anatomy final - thorax, pelvis, and abdomen high yield
1/302
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
303 Terms
overall shape of thorax
truncated cone, narrow superiorly and widening inferiorly
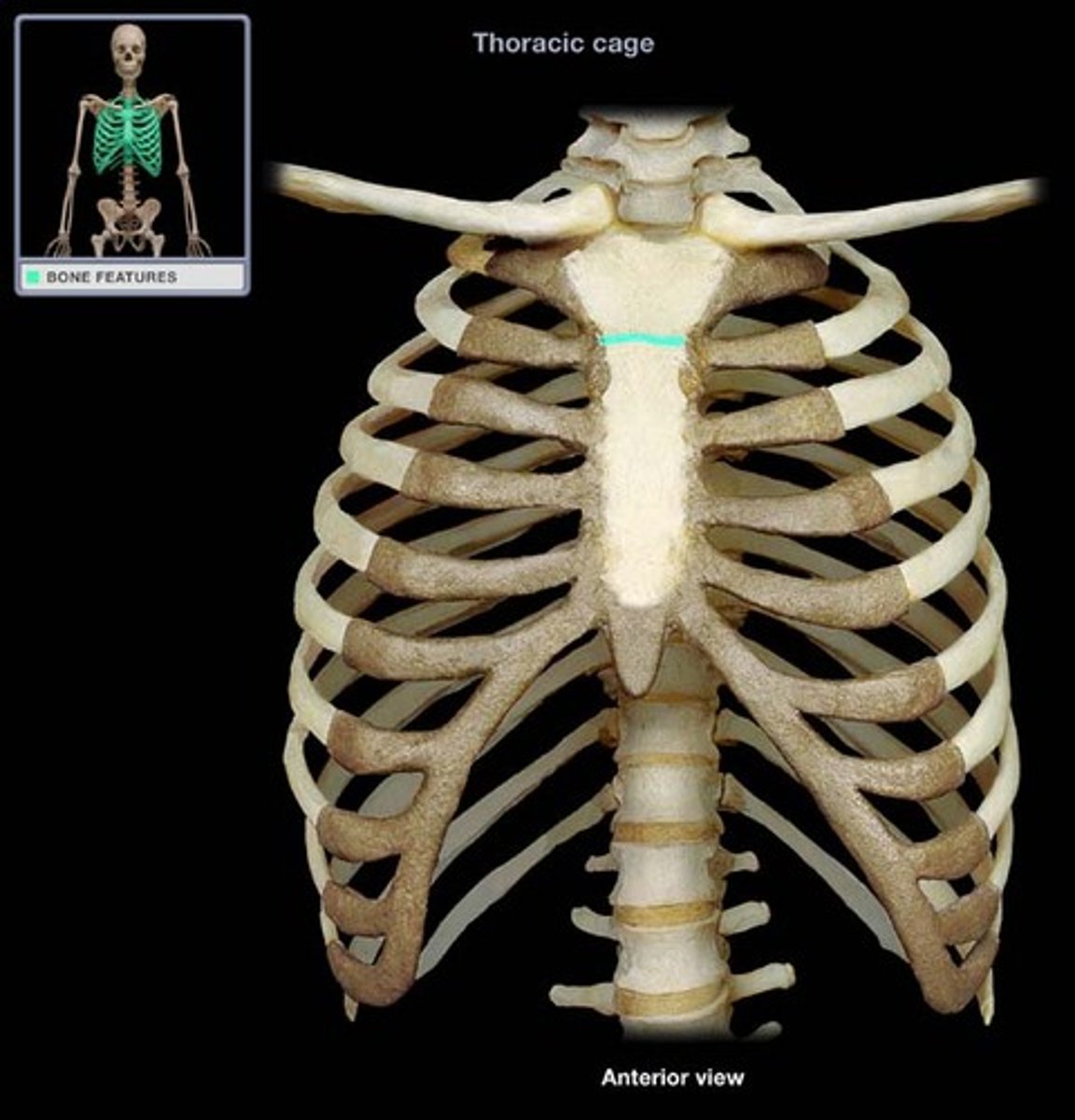
what structures form the boundaries of the bony cage of the thorax
vertebrae posteriorly, ribs laterally, and the sternum anteriorly.
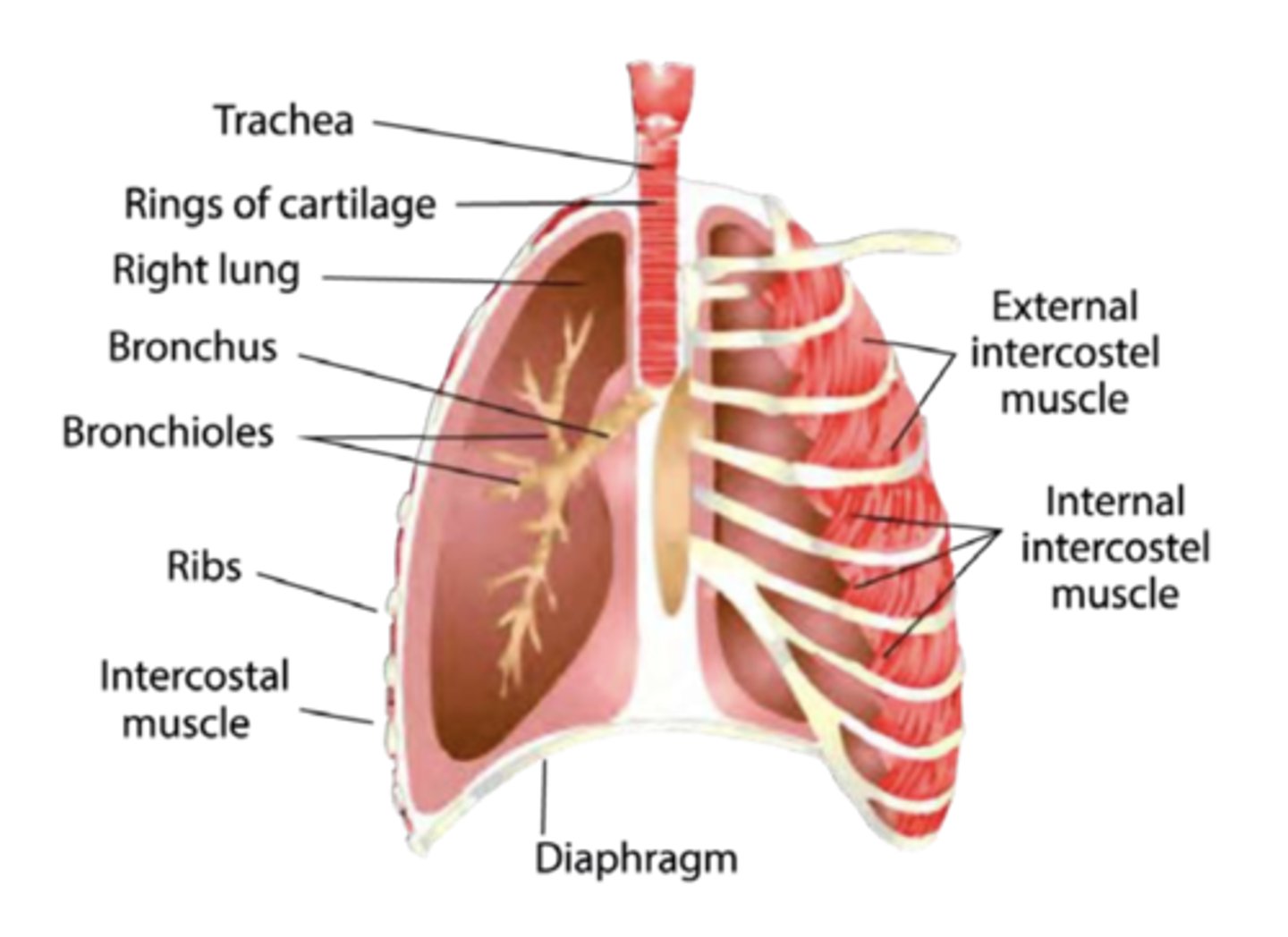
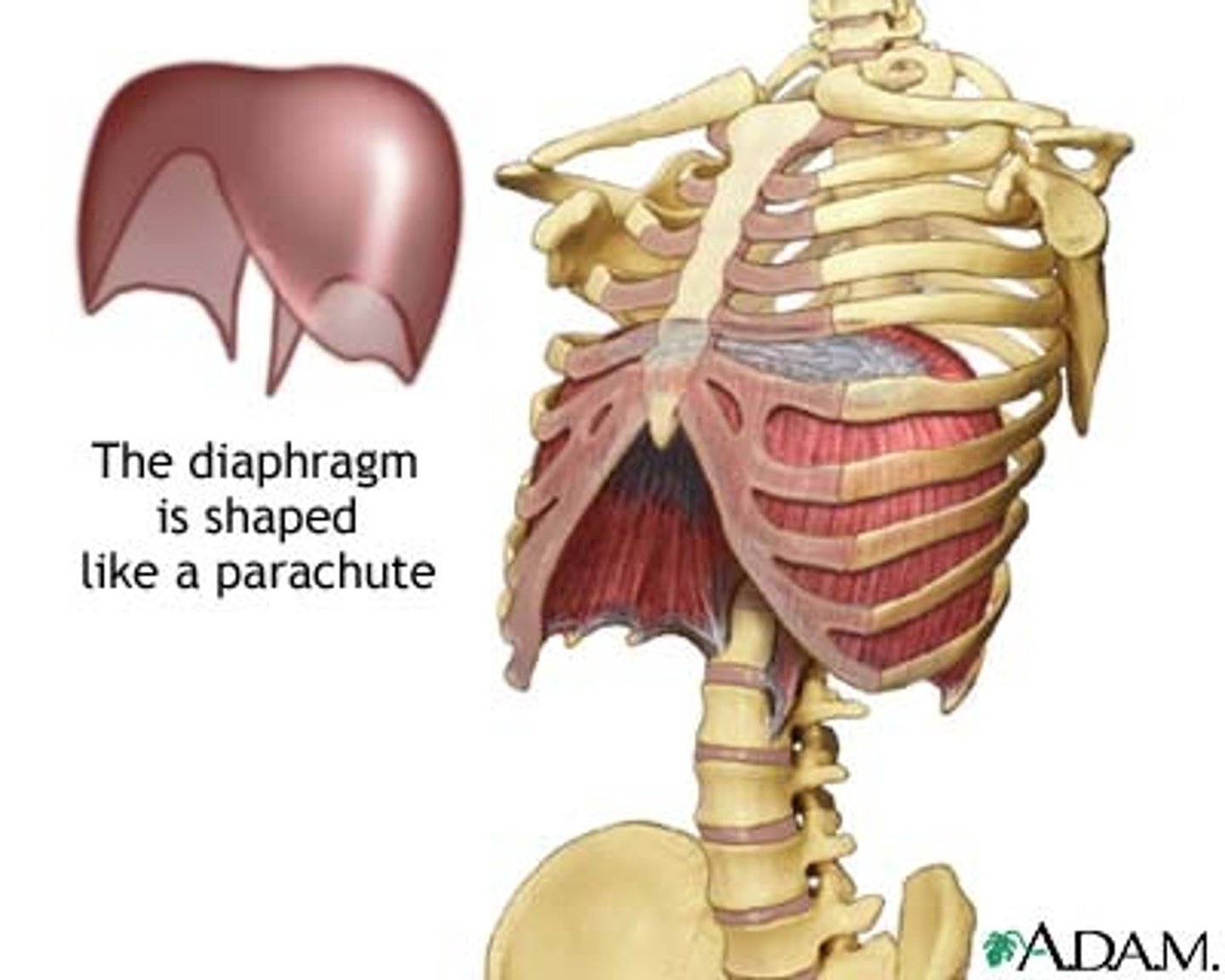
what forms the floor of the thoracic cavity and also fills the inferior thoracic aperture
diaphragm
what structures bound the superior thoracic aperture (opening)?
bounded by t1 vertebra, the 1st pair of ribs, and the manubrium.
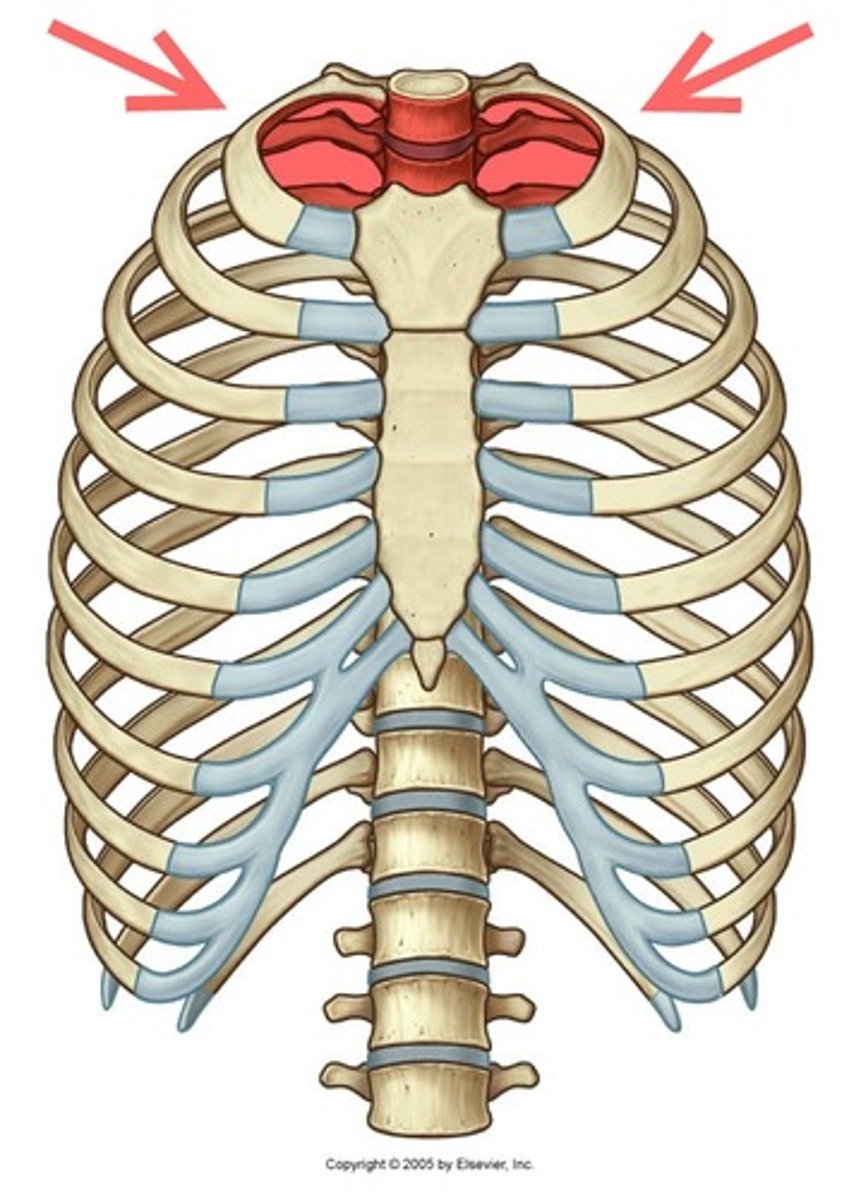
what structures typically pass through the superior thoracic aperture?
the trachea, esophagus, and neurovasculature.
three main components of the osteocartilaginous thoracic cage
-12 pairs of ribs and costal cartilages
-12 thoracic vertebrae and intervertebral discs
-sternum
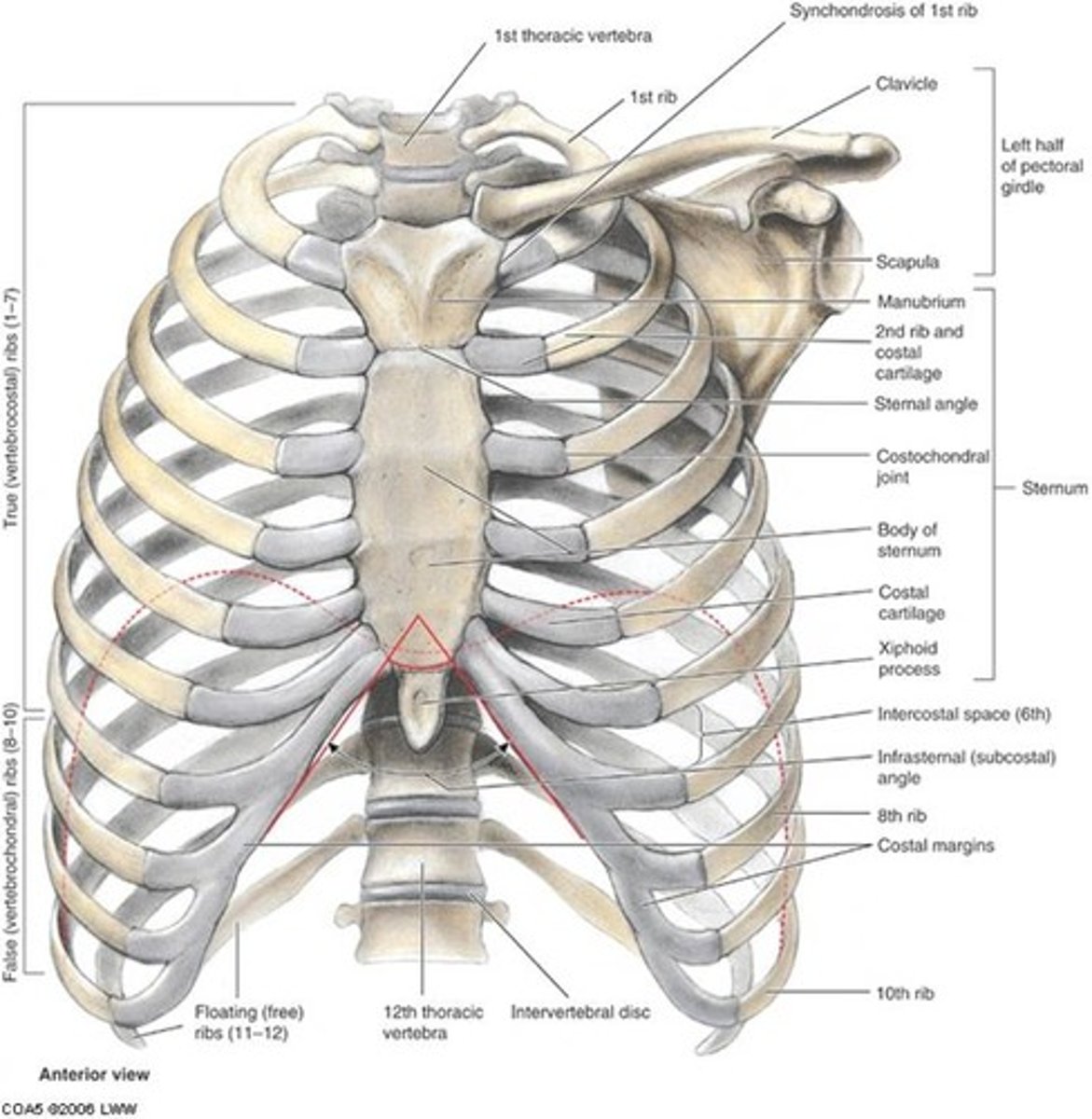
ribs (1st-7th) that articulate directly with the sternum via their own costal cartilage.
true ribs
ribs (8th-10th) whose costal cartilages articulate indirectly with the sternum by joining the cartilage of the rib above.
false ribs
ribs (11th-12th, sometimes 10th) that do not articulate with the sternum at all.
floating ribs
what are the three parts of the sternum?
manubrium, body, xiphoid process
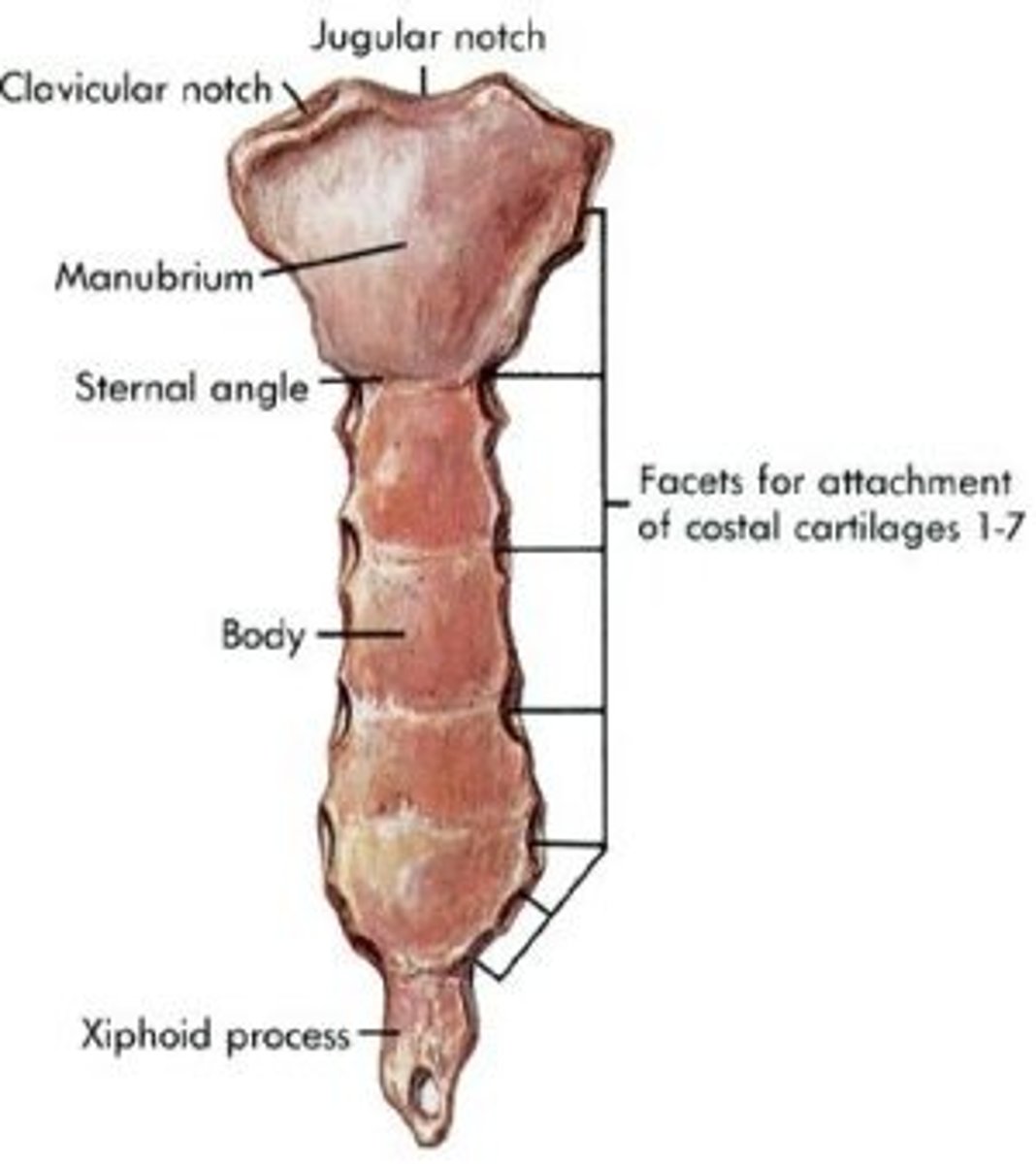
key landmark is found at the superior border of the manubrium
jugular notch
what important anatomical landmark is formed by the junction of the manubrium and the sternal body?
sternal angle (of louis) at t4-t5
this joint marks the junction of the sternum body and the xiphoid process, typically at the t10 vertebral level.
xiphisternal joint
three major spaces dividing the thoracic cavity?
central mediastinum, and the right and left pulmonary cavities.
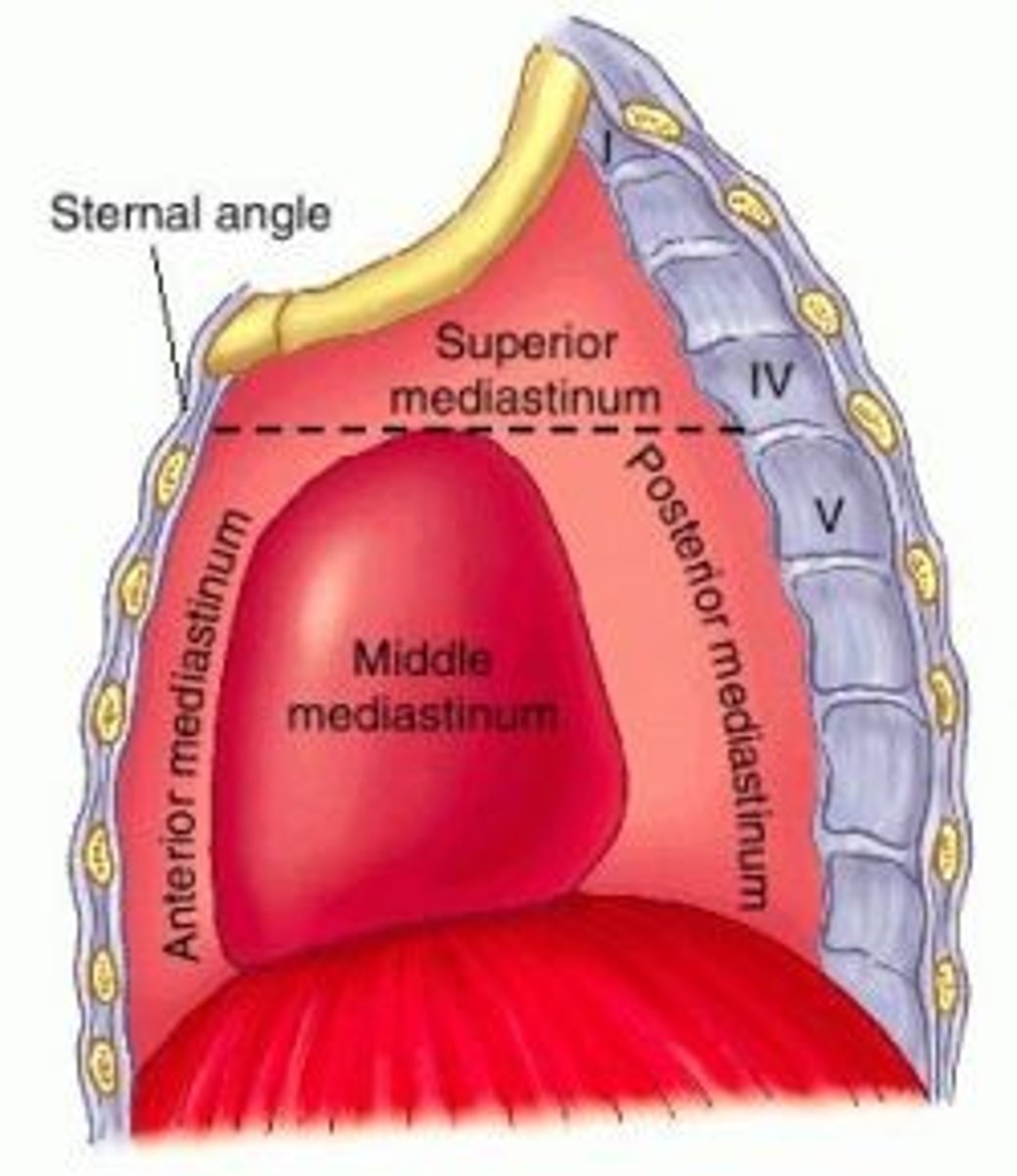
the central compartment of the thoracic cavity, located between the pulmonary cavities is termed
mediastinum
what landmark separates the superior mediastinum from the inferior mediastinum?
the transverse thoracic plane, passing from the sternal angle to the t4/t5 intervertebral disc.
key structures located in the superior mediastinum
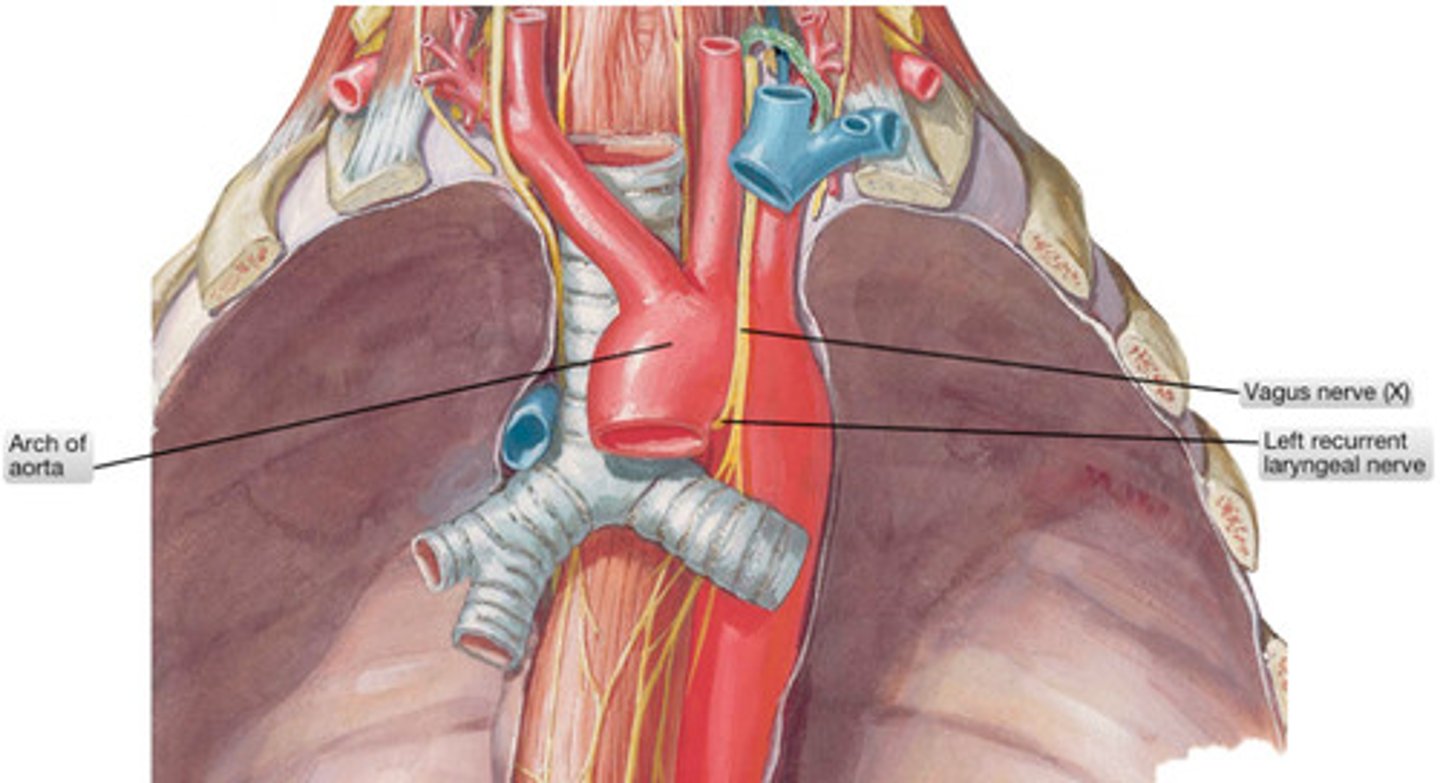
thymus, great vessels (arch of aorta, brachiocephalic veins, svc), trachea, esophagus, thoracic duct, and major nerves (vagus, phrenic).
key structures located in the posterior mediastinum.
thoracic aorta, thoracic duct, azygos system of veins, and esophagus.
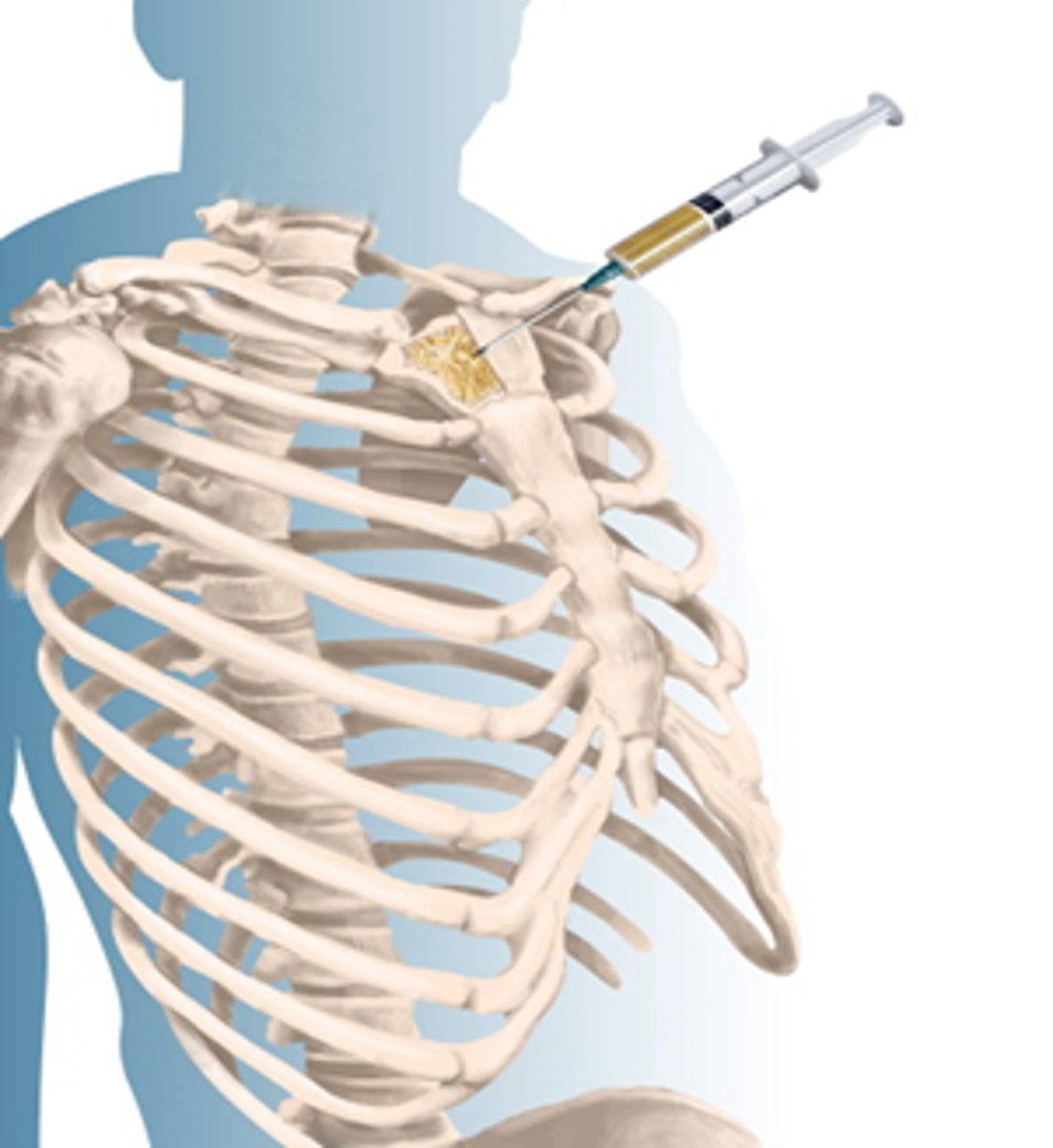
common location for bone marrow biopsy
sternum
feels like a "knot in back" and is a displacement of costal cartilage from sternum
sternal biopsy
rare to have this type of rib fracture
1st rib fracture
hallmark of severe blunt trauma
what forms the intercostal nerves?
the anterior rami of t1-t11 spinal nerves.
what is the name of the anterior ramus of t12?
the subcostal nerve.
what clinical condition causes a dermatomally distributed rash and burning pain along an intercostal nerve pathway?
herpes zoster (shingles)
what are the three primary arterial sources supplying the thoracic wall?
the thoracic aorta, subclavian artery, and axillary artery.
what type of arterial network is characteristic of the thoracic wall blood supply?
a rich network characterized by numerous anastomoses.
what is an 'intercostal nerve block' used for?
pain control, often for rib fractures, by blocking sensory nerve transmission.
what type of glands are in the subcutaneous tissue, overlying pec major and minor muscles
mammary glands
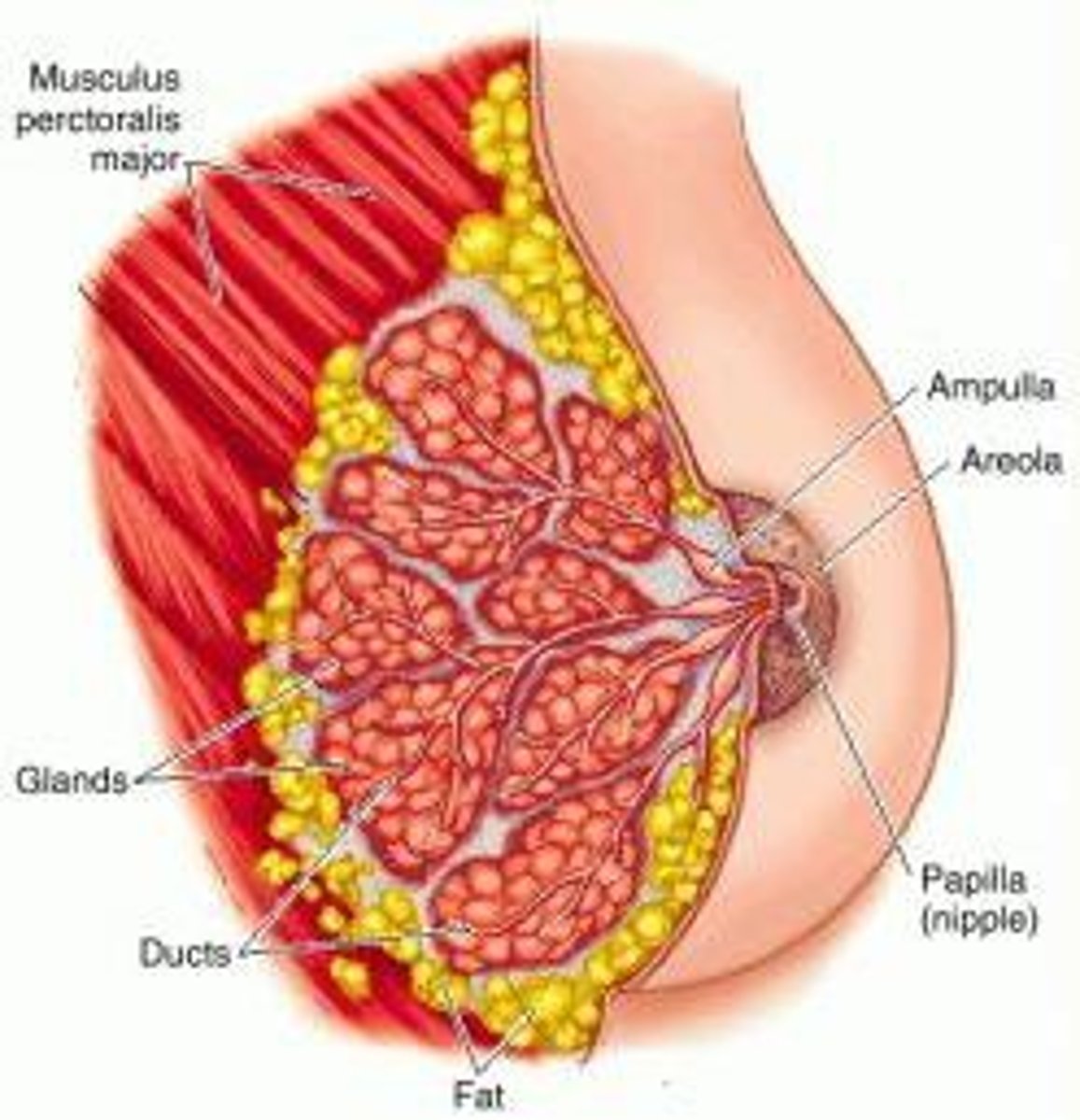
the breast is mainly supplied by this artery
medial mammary branches of perforating branches from the subclavian artery
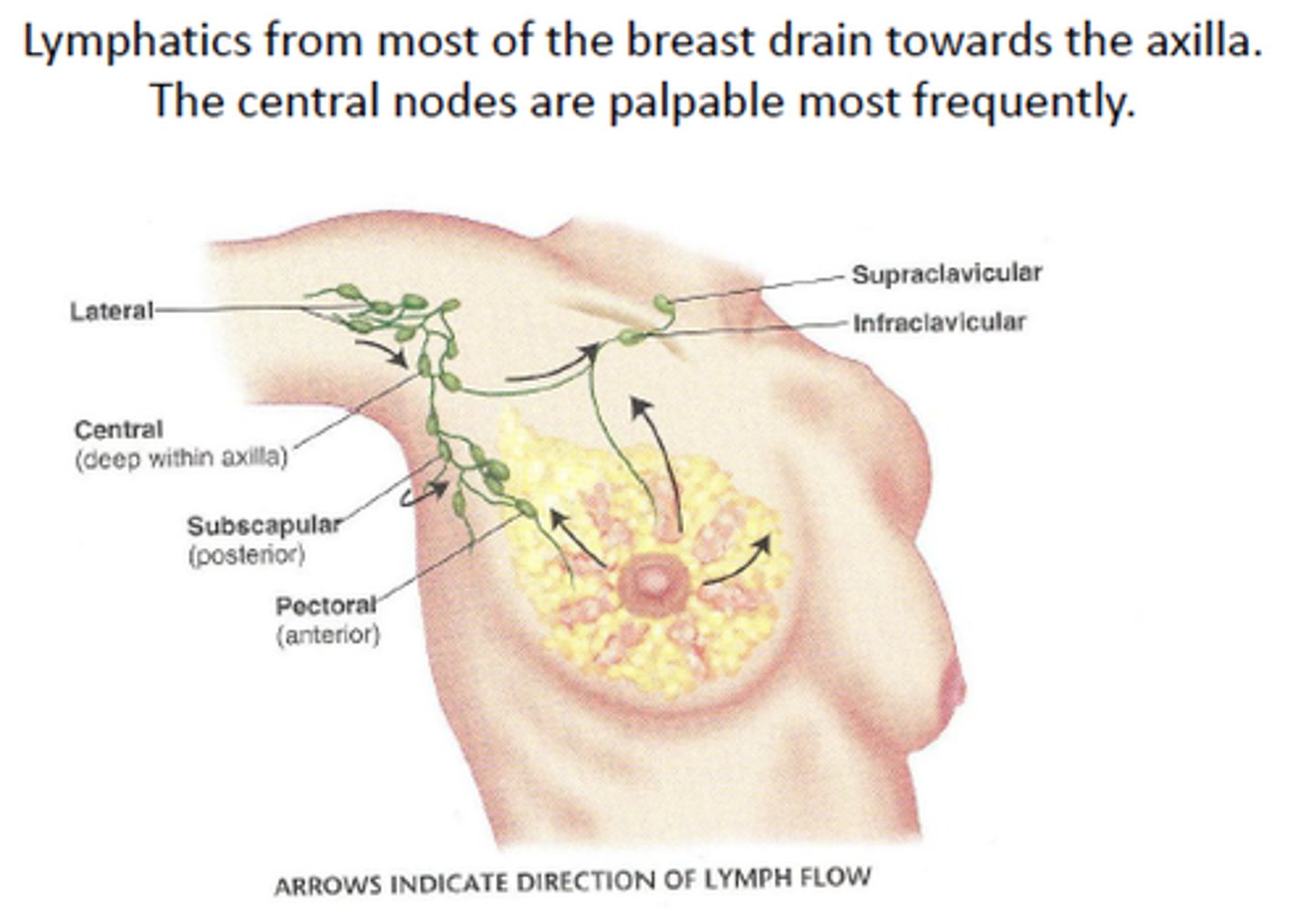
what is the primary lymphatic plexus for breast drainage?
the subareolar lymphatic plexus.
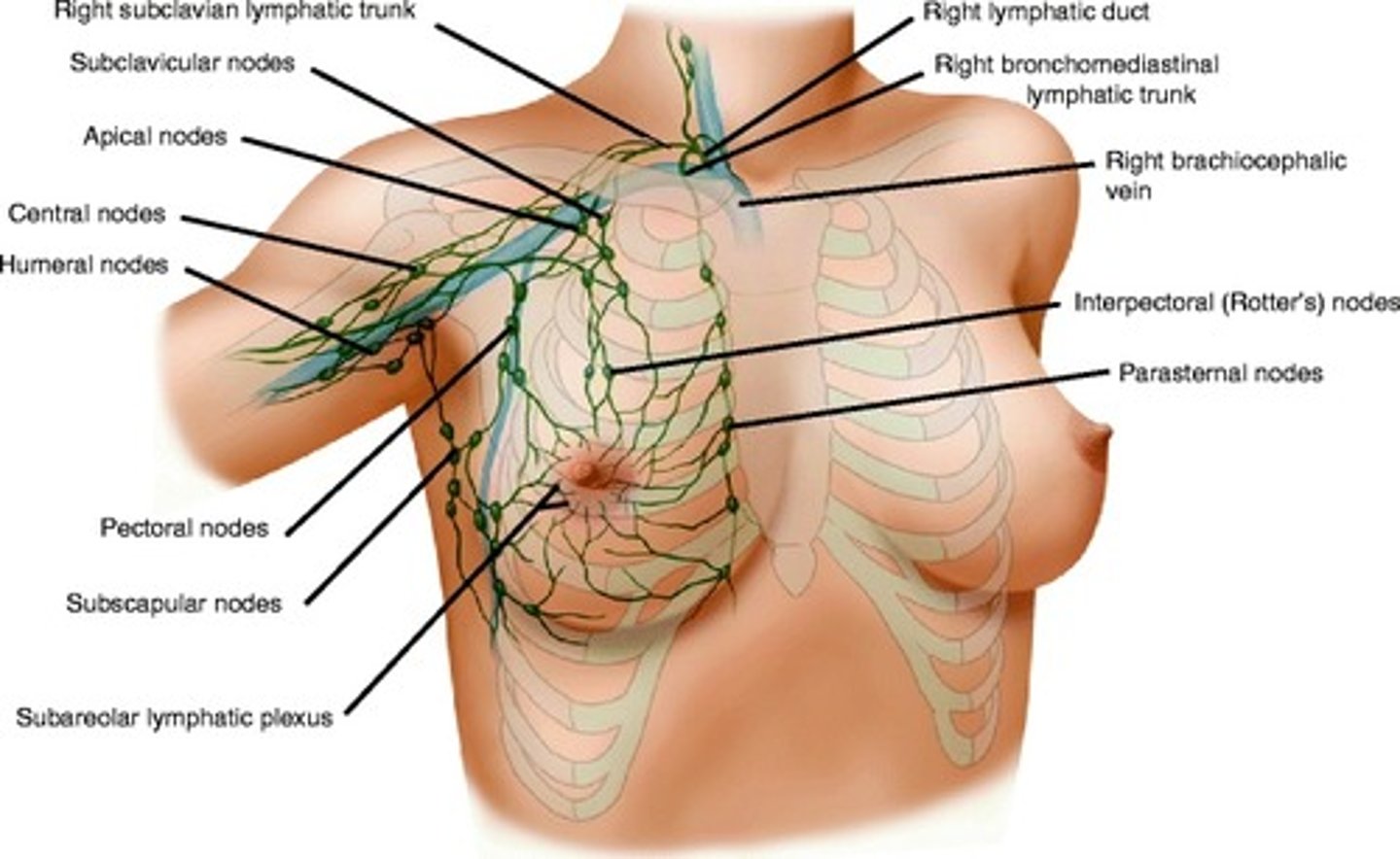
what percentage of breast lymph typically drains into the axillary lymph nodes?
over 75%.
what arteries supply the anterior thoracic wall and breast, and from where do they arise?
the internal thoracic arteries (internal mammary arteries), arising from the subclavian artery.
what are the other significant lymph nodes that receive breast lymph?
the parasternal lymph nodes (internal mammary nodes).
what is a key prognostic indicator related to breast lymphatic drainage in cancer?
the involvement of axillary lymph nodes.
why is understanding breast lymphatic drainage critical clinically?
it's crucial for predicting the spread and staging of breast cancer, as cancer cells often metastasize via these lymphatic channels.
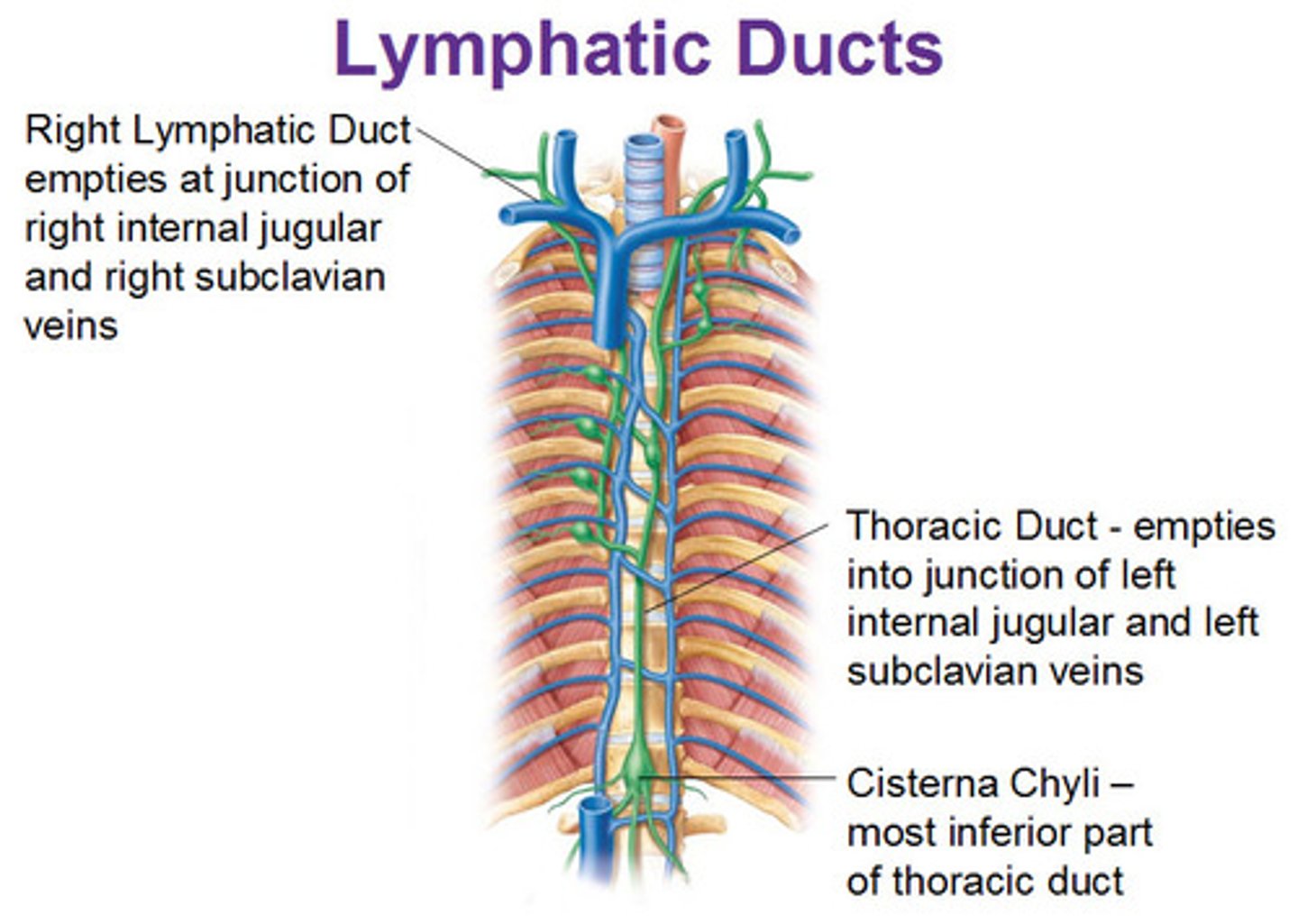
what is the largest lymphatic channel in the body?
the thoracic duct.
what is the general course of the thoracic duct through the thoracic cavity?
it ascends into the posterior mediastinum, passing through the aortic hiatus of the diaphragm.
where does the thoracic duct originate?
it originates from the cisterna chyli in the abdomen.
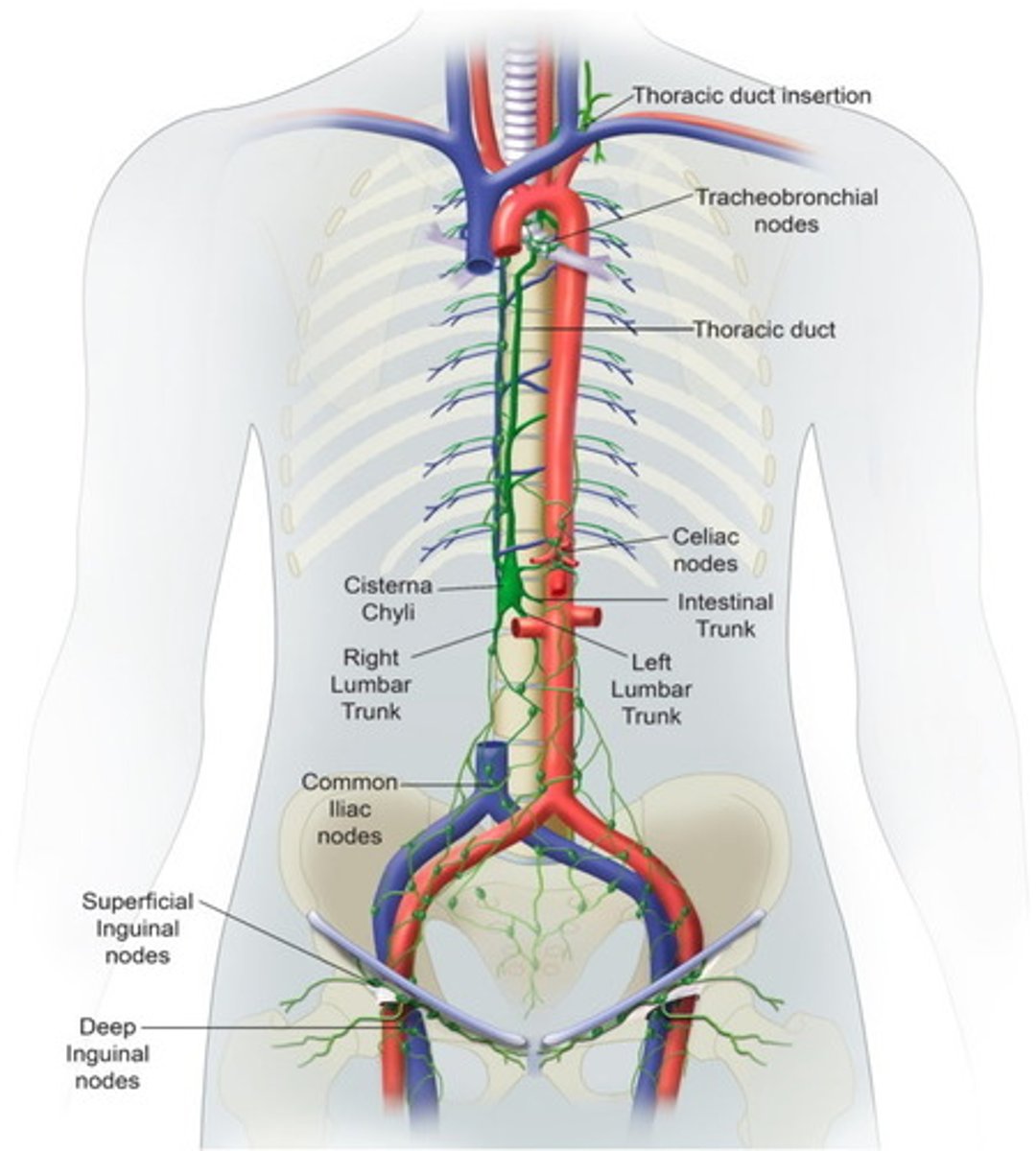
where is the thoracic duct located relative to the vertebrae in the posterior mediastinum?
anterior to the T5-T12 vertebrae.
where does the thoracic duct typically drain into the venous system?
near the left venous angle (the junction of the left internal jugular and left subclavian veins).
which major body regions does the thoracic duct NOT drain?
the right thorax, right upper limb, and the right side of the head and neck.
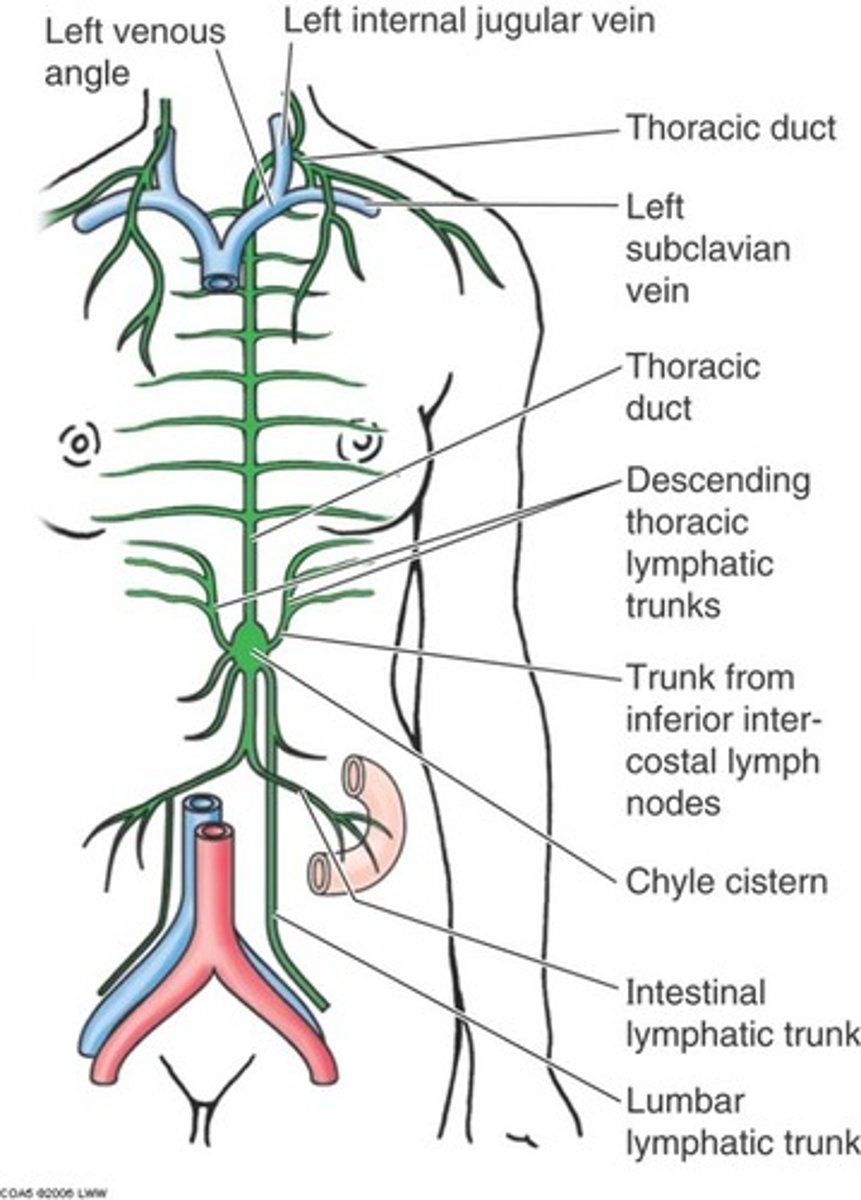
what lymphatic trunks contribute to the thoracic duct on the left side?
jugular, subclavian, and bronchomediastinal lymphatic trunks
what is the major gi tract structure found in the thoracic cavity?
the esophagus.
describe the primary function of the esophagus.
to transport food from the pharynx to the stomach through coordinated muscle contractions called peristalsis.
in which two main regions of the mediastinum does the esophagus descend?
the superior mediastinum and the posterior mediastinum.
where is the esophagus located in the superior mediastinum relative to the trachea?
posterior to the trachea and anterior to the vertebral column.
where is the esophagus located in the posterior mediastinum relative to the pericardium and vertebrae?
anterior to the t5-t12 vertebrae and posterior to the pericardium.
which opening in the diaphragm does the esophagus pass through?
the esophageal hiatus.
at what vertebral level does the esophageal hiatus typically occur?
typically at the t10 vertebral level.
what are some key structures the esophagus is closely related to in the thorax?
the trachea, aorta, and vagus nerves.
what is the primary function of the coronary arteries?
they provide the dedicated blood supply to the myocardium and epicardium (heart muscle and outer layer).
where do the coronary arteries originate?
they are the first branches directly off the ascending aorta.
which coronary artery typically descends in the coronary sulcus, giving off the right marginal branch?
the right coronary artery (rca).
what significant branch does the rca often give rise to posteriorly in most individuals?
the posterior interventricular branch (posterior descending artery, pda).
what are the two main branches of the left coronary artery (lca)?
the anterior interventricular branch (lad) and the circumflex branch.
what is the common name for the lad (left anterior descending) artery due to the severity of blockages there?
the widowmaker.
which branch of the lca runs in the coronary sulcus around the left side of the heart?
the circumflex branch.
what does coronary dominance refer to?
it refers to which coronary artery gives rise to the posterior interventricular branch (pda).
what is the most common pattern of coronary dominance?
right dominant (67% of people).
what is the primary pathway for venous drainage of the posterior thoracic wall?
the azygos venous system.
describe the azygos vein's location and drainage.
it runs on the right side of the vertebral column and drains into the superior vena cava (svc).
what veins typically run on the left side of the vertebral column and often drain into the azygos vein?
the hemi-azygos vein and accessory hemi-azygos vein.
what important collateral pathway does the azygos system form?
a collateral pathway between the svc and ivc.
how is the anterior thoracic wall primarily drained venously?
by the internal thoracic veins, which typically drain into the brachiocephalic veins.
what is the major venous structure that collects most of the coronary venous blood?
the coronary sinus.
where is the coronary sinus located and where does it drain?
it's a large vein in the posterior part of the coronary sulcus, draining into the right atrium.
name three major tributaries of the coronary sinus.
the great cardiac vein, middle cardiac vein, and small cardiac vein.
what three major vessels deliver deoxygenated blood to the right atrium?
the superior vena cava (svc), inferior vena cava (ivc), and coronary sinus.
what valve does deoxygenated blood pass through to move from the right atrium to the right ventricle?
the tricuspid valve (right av valve).
what are the rough muscular elevations lining the interior of the right ventricle?
trabeculae carneae.
what valve does blood pass through to leave the right ventricle and enter the pulmonary circulation?
the pulmonary valve (a semilunar valve).
what vessel carries deoxygenated blood from the right ventricle to the lungs?
the pulmonary trunk, which then divides into the right and left pulmonary arteries.
what vessels return oxygenated blood from the lungs to the left atrium?
the four pulmonary veins.
what valve does oxygenated blood pass through from the left atrium to the left ventricle?
the mitral valve (bicuspid valve, left av valve).
which heart chamber forms the apex of the heart and has the thickest walls?
the left ventricle.
what valve does blood pass through to leave the left ventricle and enter systemic circulation?
the aortic valve (a semilunar valve).
what is the function of the heart's fibrous skeleton?
it anchors myocardial fibers, maintains valve orifices, provides attachment for valve leaflets, and electrically insulates the atria from the ventricles.
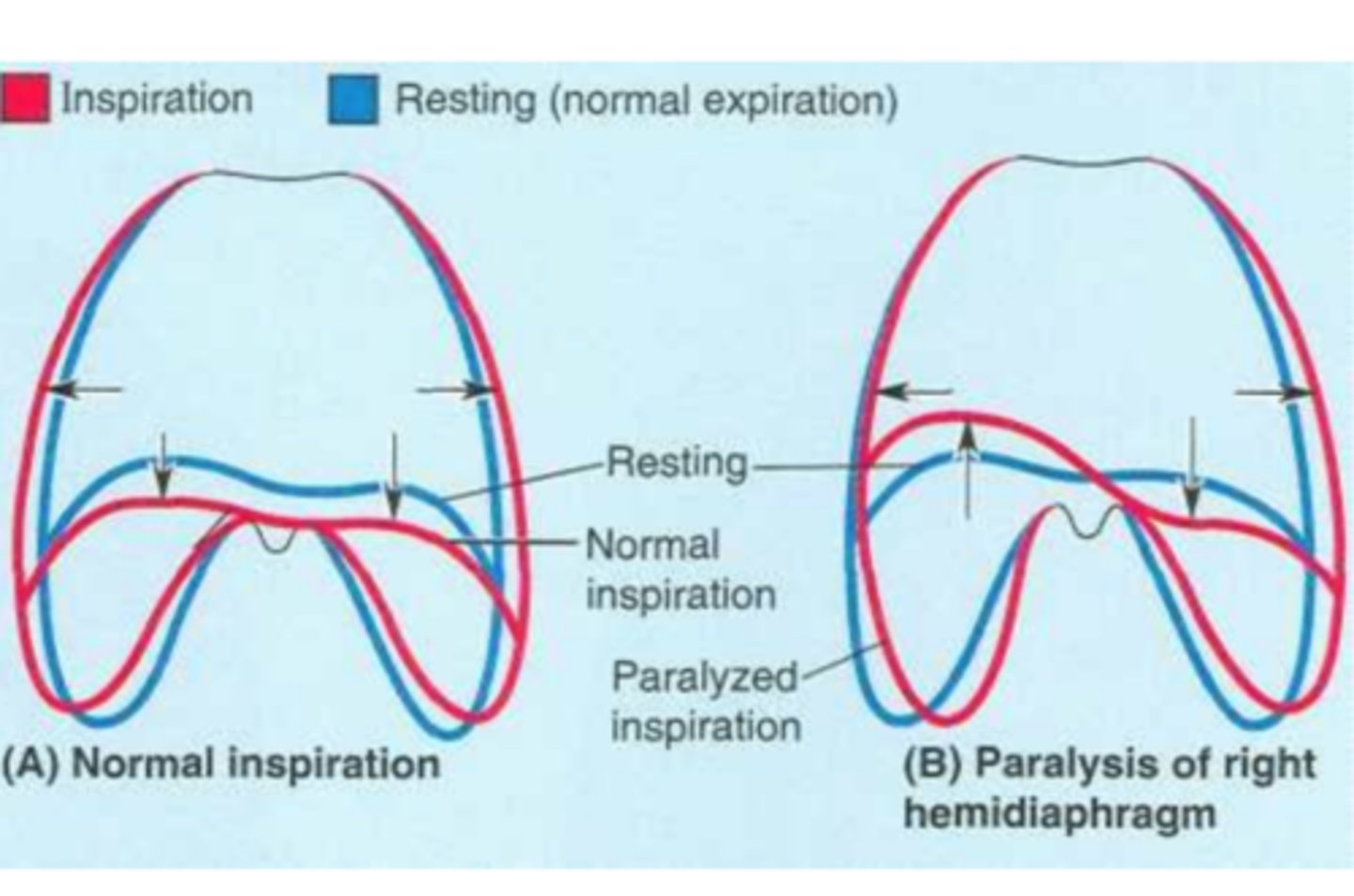
what nerve innervates the diaphragm?
the phrenic nerves.
from which cervical spinal nerves do the phrenic nerves originate?
c3, c4, and c5.
what clinical condition results from disruption of the phrenic nerve's impulse to the diaphragm?
hemidiaphragm paralysis.
what is 'paradoxical movement' of the diaphragm in hemidiaphragm paralysis?
the paralyzed side moves up during inspiration instead of descending, due to negative intrathoracic pressure.
what plexus provides innervation to the lungs and visceral pleura?
the pulmonary plexus.
what is the general effect of sympathetic stimulation on the lungs?
bronchodilation and pulmonary vasoconstriction.
what is the general effect of parasympathetic stimulation (via vagus nerve) on the lungs?
bronchoconstriction and pulmonary vasodilation.
what type of fibers carry subconscious sensations and pain signals from the lungs and pleura?
afferent visceral fibers.
which pleura is insensitive to pain, and which is highly sensitive?
the visceral pleura is insensitive; the parietal pleura is highly sensitive.
what intrinsic ability does the heart possess regarding impulse generation?
autorhythmic ability (it can generate its own impulses).
what is the effect of sympathetic stimulation on the heart?
increases heart rate (chronotropy) and force of contraction (inotropy), and causes coronary vasodilation.
what is the effect of parasympathetic stimulation (via vagus nerves) on the heart?
decreases heart rate and force of contraction, and causes coronary vasoconstriction.
what is the heart's natural pacemaker?
the sinu-atrial (sa) node, located near the svc in the right atrium.
what is the function of the atrioventricular (av) node?
it receives impulses from the sa node and introduces a slight delay before transmitting them to the ventricles.
what structures distribute electrical impulses throughout the ventricular myocardium?
the subendocardial branches (purkinje fibers).
three major openings (hiatuses) in the diaphragm and the primary structures that pass through them.
caval opening (t8): inferior vena cava (ivc).
esophageal hiatus (t10): esophagus and vagus nerves. aortic hiatus (t12): aorta, azygos vein, and thoracic duct.
pericardium
a fibroserous sac that surrounds and protects the heart and the roots of the great vessels.
two main layers of the pericardium
the tough outer fibrous pericardium and the inner double-layered serous pericardium.
two layers of the serous pericardium
the parietal layer (lining the fibrous pericardium) and the visceral layer (epicardium) (adhering to the heart surface).
function of the serous fluid in the pericardial cavity
to reduce friction during heartbeats.
cardiac tamponade
a life-threatening condition where excessive fluid/blood in the pericardial cavity compresses the heart, restricting its filling and decreasing cardiac output.
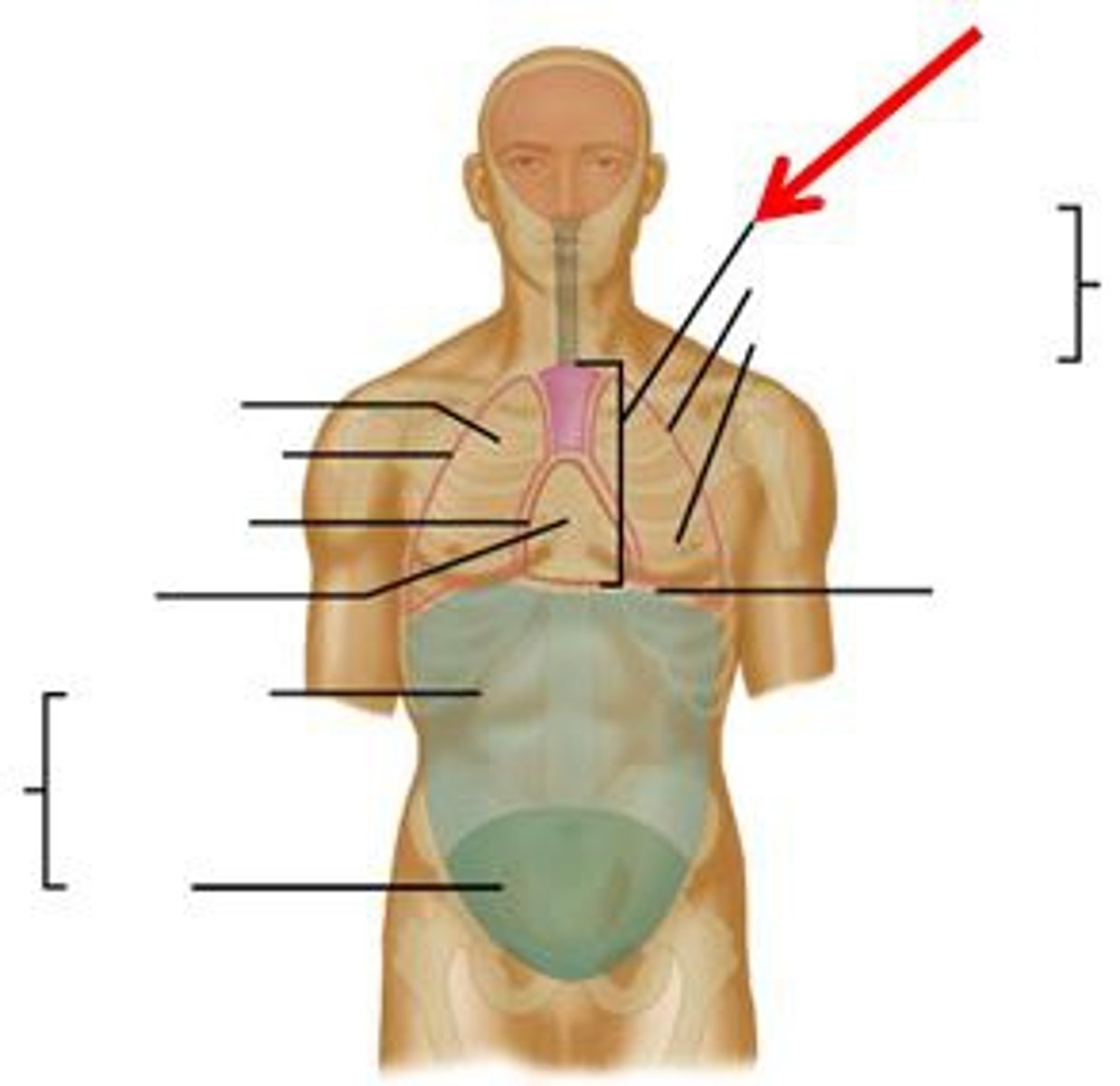
the most inferior aspect of the abdominopelvic cavity. it is surrounded by the pelvic girdle.
the pelvis
how is the pelvis subdivided?
into the greater pelvis (above the pelvic brim) and the lesser pelvis (below the pelvic brim).