Preclinical Exam 2
1/217
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
218 Terms
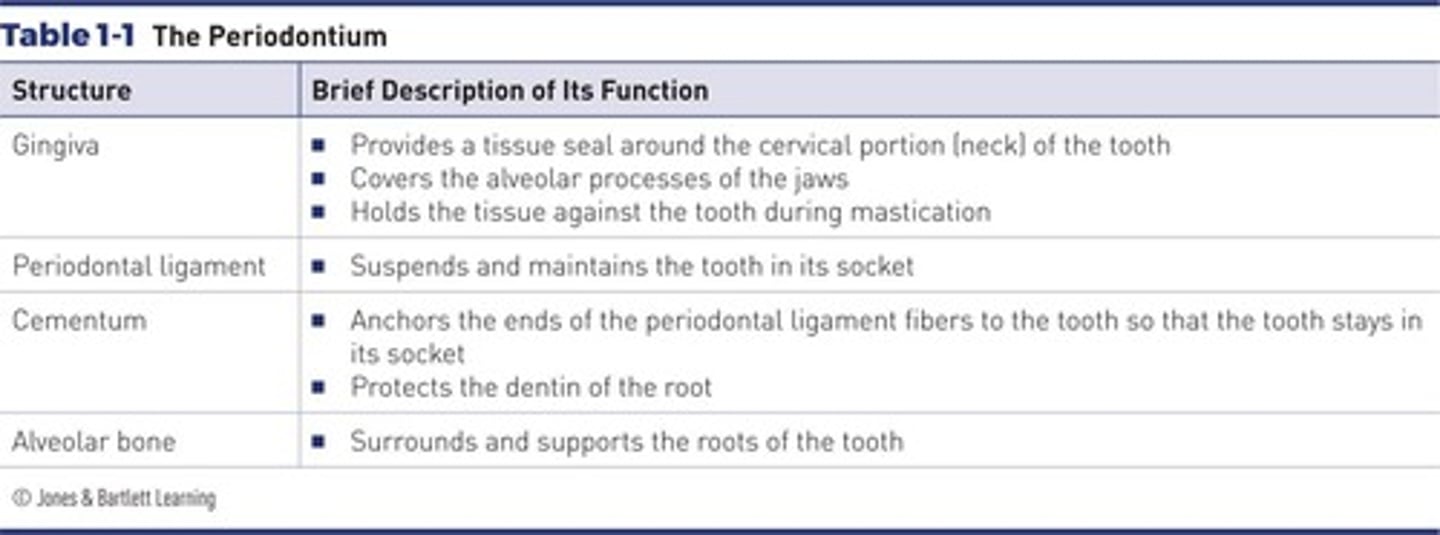
What is the definition of the periodontium?
The tissues/structures that surround, support, and are attached to the teeth.
What are the four physical units of a healthy periodontium?
Gingiva, periodontal ligament (PDL), alveolar process, and cementum.
What is the significance of maintaining the health of the periodontium?
It is the most significant factor in the longevity of the dentition.
What is the role of the gingiva in periodontal health?
It covers the alveolar process and the surrounding cervical portion of the teeth.
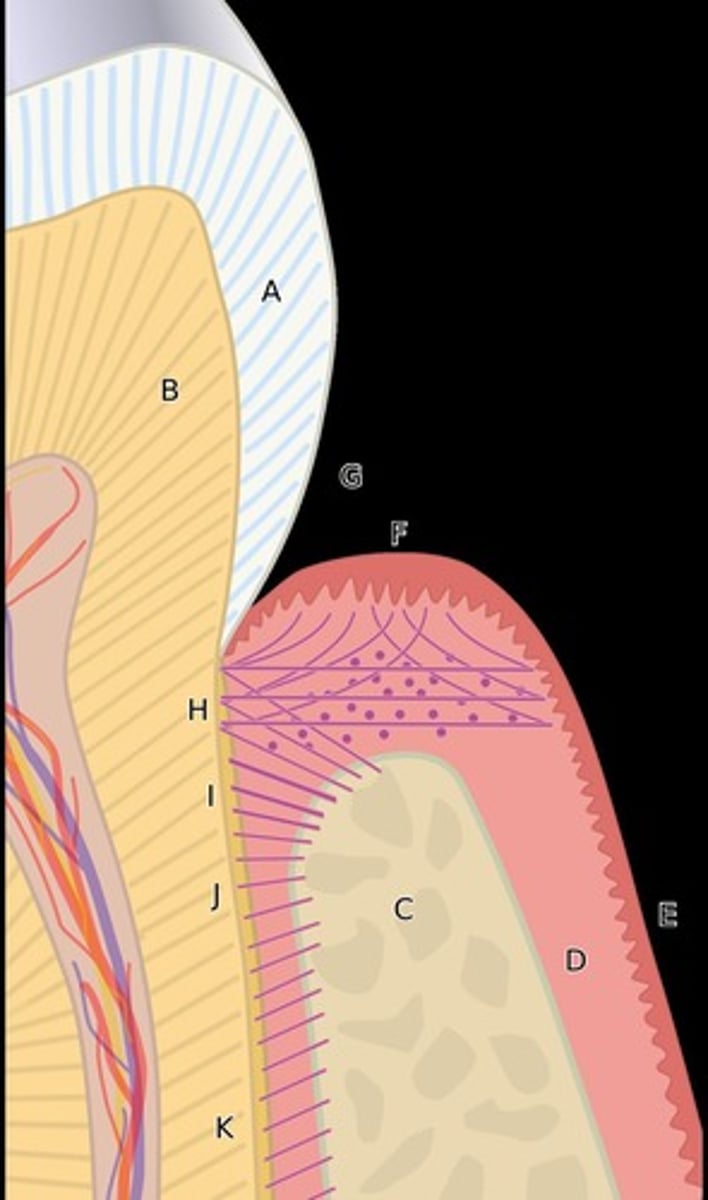
What is the periodontal ligament (PDL)?
Fibrous connective tissue that surrounds and attaches tooth roots to alveolar bone.
What is the function of the alveolar process?
It supports the teeth and where PDL fibers are anchored.
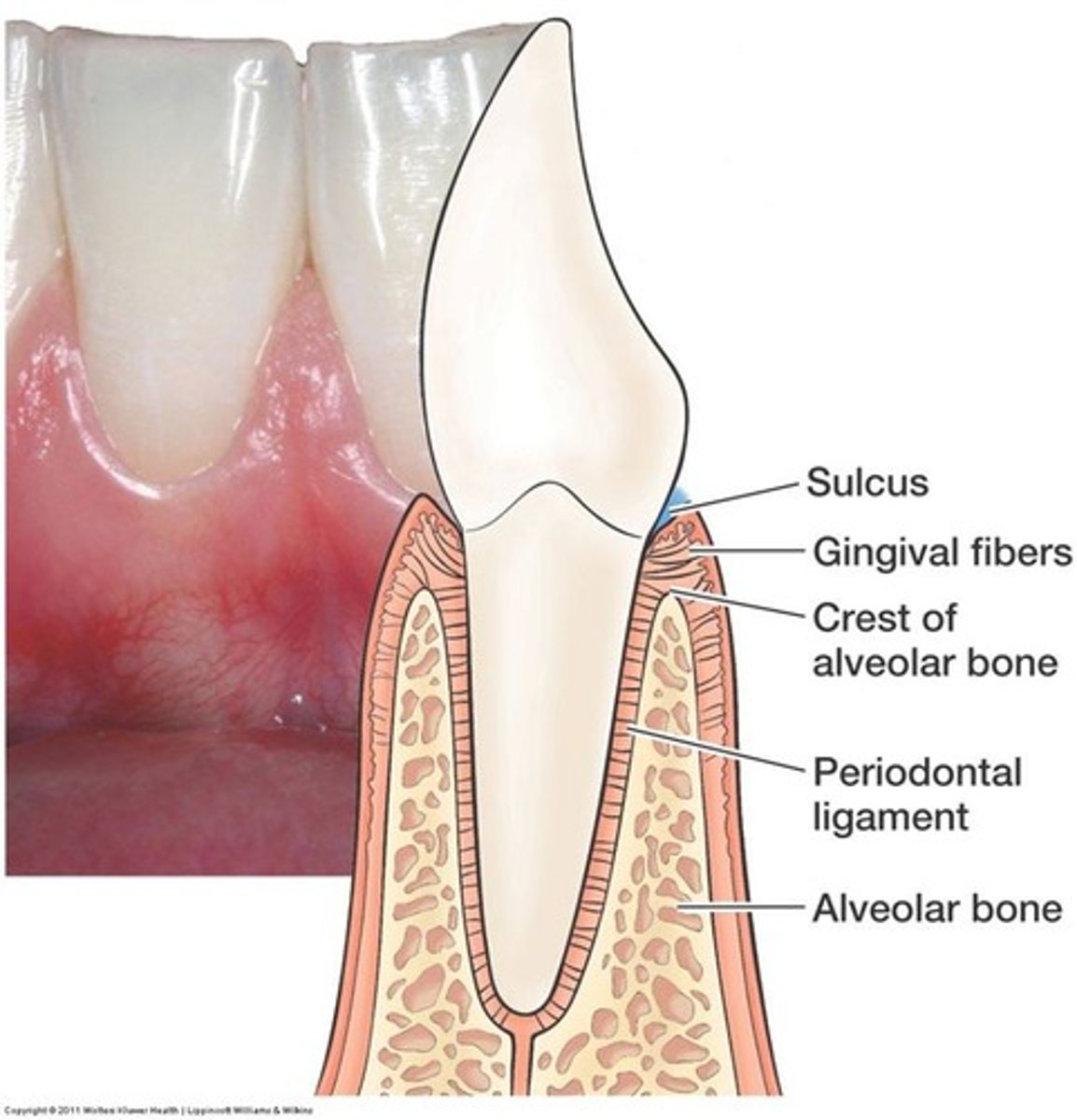
What is cementum?
A mineralized bonelike substance that covers the roots of the teeth and provides attachment for periodontal fibers.
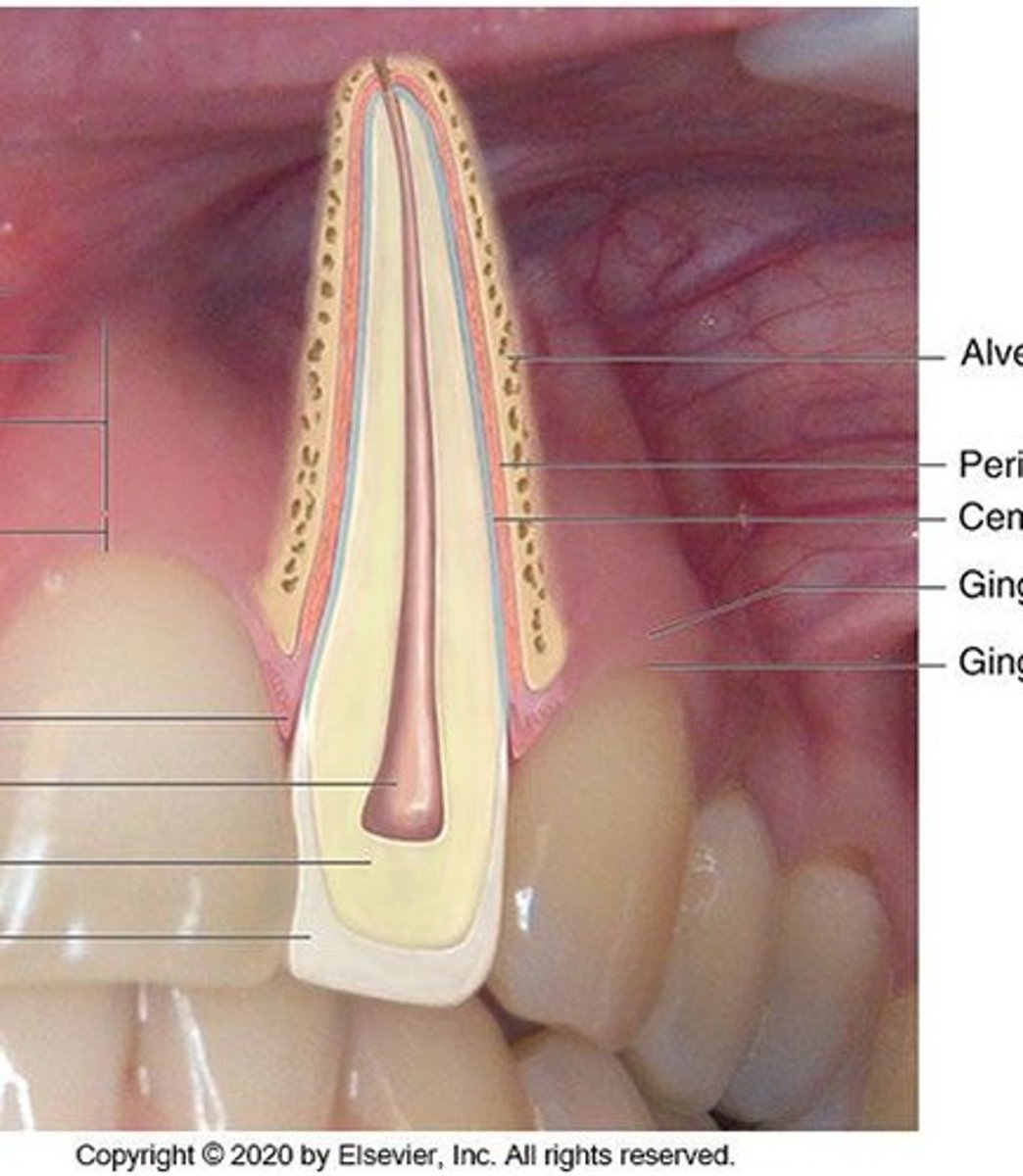
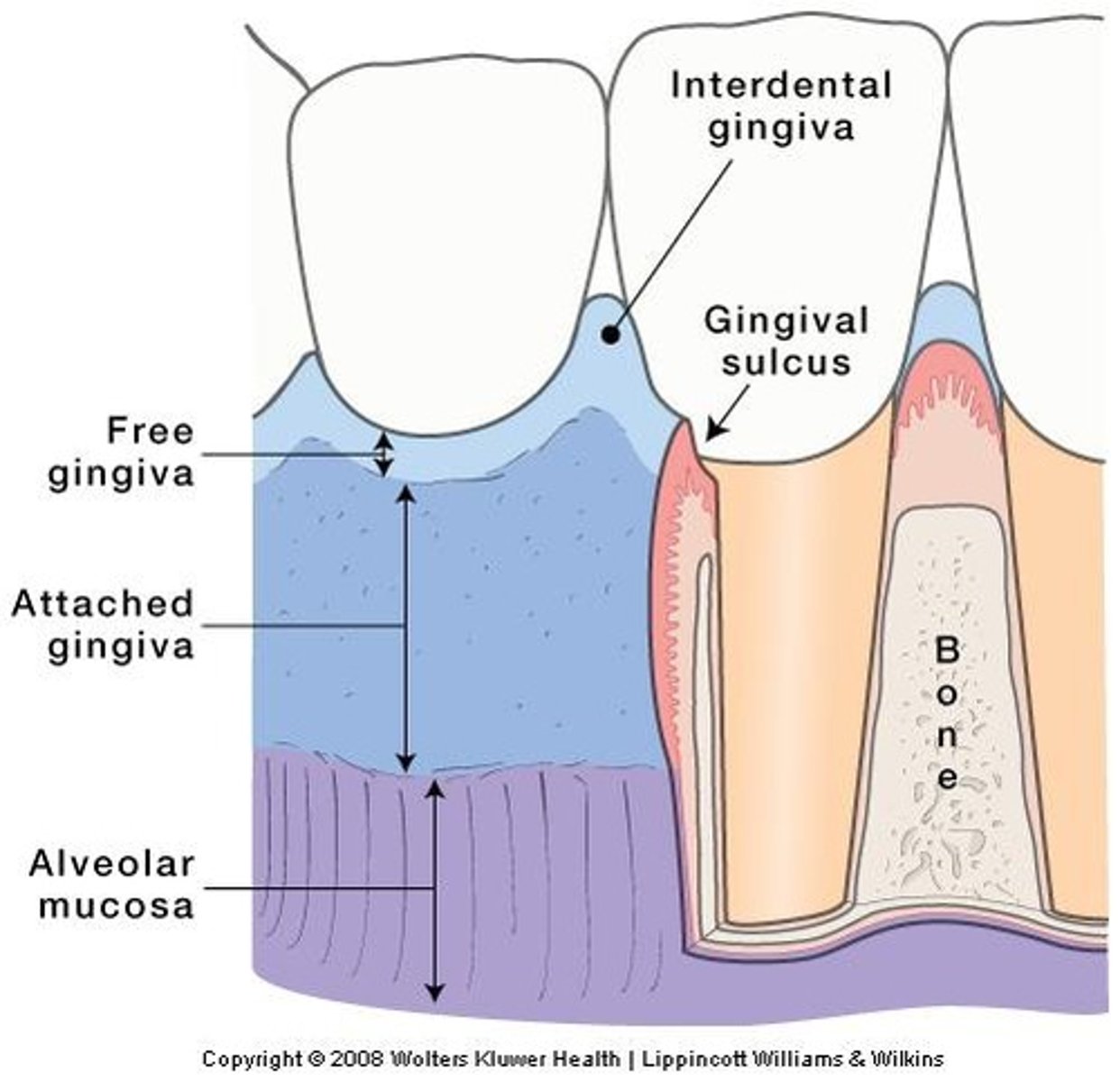
What are the boundaries of the gingiva?
Gingival margin and alveolar mucosa.
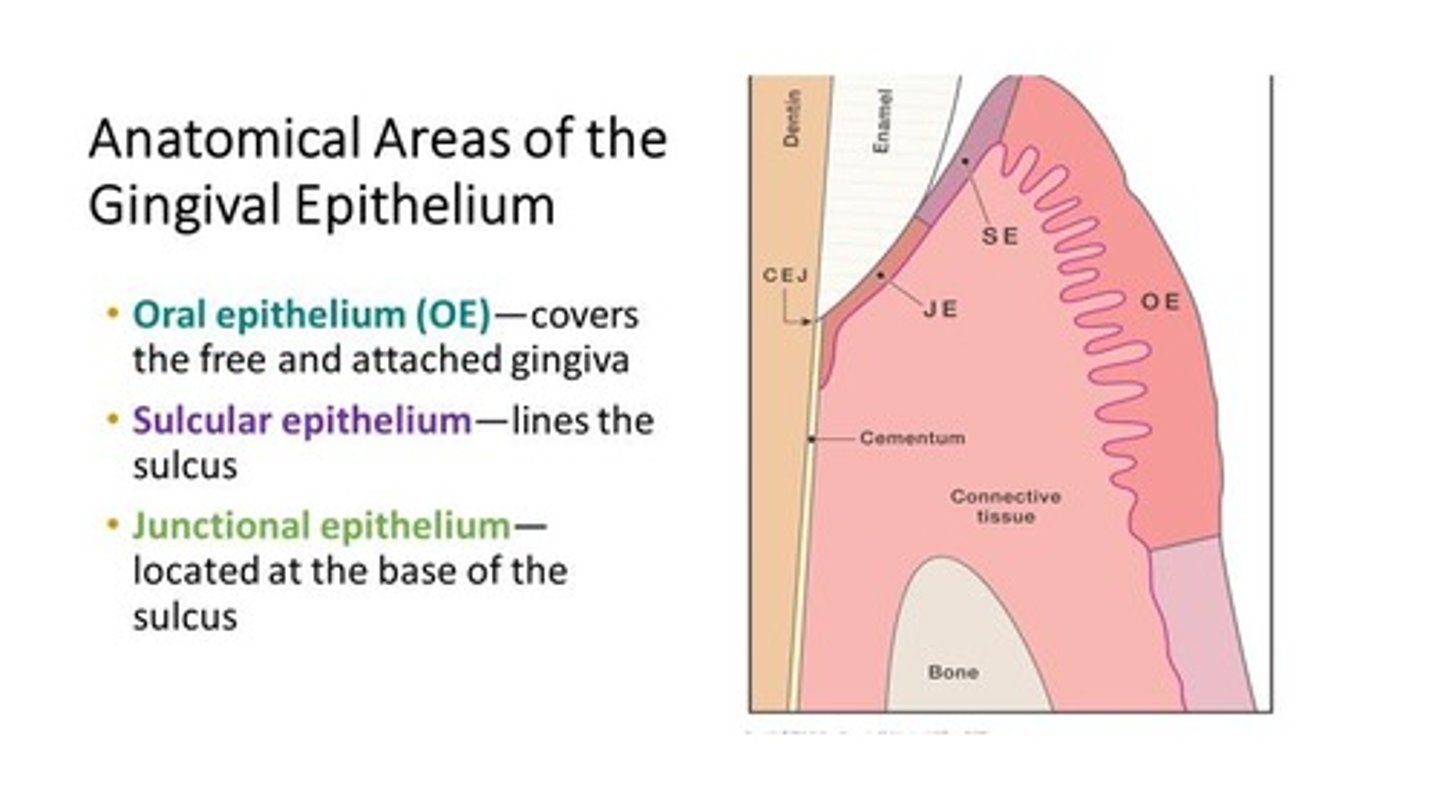
Where are the sulcular and junctional epithelium located?
The sulcural lines the sulcus and the junction is located at the base of the sulcus.
What is the free gingiva?
The part of the gingiva that surrounds the tooth like a turtleneck and is attached by the JE.
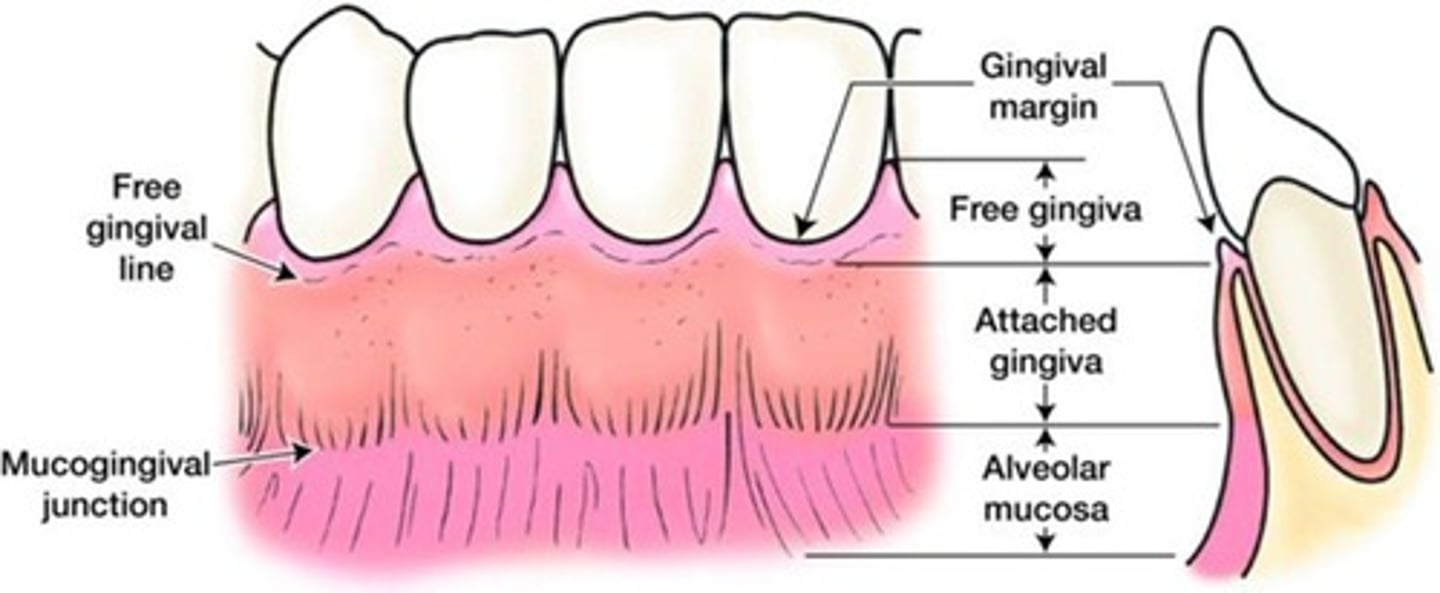
The free gingiva connects with what at the free gingival groove?
Attached gingiva
What is attached gingiva?
Continuous with free gingiva, tightly bound to the underlying cementum and periosteum of alveolar bone.
What is interdental gingiva?
The portion of the gingiva that fills the interdental embrasure between two adjacent teeth.
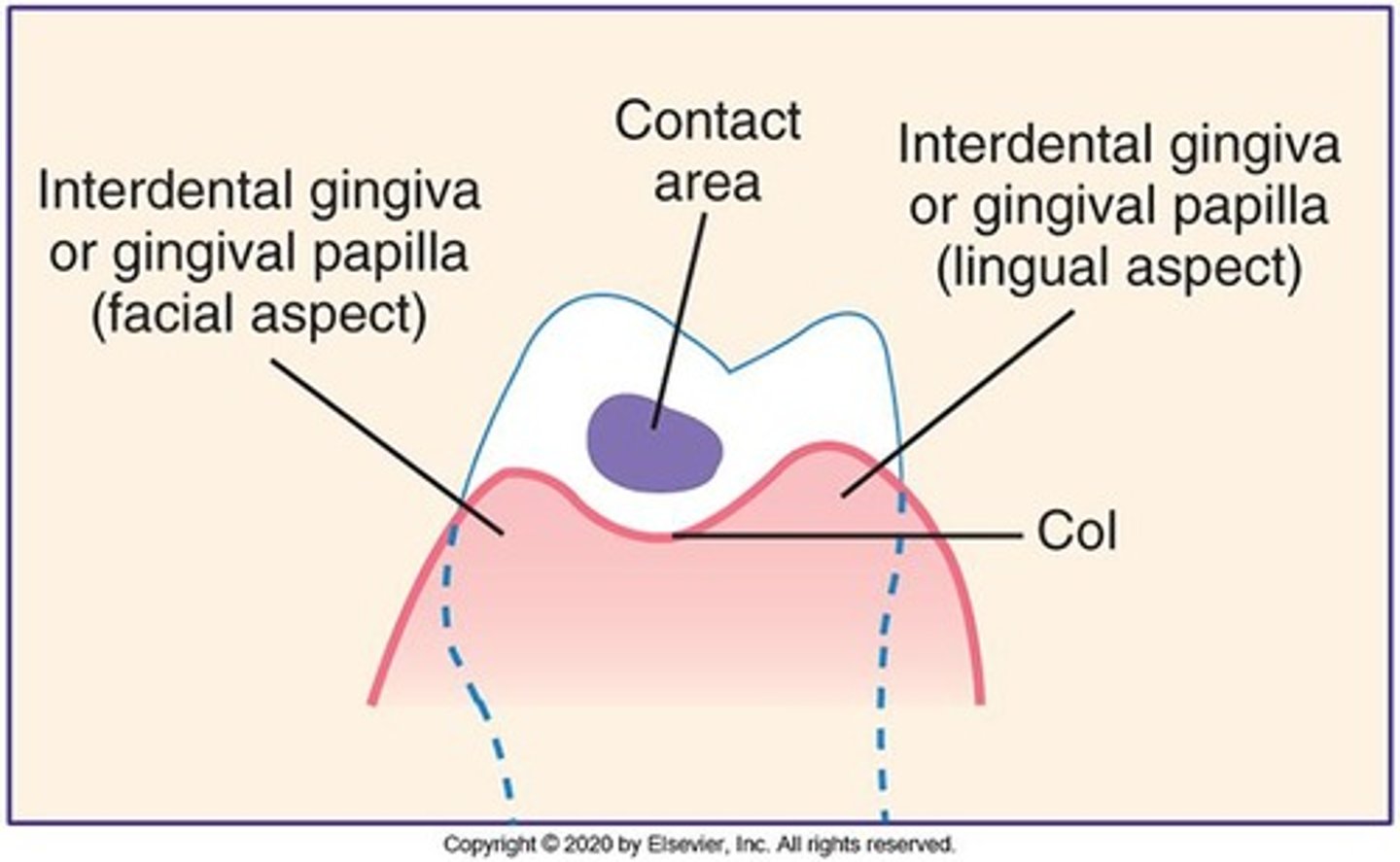
What is the function of the interdental col?
It connects the facial and lingual papillae and prevents food from packing between teeth when chewing.
What is the clinical appearance of healthy gingiva?
Coral pink color, firm consistency, and no bleeding upon probing.
What is the significance of the junctional epithelium (JE)?
It attaches the gingiva to the tooth at the coronal portion of the JE and is attached the base of the sulcus.
What is gingival crevicular fluid (GCF)?
A serum-like fluid secreted from underlying connective tissue into the sulcular space, part of the body's defense mechanism.
What factors influence gingival health?
Degree of vascularity, amount of melanin pigmentation, degree of epithelial keratinization, and thickness of epithelium.
What is the probing depth for healthy gingiva?
1-3 mm.
In healthy, gingivitis, and periodontally involved patients, where is the JE?
In healthy sulcus: JE is coronal to CEJ
Gingivitis: JE is at CEJ
Perio: JE is apical / on cementum
to CEJ
What are the characteristics of healthy tissue?
Firm, resilient tissue, coral pink color, normal stippling, and less than 10% bleeding.
Periodontal clinical assessment instruments include what?
Source of light, compressed air to dry tissues, mouth mirror, explorer, probe and current full mouth radio graphic series.
What are common local factors that influence gingival health?
Plaque/biofilm, calculus, restorative complications, appliances, and medications.
What is the role of the alveolar mucosa?
Moveable tissue that is loosely attached to underlying alveolar bone and smooth and shiny.
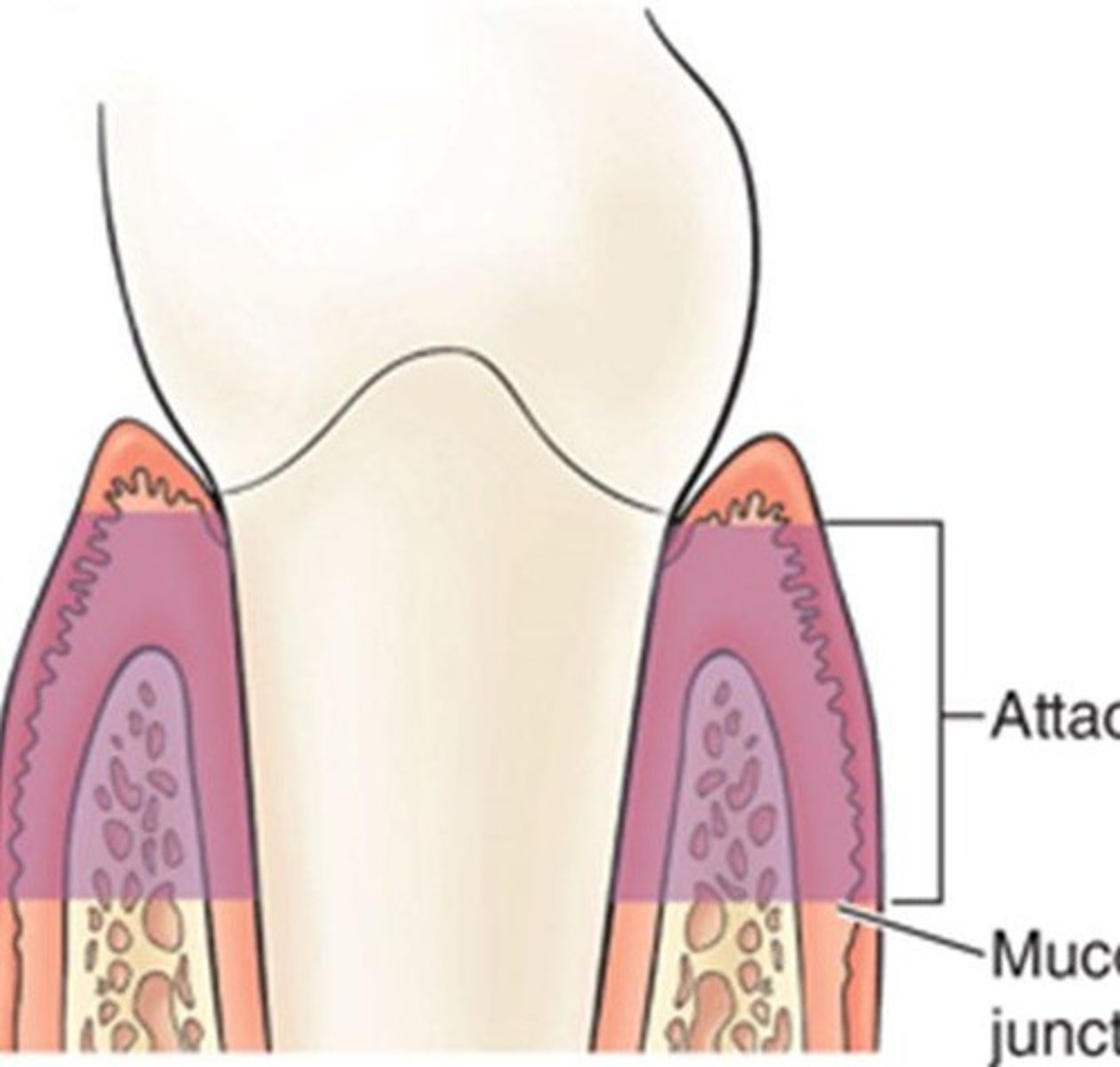
What is the significance of the mucogingival junction (MGJ)?
It separates the attached gingiva from the alveolar mucosa.
What are the signs of inflammation that may be present in gingival tissue?
Redness/erythema, swelling/edema, pain, loss of function, bleeding, and chronic bad taste.
What is the consistency of inflamed gingival tissue?
Soft and spongy.
What color variations can inflamed gingival tissue exhibit?
Red, bluish red, or pink if fibrotic.
What is the probing depth indicative of gingivitis?
4mm or greater.
What is the contour of diseased gingival tissue?
Irregular from edema, may be rounded, rolled, or bulbous. Coronal to CEJ.
What is the appearance of healthy gingival tissue?
Coral pink, but can vary in shade based on complexion and race.
What is the significance of stippling in healthy gingival tissue?
Healthy attached gingiva shows stippling, giving a pitted, orange-peel appearance.
What is the appearance of acute inflammation in gingival tissue?
Bright red due to inflammation and capillary dilation.
What does chronic inflammation in gingival tissue look like?
Dark red, bluish red, or deep blue due to engorged vessels.
What is the definition of mucogingival involvement?
When a pocket extends beyond the microbial junction into the alveolar mucosa.
Mucogingival involvement equals what?
IAG or inadequate attached gingiva.
What are the characteristics of healthy marginal gingiva?
Knife-edged, fits snugly, and tapers to meet the tooth at a fine edge.
What are the characteristics of diseased marginal gingiva?
Papillae may become bulbous, blunted, or cratered due to edema.
What is a McCall's festoon?
A life-saver shaped gingival contour often seen in gingival disease.
What causes gingival clefts?
Localized recession causing a V-shaped slit, often due to incorrect brushing or flossing.
What does the firmness of gingival tissue indicate?
Firmness indicates healthy tissue; edematous tissue is soft and spongy.
What is the significance of bleeding upon probing?
Bleeding is a sign of inflammation and should be documented.
What does gingival recession indicate?
Exposure of the root surface due to apical migration of the JE.
What is the difference between localized and generalized inflammation?
Localized affects up to 30% of tissue, while generalized affects more than 30%.
What role do dental hygienists play in periodontal health?
They assess periodontal health, diagnose diseases, educate patients, and implement therapy.
What is the objective of periodontal treatment?
To restore diseased tissues to a maintainable state of health.
What are the signs of unhealthy gingival tissue?
Smooth, shiny surface, loss of stippling, and potential hyperkeratosis.
What is the appearance of fibrotic gingival tissue?
Firm, hard, and usually a lighter, whitish pink.
What does generalized papillary edema indicate?
Swelling of the papillae, often a sign of inflammation.
What is the appearance of gingival enlargement?
Gingival margin positioned coronally due to swelling.
What is the effect of medications on gingival health?
Medications can cause gingival enlargement and changes in tissue appearance.
How to calculate ACTUAL attachment loss?
Pocket depth + recession. Pocket depth= gingival inflammation coronal to CEJ.
What is the difference between superbony and intrabony pockets?
Suprabony is horizontal and JE above crest and intrabony is vertical and JE bellow alveolar crest.
How do you calculate CAL when the gingival margin is coronal to the CEJ?
Probing depth MINUS gingival margin level
How do you calculate CAL when recession is present?
Probing depth PLUS gingival margin level
What is a gingival pocket?
When the JE is at the CEJ with supragingival fiber destruction.
What is a periodontal pocket?
When the JE is on the cementum and the PDL and alveolar bone are destroyed.
What is probing depth?
Mm from the gingival margin to the sulcus base or periodontal pocket.
What are the characteristics of the gingiva?
- Color
- Size
- Position of Margin
- Shape of Margins and Papillae
- Texture and Consistency
- Bleeding
- Exudate
Describe healthy gingiva.
- Tissue fits snugly around the tooth.
- Meets tooth at a fine edge.
- Papillae are pointed and fill the embrasure spaces.
- Firm, resilient tissue.
What changes in the margins are caused by disease?
Gingival margin becomes coronal to (above) or apical to (below) the cementoenamel junction.
What is the size of healthy gingiva?
Fits snugly around the tooth.
What is the size of diseased gingiva?
Englarged.
What is a normal margin position?
Near the cementoenamel junction, 1-2 mm coronal.
What is a unhealthy margin position?
More than 2 mm coronal to or apical to the cementoenamel junction.
What is a normal margin shape?
- Tapered and slightly rounded edge.
- Fits snugly around the tooth.
What shape of margin indicates disease?
- Rolled
- Festooned.
- Cleft.
What is a normal papilla shape?
- Flat, pointed papilla.
- Fits interproximal space.
What is a diseased papilla shape?
- Bulbous.
- Blunted.
- Cratered.
- Missing.
What is a normal texture of gingiva?
Stippled.
What is a diseased texture of gingiva?
- Smooth and shiny.
- Nodular.
What is a healthy consistency of gingiva?
- Firm.
- Resilient.
What is a diseased consistency of gingiva?
- Soft, flaccid.
- Spongy, puffy.
- Leathery.
- Not resilient.
What are the possible classifications of periodontal disease?
Health, biofilm-induced gingivitis, non-gingival disease, periodontitis, other periodontal conditions, or peri-implant diseases.
What are the two classifications of gingival diseases?
Dental biofilm-induced gingivitis and nonplaque-induced gingival diseases.
What factors can exacerbate periodontal destruction?
Systemic conditions such as sex steroid hormones, hyperglycemia, leukemia, smoking, and malnutrition.
What characterizes dental biofilm-induced gingivitis?
Inflammation of gingival tissue, presence of bacterial burden, bleeding on probing, reversible with biofilm removal, and no bone loss or apical migration.
What are oral factors that enhance plaque accumulation?
Subgingival restoration margins, hyposalivation, and drug-influenced gingival enlargements.
What are the three distinct categories of periodontitis according to AAP-EEP classification?
Periodontitis, necrotizing periodontal diseases, and other conditions affecting the periodontium.
What is the nature of periodontitis?
A chronic, multifactorial disease associated with dysbiotic plaque accumulation, cyclic in nature with periods of inactivity and exacerbation.
What is necrotizing periodontal disease characterized by?
Papillary necrosis, bleeding, and pain, typically with a rapid onset.
What defines peri-implant health?
Absence of redness, swelling, bleeding, and suppuration of the tissue surrounding a dental implant.
What is peri-implant mucositis?
Inflamed gingival tissue surrounding a dental implant characterized by redness, bleeding, swelling, and/or suppuration.
What is peri-implantitis?
A dental biofilm-induced disease that can also result from implant placement or surgical trauma.
What are the four stages of histopathologic changes in periodontal disease?
Initial lesion, early lesion, established lesion, and advanced lesion.
What are the signs of dental biofilm-induced gingivitis?
Changes in gingival color, bleeding on probing, swelling or edema, and presence of exudate.
What is a periodontal pocket?
A space that forms between the tooth and surrounding tissue, which can be suprabony or intrabony.
What is the clinical attachment level (CAL)?
The distance from the gingival margin to the base of the periodontal pocket.

What does furcation involvement indicate?
Loss of interradicular bone and periodontal support, assessed using a furcation probe.
What is the significance of radiographic images in periodontal assessment?
They are essential for assessing alveolar bone presence and loss, and identifying local bacterial biofilm retentive factors.
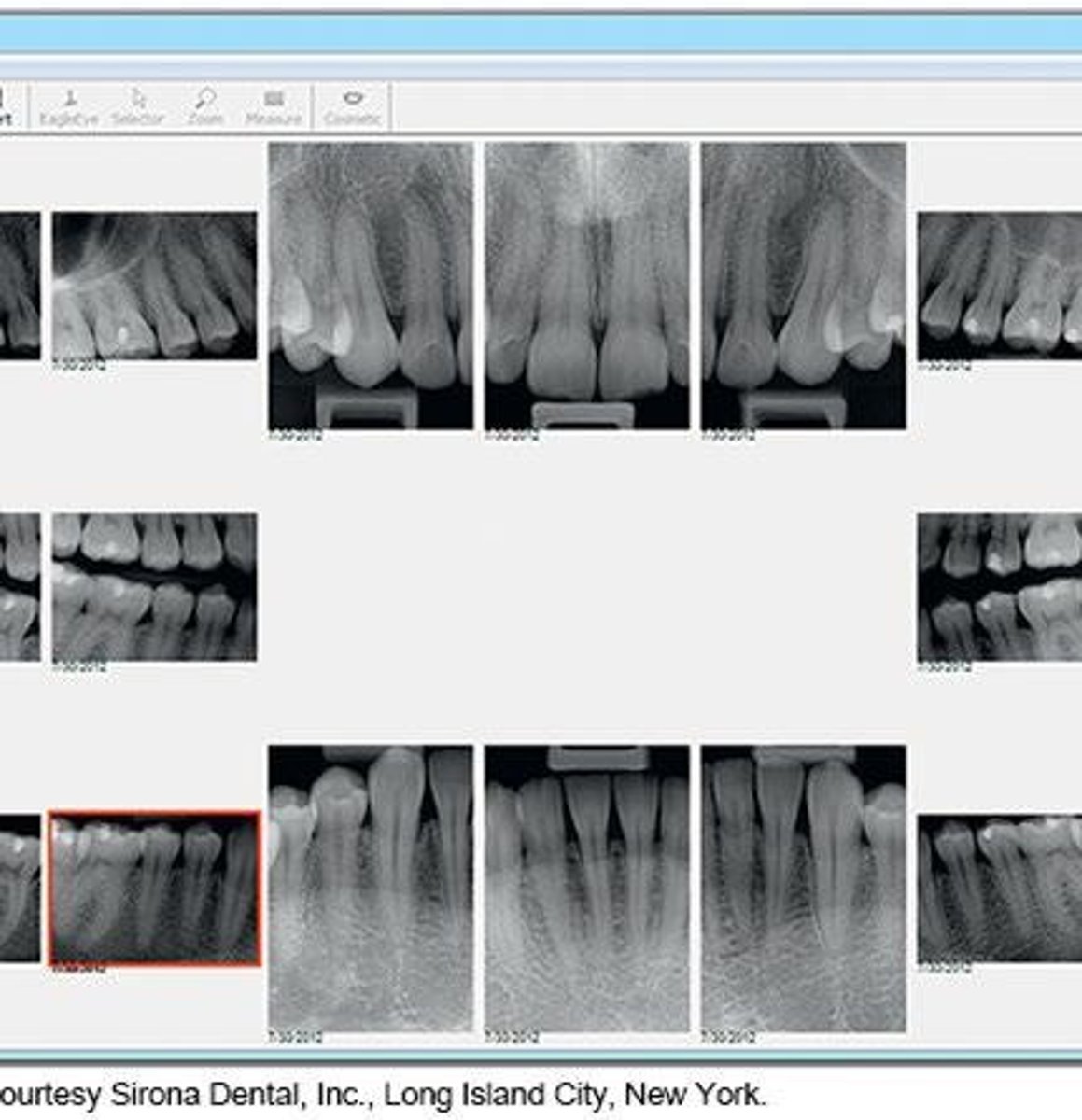
What types of radiographic images are preferred for evaluating periodontal disease?
Periapical and vertical bitewings; horizontal bitewings are not effective for moderate to severe bone loss.
What are the signs of disease progression in periodontitis?
Gingival recession, tooth mobility, fremitus, and clinical attachment loss.
What is the impact of occlusal traumatism on periodontal health?
It can lead to heavy forces and inadequate attached gingiva, contributing to periodontal disease.
What distance from the CEJ to crestal bone indicates evidence of periodontal disease?
A distance greater than 2 mm.
What is a reliable indicator of periodontal health?
Continuous absence of bleeding on probing (BOP).
What is the best method for determining periodontal disease activity?
Radiographs and probing, along with clinical signs of inflammation.
What is the significance of measuring attachment loss in periodontal disease?
An increase in distance from the CEJ to the base of the sulcus indicates disease progression.
What are salivary diagnostics used for in periodontal assessments?
To identify bacteria associated with periodontal disease.
What factors should be considered when assessing implant periodontal status?
BOP, suppuration, probing depth, radiographic bone loss, and implant mobility.

What is the most significant risk factor for periodontal disease?
Tobacco use.