PDII E3: cardio examination
1/162
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
What occupies most of the anterior cardiac surface?
RV
What lies behind just left of the sternum and join at the sternal angle?
RV and pulmonary artery
Where is the inferior border of the RV?
below the junction of the sternum and xyphoid process
What sits behind the RV?
LV
what creates the apex and produces the apical impulse?
tapered inferior tip of LV
where is PMI normally found?
left 5th ICS just medial to MCL
(approx 1-2.5 cm)
What lies above the heart?
great vessels- PA, SVC, aorta
what are pathologic, diastolic sounds that are correlated w/ HF and AMI?
S3 & S4
what sound is an abrupt deceleration of inflow across the mitral valve?
S3
what sound is an increased LV stiffness which decreases compliance?
S4
What position should the patient be in for the cardiac examination?
supine w/ head elevated 30-45 degrees
What area?
2nd ICS, R sternal border
aortic
What area?
2nd ICS, L sternal border
Pulmonic
What area?
3rd ICS, L sternal border
Erb’s point
What area?
4th ICS, L sternal border
Tricuspid
What area?
5th ICS, L midclavicular line
Mitral
What part of the stethoscope are you using to auscultate the mitral area in the left lateral decubitus position?
bell
How do you listen for the physiologic split of S2?
2nd and 3rd L ICS, ask pt to breath quietly and slightly more deeply than normal
How do you listen for murmur of aortic regurgitation?
Have pt sitting, lean forward, exhale completely and hold while auscultating over left sternal border and apex w/ diaphragm
When do you use the bell of the stethoscope?
low pitched sounds → mid diastolic murmur of MS, S3 in HF
when do you use the diaphragm of the stethoscope?
high pitched sounds → ejection, mid systolic clicks and early diastolic murmur of AR
what brings the apex of the heart closer to the chest wall and accentuates S2, S4, and mitral murmurs?
left lateral decubitus position
Sitting, leaning forward and full exhalation accentuates _____
aortic murmurs
What rash has wavy margins and truncal distribution and is assoc w/ acute rheumatic fever?
erythema marginatum
what are Aschoff bodies?
present over bony prominences of elbow in patients w/ chronic rheumatic heart dz from previous rheumatic fever, gout, syphilis, or RA

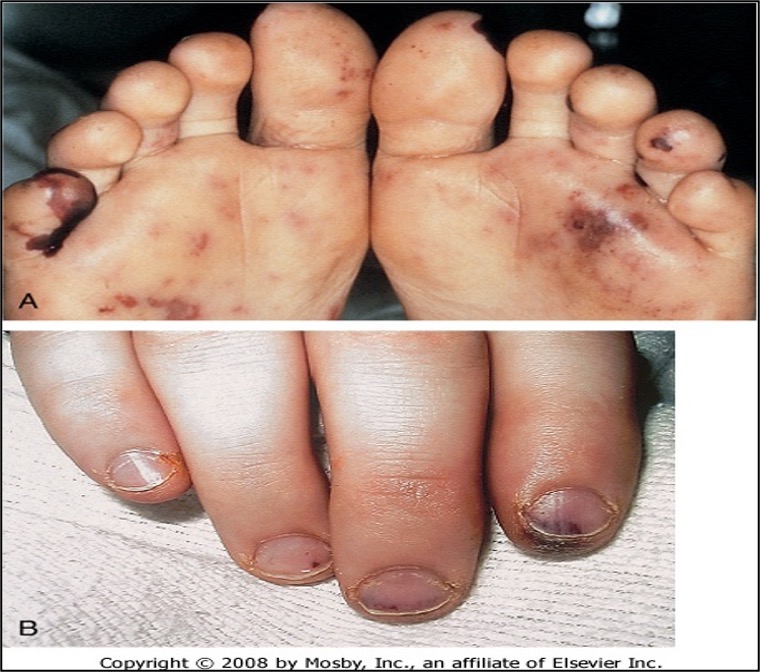
what are janeway lesions?
small, painless nodules caused by micro septic emboli (bacterial endocarditis)

what are Osler nodes?
painful erythematous nodular lesions that result from infective endocarditis

what are splinter hemorrhages?
hemorrhagic lesions / petechia seen w/ acute bacterial endocarditis
What would accentuate PMI or ventricular movements of S3/S4?
tangential lighting
What does JVP reflect?
pressures in RA (central venous pressure) best assessed from pulsations in right internal jugular vein
JVP is difficult to assess in _____
children under 12
What are visualized pulsations of the IJV from?
pressure changes from atrial filling, contraction, and emptying
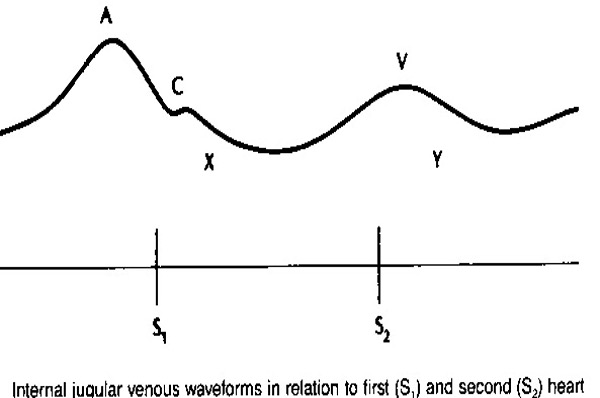
What JVP waveform is positive wave due to contraction of RA?
A
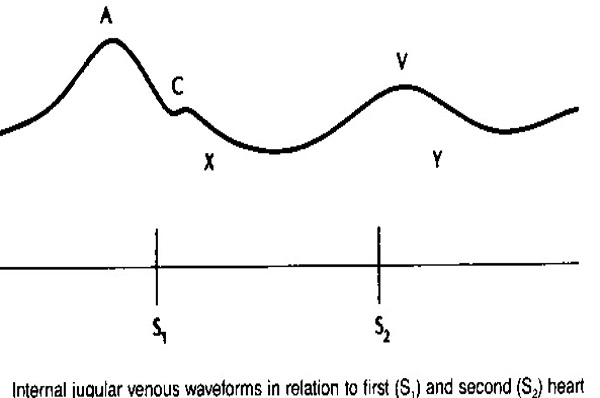
What JVP waveform is a positive deflection due to bulging of tricuspid valve toward the atria at onset of ventricular contraction?
C
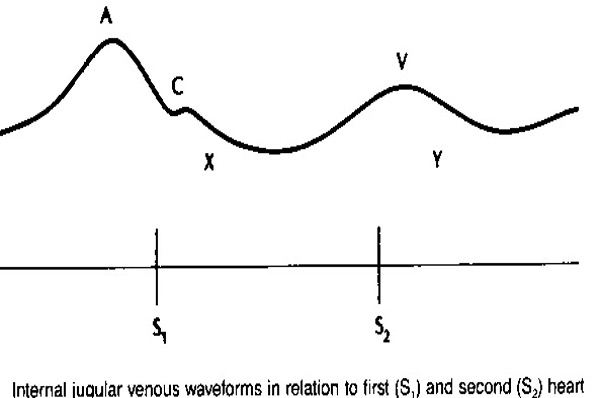
What JVP waveform is a negative deflection due to atrial relaxation?
X
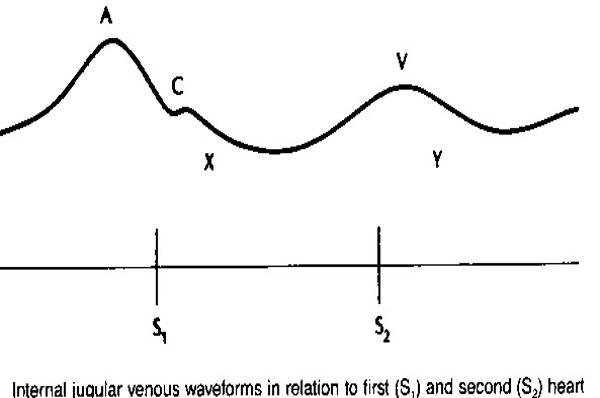
What JVP waveform is a positive deflection due to filling of RA against the closed tricuspid valve during ventricular contraction?
V
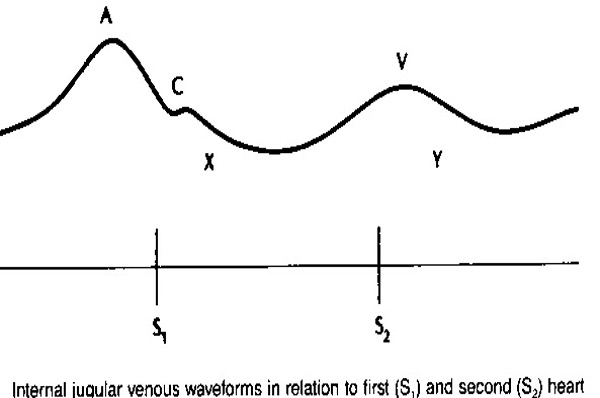
What JVP waveform is a negative deflection due to emptying of the RA?
Y
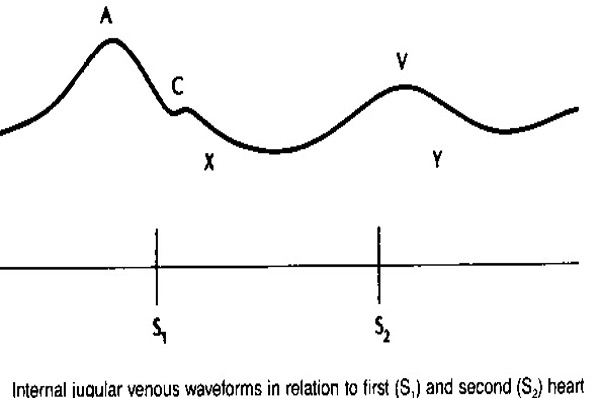
What is an increased A wave associated with?
tricuspid & pulmonic stenosis
1, 2, 3 degree AB blocks
SVT
junctional tachycardia
What might an absent A wave indicate?
A-Fib
What is an increased V wave seen in?
tricuspid regurgitation
ASD
constrictive pericarditis
At Carter’s Xing Vehicles Yield
Atrial contraction
ventriCle Contraction
atrial relaXation
Atrial Villing passively
blood from atrium to ventricle (Y not?)
How do you estimate JVP?
find highest point of oscillation of IJV
measure vertical distance from sternal angle (2nd rib joins the manubrium)
where is the sternal angle?
5cm above the RA, regardless of position of pt
How is JVP reported?
y + 5 = x
(y = measure; x = JVP)
If the bed is raised to 30 deg, the JVP …
cannot be measured bc meniscus is above jaw line
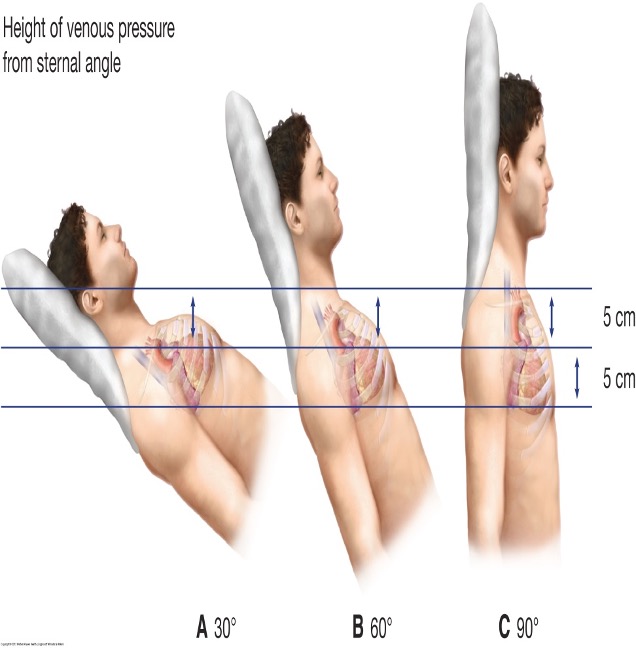
If the bed is raised to 60 deg, the JVP …
can be measured bc meniscus is visible
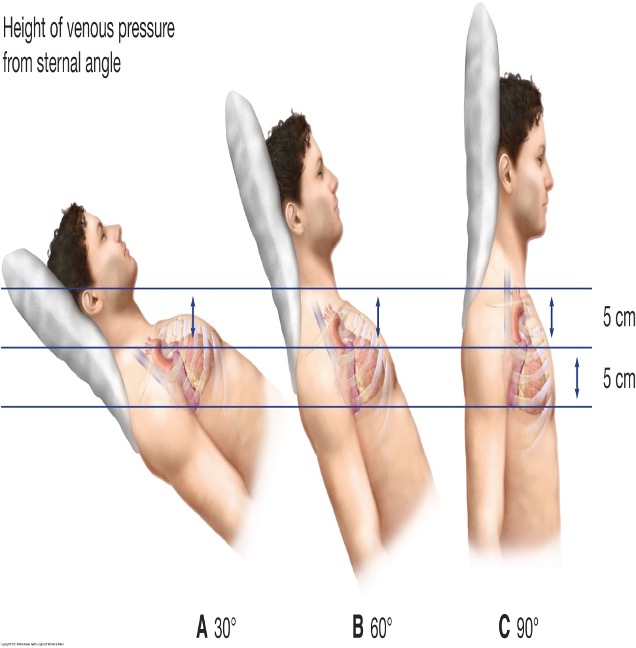
If the pt is upright, the JVP …
can’t be measured bc the veins are barely discernible above the clavicle
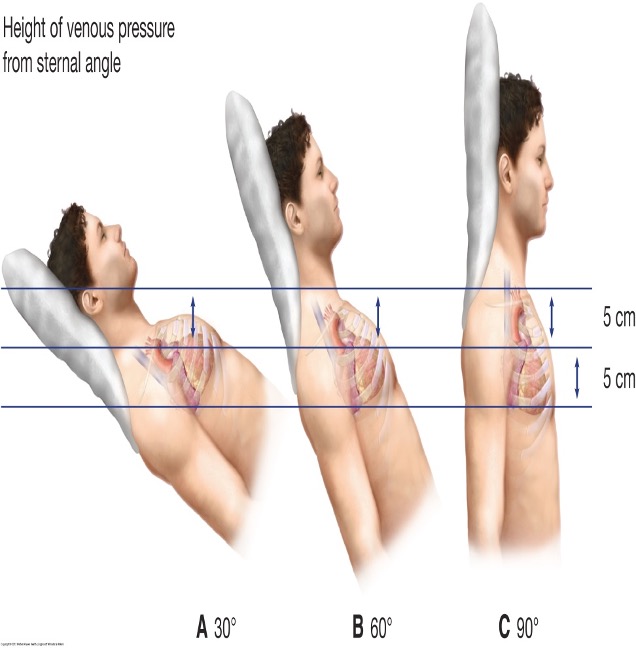
What is considered an elevated and abnormal JVP?
>3cm above sternal angle
>8cm above RA
obstructive lung dz will have an elevated venous pressure, but _____
the veins collapse on inspiration
How do you evaluate hepatojugular / abdominojugular reflex?
pt supine at 20-40 degrees
pressure applied above umbilicus for 30-60 s
normal: ≤ 3 cm inc in meniscus
abnormal: ≥ 4 cm inc in meniscus
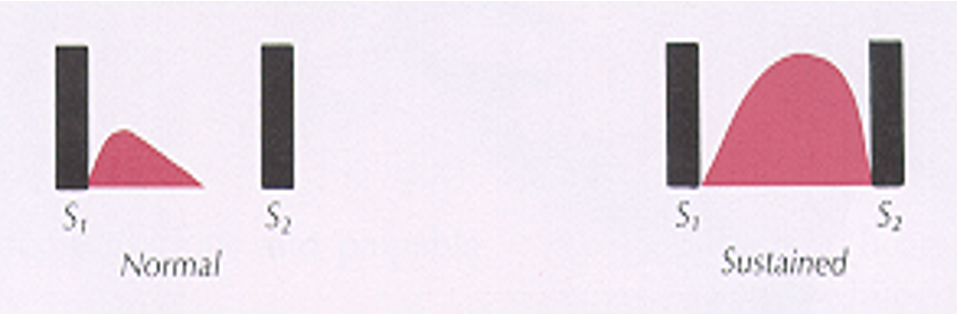
what does a sustained impulse indicate?
pressure overload seen in aortic stenosis or HTN
what does a diffuse or widened PMI indicate?
dilatation of LV seen in chronic volume overload
what does a PMI > 3cm indicate?
LVH
When evaluating PMI, if hypertrophy you may palpate _____
S4 gallop
when evaluating PMI, if dilatation you may palpate ____
S3 gallop
PMI amplitude is _____ after exercise, in hyperthyroidism, HTN, or severe anemia.
increased
PMI amplitude is _____ in dilated cardiomyopathy.
decreased
How long into systole would a normal apical impulse last?
first 2/3s
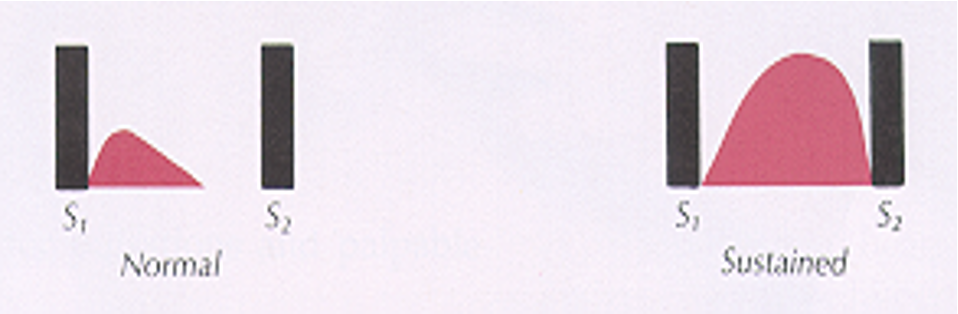
What would an apical impulse that’s sustained through systole indicate?
LVH
What should you do if you cannot identify PMI w/ pt in supine?
plate pt in left lateral decubitus position and ask them to exhale fully and hold for a few seconds
What are heaves or lifts?
large area of sustained outward motion
what are thrills?
superficial vibratory sensations felt on skin overlying a loud murmur (like vibrating cell phone)
How do you palpate thrills?
with metacarpal heads
When palpating anterior chest wall, what would a marked increase in amplitude be seen in?
chronic volume overload of RV such as ASD or pulmonary HTN
Percussion is not typical in a cardiovascular exam. When would you use percussion?
if unable to feel the apical impulse bc it suggests where to search
Explain how you would use percussion to locate the apical impulse.
percuss 3rd, 4th, and 5th ICS starting from left anterior axillary line and moving towards sternum
note the distance form left sternal border at which resonance changes to dullness
normal: ~6cm
How many different positions are you auscultating in?
4
(supine, sitting, leaning forward, and left lateral decubitus)
Where is S1 usually loudest?
at apex (tricuspid and mitral valve)
Where is S2 usually loudest?
at base (aortic and pulmonic valve)
what are distinct heart sounds that are distinguished by their pitch and their longer duration that is secondary to turbulent flow?
murmurs
which murmurs are almost always pathologic?
diastolic
When would splitting of S1 be heard?
only w/ coexisting RBBB and pulmonary HTN
Where and how would you hear physiologic splitting of S2?
heard in pulmonic area
loudest at base of 2nd ICS
sound at the end of systole
accentuated by inspiration
What should you suspect if splitting of S2 is heard at apex or P2 ≥ A2?
pulmonary HTN
S1 =
M1 + T1
S2 =
A2 + P2
when is S1 normally heard?
beginning of systole (softer at base, louder at apex)
What might be reasons for innocent/benign murmurs?
pregnancy, anemia, HTN, fever, hyperthyroidism
what are 3 things that impair forward blood flow?
the pump fails; LV has been damaged → signs of HF
the valve fails; blood goes in wrong direction → signs of valve failure
the arteries are obstructed, preventing blood flow to tissues
what are mid systolic murmurs typically due to?
blood flow across the semilunar valves
innocent, physiologic, or pathologic (AS, HOCM, pulmonary stenosis)
What is a pansystolic murmur usually due to?
chamber of high pressure to low pressure through an incompetent valve (MR, TR, VSD)
Continuous murmurs through systole and diastole are typically ____
non-valvular
(venous hum, pericardial friction rub, PDA, AV fistula)
What murmurs are high frequency?
MR
TR
AR
VSD
What murmurs are low frequency?
MS
TS
What murmurs are medium frequency?
AS
PS
HOCM
What grade murmur is very soft and not immediately apparent?
I
What grade murmur is soft but immediately audible?
II
What grade murmur is loud, but no palpable thrill?
III
What grade murmur is audible w/ palpable thrill?
IV
What grade murmur can be heard w/ stethoscope barely touching the skin and has a thrill?
V
What grade murmur can be heard w/ stethoscope not even touching the skin and has a thrill?
VI
what ssx correlate w/ murmurs?
EKG changes
extra heart sounds
abnormal CXR (widened mediastinum, cardiomegaly)
SOB
CP
palpitations
advanced age
who are innocent systolic murmurs common in?
young adults
describe innocent systolic murmurs
no evidence of physiologic / structural abnormalities in CV system
almost always < grade 3 intensity (NOT assoc. w/ thrill)
no radiation to the carotid arteries or axillae
systolic ejection in nature
what conditions increase the forward flow therefore increase murmur intensity?
exercise, anxiety, fear, increased SV assoc w/ long diastolic filling after a premature beat
Intensity of ejection murmurs closely parallel ____
changes in CO
Causes of aortic stenosis?
stenosis or narrowing of aortic valve
causes LVH due to obstructed blood flow → LV enlarges and holds less blood
causes: usually congenital, bicuspid aortic valve, rheumatic fever
where is aortic stenosis heard?
R 2nd ICS
what sx are associated w/ aortic stenosis?
syncope
angina
dyspnea
(SAD)
What tests should be performed for aortic stenosis?
ECHO or CT/MRI
shows dec mobility of aortic valve w/ small opening; valve often thickened and calcified