Esophageal Disorders and Neoplasms
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
30 Terms
Achalasia
The loss of peristalsis in the distal 2/3 of the esophagus and impaired relaxation of the LES leading to unabated constriction of the esophagus
Worsening dysphagia (solids then liquids) the progresses over months to years, patients may adopt techniques such as stretching the neck, tiny bites, and liquids to wash down solids
Hallmarks of Achalasia
Endoscopy (retained food, difficulty passing the scope), Esophageal manometry (definitive diagnostic), CXR (fluid/food in esophagus), Barium swallow study (Gold standard - bird’s beak)
45 y/o male presents to the clinic for dysphagia that has worsened over the past few months. He notes that he tends to feel “full in the chest” after eating, and has been vomiting several hours after the meal. He states that he has loss 30 lbs in the last few months. Which diagnostics do you want?
pneumatic balloon dilation (33-50% will require another one), surgical myotomy (high risk, high reward)
45 y/o male presents to the clinic for dysphagia that has worsened over the past few months. He notes that he tends to feel “full in the chest” after eating, and has been vomiting several hours after the meal. He states that he has loss 30 lbs in the last few months. On a barium swallow study you notes a bird’s beak tapering and on esophageal manometry notes the complete absence of peristalsis. Let’s say he’s a low risk surgical patient, what is your treatment plan?

Botox into the esophageal muscles (relapses in 2-3 months)
45 y/o male presents to the clinic for dysphagia that has worsened over the past few months. He notes that he tends to feel “full in the chest” after eating, and has been vomiting several hours after the meal. He states that he has loss 30 lbs in the last few months. On a barium swallow study you notes a bird’s beak tapering and on esophageal manometry notes the complete absence of peristalsis. Let’s say he’s a high risk surgical patient, what is your treatment plan?

Esophageal strictures
A narrowing of the esophagus with scar tissue, most commonly as a result of esophageal injury
GERD (most common), ingestion related caustic injuries, radiation therapy, previous esophageal surgeries. eosinophilic esophagitis (chronic inflammation), cancer
Risk factors of Strictures
Barium Esophagram (do 1st if proximal or complicated), Upper Endoscopy (1st draft pick - inspect and biopsy)
67 y/o patient presents to the clinic for his 1st check up in years. PMX is positive for GERD, which he states that he doesn’t have any more. He does report that recently he has had trouble eating solid foods, but liquids are good. What diagnostics do you want?
Mechanical/pneumatic dilation, PPI post-dilation, If refractory try steroid injections, temporary plastic stent placement (last resort)
67 y/o patient presents to the clinic for his 1st check up in years. PMX is positive for GERD, which he states that he doesn’t have any more. He does report that recently he has had trouble eating solid foods, but liquids are good. Barium swallow study and endoscopy diagnose a stricture. What is your treatment plan?

GERD, Barretts, esophageal tumors, Chagas, esophageal spasm, nutcracker esophagus, stroke, scleroderma, zenker diverticulum
DDX for achalasia and strictures
Mallory-Weiss tear (MWT)
A partial thickness esophageal laceration/tear that accounts for 5% of upper GI bleeds and is more common in males
Retching/vomiting (most common), heavy lifting, iatrogenic injury
Causes of a MWT
CBC (anemia), CMP, Coags (if she’s on any blood thinners), Endoscopy (GOLD STANDARD)
Patient presents to the ER for N/V. Patient states that she was working out and started to “puke out all of her blood.” She states that the blood was bright red and that her back hurts. On a physical exam you note mid-epigastric tenderness. Vitals are stable. What diagnostics do you want?
Spontaneous resolution (most cases), Endoscopic intervention (electrocautery, epi injections, band ligation, clips), hospitalize and observe, PPI/H2 for 1-2 weeks, Antiemetics (ondaestron, promethazine)
Patient presents to the ER for N/V. Patient states that she was working out and started to “puke out all of her blood.” She states that the blood was bright red and that her back hurts. On a physical exam you note mid-epigastric tenderness. Vitals are stable. Endoscopy shows a mucosal tear. What is your treatment plan?
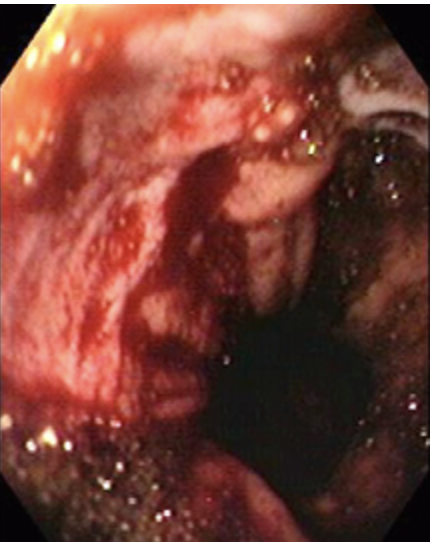
within 48 hours
When is rebleeding of MWTs more likely to occur?
Bleeding esophageal varices, boerhaave syndrome (full thickness tear), esophagitis, esophageal mechanical injury, capillary rupture
DDX for MWTs
Zenker Diverticulum
A sac-like outpouching of the mucosa and submucosa through Killian's triangle at the pharyngeal junction more common in males
chronic increased pressure on an already weak area → increased resistance of UES or abnormal esophageal motility
What causes a Zenker Diverticulum?
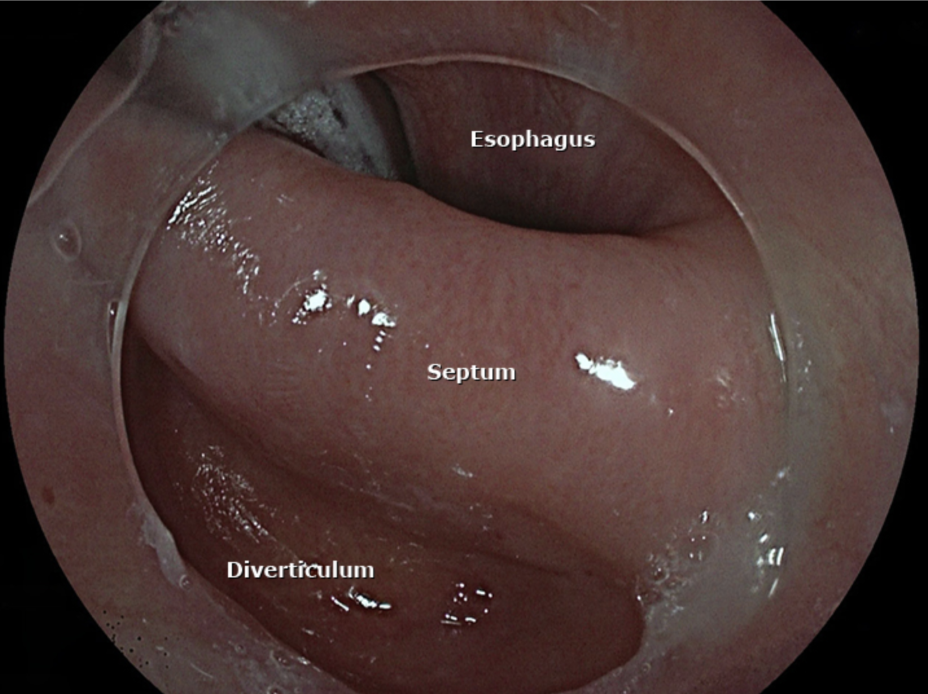
Barium Swallow study (1st line - we aint trying to perforate), Upper endoscopy (definitive diagnosis and treatment)
58 y/o male presents to the the ER for dysphagia that “feels like choking.” He also notes that he often throws up at night and has trouble sleeping due to a choking sensation. On a physical exam you note halitosis and a palpable mass in the neck. What diagnostics do you want?
Flexible endoscopic myotomy and diverticulectomy (5% will develop a clinically insignificant diverticulum post-surgery)
58 y/o male presents to the the ER for dysphagia that “feels like choking.” He also notes that he often throws up at night and has trouble sleeping due to a choking sensation. On a physical exam you note halitosis and a palpable mass in the neck. See barium swallow. What is your treatment of choice?

GERD, esophageal stricture, Achalasia, Neoplasms, scelroderma
DDX for zenker diverticulum
Squamous cell carcinoma (upper 2/3), adenocarcinoma (lower 1/3)
What are the 2 types of Esophageal neoplasms?
50-70 y/o male
Typical esophageal neoplasm patient
Chronic EtOH, tobacco, achalasia, strictures, other head and neck cancers
Risk factors for squamous cell carcinomas
Sequelae of chronic gastric reflux and Barrett Esophagus, obesity
Risk factors for adenocarcinomas
Fecal occult blood (positive), Barium Swallow study (complex lesions), Upper endoscopy with biopsy (definitive)
69 y/o male patient presents to the clinic for dysphagia that has been getting worse over the past few months. He states that he’s lost weight because he hasn’t been able to eat any solid food without pain. He also notes a persistent cough and back pain. On a physical exam you note that the patient has a hoarse voice and a neck mass. What diagnostics do you want?
Radiation + chemo with/without surgery
Gameplan for non-metastatic, localized tumors
Localized (30%), Regional (15%), Metastatic (under 5%)
5-year survival rates for esophageal cancers
GERD, esophagitis, esophageal stricture, zenker diverticulum, achalasia, scleroderma
DDX for esophageal neoplasms
Palliative care
For patients with distant metastasis → who we calling?