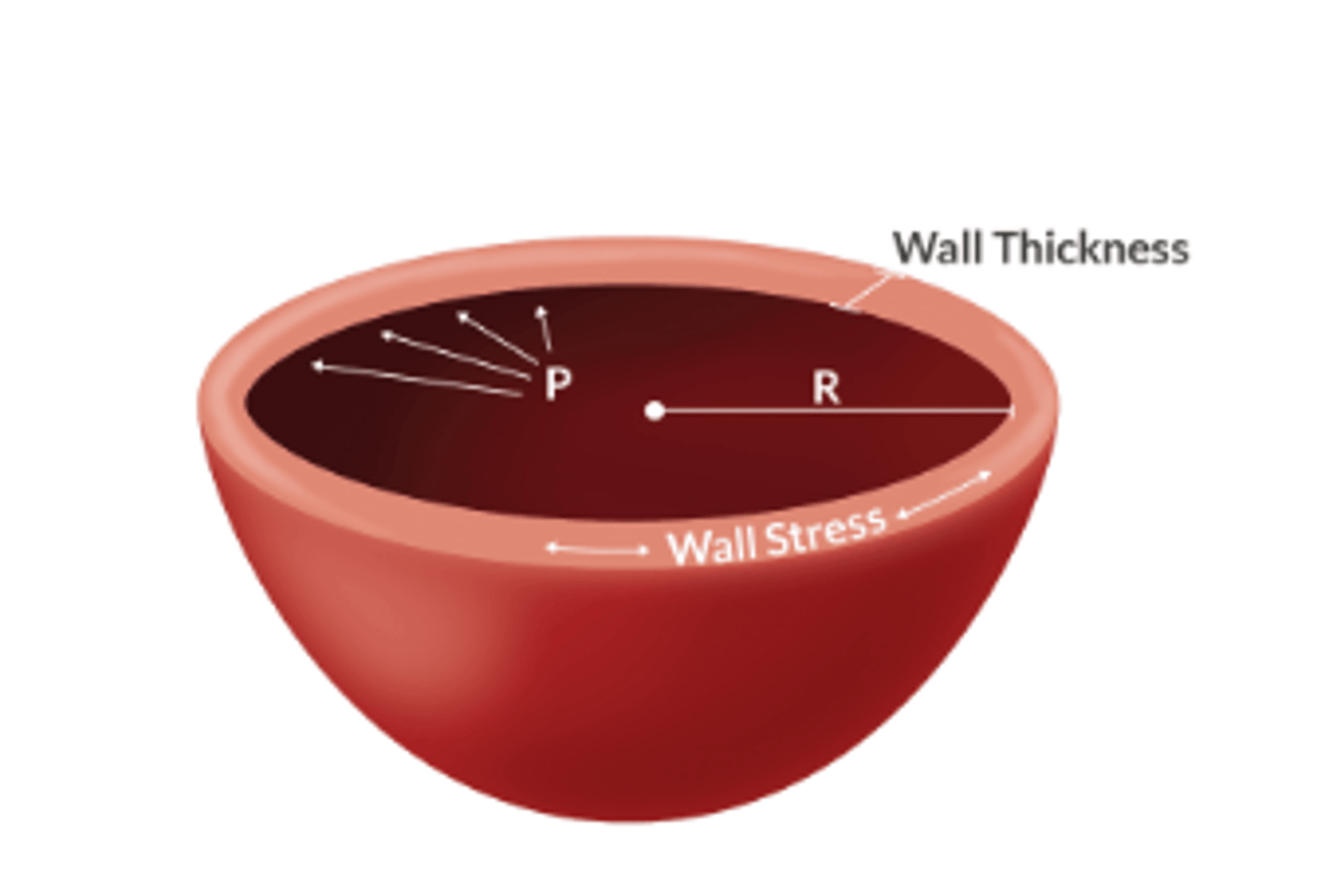
What law can be applied to understand how afterload affects myocardial wall stress?
Law of Laplace