ECG
1/55
Earn XP
Description and Tags
EMRG1230
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
ECG Paper
Made up of big and little boxes. Each big box contains 5 little boxes.
1 little box is 0.04 seconds
Each large box is 0.2 seconds
A full ECG is 10 seconds long
P wave
Formed as impulse is generated in atria. Represents atrial depolarization
Smooth round upright shape immediatly proceding QRS complex
Duration: <110 ms
Amplitude: <2.5 mm tall
What to look for with P wave?
If there is no P wave
If it is present but not followed by a QRS complex
Can give clues on Pacemaker site
P waves that vary in size and configuration
Morphology: upright or inverse
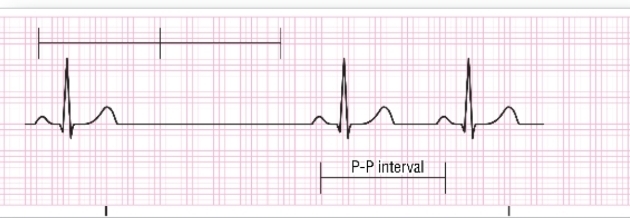
PR interval
Time it takes for atria to depolarize and impulse to get to the AV Node
A slight delay normally occurs
Measured from start of P wave until the begining of the QRS complex
Usually 0.12-0.20 seconds
First Degree AV Block
A PR interval that is longer than 0.20 seconds
May indicate injury to AV junction
Wolff-Parkinson-White Syndrome
PR interval shorter than 0.12 seconds is present in these cases
Variable PRI
Variable PRI may indicate either a wandering atrial pacemaker or a second-degree AV nodal block
PR depression may occurr with pericarditis
QRS Complex
Narrow with sharply pointed waves. Has a duration less than 0.12 seconds
Represents depolarization of simultaneously contracting ventricles
Should follow each P wave
Q Wave
First negative deflection after P wave
Can be present or absent
R Wave
First positive deflection after the P wave
if there is no Q wave visible, this will be the first initial wave of the QRS complex
S Wave
First negative deflection after the R wave
J Point
Point where QRS complex ends and ST segment begins
Represents end of ventricular depolarization and the beginning of ventricular repolerization
Note:
Locating the J point may make it easier to identify the ST segment when you are looking for elevation
ST Segment
Lime between the end of the QRS complex and beginning of the T wave
T Wave
Represents ventricular repolerization
Asymmetric and is half the size of the QRS wave
Typically have a slower uppstroke and a faster downstroke
TP Segment
Isoelectric line or baseline
Neither positive nor negative
Flat, straight, horizontal line that begins at the end of the T wave and ends at the start of the next P wave
QT Interval
Represents all the electrical activity of one complete ventricular cycle from ventricular depolarization to ventricular repolerization
Begins with onset of Q and ends at T
If no Q wave, Begins at R wave
Normally lasts 0.36 to 0.44 seconds varying based on HR, Age, Sex
QT Interval lengths
As the HR decreases, the QT interval shortens
As the HR increases, the QT interval lengthens
Prolonged QT indicates that the heart is experiencing an extended refractory period
5 Step Method To Reading an ECG Rhythm Strip
You will usually use lead II to perform rhythm interpretation; five-step method
Determine if the QRS complex is wide or narrow.
Identify the P waves and measure the PRI.
Determine the relationship of the P waves with the QRS complex.
Determine rhythm regularity.
Measure the heart rate.
When Reading RCG Rythm Strip
Use 120 ms as the cut-off between narrow and wide QRS complexes
Note whether P waves are upright and within normal parameters or absent.
Check PRI for evidence of AV nodal delay.
Is there only one P wave for every QRS complex
Determining HR (6 Sec Method)
Remember that the P wave rate and QRS complex rate may be different
Simplest and most accurate method when rhythm is irregular or between approximately 50 and 100
Count the number of QRS complexes in a 6-second strip, and multiply that number by 10 to obtain the rate per minute
Determining HR (Sequence Method)
Memorize the following sequence: 300, 150, 100, 75, 60, 50, 43, 38, 33.
Find an R wave on a heavy line and count off “300, 150, 100 . . .” until you reach the next R wave
If the R-R interval spans fewer than three large boxes, the rate is greater than 100.
If it covers more than five large boxes, the rate is less than 60.
Systematic Analysis of ECG Strip
Are QRS complexes present?
Are there P waves?
What is the PRI?
Is the rhythm regular or irregular?
What is the rate?
Specific Cardiac Dysrhythmias
AV node blocks or bundle branch blocks
Ventricular fibrillation
Bradycardias and tachycardias
Atrial fibrillation
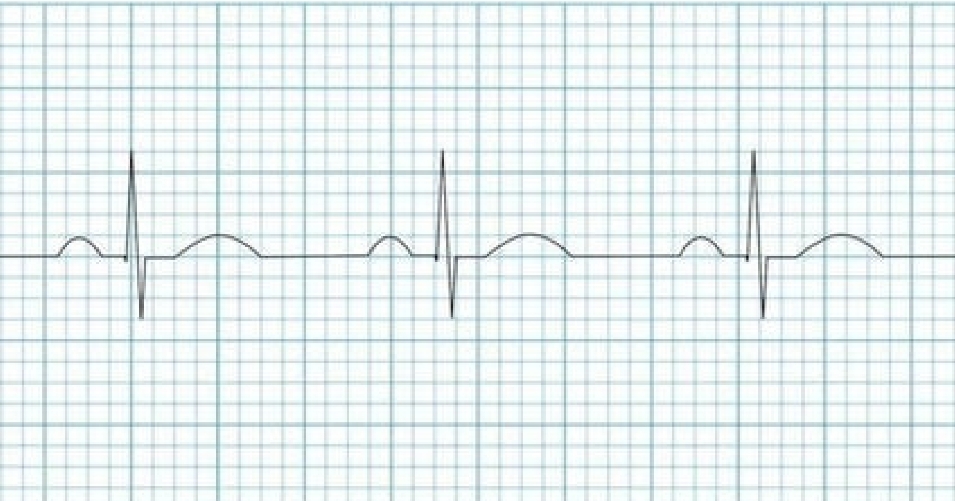
Normal Sinus Rythms
Intrinsic rate of 60 to 100 beats/minute
Regular, with minimal variation between RR intervals
P wave is present, upright, and precedes each QRS complex (<100ms wide)
Constant PR Interval
Sinus Bradycardia
Complexes and morphology the same as NSR, only the rate differs
Rate of less than 60 beats/minute
Rhythm is regular.
Treatment focuses on the patient’s tolerance to the bradycardia
Sinus Tachycardia
Rate of more than 100 beats/minute
Rhythm is regular.
Increases the work of the heart
Treatment is related to the underlying cause

Sinus Arrhythmia
Slight variation of a sinus rhythm
Bainbridge reflex- sudden changes in pressure
Increases SV and blood pressure
Normal finding in children and young adults

Sinus Arrest
SA node fails to initiate an impulse.
SA node resumes normal functioning.
Occasional episodes are not significant.
Treatment based on the overall HR and tolerance
Sick Sinus Syndrome
Encompasses a variety of rhythms. All evidence that the SA node is not functioning normally
Some patients may experience a syncopal or near syncopal episode, dizziness, and palpitations
Sinoatrial Block
Results from either the Pacemaker cells or the transitional cells failing to produce an impulse
After the dropped beat, the cycle continues on time
Characteristics:
Rate: varies
Irregular
P waves present, except when dropped
P:QRS- 1:1
QRS width is normal
Atrial Rhythms
Rhythms originating from the atria will have upright P waves that precede each QRS complex but that are not as well rounded as those coming from the SA node.
Wandering Atrial Pacemaker
Pacemaker moves from the SA node to various areas within the atria.
Rhythm is slightly irregular.
Patients with significant lung disease
Treatment is usually not indicated.


Supraventricular Tachycardia (SVT)
Typically, P waves are not present, due to the rate they are “buried” in the QRS complex
May sometimes appear inverted or retrograde
Regular rhythm
Narrow QRS (usually less the 120ms)
Rate typically 140-280 bpm
PSVT- Paroxysmal SVT
An abrupt onset and offset can be seen
Atrial Flutter
Atrial rate and ventricular rate will be different, (ventricular will be a fraction of the atrial)
Atrial commonly 250-350 bpm
Usually regular, but may be variable
P waves- “saw tooth” appearance
QRS width is normal
P:QRS ratio- variable, most commonly 2:1 but can
go higher
Atrial Fibrillation
No discernable P waves
QRS complexes are innervated haphazardly in an irregularly irregular pattern
Ventricular rate is guided by occasional activation from one of the pacemaker sources
QRS width is normal
Rate is variable, ventricular response can be fast or slow
Fibrillatory waves may mimic P waves- this will lead to misinterpretation
Multifocal Atrial Tachycardia (MAT)
HR >100, usually between 100-150
Irregularly irregular
At least 3 distinct P wave morphologies
Absence of single dominant arial pacemaker
Some P waves may be non conducted
Junctional Escape Rhythm
Junctional rhythm with a rate of 40-60 bpm
QRS complexes typically narrow (<120ms)
No relationship between the QRS complex and any preceding atrial activity
Regular rhythm
P waves may appear inverted, before, during or after
the QRS
Occurs when the rate of the supraventricular impulses arriving at the AV node or ventricle is less then the intrinsic rate of the ectopic pacemaker
Accelerated Junctional Rhythm
Occurs when the junctional pacemaker that is firing the impulses takes over the normal pacing function of the SA due to damage to/issues with normal conduction (slow SA)
Rate of 60-100
Regular
P wave may be absent, antegrade or retrograde
QRS width is normal
P:QRS- if present, 1:1, if absent, none
Junctional Tachycardia
Same etiology as junctional rhythms, however the rate is >100 bpm
P waves- retrograde
QRS- narrow
PR Interval is short
Regular rhythm
Premature Junctional Complex (PJC’s)
A beat that originates prematurely in the AV node. Travels through the normal conduction system of the ventricles, so the QRS complex it creates is identical to the others. Can occur sporadically or as part of a regular, grouped pattern (bigeminy, trigeminy)
Characteristics:
Narrow QRS either without a preceding P wave or a retrograde P wave
Occurs sooner then the next beat is expected
First Degree Heart Block
Characteristics:
Rate- depends on underlying rhythm
Regular
P waves- Normal
PR Interval- >0.20 seconds
Each impulse is delayed slightly longer. Impulse eventually passes.
Least serious of the heart blocks and is first indication of damage to the AV node
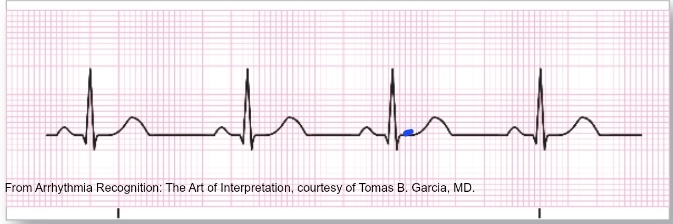
Second Degree Heart Block (Type 1) Wenckebach
Caused by a diseased AV node with a long refractory period. This results in the PR interval lengthening between successive beats until a beat is dropped. At that point, the cycle begins again
Characteristics:
Regularly irregular
Dropped beats
P:QRS- Variable
Second Degree Heart Block Type II
Groups beats with one dropped beet between each group
PR interval is THE SAME
Caused by a diseased AV node- typically indicative of worsening cardiac issues, specifically complete heart block
Third Degree Heart Block (Complete Block)
All impulses are prevented and ventricles develop their own pacemaker
Complete absence of AV conduction
None of the supraventricular impulses are conducted to the ventricles
Atria and ventricles firing separately
Typically a bradycardic rate
Idioventricular Rhythm (Wide and slow, It’s Idio)
Occurs when a ventricular focus acts as the primary pacemaker for the heart. QRS complexes are wide and bizarre
Characteristics:
Rate: 20-40 bpm
Regular
P waves- Absent
P:QRS- N/A
QRS Width- wide (>120ms/.120 s), bizarre appearance
Accelerated Idioventricular Rhythm (AIVR)
Characteristics:
Rate of 40-100 bpm
Regular rhythm
P waves- Absent
QRS: Wide (>0.12s), bizarre appearance
Faster version of Idioventricular rhythm
Ventricular Tachycardia (V-Tach)
Rate exceeding 100 beats/minute; QRS complex will measure greater than 0.12 s
Regular, with no variation between RR intervals
P waves are not normally visualized.
QRS complexes are monomorphic.
Polymorphic
Extremely serious
Sustained- duration of > 30 seconds or requiring intervention due to hemodynamic instability
Non Sustained- 3 or more consecutive ventricular complexes terminating spontaneously in <30 seconds
Monomorphic V-Tach
Regular rhythm
Originated form a single focus within the ventricles
Produces uniform QRS complexes
Classified as stable vs. non stable
Polymorphic V-Tach
A form of Ventricular Tachycardia in which there are multiple ventricular foci and the resultant QRS complexes vary in size and shape.
Most common cause is myocardial ischemia
Torsades De Pointes
Occurs when there is an underlying prolonged QT interval
A type of polymorphic V-Tach
Axis of the QRS complex changes from positive to negative in a haphazard fashion
Means “twisting of points”
Can convert to NSR or V Fib- treat this vey carefully as it precursor/notifier of death!
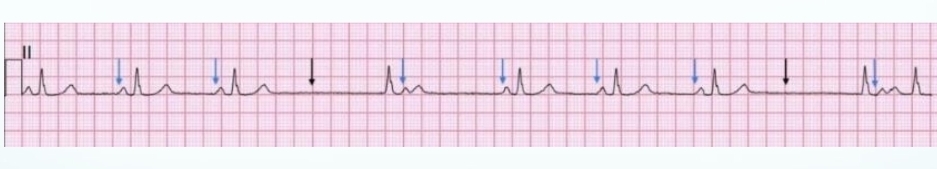
Premature Ventricular Complex (PVC)
Caused by the premature firing of the ventricular cell. Ventricular pacer fires before the SA node. This causes the ventricles to be in a refractory state when the normal impulse tries to get through, causing the ventricles do not fire at their normal time
Underlying pacing rhythm/schedule is not altered, so the beat following the PVC will arrive on time
This is a compensatory pause
Multifocal Vs Unifocal
Multifocal- arising from 2 or more ectopic foci. Results in multiple QRS morphologies
Unifocal- arising from a single ectopic foci. Results in each PVC looking identical
Repeating Pattern Types for PVC’s
Couplet- two consecutive PVC’s
Bigeminy- every other beat is a PVC
Trigeminy- every third beat is a PVC
Quadrigeminy- every fourth beat is a PVC
Ventricular Fibrillation (V-Fib)
Rhythm in which the entire heart is no longer contracting. Quivering without organized contraction, cardiac chaos, approx. 500 bpm firing
Random depolarization of many cells
Rhythm most commonly seen in cardiac arrests
Responds well to defibrillation
CPR compressions help make the heart more susceptible to defibrillation
Asystole
“Flatline”
Entire heart is no longer contracting.
Many cells have no energy for contraction.
Generally a confirmation of death
May be treated in certain circumstances