Congenital Heart Disease
1/66
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
67 Terms
Ductus venosus, oval foramen, ductus arteriosus
What are the 3 structures that are the most important in the transition from fetal cardiovascular system to the neonatal cardiovascular system?
placenta → umbilical vein → ductus venous → IVC → RA → oval foramen → LA → LV → Aorta (ductus arteriosus) → systemic blood flow
Describe the route of blood flood for the fetus starting at the placenta
directs blood flow from RA through oval foramen into LA
What is the purpose of the crista dividens?
10% of the blood passes into the RV → pulmonary vessels → lungs
How do the fetal lungs get their oxygen
sphincter in the ductus venosus constricts, increased pressure in LA closes the oval foramen, flow in the DA reverses due to increased pulmonary vascular resistance, DA closes due to oxygen and prostaglandins, umbilical arteries constrict
What changes occur at birth to transition the cardiovascular system as the neonate’s lung expand and begin to function
foramen ovale closes in 1 hour, DA in 2-3 days (decrease in prostaglandin), left side becomes dominant in 6-8 weeks
When do the changes after birth occur?
bicuspid aortic valve
What is the most common congenital heart disease?
prematurity (2-3x), family hx (3x), genetic syndromes, maternal factors, assisted reproductive technology (ART), in utero infection (TORCH)
Risk factors for congenital heart disease
cyanotic congenital heart disease
What includes lesions that allow circulation of deoxygenated blood in the systemic circulation via intracardiac/extracardiac shunting
left to right shunts
What is characterized by when oxygenated blood from the left heart/aorta shunts to the right side of the heart/pulmonary artery through communication between the 2 sides?
obstructive lesions
What occurs when blood flow is obstructed, causing a pressure gradient across the obstruction; pressure overload proximal may result in hypertrophy and HF
ASD (atrial septal defect)
What is characterized by an opening in the atrial septum allowing the flow of blood between the 2 atria
ostium secundum (most common), ostium primum, sinus venosus, coronary sinus
Types of atrial septal defect
other congenital heart defects, family hx, thalidomide/EtOH/smoking exposure in utero, maternal age 35 yr+
Risk factors for ASD
Holt-Oram, Ellis-van Creveld, VACTERL syndrome, Noonan syndrome
What conditions are often associated with ASDs
asymptomatic in childhood, found on routine physical
What are some characteristics of small ASDs?
right-sided HF, recurrent respiratory infections, failure to thrive
What are some characteristics of a large ASD
age 40 (atrial arrhythmias, exercise intolerance, dyspnea, fatigue)
In uncorrected ASDs, when do folks become symptomatic
Echo (transthoracic doppler, maybe transesophageal)
3 y/o male presents to the clinic for a routine physical. While conducting a physical you note the child is small for his age. You also note a fixed, widely split S2, RV heave, a palpable pulmonary pulse at LUSB, and an S4. What diagnostic test do you want to order?
systolic ejection murmur, low-pitched diastolic rumble, diastolic murmur, systolic murmur
Other than the fixed, wide S2 split, what other murmurs might you see with ASD?
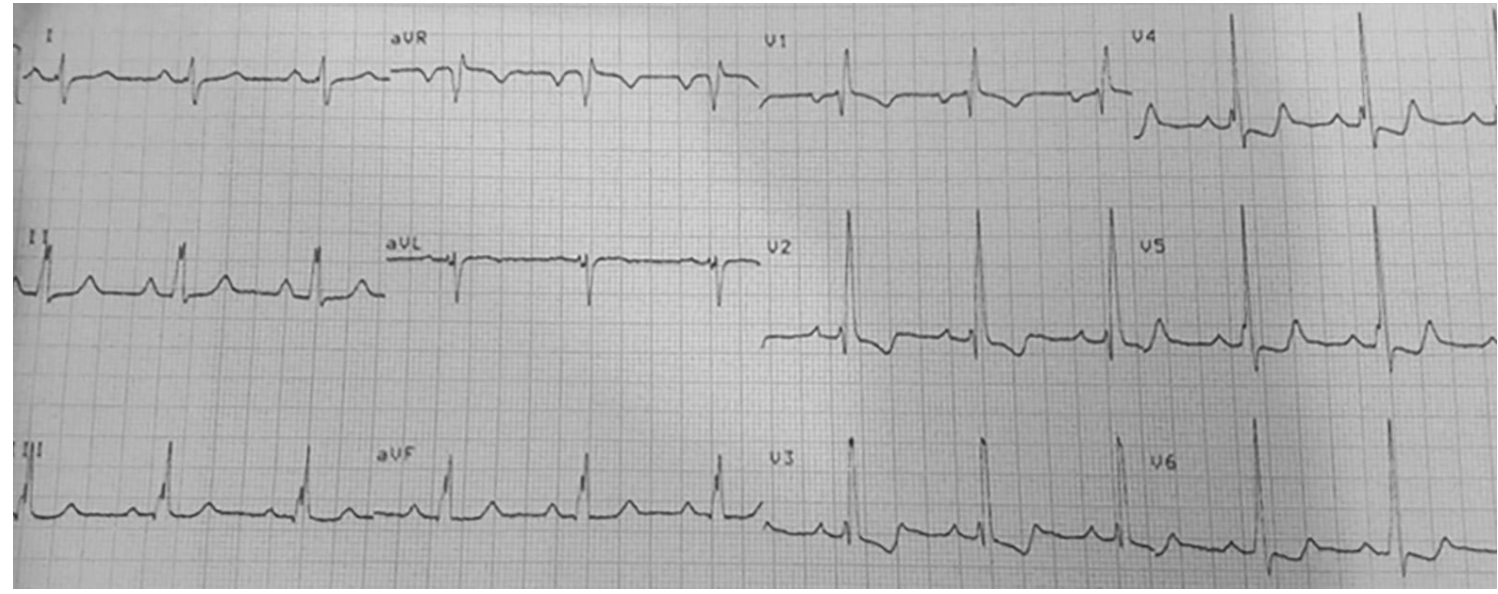
RAD, RAE, RV conduction delay, Q in V1, RBBB, crochetage pattern
What might you see on EKG for ASD?
close follow up, most (75%) spontaneously close
What is the treatment plan for small secundum ASDs (less than 8mm)
8 mm+, primum and sinus venosus, coronary sinus
Which ASDs require surgical closure?
treat a fib like a fib (anticoag and cardioversion, rate control) treat HF like HF (diurectics, oxygen, digoxin, etc), pulmonary vasodilator therapy
1st line medication treatment for ASD
Recommended before dental or invasive procedures for 6 months after closure, and longer if there's residual shunting near a prosthetic device; Not given for unrepaired/isolated lesions
When do we give antibiotics (amoxicillin, azithromycin) for ASD
defect 8+mm in kids older than 2, any size in child 5+ with related symptoms
When is surgical closure of ASD indicated in children?
Right side heart enlargement, pulmonary systemic flow ratio 2:1 (if under 21 than 1.5:1), documented shortness of breath when standing (playpnea), orthodeoxia, paradoxical embolism
When is surgical closure via percutaneous transcatheter device of ASD indicated in adults?
irreversible severe pulmonary HTN (shunt is keeping them alive), no symptoms, small asymptomatic secundums
When are we NOT closing an ASD?
VSD (ventricular septal defect)
Second most common congenital heart defect that is characterized by a defect of the interventricular septum that allows communication of blood between the LV and RV (also occurs as a complication of AMI)
Eisenmenger Complex
What happens with a VSD over time as the RV gets swole and the flow reverses becoming a right to left shunt?
family hx, prematurity, prenatal exposure to weed, ibuprofen, organic solvents, febril illness
Risk factors of a congenital VSD
1st MI, HTN, 1st week after MI, anterior MI
Risk factors of a VSD as a result of a MI
membranous (most common 70%), muscular, AV canal type, supracristal
Types of congenital VSD
Cardiac Cath (gold standard), echo,
1 month old infant reports to the clinic for failure to thrive. On a physical exam you note tachypnea and tachycardia. You auscultate a harsh holosystolic murmur at LLSB with a thrill, diastolic rumble at apex, and an increased intensity of P2. What diagnostic test do you want to order
harsh holosystolic murmur at LLSB detected at 4-8 weeks
What might you hear with a small VSD?
holosystolic murmur throughout the precordium with diastolic rumble at apex with precordial bulge and hyperactivity (maybe no murmur), if CHF than tachycardia, tachypnea, hepatomegaly
What might you find with a large VSD?
cyanosis, clubbing, holosystolic murmur throughout the precordium with diastolic rumble at apex with precordial bulge and hyperactivity (maybe no murmur)
What might you find with a large VSD with Eisenmeneger’s complex
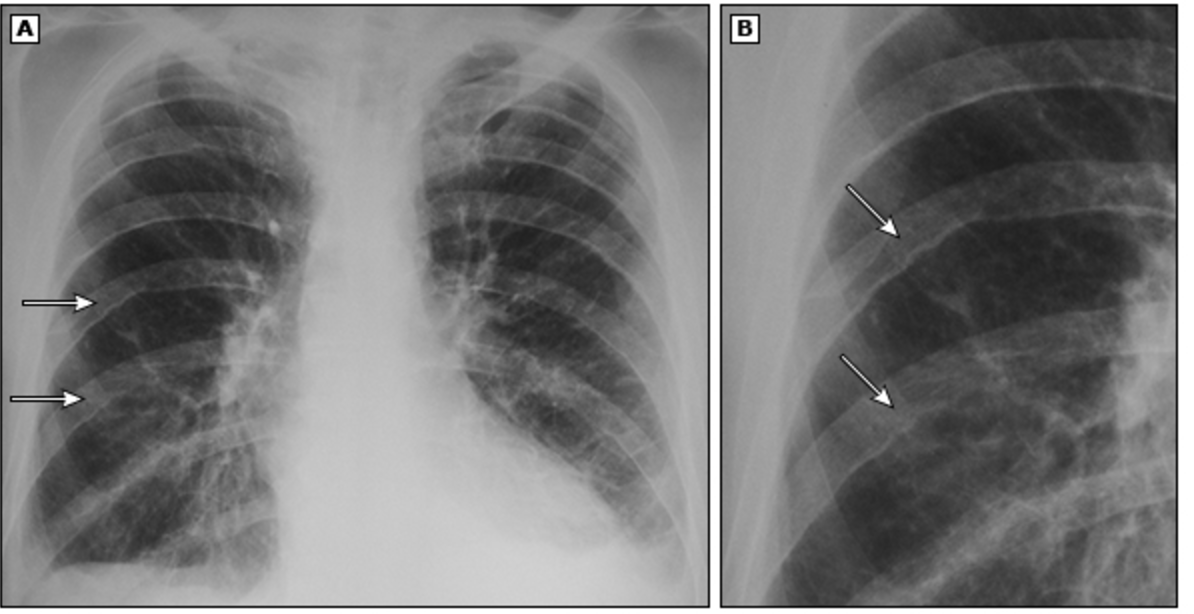
12 lead (LVH, LAE, RVH), CXR (haziness in the lungs, cardiomegaly), Echo, Color flow doppler (direction of flow, estimated RV pressure)
What other tests could you use for VSD?
Watch for overload (diuretics, minimize IV fluids), ACEI, digoxin, NG feeds, treat anemias
General game plan for VSD
Complex cyanotic heart disease is present, 6 months following repair, if any residual lesions are present post surgery
When are we giving VSD peeps antibiotics prophylactically?
furosemide, spironolactone, captopril, digoxin
Medication treatments of VSD (Peds)
digoxin, diuretics
Medication treatments of VSD (grown folks)
pulmonic-systemic flow is more than 2:1, poorly controlled pulmonary circulation, infant with persistent pulmonary HTN/failure to thrive
Indication for surgical repair of VSD
Corrected with patch or repair (RBBB are common afterward)
How are VSDs surgically repaired?
Small ones may close spontaneously, Large ones causing CHF/failure to thrive need repair
Prognosis of congenital VSD
worse with anterior MI, 80-90% mortality in 1st 2 weeks
Prognosis of post-MI VSD
PDA (patent ductus arteriosus)
Persistence of the fetal communication between the descending aorta and main pulmonary descending (normally closes due to O2 and decreased prostaglandins)
Echo with doppler (transesophageal), CXR, Cardiac MRI/CT, cardiac cath
2 y/o Patient presents to the clinic for a routine check up. The mother notes that the child becomes very tired and breaths heavily when playing. While auscultating the heart you note a washing machine murmur over the left scapula, a displaced apex beat, increased JVP. What diagnostic tests do you want to order?
Qp:Qs less than 1.5:1
What is classified as a small PDA
Qp:Qs 1.5-2.2:1
What is classified as a moderate PDA
Qp:Qs more than 2.2:1
What is classified as a severe PDA
LAE, LVH, if pulmonary HTN has occurred RAD, RVH, RAE
What might you see on EKG with someone with a PDA
NSAIDs (indomethacin, ibuprofen)
Treatment of PDAs in premature infants
signs of volume overload, pulmonary HTN, audible murmur
When should PDAs be closed (DO NOT CLOSE IF EISENMEYER IS THERE)
Coarctation of the aorta (CoA)
A constricting lesion at any point along the aorta (usually congenital) that causes outflow obstruction and HYN proximal to the site with LV pressure overload, myocardial hypertrophy, and possible HF
male, turners syndrome family Hx
Risk Factors for CoA
biscuspid aortic valve, PDA, VSD, mitral valve abnormalities, turners syndrome, transposition of the great vessels, aneurysm of circle of willis
Conditions commonly associated with CoA
Echo, CXR (rib notching), EKG (RVH, LVH), BNP
3 y/o Patient presents to the ER for syncope. Mother reports that he hasn’t eating well and gets tired very easily. On a physical you note a brachial-femoral pulse delay, upper extremity HTN, prominent neck pulsations, and corkscrew tortuosity of retinal arteries. What diagnostic tests do you want to order?
Alprostadil (prostaglandins) continuous IV infusion, short term esmolol/nitroprusside, longterm beta blocker and ACEI, manage HF
What is the medication game plan for ductal dependent CoA?
surgical correction, balloon angioplasty
How is CoA repaired in neonates, infants, and small children? In older children and adolescents?
VSD, pulmonary valve stenosis, overriding aorta, RV hypertrophy
4 thangs in tetralogy of Fallot
Echo, CXR (boot heart), cardiac cath, cardiac MRI, CBC (polycythemia), ABG, EKG (RAD, RVH, RAE), exercise testing
A 3 y/o male presents to the clinic for failure to thrive. The mother notes that he has extreme dyspnea on exertion and gets into a squatting position. On a physical exam you note cyanosis of the nail beds, digital clubbing, a palpable RV impulse, systolic thrill along left sternal border, crescendo/decrescendo systolic murmur LUSB with posterior radiation. What diagnostic tests do you want?
tet spells
paroxysmal episodes of worsening cyanosis with rapid and deep breathing that occurs when there is transient increase RV outflow tract obstruction
persistent foramen ovale, ASD, pulmonary artery anomalies, Right aortic arch, left superior vena cava to coronary sinus, additional VSDs, coronary artery anomalies, aortic regurg
ToF is associated with what other cardiac defects?
O2, prostaglandins, phenylephrine (increase systemic vascular resistance), morphine (decrease pulmonary resistance), Beta blockers (decrease RV outflow tract)
Treatment plan for ToF
close VSD with patch, relieve RV outflow obstruction
Complete surgical repair of ToF
increase pulmonary blood flow, improve O2 sats to allow for pulmonary artery growth
Palliative surgery of ToF