Blood Typing and Transfusions
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Important Anemia History
-history and symptoms of anemia
-liver disease
-coagulopathies
-thrombotic history
-previous blood transfusions
Anemia Pre-Op Eval
-CBC (Hgb/Hct)
-identify cause
-build Hgb before surgery to avoid transfusion
Further work up is needed for a female pt with a Hgb ___ or male ___ before a surgical procedure
<12; <13
iron deficiency is a __________ anemia
microcytic
treatment for pre-op iron deficiency anemia
IV iron
B12 deficiency and folate deficiency are __________ anemias
macrocytic
treatment for pre-op macrocytic anemia
B12 or folate (oral or injection)
anemia of chronic disease is a ________ anemia
normocytic
treatment for anemia of chronic disease
epoetin
Blood Types
-A
-B
-O
-Rh
_____ consists of checking recipients' plasma for atypical antibodies
screening
Indirect Coombs Test
-screening test that mixes recipients blood with donor blood (cross matching)
-clumping indicates antibodies to antigens
-prevent transfusion reactions
O Neg
-universal donor
-lacks antigens
AB Positive
-universal recipient
-lack of antibodies
AB Plasma
universal plasma donor
___ and ___ can be given in emergent situations without knowing a recipient's blood type
AB plasma and O neg blood
__________ don't have to be crossmatched
platelets
Rh-negative patients should be transfused with only ___________
Rh negative RBCs
__________ should not be transfused to Rh- females of childbearing age
Rh + RBCs (okay in men or postmenopausal women)
Rh- mothers are given anti-Rh antibodies during pregnancy and at delivery to prevent ______________
hemolytic disease of the newborn
whole blood is primarily used in __________
hemorrhagic shock
Whole Blood contains which components?
RBCs, platelets, and coag factors
Packed Red Blood Cells
80% of plasma is removed so it is mostly just RBCs used for an anemic patient
transfusion of PRBCs considered in a stable patient at a HgB <_________
7
transfusion of PRBCs considered in a patient with pre-existing CV disease, or pts having cardiac or ortho surgery at a HgB <_________
8
Platelet Indications
-management of active bleeding in TCP patients
-prophylactically in pts undergoing minor surgery/ procedures when platelets <50,000
-prophylactically in patients undergoing major surgery when platelets <50,000-75,000
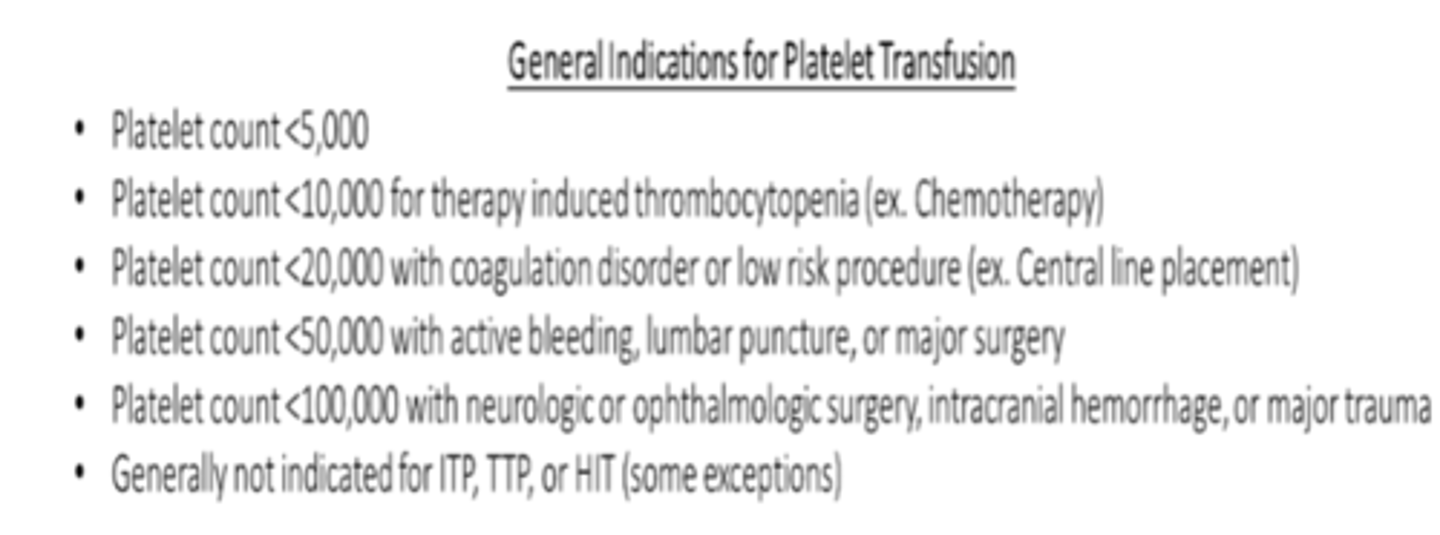
Platelets are not indicated in ___, ___, or ___ due to potential worsening of thrombosis
ITP, TTP, HIT
FFP
contains 1 unit of each coag factor and 2mg of fibrinogen
FFP indications
To replace coagulation factors in patients with deficiencies of multiple clotting factors (ex. liver disease, DIC, warfarin overdose)
FFP is NOT indicated for ____
overdose of DOACs
Transfusion Indications
-improve oxygen carrying capacity
-treat anemia
-replenish blood volume
Transfusion Complications
-infection (viral or bacterial)
-allergic reactions
-hemolytic reactions
-febrile nonhemolytic reactions
-transfusion associated circulatory overload (TACO)
-transfusion related acute lung injury (TRALI)
Possible Transfusion Infections
-HIV
-human T cell lymphotrophic virus type 1 and 2
-Hep B
-Hep C
-Parvovirus B19
Allergic Reaction
-most often urticaria and pruritus
-can cause anaphylaxis
-immune response to plasma proteins
Hemolytic Reactions
-acute or delayed
-recipients antibodies recognize and induce hemolysis of donor RBCs
hemolytic reactions are most commonly due to ______ incompatibility and can lead to DIC
ABO
Hemolytic Reaction S/S
-back pain
-fever
-dyspnea
-tachycardia
-bleeding
-shock
Febrile Nonhemolytic Reaction
-fever during or within 4 hours of transfusion
-recipient antibody against donor leukocytes and release of cytokines produced during storage
-platelet transfusions pose more risk
Transfusion associated circulatory overload (TACO)
-respiratory compromise from circulatory overload
-occurs with rapid infusion of blood, plasma, or crystalloids
-elderly with underlying heart disease most at risk
TACO S/S
-dyspnea
-hypoxia
-pulmonary edema
-normal to high BP
-exudative edema fluid (high protein, cloudy)
TACO diagnostics
-vascular congestion and pleural effusion on CXR
-high BNP
-abnormal ejection fraction
-high Pulmonary Artery Occlusion Pressure (PAOP) AKA Pulmonary Capillary Wedge Pressure (PCWP)
TACO treatment
diuresis and slow down infusion
Transfusion Related Acute Lung Injury (TRALI)
-uncommon
-due to Anti-leukocyte antibodies in donor product that produce PMN leukocyte degranulation in the lung
TRALI is most common with _______
plasma transfusions
TRALI S/S
-symptoms similar to ARDS
-noncardiogenic pulmonary edema
-low to normal BP
-normal to high temp
-transudative edema fluid (low protein, clear)
TRALI diagnostics
-no vasc congestion on CXR
-low BNP
-low-normal PAOP
-normal EJF
TRALI must be differentiated from circulatory overload as diuresis can cause _____________
rapid deterioration
TRALI treatment
supportive care, DO NOT DIURESIS
Avoiding Transfusion Reactions
-careful processing with type and cross
-start with slow infusion rate
-infuse each unit over 4 hours
-pretreat with Tylenol and/or Benadryl for patients with history of transfusion reaction
Transfusion Reaction Steps
1. Stop the transfusion
2. Contact blood bank that issued the product
3. Treat based on type of reaction