Biosci 221 Exam 4
5.0(1)
Card Sorting
1/26
Earn XP
Last updated 12:27 AM on 5/23/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
1
New cards
low dose organisms
if an organism has a low infective dose, the water treatment process would have to kill off or filter out every last organism to prevent potential illness
2
New cards
resistant organisms
organisms that are resistant to the methods of water treatment, like disinfection
3
New cards
Indicator Organisms and Why do we use them?
* Testing for the organisms rather than testing for the contamination
* We rely on them for public health as we can not afford and nor would we have the time and resources to test all water for all concerns. So we rely on indicator organisms to indicate that there is a problem. Most of the concerning organisms are associated with feces → so we don’t want to drink water that has feces in it
* We rely on them for public health as we can not afford and nor would we have the time and resources to test all water for all concerns. So we rely on indicator organisms to indicate that there is a problem. Most of the concerning organisms are associated with feces → so we don’t want to drink water that has feces in it
4
New cards
What are the characteristics of an **ideal indicator**?
(enteric = intestinal)
* Suitable for analysis of all types of water
* Present whenever enteric pathogens are present
* Survives longer than the hardiest enteric pathogen
* Most of the indicator organisms we use DO NOT fulfill this requirement
* Does not reproduce in contaminated water
* Its level in water reflects the degree of fecal pollution
* Detected by highly specific test
* Tests are easy to do and sensitive
* Harmless to humans
* Suitable for analysis of all types of water
* Present whenever enteric pathogens are present
* Survives longer than the hardiest enteric pathogen
* Most of the indicator organisms we use DO NOT fulfill this requirement
* Does not reproduce in contaminated water
* Its level in water reflects the degree of fecal pollution
* Detected by highly specific test
* Tests are easy to do and sensitive
* Harmless to humans
5
New cards
Examples of indicator organisms
* Which ones would we use and why
* Which ones would we use and why
* **Coliforms**
* Tells us that there is LIKELY fecal contamination, but it doesn’t say there is ABSOLUTELY fecal contamination
* Like E. coli ← the most abundant bacteria in feces
* **Enterococci**
* Increasingly used to test brackish and marine water
* Studies found a higher correlation to intestinal illness
* Also used with refrigerated and frozen foods
* More __cold__ tolerant than coliforms
* i.e *Enterococcus faecalis* ← the most common GPC in the intestines
* Fecal organisms like nice warm, high nutrient conditions → put them in the cold, low nutrient waters, what would their survival look like?
* Studies show that Enterococci in recreational waters have a higher correlation with actual illness
* **Fecal coliforms**
* A subset of coliforms
* More specific to really identify that these coliforms REALLY ARE of fecal origin
* Likely to get FALSE NEGATIVES
* **Coliphage**
* Viruses that are specific to *E. coli*
* Even after *E. coli* dies off, coliphage will still be there
* Coliphage stands a better chance of lasting longer and could be more successful as an indicator that could last as long as the hardiest enteric pathogen
* Tells us that there is LIKELY fecal contamination, but it doesn’t say there is ABSOLUTELY fecal contamination
* Like E. coli ← the most abundant bacteria in feces
* **Enterococci**
* Increasingly used to test brackish and marine water
* Studies found a higher correlation to intestinal illness
* Also used with refrigerated and frozen foods
* More __cold__ tolerant than coliforms
* i.e *Enterococcus faecalis* ← the most common GPC in the intestines
* Fecal organisms like nice warm, high nutrient conditions → put them in the cold, low nutrient waters, what would their survival look like?
* Studies show that Enterococci in recreational waters have a higher correlation with actual illness
* **Fecal coliforms**
* A subset of coliforms
* More specific to really identify that these coliforms REALLY ARE of fecal origin
* Likely to get FALSE NEGATIVES
* **Coliphage**
* Viruses that are specific to *E. coli*
* Even after *E. coli* dies off, coliphage will still be there
* Coliphage stands a better chance of lasting longer and could be more successful as an indicator that could last as long as the hardiest enteric pathogen
6
New cards
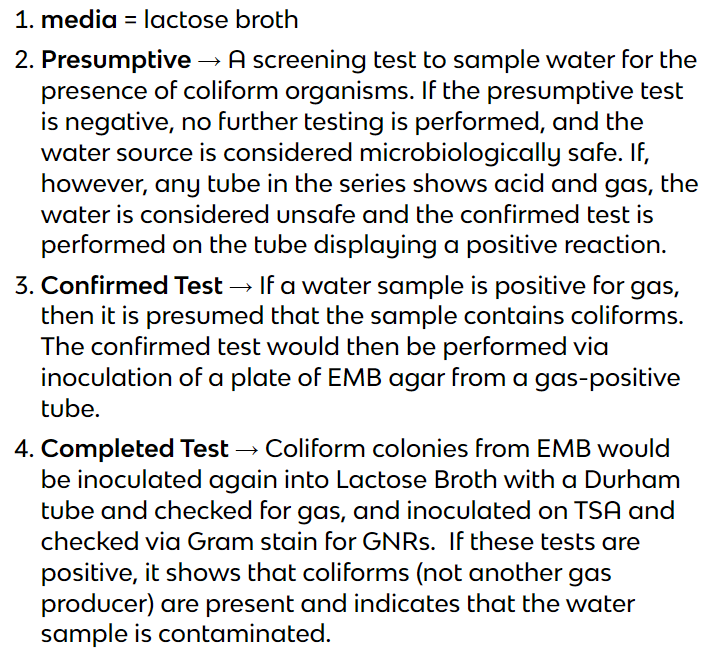
**Water testing** - What are the advantages and disadvantages of each method
__No acceptable__ level for fecal coliforms, enterococci, viruses, or pathogenic protozoans in drinking water
* **MPN**
* aka Most Probable Number
* Presumptive, confirmatory, and completed tests (photo)
* ADVANTAGES
* Reliable, easy, cheap, test
* Lactose broth is a very nurturing media, so even stressed bacteria may be nurtured into a more viable state
* DISADVANTAGES
* You only get a statistical estimation
* Time-consuming (takes 6 days)
* does not differentiate between coliforms and fecal coliforms
* **Membrane Filtration**
* Not a required test, but frequently performed b/c it is a quick way of identifying coliform
* After filtration, the filter is placed on selective and differential media, incubated, then colonies are presumptively identified and counted
* ADVANTAGES
* Quicker than MPN
* Can filter large quantities of water
* You will get an actual count
* DISADVANTAGES
* You are taking potentially injured/fragile/VBNC organisms, and putting them onto a harsh medium which leads to FALSE NEGATIVES → need to do more tests
* **HPC**
* Heterotrophic Plate Count
* Shows us an estimate of how many (heterotrophic) bacteria might be in the water
* We would not expect there to be a lot of organisms growing in water - if there are, that would indicate a general concern as to why
* shows the effectiveness of disinfectants used in water treatment
* ADVANTAGES
* Shows a range of bacteria, not just potential pathogens
* DISADVANTAGES
* Doesn’t indicate the specific bacteria (is not specific for coliforms)
* **MPN**
* aka Most Probable Number
* Presumptive, confirmatory, and completed tests (photo)
* ADVANTAGES
* Reliable, easy, cheap, test
* Lactose broth is a very nurturing media, so even stressed bacteria may be nurtured into a more viable state
* DISADVANTAGES
* You only get a statistical estimation
* Time-consuming (takes 6 days)
* does not differentiate between coliforms and fecal coliforms
* **Membrane Filtration**
* Not a required test, but frequently performed b/c it is a quick way of identifying coliform
* After filtration, the filter is placed on selective and differential media, incubated, then colonies are presumptively identified and counted
* ADVANTAGES
* Quicker than MPN
* Can filter large quantities of water
* You will get an actual count
* DISADVANTAGES
* You are taking potentially injured/fragile/VBNC organisms, and putting them onto a harsh medium which leads to FALSE NEGATIVES → need to do more tests
* **HPC**
* Heterotrophic Plate Count
* Shows us an estimate of how many (heterotrophic) bacteria might be in the water
* We would not expect there to be a lot of organisms growing in water - if there are, that would indicate a general concern as to why
* shows the effectiveness of disinfectants used in water treatment
* ADVANTAGES
* Shows a range of bacteria, not just potential pathogens
* DISADVANTAGES
* Doesn’t indicate the specific bacteria (is not specific for coliforms)
7
New cards
Be able to describe 1 method of controlling bacterial growth in food besides using temperature (cooking and refrigerator/freezing)
* **Modified Atmospheric Packaging (MAP)**
* Food packed in low O2 or high CO2 limits growth and prevents abiotic oxidation
* By modifying the atmosphere of the package, it inhibits microbial growth and prevents fungal growth
* Effective and significantly helps to preserve foods w/o damaging those foods or creating any unhealthy byproducts
* **Food Irradiation**
* Food is exposed to ionizing radiation, which sterilizes food and improves shelf life
* Hazards to workers involved in the irradiation process
* Radiation affects food chemistry
* Despite being approved by the FDA (as it could possibly save lives if it were utilized), many experts report changes in high protein foods (i.e. rubbery textures, unappetizing odors, etc.)
* **Bacteriophages**
* Use of bacteriophages that kill: *Listeria, monocytogenes, Salmonella* (Salmonelex), *E. coli* 0157:H7, *Campylobacter*
* Has been approved by the FDA but has not been actively utilized either
* Food packed in low O2 or high CO2 limits growth and prevents abiotic oxidation
* By modifying the atmosphere of the package, it inhibits microbial growth and prevents fungal growth
* Effective and significantly helps to preserve foods w/o damaging those foods or creating any unhealthy byproducts
* **Food Irradiation**
* Food is exposed to ionizing radiation, which sterilizes food and improves shelf life
* Hazards to workers involved in the irradiation process
* Radiation affects food chemistry
* Despite being approved by the FDA (as it could possibly save lives if it were utilized), many experts report changes in high protein foods (i.e. rubbery textures, unappetizing odors, etc.)
* **Bacteriophages**
* Use of bacteriophages that kill: *Listeria, monocytogenes, Salmonella* (Salmonelex), *E. coli* 0157:H7, *Campylobacter*
* Has been approved by the FDA but has not been actively utilized either
8
New cards
Define, in detail, Foodborne Infection versus Foodborne Intoxication
* **Foodborne Infection**
* Ingesting of whole microbes that target the intestine
* *Salmonella, Shigella, Campylobacter, Listeria (very important b/c it has the highest fatality rate of any of these, especially to pregnant women and their fetuses), E. coli (specifically the STECs/0157:07)*
* A significant cause of morbidity and mortality in the U.S.
* **Foodborne Intoxication**
* Results from ingesting exotoxins secreted from bacterial cells growing in food
* Caused by organisms such as Staphylococcus aureus or Clostridium botulinum
* Ingesting of whole microbes that target the intestine
* *Salmonella, Shigella, Campylobacter, Listeria (very important b/c it has the highest fatality rate of any of these, especially to pregnant women and their fetuses), E. coli (specifically the STECs/0157:07)*
* A significant cause of morbidity and mortality in the U.S.
* **Foodborne Intoxication**
* Results from ingesting exotoxins secreted from bacterial cells growing in food
* Caused by organisms such as Staphylococcus aureus or Clostridium botulinum
9
New cards
Know the differences between infection and intoxication
* **Infection**
* The infection comes from ingesting the bacteria and then having them grow and cause symptoms in the body
* Yes, they produce enzymes and toxins to cause symptoms and damage to the body but, unlike intoxication, it is the growth of the bacteria causing the symptoms
* Treating with an antibiotic could be successful
* Longer incubation period
* More likely to have fevers and lower intestinal symptoms
* **Intoxication**
* Intoxication comes from ingesting toxins in the food, those toxins got there by bacteria growing in the food, but it is not the bacteria that cause the symptoms, it is the toxins ALREADY produced.
* Again, it is purely the toxin causing the illness
* Treating with an antibiotic would be worthless
* Have to recover on your own or be treated with an antidepressant
* Onset times are quicker
* More likely to have vomiting
* The infection comes from ingesting the bacteria and then having them grow and cause symptoms in the body
* Yes, they produce enzymes and toxins to cause symptoms and damage to the body but, unlike intoxication, it is the growth of the bacteria causing the symptoms
* Treating with an antibiotic could be successful
* Longer incubation period
* More likely to have fevers and lower intestinal symptoms
* **Intoxication**
* Intoxication comes from ingesting toxins in the food, those toxins got there by bacteria growing in the food, but it is not the bacteria that cause the symptoms, it is the toxins ALREADY produced.
* Again, it is purely the toxin causing the illness
* Treating with an antibiotic would be worthless
* Have to recover on your own or be treated with an antidepressant
* Onset times are quicker
* More likely to have vomiting
10
New cards
Discuss why it is important to know and understand the difference between an infection and intoxication (think of 3 important points related to diagnosis, treatment, and prevention)
Food infection and food intoxication are 2 types of food poisoning. However, both of these terms are in contrast to the diagnosis, treatment, and prevention. Knowing the differences between food infections and food intoxication is essential to ensure effective management and recovery.
Food infection is caused by pathogens when ingested. Treat with an antibiotic? Prevent food infections by heating your food properly and avoiding raw milk and unpasteurized dairy products and juices.
On the other hand, food intoxication is primarily caused due to the presence of toxins in the food consumed. Vomiting is a key symptom of intoxication because the body wants to immediately get rid of the toxin and the fastest way to do that is by vomiting it out. A prolonged bout of vomiting can cause the body to be dehydrated so drink plenty of liquids. Prevent food intoxication by cleaning your food, your kitchen area, and your hands before and when handling food; as well as properly chilling food and cooking food.
Food infection is caused by pathogens when ingested. Treat with an antibiotic? Prevent food infections by heating your food properly and avoiding raw milk and unpasteurized dairy products and juices.
On the other hand, food intoxication is primarily caused due to the presence of toxins in the food consumed. Vomiting is a key symptom of intoxication because the body wants to immediately get rid of the toxin and the fastest way to do that is by vomiting it out. A prolonged bout of vomiting can cause the body to be dehydrated so drink plenty of liquids. Prevent food intoxication by cleaning your food, your kitchen area, and your hands before and when handling food; as well as properly chilling food and cooking food.
11
New cards
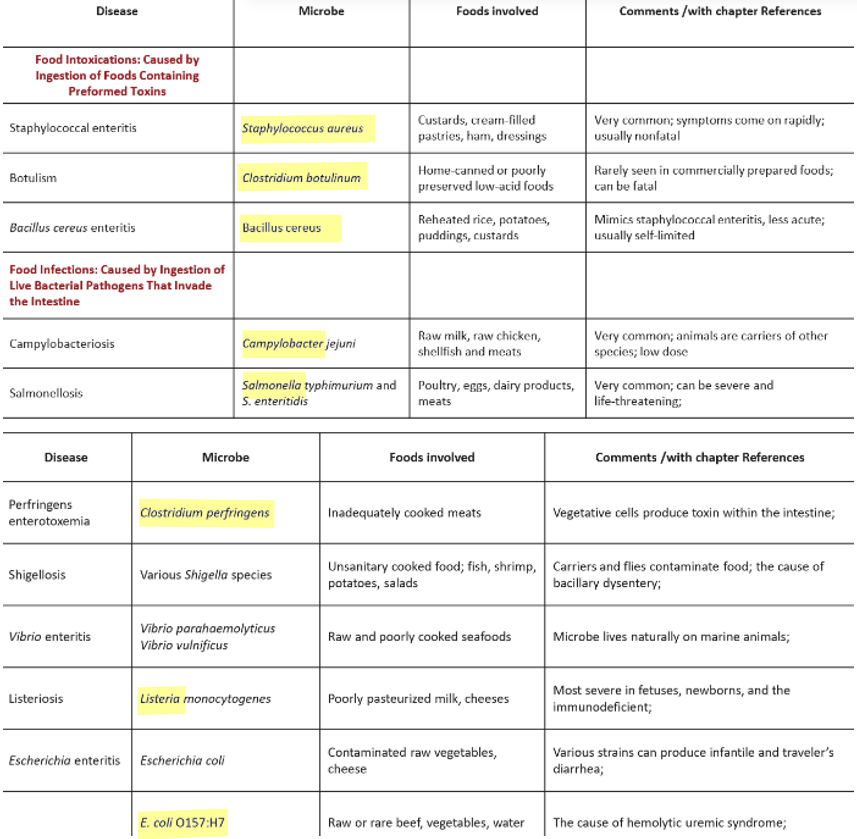
**Examples of each (infection and intoxication)** (names of bacteria and characteristics of those various ones we learned about before - *Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, Clostridium botulinum, Salmonella, E. coli 0157:H7, Campylobacter, Listeria)*
* *Staphylococcus aureus*
* Food intoxication
* Causes Staphylococcal enteritis
* Very common; symptoms come on rapidly; usually nonfatal
* *Bacillus cereus*
* Food intoxication
* Causes Bacillus cereus enteritis
* Mimics staphylococcal enteritis but is less acute; usually self-limited (ultimately resolving itself w/o treatment)
* *Clostridium perfringens*
* Food infection
* Causes Perfringens enterotoxemia
* Vegetative cells produce toxins within the intestine
* *Clostridium botulinum*
* Food intoxication
* Causes Botulism (note: toxin is sensitive to heat)
* Rarely seen in commercially prepared foods; can be fatal
* *Salmonella*
* Food infections (usually caused by S. typhimurium and S. enteritidis)
* Causes Salmonellosis
* Very common; can be severe and life-threatening
* *E. coli 0157:H7*
* Food infection
* Causes Escherichia enteritis
* The cause of hemolytic uremic syndrome (a condition that affects blood and blood vessels)
* *Campylobacter*
* Food infection (usually caused by C. jejuni)
* Causes Campylobacterosis
* Very common; animals are carriers of other species; low infective dose
* *Listeria*
* Food infection
* Causes Listeriosis
* Most severe in fetuses, newborns, and the immunodeficient
* Food intoxication
* Causes Staphylococcal enteritis
* Very common; symptoms come on rapidly; usually nonfatal
* *Bacillus cereus*
* Food intoxication
* Causes Bacillus cereus enteritis
* Mimics staphylococcal enteritis but is less acute; usually self-limited (ultimately resolving itself w/o treatment)
* *Clostridium perfringens*
* Food infection
* Causes Perfringens enterotoxemia
* Vegetative cells produce toxins within the intestine
* *Clostridium botulinum*
* Food intoxication
* Causes Botulism (note: toxin is sensitive to heat)
* Rarely seen in commercially prepared foods; can be fatal
* *Salmonella*
* Food infections (usually caused by S. typhimurium and S. enteritidis)
* Causes Salmonellosis
* Very common; can be severe and life-threatening
* *E. coli 0157:H7*
* Food infection
* Causes Escherichia enteritis
* The cause of hemolytic uremic syndrome (a condition that affects blood and blood vessels)
* *Campylobacter*
* Food infection (usually caused by C. jejuni)
* Causes Campylobacterosis
* Very common; animals are carriers of other species; low infective dose
* *Listeria*
* Food infection
* Causes Listeriosis
* Most severe in fetuses, newborns, and the immunodeficient
12
New cards
**Concerns in milk** - raw milk and pasteurized milk (think about the article too)
* Milk comes from a living source and contains many bacteria naturally
* Difficult to control bacteria growing in and on cows
* Contamination during the milking process
* 10 coliforms/ml is the standard for **raw milk**
* No matter how clean a dairy may be, it is difficult to be sure that cows are not carrying any potential pathogens, even frequent testing will not detect all, that is why consuming raw milk IS a risk
* **Pasteurized milk**
* Pasteurization reduces the number of bacteria and should kill off pathogens
* Difficult to control bacteria growing in and on cows
* Contamination during the milking process
* 10 coliforms/ml is the standard for **raw milk**
* No matter how clean a dairy may be, it is difficult to be sure that cows are not carrying any potential pathogens, even frequent testing will not detect all, that is why consuming raw milk IS a risk
* **Pasteurized milk**
* Pasteurization reduces the number of bacteria and should kill off pathogens
13
New cards
Phosphatase test
Checks for the presence of phosphatase, the enzyme is destroyed by heat and should not be present after pasteurization
14
New cards
Microscopic counts for bacteria and white blood cells
High numbers of white blood cells could indicate an ill cow in the mix
15
New cards
Antibiotic residual
It is crucial that a cow that has been on an antibiotic does not contribute milk for a specified amount of time so there is no chance that residual antibiotics can still be in the system
* There are many individuals who have antibiotic allergies
* There are many individuals who have antibiotic allergies
16
New cards
Food, Water and Milk Discussion:
BE PREPARED TO HAVE ONE OF THESE QUESTIONS ON YOUR EXAM 4
BE PREPARED TO HAVE ONE OF THESE QUESTIONS ON YOUR EXAM 4
1. what are ARGs and, based on this article, why are they a concern
1. **ARGs** are antimicrobial resistance genes and they are a concern because they are transferrable and can thus pass to other microorganisms leading to more antibiotic resistance in the environment.
2. what is AMR and, based on this article, why is it a concern
1. **AMR** is antibiotic resistance and they are a concern because if more bacteria are resistant to our antibiotics, we are less able to treat infections and illnesses; what was once an effective treatment can be void.
3. based on this article, why would there be a concern about leaving milk at room temperature
1. Leaving milk at room temperature is a concern because __it would enrich the ARGs;__ the milk would become a reservoir of ARGs.
4. based on this article, what does this mean for the US and low-income countries
1. According to the article, one recent study evaluated the risk factors associated with the carriage of antibiotic-resistant E. coli from people in northern Tanzania, and __direct microbial transmission in raw milk was found to be the primary predictor of the prevalence of AMR__. This demonstrates that raw milk would maintain reservoirs of ARGs and transmit antibiotic resistance.
5. based on this article, what are the different types of bacteria found and are they considered to be pathogens
1. Many different types of bacteria were found but especially *Pseudomonadaceae*; it was dominant in raw, vat-pasteurized, and ultra-pasteurized milk, while *Streptococcaceae* was more prevalent in high-temperature short-time pasteurized milk samples. Both are considered to be pathogens.
6. what types of conclusions (if any) can be drawn from this study
1. __Pasteurization matters.__ Raw milk has a distinct microbiota with a higher abundance of viable bacteria containing antimicrobial resistance genes, both of which are amplified by spontaneous fermentation at room temperature. This work indicates that raw milk consumption poses an additional risk to consumers through the transfer of antimicrobial resistance genes.
17
New cards
**Microbial Death** definition
* __Permanent__ loss of reproductive capability even under ideal conditions
* In other words... The irreversible loss of the ability to grow
* Hard to detect, microbes often reveal no conspicuous vital signs to begin with
* In other words... The irreversible loss of the ability to grow
* Hard to detect, microbes often reveal no conspicuous vital signs to begin with
18
New cards
How microbes die off – **Pattern of microbial death**
* Microorganism populations are not killed instantly but die off according to first-order kinetics - which determines that it is a linear die-off (Chick’s Law)
* Meaning… the cells in a population die at a constant rate
* Population death usually occurs exponentially
* Even VBNC cannot become viable again
* Meaning… the cells in a population die at a constant rate
* Population death usually occurs exponentially
* Even VBNC cannot become viable again
19
New cards
D value
* Decimal reduction time
* The time required to kill 90% of cells
* So, it’s a measure of an agent’s killing efficiency
* Must be sure persister cells (VBNC condition) are dead
* Once they recover they may regain the ability to reproduce and cause infection
* The time required to kill 90% of cells
* So, it’s a measure of an agent’s killing efficiency
* Must be sure persister cells (VBNC condition) are dead
* Once they recover they may regain the ability to reproduce and cause infection
20
New cards
Concept and importance of **VBNC microbes**
* Viable But Not Culturable
* Retains virulence
* A threat to public health and food safety due to their non-detectability through conventional food and water testing methods
* Retains virulence
* A threat to public health and food safety due to their non-detectability through conventional food and water testing methods
21
New cards
**Are there any factors that impact the ability of these methods to work properly?** (ex. extraneous organic materials, nature of the microbes you are trying to control, amounts of contaminants, environment)
Only when enough molecules of an essential protein or gene are damaged will the cell die. Several factors influence the speed at which lethal damage accumulates:
* Initial population size (the larger the population, the longer it takes to decrease it to a specific number)
* Population composition (are spores involved?)
* Agent concentration, or dose of radiation
* Duration of exposure
* Presence of organic material (such as blood or feces) that can inhibit disinfectant action; also called “organic load”
* Initial population size (the larger the population, the longer it takes to decrease it to a specific number)
* Population composition (are spores involved?)
* Agent concentration, or dose of radiation
* Duration of exposure
* Presence of organic material (such as blood or feces) that can inhibit disinfectant action; also called “organic load”
22
New cards
**Modes/Mechanisms of Action of Antimicrobial Agents** - you should have had an opportunity to look at these in our Disinfectants, Antiseptics, and Use Dilution Lab AND in the Norton SmartWorks Required Assignment - which ones to know for the exam will be discussed in the lecture - I didn't ask you to memorize any of these mechanisms)
Sections 13.2 and 13.3 in the book
* Moist and dry heat
* Moist heat kills better than dry heat, thanks to the ability of water to penetrate cells.
* Filtration
* For heat-sensitive media or chemical additives
* A form of sterilization
* Filtration through a filter with a pore size…
* 0.2 um → removes bacteria and bacterial endospores, yeasts, mold spores, algae, and protozoa
* 20 nm → removes viruses
* Irradiation
* Can kill pathogens in foods w.o damaging the food itself
* food is bombarded with high-energy electromagnetic radiation
* UV does not penetrate liquids or solids well; it is useful only for surface sterilization
* Gamma rays (cobalt-60), electron beams, and X-rays are more effective at irradiation
* A potent strategy for sterilizing food after harvesting
* A microorganism’s sensitivity to irradiation depends on a lot of factors
* Irradiation of food is effective in eliminating parasites and bacteria but is inadequate for eliminating viruses or prions
* Halogens – Chlorine, Iodine
* Disinfectant
* Corrodes tissues; destroy proteins
* Used for: disinfection of drinking water, pools, and hospital equipment; sanitation; wound antisepsis
* Gas highly toxic
* Phenolics
* Disinfectant
* Denatures proteins
* Standard use
* Can cause dermatitis; vapor affects the lungs
* Alcohols
* Disinfectant
* Cause dehydration; denatures proteins; dissolves membrane lipids
* Used for: cleaning of instruments; cleaning of the skin
* Dries skin; toxic if ingested
* Hydrogen Peroxide
* Disinfectant
* Hydroxyl radicals attack membrane lipids, DNA, protein
* Used for: wound cleaning; sterilization of contact lenses
* Will whiten skin
* Aldehydes
* Glutaraldehyde
* Disinfectant
* Alkylation damages protein, DNA, and RNA
* Used for: disinfection of medical equipment
* Irritates skin, mucous membranes
* Formaldehyde
* Disinfectant
* Reacts with protein, DNA, and RNA; cross-links proteins and DNA
* Used for: embalming; preservation of anatomical specimens
* Pungent odor, irritating fumes; carcinogen
* Heavy Metals
* ^^Bisphenols?? Is BPA a heavy metal? meh^^
* Disinfectant
* Disrupts membranes and proteins
* Used for: disinfection of solid surfaces
* Very toxic if swallowed
* Quaternary ammonium compounds (cationic agents)
* Disinfectant
* Disrupts membrane
* Used for: sanitation of floors, walls, blood pressure cuffs
* Toxic if ingested; irritates mucous membranes
* Moist and dry heat
* Moist heat kills better than dry heat, thanks to the ability of water to penetrate cells.
* Filtration
* For heat-sensitive media or chemical additives
* A form of sterilization
* Filtration through a filter with a pore size…
* 0.2 um → removes bacteria and bacterial endospores, yeasts, mold spores, algae, and protozoa
* 20 nm → removes viruses
* Irradiation
* Can kill pathogens in foods w.o damaging the food itself
* food is bombarded with high-energy electromagnetic radiation
* UV does not penetrate liquids or solids well; it is useful only for surface sterilization
* Gamma rays (cobalt-60), electron beams, and X-rays are more effective at irradiation
* A potent strategy for sterilizing food after harvesting
* A microorganism’s sensitivity to irradiation depends on a lot of factors
* Irradiation of food is effective in eliminating parasites and bacteria but is inadequate for eliminating viruses or prions
* Halogens – Chlorine, Iodine
* Disinfectant
* Corrodes tissues; destroy proteins
* Used for: disinfection of drinking water, pools, and hospital equipment; sanitation; wound antisepsis
* Gas highly toxic
* Phenolics
* Disinfectant
* Denatures proteins
* Standard use
* Can cause dermatitis; vapor affects the lungs
* Alcohols
* Disinfectant
* Cause dehydration; denatures proteins; dissolves membrane lipids
* Used for: cleaning of instruments; cleaning of the skin
* Dries skin; toxic if ingested
* Hydrogen Peroxide
* Disinfectant
* Hydroxyl radicals attack membrane lipids, DNA, protein
* Used for: wound cleaning; sterilization of contact lenses
* Will whiten skin
* Aldehydes
* Glutaraldehyde
* Disinfectant
* Alkylation damages protein, DNA, and RNA
* Used for: disinfection of medical equipment
* Irritates skin, mucous membranes
* Formaldehyde
* Disinfectant
* Reacts with protein, DNA, and RNA; cross-links proteins and DNA
* Used for: embalming; preservation of anatomical specimens
* Pungent odor, irritating fumes; carcinogen
* Heavy Metals
* ^^Bisphenols?? Is BPA a heavy metal? meh^^
* Disinfectant
* Disrupts membranes and proteins
* Used for: disinfection of solid surfaces
* Very toxic if swallowed
* Quaternary ammonium compounds (cationic agents)
* Disinfectant
* Disrupts membrane
* Used for: sanitation of floors, walls, blood pressure cuffs
* Toxic if ingested; irritates mucous membranes
23
New cards
Therapeutic Index
The ratio of the toxic dose to therapeutic dose
* Toxic dose: maximum dose tolerated by the patient
* Therapeutic dose: minimum dose per kg of body weight that stops growth
* Toxic dose: maximum dose tolerated by the patient
* Therapeutic dose: minimum dose per kg of body weight that stops growth
24
New cards
Selective toxicity
Antibiotics kill or inhibit bacteria w/o damaging the eukaryotic organisms
25
New cards
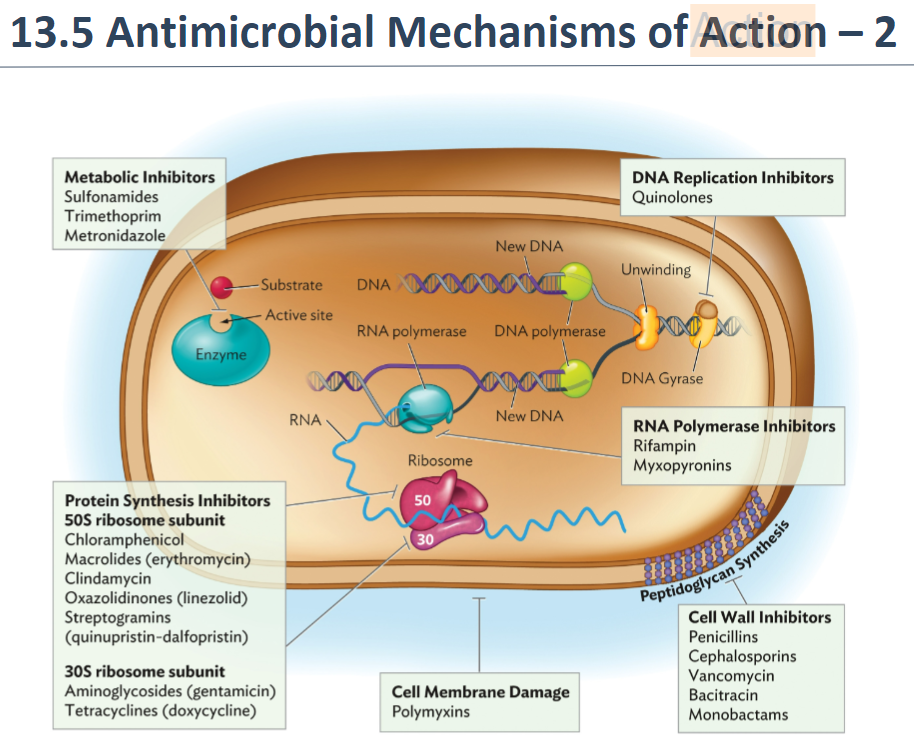
^^Modes/Mechanisms of Action of Chemotherapeutic Agents/Antibiotics (5) and 1 example of each^^
(photo)
26
New cards
Antibiotic Resistance Mechanisms - **describe** 1 (needs to be at least a few sentences) (How the bacterium is resistant to the antibiotic)
**Ribosome protection (or rescue):** Gram-positive organisms can produce proteins (for example, MsrE or TetO) that bind to ribosomes and dislodge antibiotics bound near the peptidyltransferase site.
27
New cards
Several of the important essay questions are going to be *related* to:
* Indicator organisms - what they are, why they are important, what makes an ideal one, examples of those currently used, important advantages and disadvantages
* Foodborne illnesses - what is the difference between FB Infection versus FB Intoxication, why would it be important to know, what are examples of each
* The diversity found in bacteria -what examples of bacteria or groups of bacteria represent the diverse world of bacteria
* Foodborne illnesses - what is the difference between FB Infection versus FB Intoxication, why would it be important to know, what are examples of each
* The diversity found in bacteria -what examples of bacteria or groups of bacteria represent the diverse world of bacteria