BIO307: Test #3: Chapter 14: Cardiovascular
0.0(0)
Card Sorting
1/27
Earn XP
Description and Tags
Last updated 2:48 PM on 11/2/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
1
New cards
septum
Dividing walls between the chambers of the heart
2
New cards
Pulmonary Arteries
Carry blood from heart to lungs
3
New cards
Pulmonary Veins
carry blood from lungs to heart
4
New cards
resistance
(in relation to fluid), resistance increases as length of tube and viscosity of fluid increases, and as radius of tube decreases. Radius has the largest effect of resistance.
5
New cards
Electrocardiogram (ECG)
surface recording of the electrical activity of the heart
6
New cards
Autorhythmic Cells
Cells that depolarize spontaneously, having an unstable membrane potential which is referred to as the pacemaker potential
7
New cards
Vasodilation
widening of blood vessels as a result of relaxation of blood vessel muscular walls
8
New cards
Vasoconstriction
narrowing of blood vessels resulting from contraction of muscular wall of the vessels
9
New cards
Pericardium
a serous membrane with two layers that surrounds the heart, consists of outer fibrous layer and inner double serous membrane
10
New cards
Myocardium
Cardiac muscular tissue of the heart, striated muscle
11
New cards
Systole
Contraction phase of cardiac cycle
12
New cards
Diastole
relaxation phase of cardiac cycle
13
New cards
Stroke Volume
amount of blood pumped by one ventricle during one contraction
14
New cards
End-Systolic Volume
volume of blood in the ventricles at the end of contraction
15
New cards
Ejection Fraction
percent of EDV (end diastolic volume) ejected with one contraction (stroke volume / EDV)
16
New cards
Order of Blood
Heart -> Arteries -> Arterioles -> Capillaries -> Venules -> Veins -> SVC/IVC -> Heart
17
New cards
Blood Flow vs Pressure Gradient
Blood flows down the pressure gradient, rate of blood flow is proportional the blood pressure difference between the two sites.
Blood Vessel Radius to Resistance: a 4th power relationship:
Ex: Do the larger number over the smaller number, the factor ^ 4 is the difference
Blood Vessel Radius to Resistance: a 4th power relationship:
Ex: Do the larger number over the smaller number, the factor ^ 4 is the difference
18
New cards
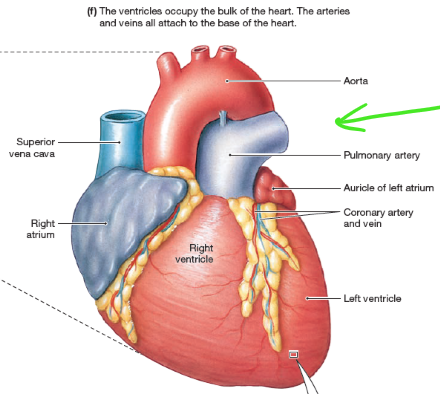
Label Heart Exterior
19
New cards
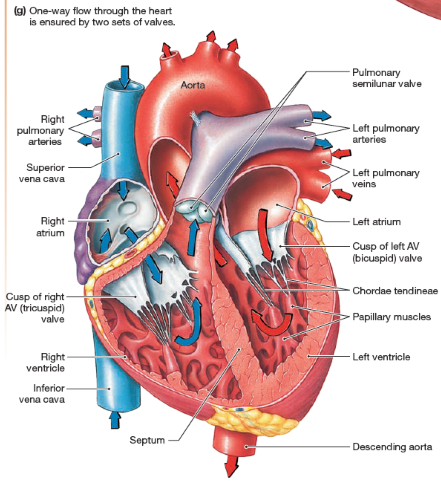
Label Heart Interior
20
New cards
Heart Valves
ensure unidirectional blood flow, are like gates, open and close to allow blood to flow from one area of the heart to another
Atrioventricular Valves: between atrium and ventricles
Semilunar: between ventricle and arteries
Issues:
Prolapse: when a chordae fails, valve is pushed back into atrium during ventricular contraction
If a valve fails, the blood would not have the control system to prevent blood from flowing backward (can be seen moving backwards through the chambers on ultrasound)
Atrioventricular Valves: between atrium and ventricles
Semilunar: between ventricle and arteries
Issues:
Prolapse: when a chordae fails, valve is pushed back into atrium during ventricular contraction
If a valve fails, the blood would not have the control system to prevent blood from flowing backward (can be seen moving backwards through the chambers on ultrasound)
21
New cards
Muscle Cells and Gap Junctions
Ions are transported between adjacent cells to allow for the electrical signaling for the pacemaker potential throughout the cardiac muscle
22
New cards
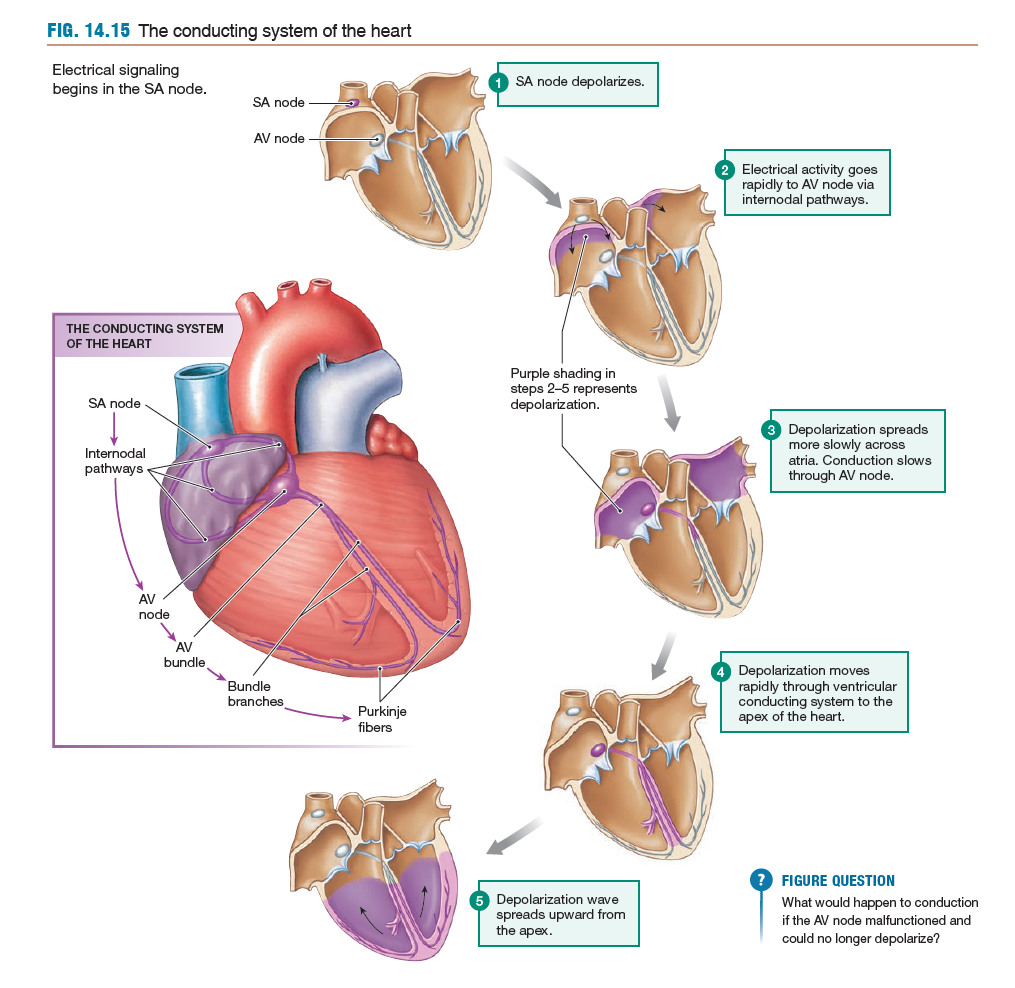
Spontaneous Generation of Action Potential in Heart
Pacemaker potential is created by autorhythmic cells
Pathway:
Sinoatrial (SA) Node -> Internodal Pathways -> Atrioventricular (AV) Node -> Atria -> Septum -> Apex of the Heart -> Upward through the Ventricle
Pathway:
Sinoatrial (SA) Node -> Internodal Pathways -> Atrioventricular (AV) Node -> Atria -> Septum -> Apex of the Heart -> Upward through the Ventricle
23
New cards
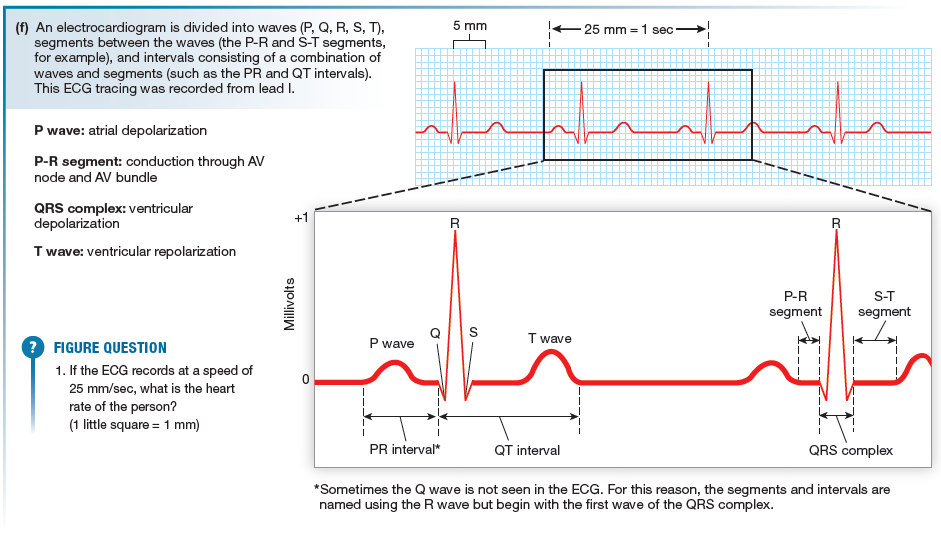
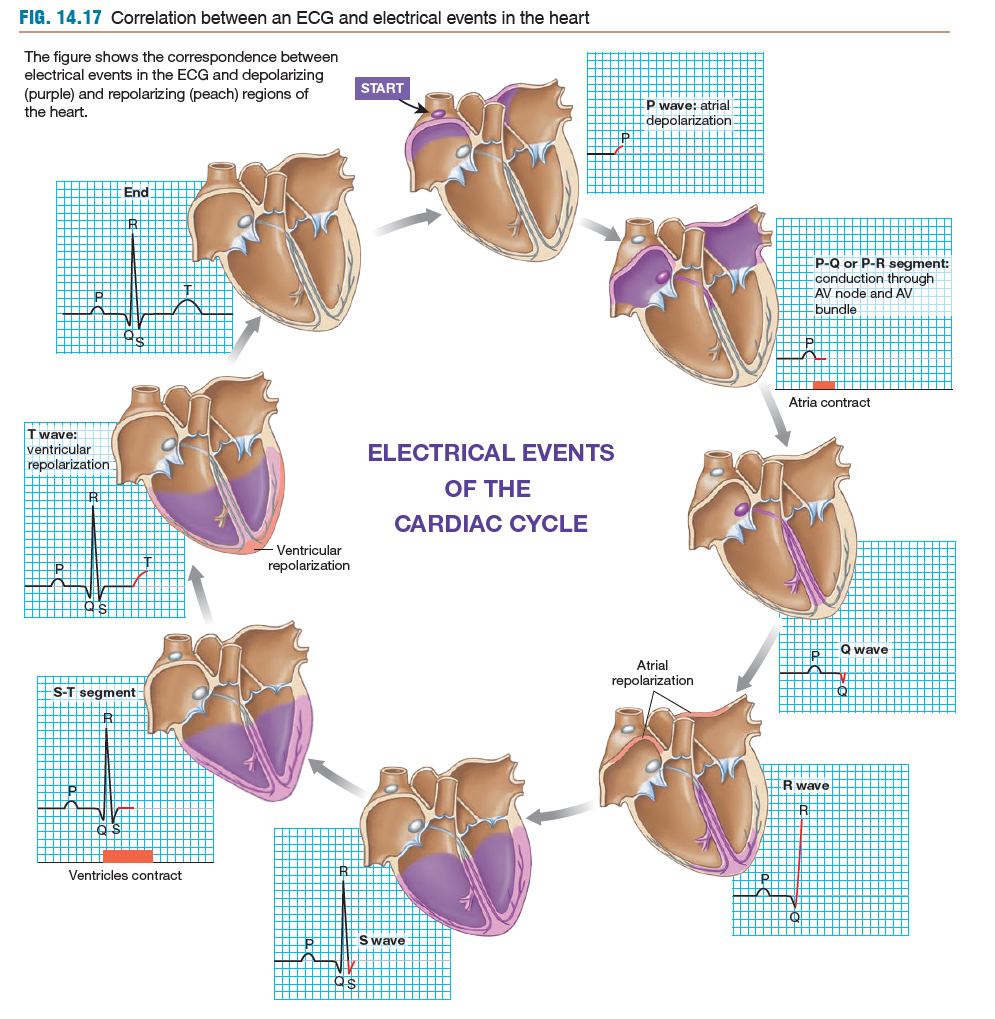
ECG/EKG Reading:
P wave: atrial depolarization
P-R segment: conduction through AV node and AV bundle
QRS complex: ventricular depolarization
T wave: ventricular repolarization
P-R segment: conduction through AV node and AV bundle
QRS complex: ventricular depolarization
T wave: ventricular repolarization
24
New cards
ECG Reading W/ Depolarization Events
Start: superior atria depolarization = P wave
medial atria + P-Q + P-R segment = conduction through AV node
Septum = Q wave
Apex of the Ventricle = R wave
Depolar. of Ventricles = S Wave
Contraction of Ventricles = S - T segment
Ventric. Repolarization = T wave
medial atria + P-Q + P-R segment = conduction through AV node
Septum = Q wave
Apex of the Ventricle = R wave
Depolar. of Ventricles = S Wave
Contraction of Ventricles = S - T segment
Ventric. Repolarization = T wave
25
New cards
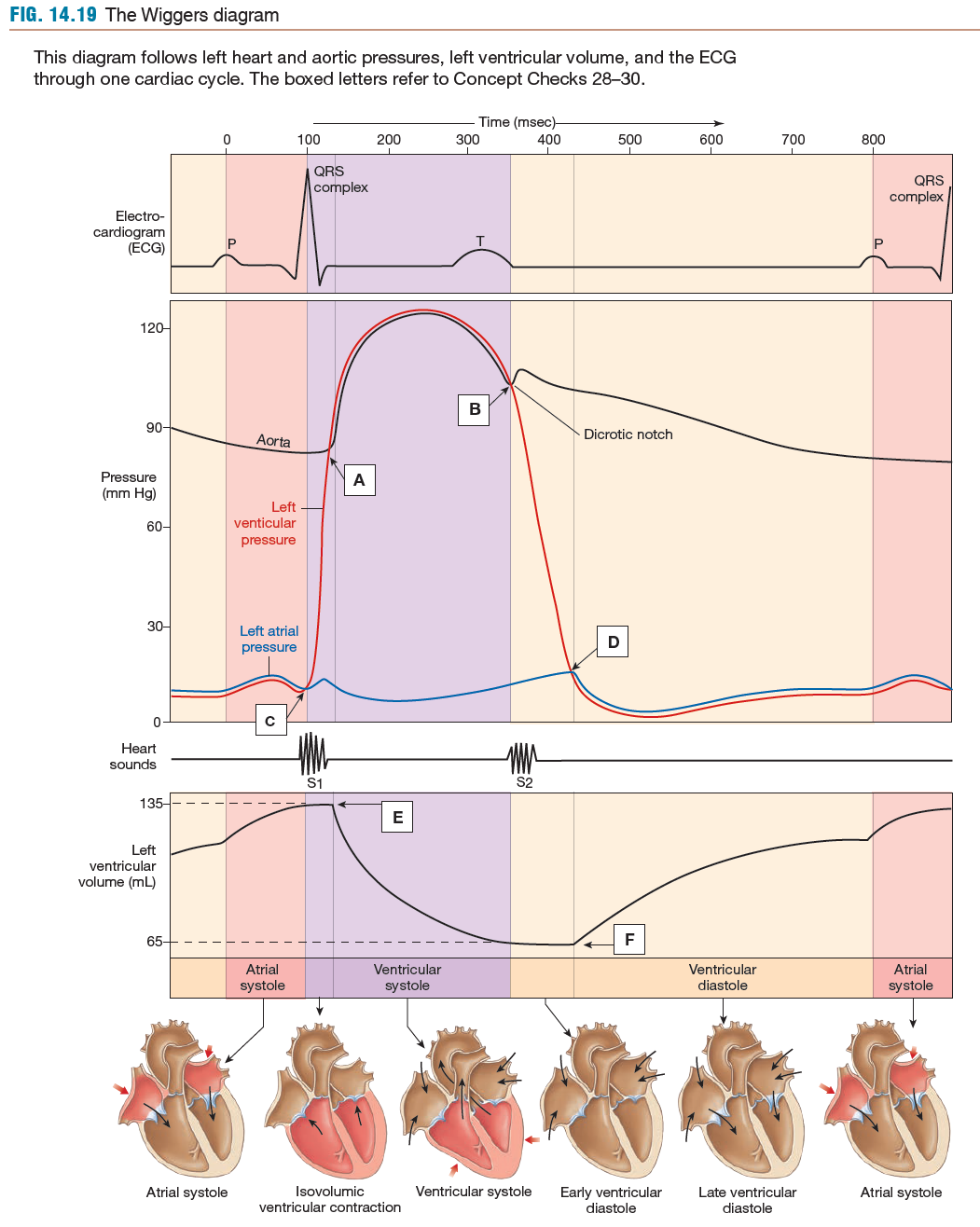
Wiggers Diagram
Shows QRS complex
26
New cards
Events of Cardiac Cycle
1) Late Diastole: both sets of chambers relaxed, ventricles fill passively
2) Atrial Systole: small amount of blood enters ventricles
3) Isovolumic Ventricular Contraction: AV valves close once cavity fills, doesn't open semilunar valves until volume of ventricle fills up
[EDV, end diastolic volume] = Max Blood Volume of Ventricle
4) Ventricular Ejection: Semilunar valves open due to ventricular pressure
5) Isovolumic ventricular relaxation: ventricles relax, ventricular pressure falls, semilunar valves now close
[ESV, end systolic volume] = Minimum Blood Volume in Ventricles
2) Atrial Systole: small amount of blood enters ventricles
3) Isovolumic Ventricular Contraction: AV valves close once cavity fills, doesn't open semilunar valves until volume of ventricle fills up
[EDV, end diastolic volume] = Max Blood Volume of Ventricle
4) Ventricular Ejection: Semilunar valves open due to ventricular pressure
5) Isovolumic ventricular relaxation: ventricles relax, ventricular pressure falls, semilunar valves now close
[ESV, end systolic volume] = Minimum Blood Volume in Ventricles
![1) Late Diastole: both sets of chambers relaxed, ventricles fill passively
2) Atrial Systole: small amount of blood enters ventricles
3) Isovolumic Ventricular Contraction: AV valves close once cavity fills, doesn't open semilunar valves until volume of ventricle fills up
[EDV, end diastolic volume] = Max Blood Volume of Ventricle
4) Ventricular Ejection: Semilunar valves open due to ventricular pressure
5) Isovolumic ventricular relaxation: ventricles relax, ventricular pressure falls, semilunar valves now close
[ESV, end systolic volume] = Minimum Blood Volume in Ventricles](https://knowt-user-attachments.s3.amazonaws.com/69271bf6a00a4aecb3f9a0513d6c7d0f.jpeg)
27
New cards
Cardiac Output
CO = SV * HR
^ Venous Return: CO increases
^ Blood Volume: CO increases
^ Sympathetic Activity: CO increases (epinephrine direct relationship on HR)
^ Parasympathetic Activity: CO decreases (Ach. direct relationship on HR)
^ Heart Rate: CO increases
^ SV: CO increases
^ Venous Return: CO increases
^ Blood Volume: CO increases
^ Sympathetic Activity: CO increases (epinephrine direct relationship on HR)
^ Parasympathetic Activity: CO decreases (Ach. direct relationship on HR)
^ Heart Rate: CO increases
^ SV: CO increases
28
New cards
Factors Normally Affect Venous Return
EDV directly affects Venous Return (amount of blood returning to heart from venous circulation)
Factors Affecting it:
1) Contraction/Compression of Veins Returning Blood
2) Pressure changes in abdomen and thorax during breathing (the respiratory pump)
3) Sympathetic innervation
Factors Affecting it:
1) Contraction/Compression of Veins Returning Blood
2) Pressure changes in abdomen and thorax during breathing (the respiratory pump)
3) Sympathetic innervation