large intestine, constipation, diarrhoea and lactose intolerance
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
why does gastrointestinal motility occur?
usually involuntary
• mostly due to the activity of smooth muscle (circular, longitudinal layers and the muscularis mucosa)
• BUT skeletal muscle is important in the mouth, pharynx, upper oesophagus and external anal sphincter
- food travels to digestive system and intestines start to absorb
what are the different types of smooth muscle involved in GI motility and what are each of their roles?
- Longitudinal muscle contraction: lumen becomes shorter and fatter - push the food to the intestine
- Circular muscle contraction: lumen becomes narrower and longer - squeeze food (digestion)
- Muscularis mucosae contraction: change in absorptive and secretory area of mucosa - enzyme release from glands
What is the enteric nervous system?
large network of neurons surrounding the digestive organs
- cell bodies of the neurones are located in ganglia, largely within the myenteric and submucous plexus. the interganglionic fibre tracts connect the two plexus
- these neurones regulate the activity of smooth muscles in intestinal tissue
- forms a reflex circuit that can operate independently of the rest of the NS, but is strongly modulated by hormones and extrinsic nerve input - also if under stress, influenced by the CNS
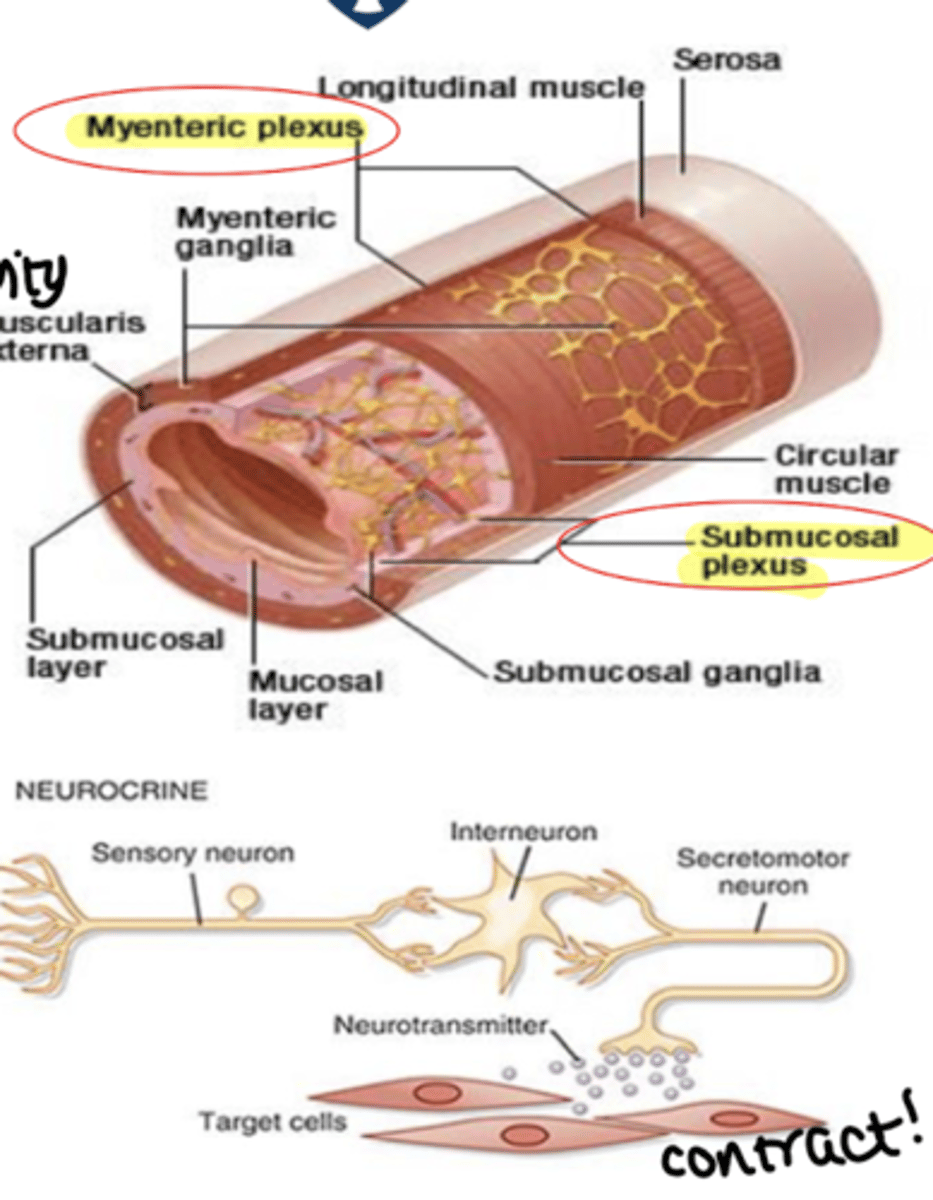
what is the enteric nervous system compromised of?
- Sensory neurons:(mechanoreceptors (by chewing food) , chemoreceptors (detecting sweet/salty), thermoreceptors)
- Interneurons: co-ordinating reflexes and motor programs
- Effector neurons: excitatory and inhibitory motor neurones
a trigger from the NS is required for contraction
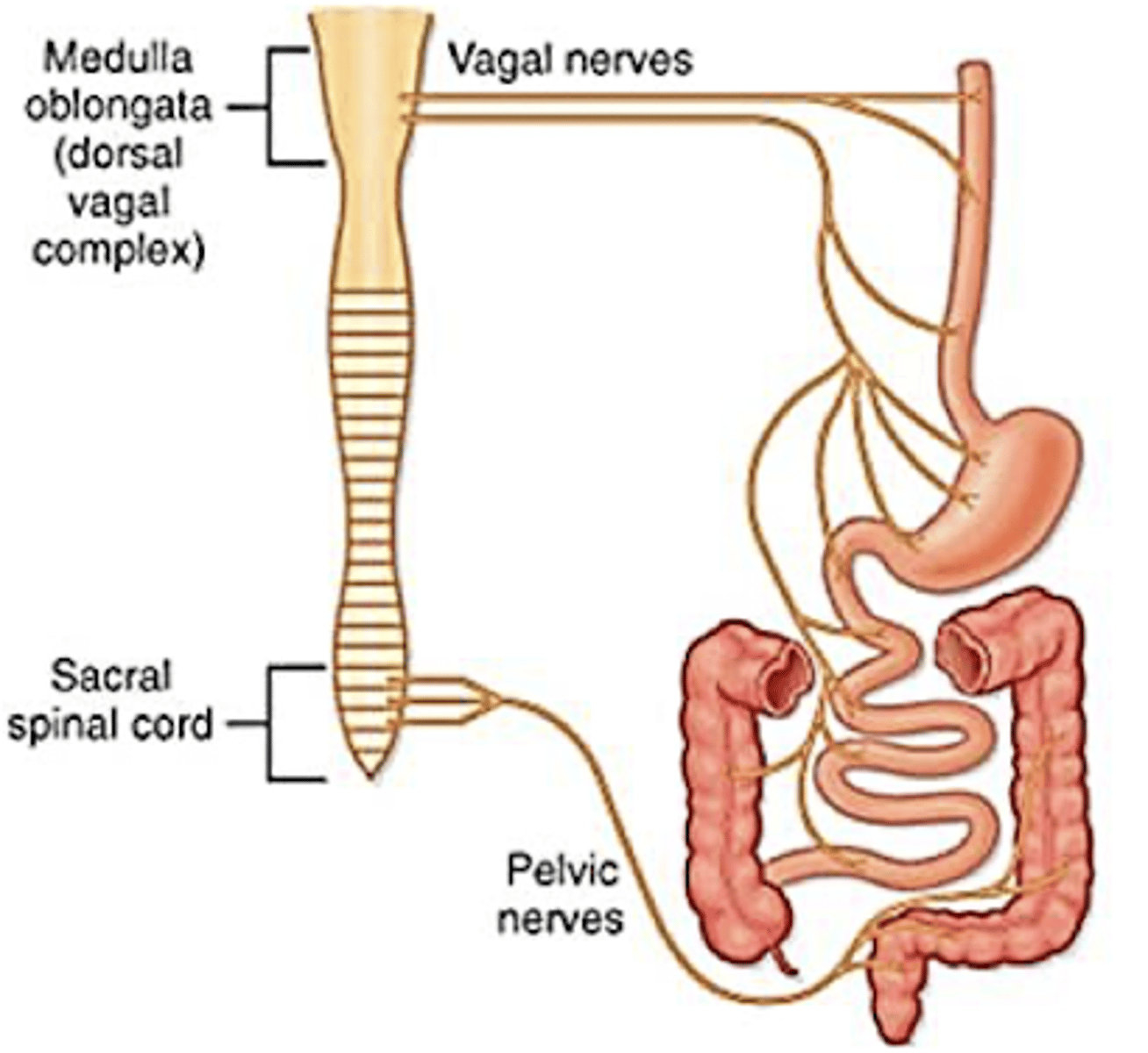
what is the dominant autonomic innervation of the GI?
parasympathetic - rest and digest
what is the parasympathetic autonomic innervation of the GI?
- neurones released from spinal cord
- from ganglia close to target organ
- Preganglionic fibres (releasing ACh) synapse with postganglionic neurones within the enteric nervous system (ENS)
Excitatory influences (MAINLY)
• Increased gastric, pancreatic and small intestinal secretion, blood flow and smooth muscle contraction
Inhibitory influences:
• Relaxation of some sphincters, receptive relaxation of stomach - stomach gets wider to acccomadate food
REST AND DIGEST
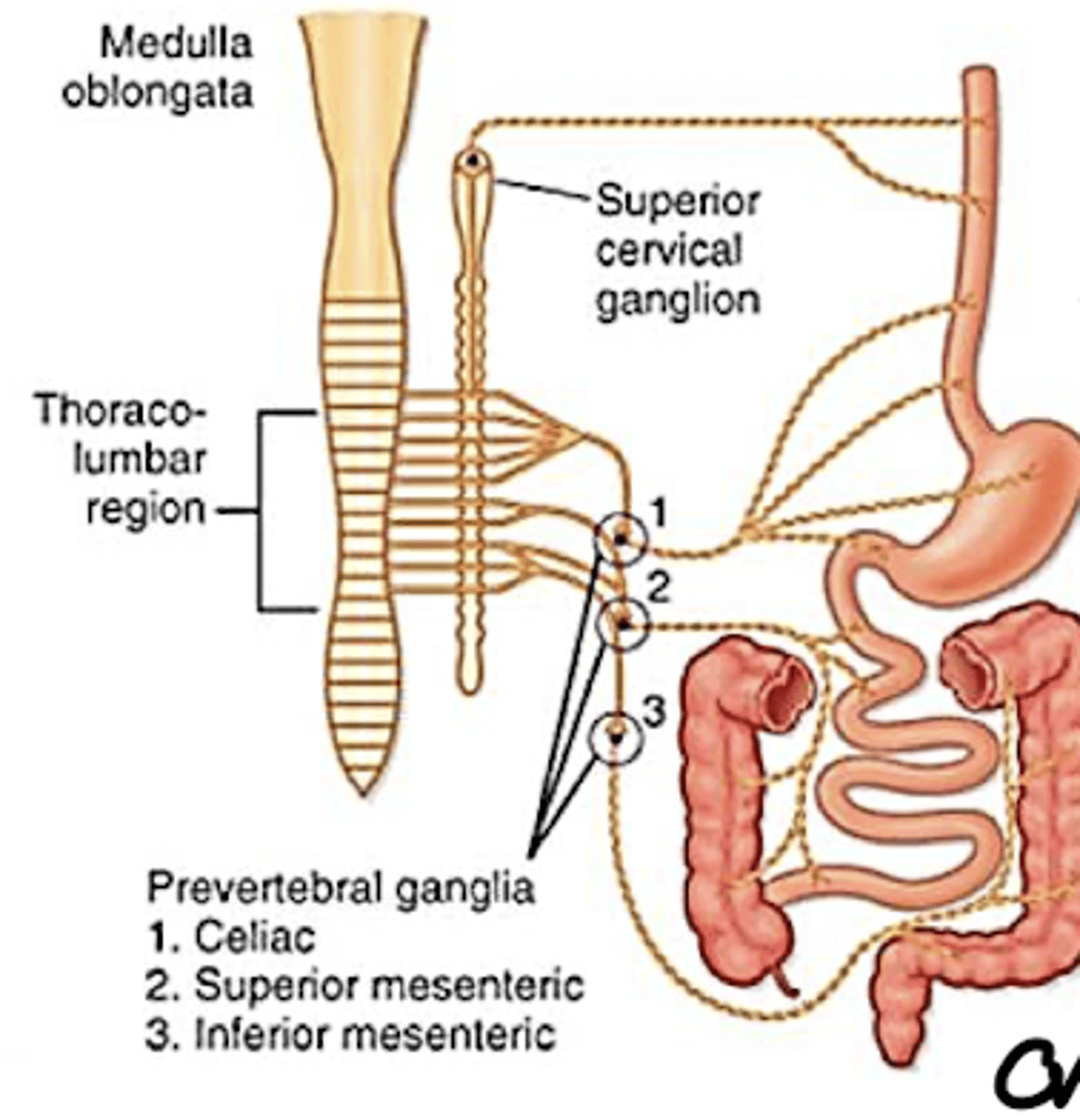
what is the sympathetic autonomic innervation of the GI?
only occurs in some circumstances - when in danger/stress body does not want to focus on digestion
• Preganglionic fibres (releasing ACh) synapse in the prevertebral ganglia. Postganglionic fibres (releasing NA) innervate mainly enteric neurones
• Functionally less important than the parasympathetic
division
• Inhibitory influences
• Decreased motility, secretion and blood flow
adrenaline inhibits digestion
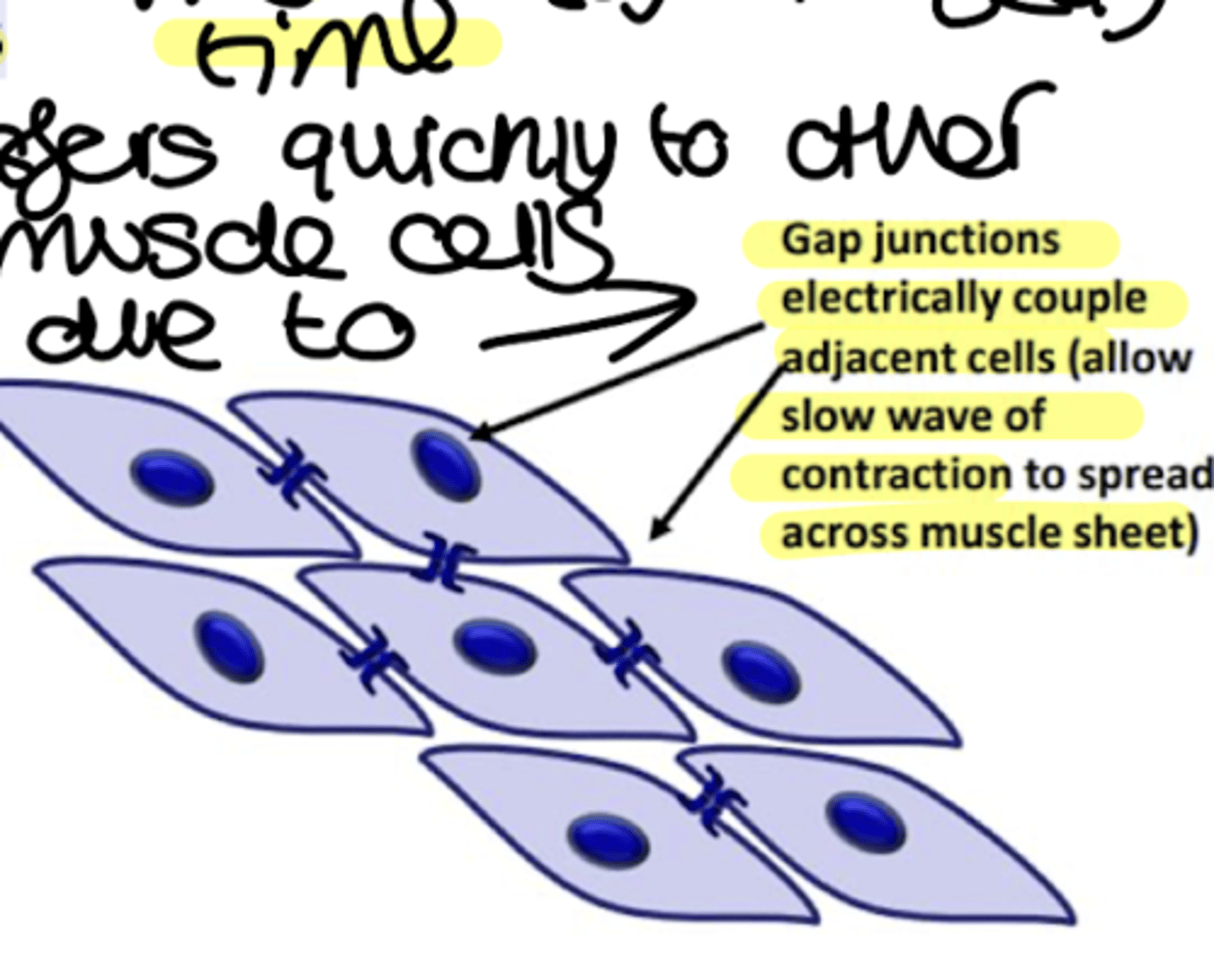
what is the spontaneous activity of the GI smooth muscle?
• Adjacent smooth muscle cells are coupled by gap junctions – allow spread of electrical currents from cell to cell forming a functional syncytium; hundreds of cells are depolarized and contract at the same time
• Spontaneous activity is modulated by:
a. Intrinsic (enteric) and extrinsic (autonomic) nervous system
b. Hormones
Spontaneous electrical activity occurs as slow waves - rhythmic patterns of membrane depolarization and repolarization that spread from cell to cell via gap junctions
what is the slow wave electrical activity of smooth muscles in GI?
• Slow waves are driven by the interstitial cells of Cajal (ICCs) which are pacemaker cells
• Contraction only occurs if the slow wave amplitude is sufficient to trigger action potentials (slow wave mediated mainly by triggering Ca2+ channel to open
- changes membrane potential of cell and may cause action potential (needed for muscle to contract)
-ICCs form gap junctions with each other and smooth muscle cells
- ICCs are located between the longitudinal and circular muscle layers and in the submucosa
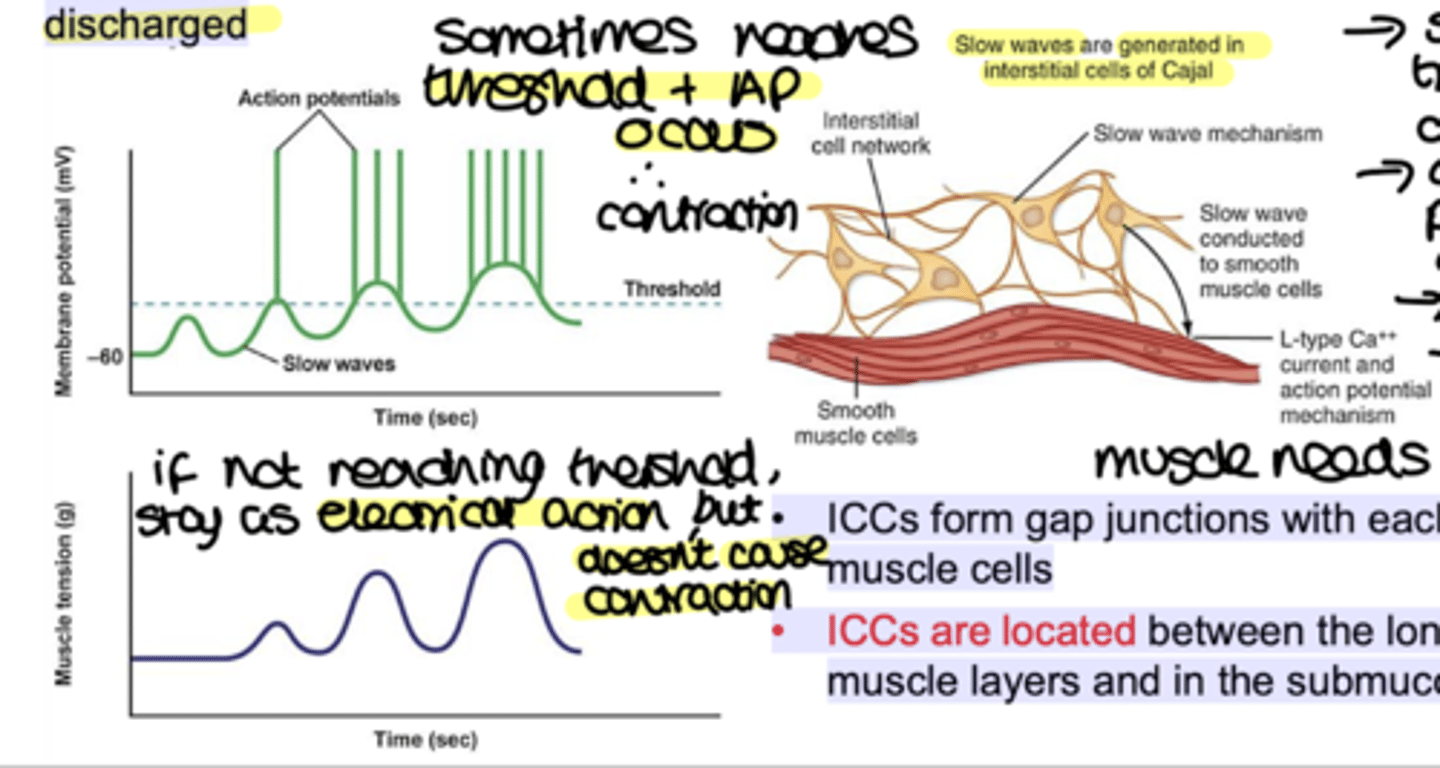
in GI, what is the basic electrical rhythm?
Slow waves determine the basic electrical rhythm (BER) - not all slow waves trigger contraction
Whether slow wave amplitude reaches threshold depends upon (for example):
• Neuronal stimuli
• Hormonal stimuli
• Mechanical stimuli
BER frequency varies along GI tract
• Stomach - 3 slow waves per minute - low, not all generate contraction
• Small intestine- approx. 1-12 waves per minute in the duodenum; approx. 8 waves per minute in the terminal ileum- tends to drive luminal contents in the aboral direction
• Large intestine - favours retention of luminal contents facilitating absorption of water and electrolytes - retains food and solidifies faeces
what are the major motility patterns in the GI tract?
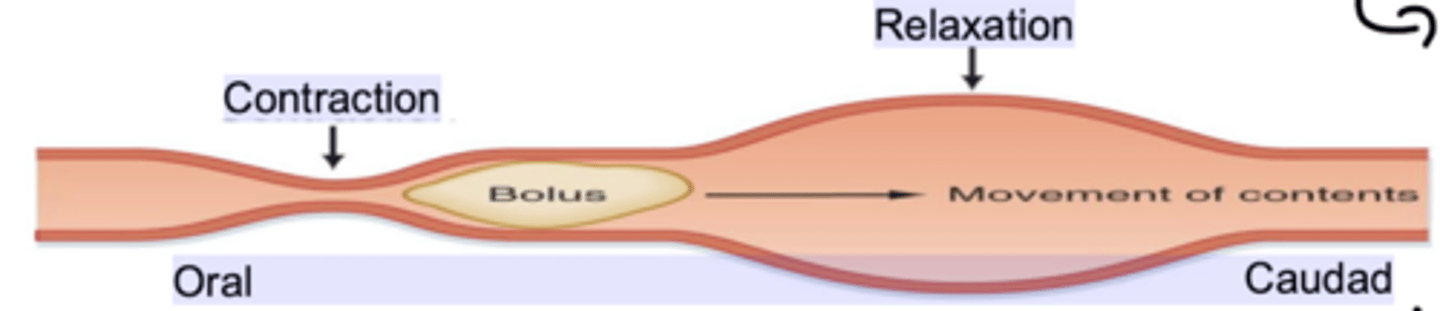
1. Peristalsis - a series of wave-like muscle contractions that move food through the digestive tract - triggered by distension of the gut wall. It involves contraction of longitudinal muscle layers, making intestine shorter and wider and pushing food in direction
2. Tonic contraction- sustained contractions found in the sphincters of the G.I. tract - allowing digestion to occur
3. Segmentation - rhythmic contractions of the circular muscle layer that mix and divide luminal contents - narrow the lumen to increase enzyme contact
what is the main absorption of water process in the GI tract?
passive driven by transport of solutes (mainly Na+) from lumen of intestines to blood stream. movement of water BY OSMOSIS ➢ Is largely driven by absorption of Na+
➢ Intestinal fluid movement is always coupled to solute movement
➢ Water may move via transcellular, or paracellular, routes
➢ Absorption of Na+ provides a (local) osmotic force for the absorption of water
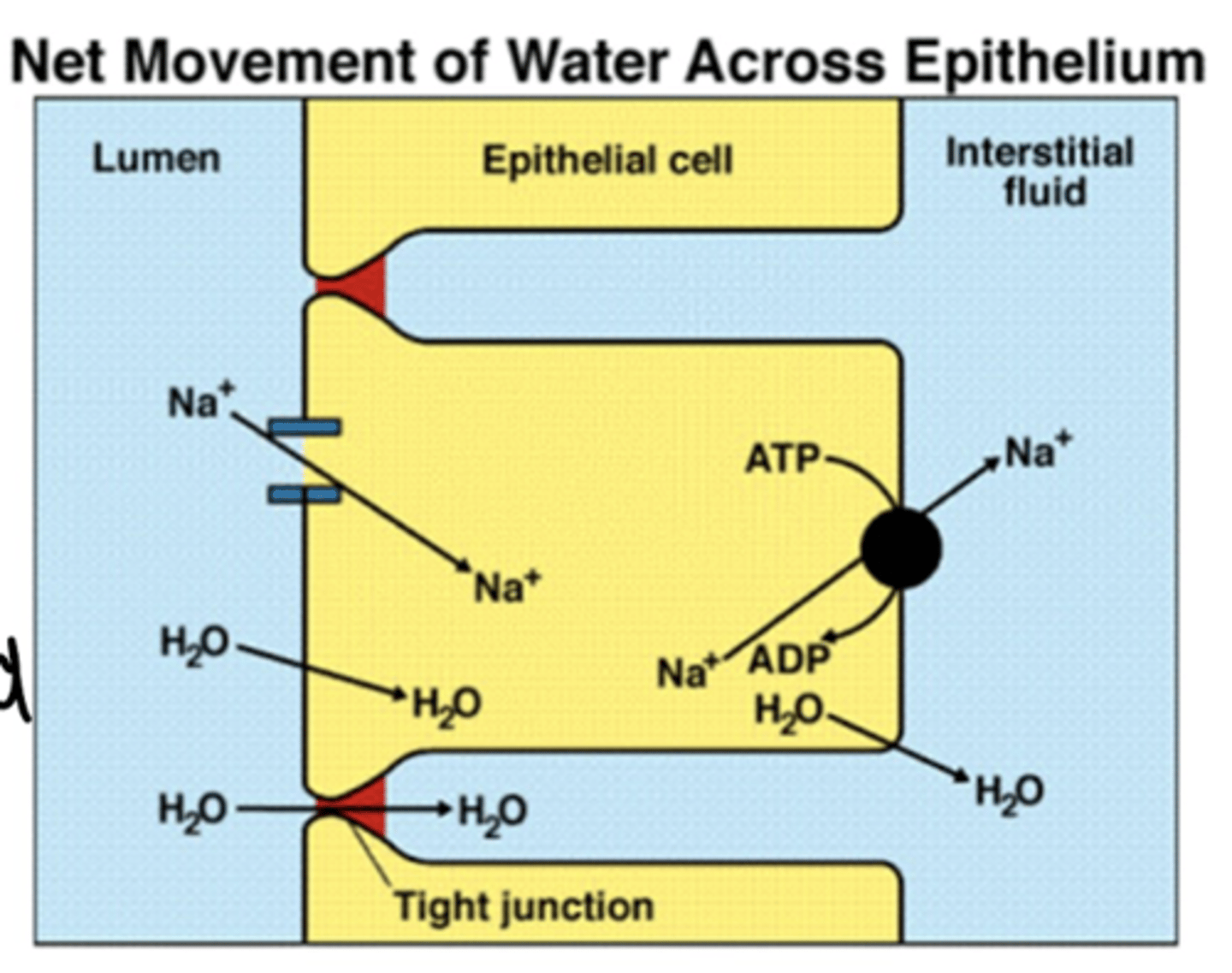
what is electrogenic water absorption?
when one group of Na+ moves from lumen to interstitial fluid, it becomes more positive - therefore charge has been changed
what is electroneutral water absorption?
when one group of Na+ is absorbed is compensated by H+ out, so charge is unchanged
what are the principle mechanisms/features of sodium/water absorption in the GI tract? where do they occur?
- Na+/glucose co transport: electrogenic, in SI
- Na+/AA co transport: electrogenic in SI
- Na+/H+ exchange: electroneutral powered by Bicarb, in duodenum and jejunum
- Parallel Na+/H+ and Cl-/HCO3- exchange: cAMP/cGMP and Ca dependnnt - in ileum and colon
- epithelial Na+ channels (ENaC): regulated by aldosterone, in distal colon
how and when is Cl- passively absorbed in the GI tract?
- when Na+ leaves the lumen it becomes too negative
- negativity of lumen repulses Cl
- therefore enters epithelial cells
this occurs:
• In the small intestine force provided by lumen negative potential due to electrogenic transport of Na+ (Na+/glucose and Na+/amino acid)
• In the large intestine force provided by lumen negative potential due to electrogenic transport of Na+ through ENaC
in Cl-/HCO3- exchange, and parallel Na+/H+ and Cl-/HCO3- exchange energy is required, and special channels are present for Cl-
what is the mechanism of Cl- secretion?
- occurs at basal (continuous) rate from crypt cells
- Low intracellular Na+ drives inward movement of Na+, K+ and 2Cl, all via NKCC1
- K+ recycles via K+ channels, but intracellular concentration of Cl- increases providing a gradient for Cl- to exit cell via CFTR (cystic fibrosis transmembrane regulator - which secrete Cl- from epi cell back to lumen) on the apical membrane
➢ CFTR channels are normally closed
➢ Lumen negative potential (negative Cl-) develops voltage-dependent secretion of Na+ through paracellular pathway, water follows this and causes diarrhoea
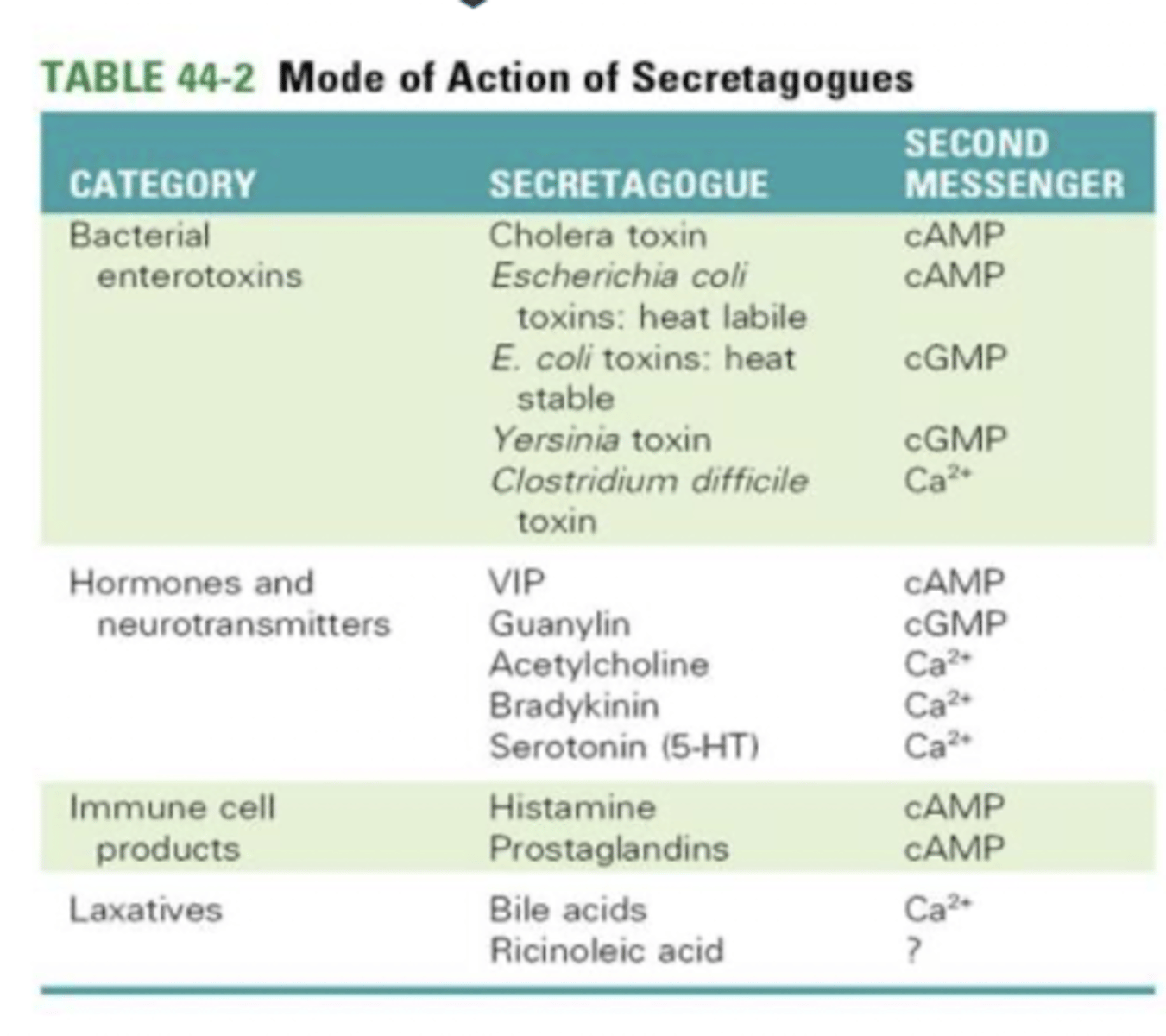
what is the role of CFTR in diarrhoea?
➢ Normally, little secretion of Cl- occurs because apical CFTR is either closed, or not present
➢ Secretion occurs when CFTR is activated by:
• bacterial enterotoxins
• hormones and neurotransmitters
• immune cells products
• some laxatives
all of these effect cAMP, cGMP and Ca2+ levels, which cause insertion of CFTR levels
- when CFTR opens: Cl- moves to lumen, Na+ and H2O attracted from intestinal fluid and diarrhoea occurs
what are the 4 main causes of diarrhoea?
1. Excessive secretion - secretory diarrhoea (eg E Coli)
2. Impaired absorption of NaCl - by:
- congenital defects in channels: less absorption of Cl-, increasing Na+ and H2O output
- infection or inflammation
- destruction of intestinal absorptive epithelium
3. Non absorbable or poorly absorbable solutes in lumen - ie lactose intolerance, lactase deficiency therefore water attracted to lactose and water stays in intestine as not absorbed
.4. Hypermotility - IBS, not enough time for absorption
how does E.Coli cause diarrhoea?
Cholera provides an additional classic example
• Cholera toxin enters enterocyte enzymatically inhibits GTPase activity of the Gsα subunit
- Gsa is couples with adenylate cyclase which activates cAMP
- cAMP stimulates CFTR
- causing hypersecretion of Cl-, with Na+ and water following causing diarrhoea
what is the consequences of diarrhoea?
• Can result in dehydration (Na+ and H2O loss) - loses water and electrolytes
• Metabolic acidosis (HCO3- loss) - usually absorbed, but here it increases acidity of lungs
• Hypokalaemia (K+ loss)
• May be fatal if severe (e.g. cholera)
what is the treatment of severe acute diarrhoea?
• Maintenance of fluid and electrolyte balance (first priority) - always hydrate and use ORT
treating the cause:
• Use of anti-infective agents (Abx - if appropriate)
• Use of anti-motility agents
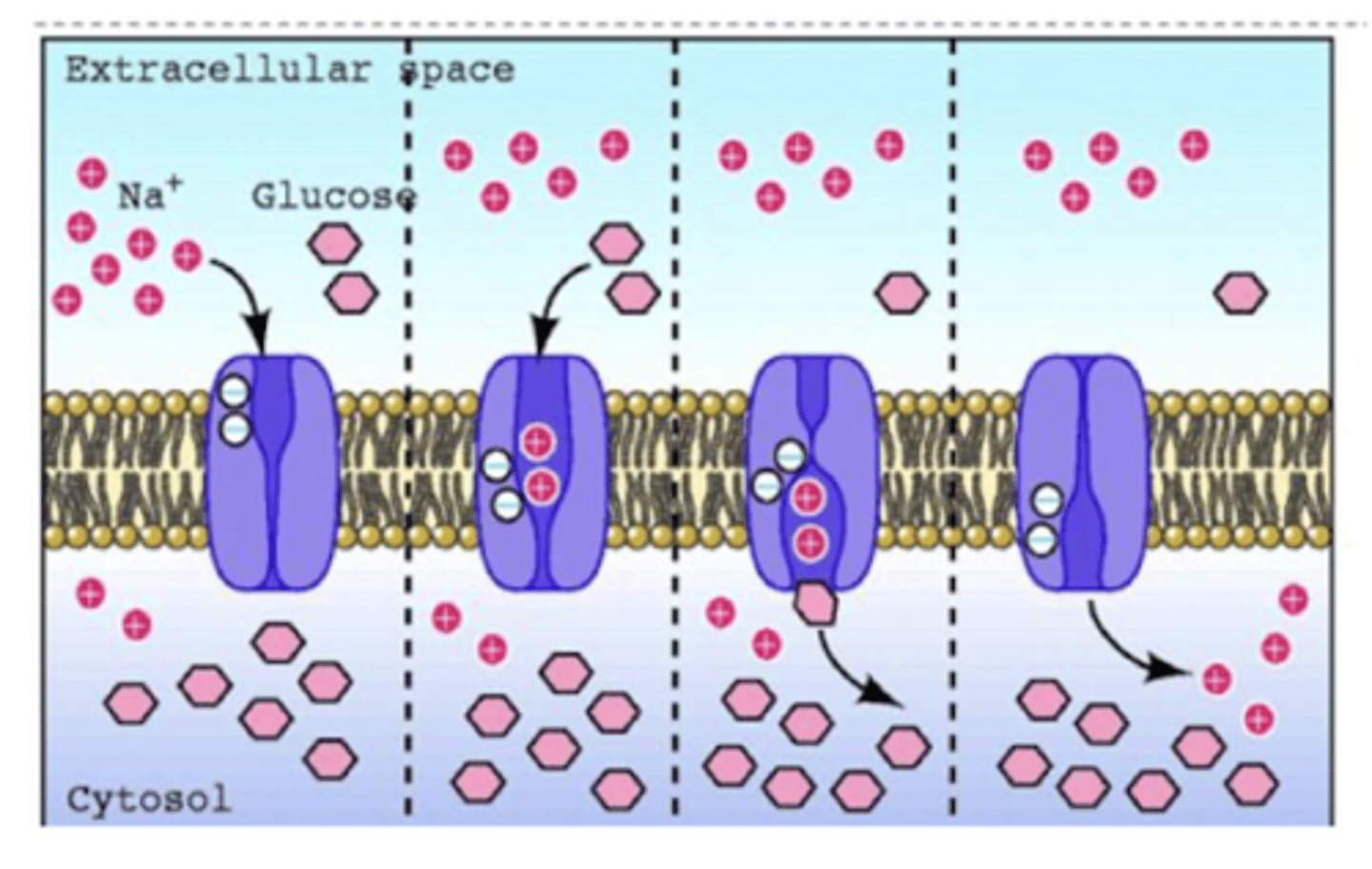
what is the mechanism of rehydration therapy?
- exploiting Na+ and gluycose channels in order for Pt to absorb Na+ and water
1. 2Na+ bind
2. affinity for glucose increases, so it binds
3. Na+ and glucose translocated from extracellular (lumen) to intracellular (interstitial fluid)
4. 2Na+ dissociate, affinity for glucose falls
5. glucose dissociates
6. cycle repeated
JUST GIVING WATER - IT WILL BE EXCRETED
what are antimotility drugs used for? how do they work?
- used for treatment of diarrheoa
- opiate drugs! as they bind to new opiate receptors and cause hyperpolarisation, which inhibits movement of intestine
actions of the alimemtary tract include:
• inhibition of enteric neurones (hyperpolarization via activation of u-opioid receptors)
• decreased peristalsis, increased segmentation (i.e. constipating)
• increased fluid absorption
• constriction of pyloric and anal sphincters
what are the anti motility agents used in treatment of diarrhoea?
➢ The major opiates used in diarrhoea are:
• Codeine - treats hypermotility but has CNS effects
• Diphenoxylate - low CNS penetration, blocks the release of acetylcholine in the synaptic cleft
• Loperamide–opiate:
• First choice for traveller’s diarrhoea
• Relatively selective for the G.I. tract.
• It reduces peristalsis, decrease the passage of faeces
• Atropine - blocks Ach receptors, decreasing intenstinal movement, causes side effects on eyes and heart
what is lactose intolerance?
Relatively common digestive problem resulting from the inability to adequately
digest lactose: caused by lactase insufficiency
- Human populations exhibit (worldwide) a variable degree of lactase persistence (LP)
- Partially due to polymorphisms in the MCM6 gene that regulates expression of the lactase gene
what can lactose intolerance result from?
• Primary lactase deficiency- due to lack of the lactase persistence (LP) allele - most common cause world wide
• Secondary lactase deficiency - caused by damage to/ infection of/ the proximal small intestine - inflammation causes damage
• Congenital lactase deficiency - rare autosomal recessive disease - no ability to digest lactose from birth
what is the consequences of lactase insufficiency?
• Hypolactasia causes no disturbance unless lactose-containing food is consumed and activity of remaining enzyme is overwhelmed
• If lactose is delivered to the colon from the ileum colonic microflora produce:
• Short-chain fatty acids (which can be absorbed)
• Hydrogen (H2- which can be detected in the breath of lactase deficient individuals following a lactose challenge)
• Carbon dioxide
• Methane
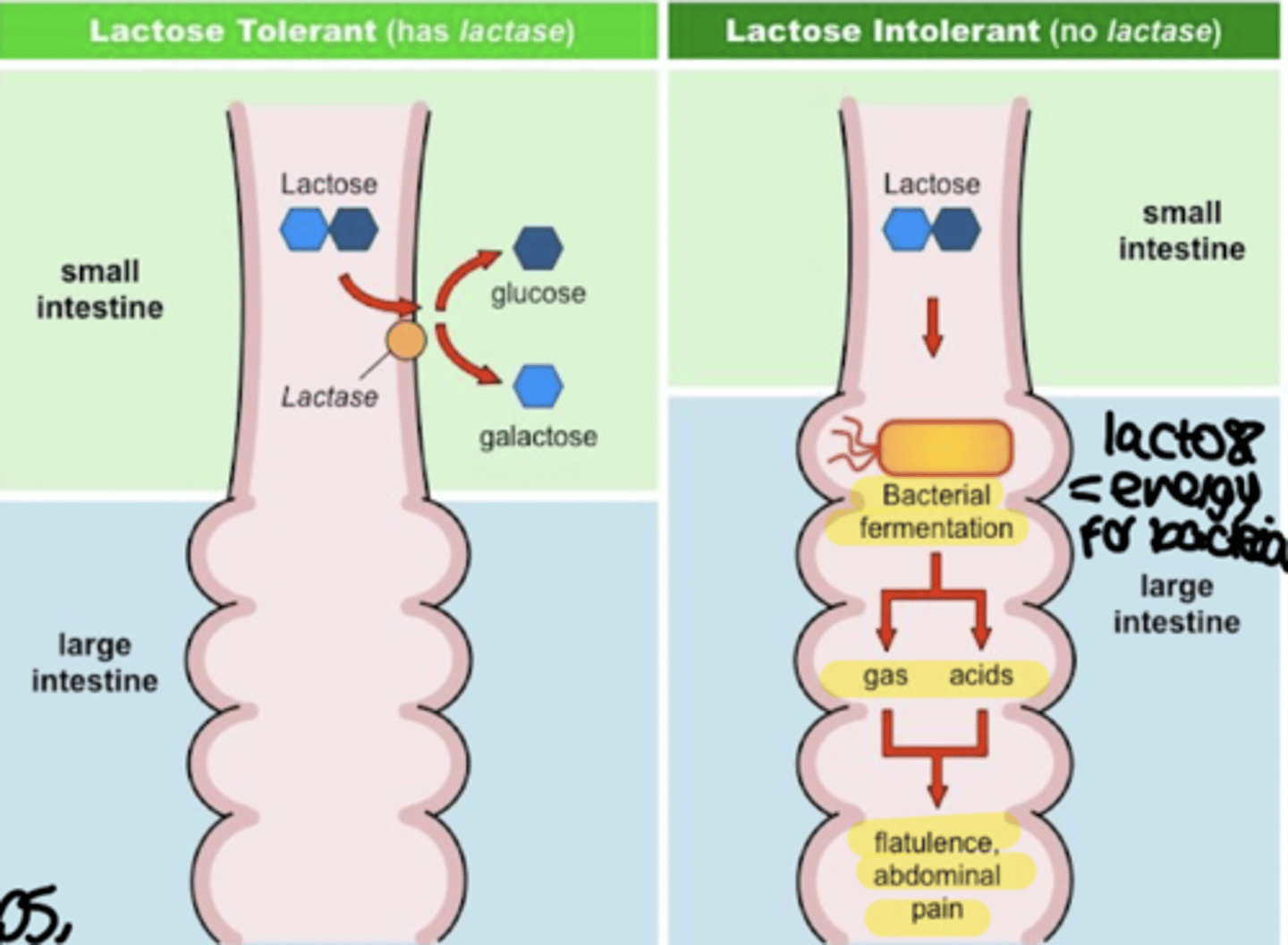
what are the symptoms of lactose intolerance?
Symptoms:
• Bloating
• Abdominal pain
• Diarrhoea due to H20 from hydroxyl groups
how is lactose intolerance diagnosed?
ased on diet observation:
• Association of symptoms with lactose consumption
• Hydrogen breath test - to know if lactose is fermented by LT bacteria
• Lactose/milk tolerance test - lactose should degrade to glucose and galactose, so blood sample should show increase glucose, but with lactose intolerance there will not be a glucose increase
what is the treatment of lactose intolerance?
Treatment:
• Reduction or elimination of consumption of milk products
• Use of milk products treated with lactase
• Use of milk lactose-free
what is constipation?
difficult/infrequent defecation
what are the causes of constipation?
• Neurogenic disorders of the large intestine leading to reduced persistalsis (E.g. Megacolon, hypothyroidism, IBD with constipation, cancer etc.)
• Abdominal muscle weakness - non exercisers
• Diet poor of fibres
• Sedentary life style
• Constant suppression of the urge to empty
• Antidepressant drugs -anticholinergics - decrease peristalsis
• Opiates
• Aging - as decreases muscle contraction and movement
how is constipation treated non pharmacologically?
- More water and less alcohol should be consumed
• Some wheat bran can be added to the diet - to create a bulky hybrid mass to increase bowel movement
• Increase your activity- exercise
• Improve your toilet routine - Keep to regular time and give yourself plenty of time to use the toilet
• Don't delay
• Feet can be rested on low stool while going to toilet
how is constipation treated pharmacologically?
• Bulk laxatives: e.g. methylcellulose -Polysaccharide polymers not digestible
• Osmotic laxatives (e.g magnesium hydroxide, lactulose): -Poorly absorbed solutes
• Faecal softeners (e.g. arachis oil, docusate sodium) -Enema
• Stimulant laxatives (e.g. senna, dantron) -Drugs that directly increase peristalsis, by increasing cAMP
- Drugs that increase G.I. motility without purgation - Antiemetics (e.g. domperidone, metoclopramide) -Increase gastrointestinal motility and gastric emptying