Microbiology Complete
1/479
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
480 Terms
Spore
Specialized structure formed by some bacteria that allows them to survive in harsh conditions.
Capsule
Discrete layer usually made of polysaccharides that protects bacteria against phagocytosis.
Slime (S) layer
Loose network of polysaccharides that mediates adherence to surfaces and plays a role in biofilm formation.
Outer membrane
Outer leaflet of the cell envelope in gram-negative bacteria, which contains endotoxin (LPS/LOS) and embedded proteins.
Periplasm
Space between the cytoplasmic membrane and outer membrane in gram-negative bacteria, which accumulates components exiting the cells.
Cell wall
Structure made of peptidoglycan that gives bacteria rigid support and protects against osmotic pressure damage.
Gram stain
Laboratory test used to differentiate bacteria based on their cell wall structure.
Peptidoglycan
Sugar backbone with peptide side chains that forms the netlike structure of the bacterial cell wall.
Gram-positive
Bacteria that retain the crystal violet dye in the Gram stain due to their thick peptidoglycan layer.
Gram-negative
Bacteria that turn red or pink in the Gram stain due to their thin peptidoglycan layer.
Acid-fast bacteria
Bacteria that retain the carbol fuchsin stain in the Ziehl-Neelsen stain due to their high lipid content in the cell wall.
Chocolate agar
Type of culture medium used to isolate Haemophilus influenzae, which contains factors V (NAD+) and X (hematin).
Thayer-Martin agar
Selective culture medium that favors the growth of Neisseria species by inhibiting the growth of other bacteria.
Bordet-Gengou agar
Culture medium used to isolate Bordetella pertussis, which contains potato extract, charcoal, blood, and antibiotics.
MacConkey agar
Culture medium used to differentiate lactose-fermenting enteric bacteria, which turn pink due to acid production.
Sabouraud agar
Culture medium used to isolate fungi.
Opsonization
Process of coating bacteria with antibodies or complement proteins to enhance their recognition and phagocytosis by immune cells.
Polysaccharide antigen
Type of antigen composed of sugar molecules, often found in the capsules of bacteria.
Urease-positive organisms
Microorganisms that produce the enzyme urease, which hydrolyzes urea to release ammonia and carbon dioxide.
Catalase-positive organisms
Microorganisms that produce the enzyme catalase, which breaks down hydrogen peroxide into water and oxygen.
Pigment-producing bacteria
Bacteria that produce pigments, which can give them distinct colors.
Biofilm-producing bacteria
Bacteria that can form biofilms, which are communities of microorganisms embedded in a self-produced matrix.
Spore-forming bacteria
Bacteria that can form spores, which are highly resistant structures that allow them to survive in harsh conditions.
Capsular polysaccharide
Polysaccharide structure found in the capsule of bacteria, which helps protect them from phagocytosis and complement-mediated lysis.
Protein A
Protein produced by Staphylococcus aureus that binds to the Fc region of IgG antibodies, preventing opsonization and phagocytosis.
IgA protease
Enzyme produced by certain bacteria (N gonorrhoeae N meningitidis, S pneumoniae, H influenzae) that cleaves IgA antibodies, allowing the bacteria to adhere to and colonize mucous membranes.
M protein
Protein produced by group A streptococci that helps prevent phagocytosis and may contribute to the development of autoimmune responses.
Transformation
Process by which competent bacteria can bind and import short pieces of environmental naked bacterial chromosomal DNA, resulting in the transfer and expression of newly transferred genes.
Competent bacteria
Bacteria that are capable of undergoing transformation.
Recipient cell
Bacterial cell that receives the transferred DNA during transformation.
Conjugation
Process by which genetic material, usually in the form of plasmids, is transferred between bacteria through direct cell-to-cell contact.
F+ cell
Bacterial cell that contains a plasmid called F+ plasmid, which carries genes required for sex pilus formation and conjugation.
F- cell
Bacterial cell that does not contain the F+ plasmid and is unable to form a sex pilus.
Sex pilus
Sructure formed by the F+ bacterium that contacts the F- bacterium during conjugation, allowing for the transfer of genetic material.
Hfr cell
Bacterial cell that contains the F+ plasmid incorporated into its chromosomal DNA, resulting in high-frequency recombination during conjugation.
Transduction
Process by which bacterial genes are transferred from one bacterium to another through the infection of a bacteriophage (a virus that infects bacteria).
Generalized transduction
Type of transduction where parts of bacterial chromosomal DNA become packaged in the phage capsid and are transferred to another bacterium upon infection.
Specialized transduction
Type of transduction where viral DNA incorporates into the bacterial chromosome, and upon excision, flanking bacterial genes may be excised with it and transferred to another bacterium.
Transposition
Process involving a transposon, a specialized segment of DNA, that can copy and excise itself and then insert into the same DNA molecule or an unrelated DNA.
Lipid A
Component of endotoxins that is part of the lipopolysaccharide (LPS) structure of gram-negative bacteria.
Some of the clinical effects associated with exotoxin-mediated infections.
Fever, shock, DIC
Examples of diseases caused by exotoxin-producing bacteria.
Tetanus, botulism, diphtheria, cholera
Examples of diseases caused by endotoxin-producing bacteria
Meningococcemia; sepsis by gram-negative rods
Pro-inflammatory cytokines induced by exotoxins that can lead to downstream cellular reactions.
TNF, IL-1, IL-6
Diphtheria toxin
Exotoxin produced by Corynebacterium diphtheriae that inactivates EF-2 via ribosylation → blocks host cell protein synthesis.
Diphtheria infection manifestation
Pharyngytis with pseudomembranes in the throat and severe lymphadenopathy (bulk neck), myocarditis.
Bacterias that inactivate elongation factor (EF-2) through ADP-ribosylation
Corynebacterium diphtheriae and Pseudomonas aeruginosa
Exotoxin A
Exotoxin produced by Pseudomonas aeruginosa that inactivates EF-2 via ribosylation → blocks host cell protein synthesis
Shigella spp
Group of bacteria that can cause severe gastrointestinal infections, leading to dysentery.
Shiga toxin
Exotoxin produced by Shigella spp that inactivates 60s ribosomes and damages the gastrointestinal mucosa.
Hemolytic-uremic syndrome (HUS)
Common cause of acute kidney failure in children. Presents with microangiopathic hemolitic anemia, kidney failure, and thrombocytopenia. Most cases develop following a diarrheal illness caused by Shiga toxin-producing organisms (E coli O157 H7, S dysenteriae). Transmission: undercooked beef.
Enterohemorrhagic E
Strain of E. coli that produces Shiga toxin and can cause severe gastrointestinal infections.
Enterotoxigenic E
Strain of E. coli that produces heat-labile and heat-stable toxins, leading to watery diarrhea.
Heat-labile toxin (LT)
Heat-sensitive toxin produced by Enterotoxigenic E. coli that overactivates adenylate cyclase, leading to increased secretion of fluid in the gut.
Heat-stable toxin (ST)
Heat-resistant toxin produced by Enterotoxigenic E. coli that overactivates guanylate cyclase, leading to decreased resorption of sodium and water in the gut.
Anthrax toxin
Exotoxin produced by Bacillus anthracis that mimics adenylate cyclase, leading to increased cAMP levels in host cells → neutrophil and macrophage disfunction and tissue edema.
LPS (lipopolysaccharide)
Component of the outer membrane of gram-negative bacteria.
α-hemolytic bacteria
Bacteria that cause partial oxidation of hemoglobin, resulting in a greenish or brownish color without clearing around the growth on blood agar. Examples include Streptococcus pneumoniae and viridans streptococci.
β-hemolytic bacteria
Bacteria that cause complete lysis of red blood cells, resulting in a pale/clear area surrounding the colony on blood agar. Examples include Staphylococcus aureus, Streptococcus pyogenes (group A strep), Streptococcus agalactiae (group B strep), and Listeria monocytogenes.
Staphylococcus aureus
Gram-positive, β-hemolytic bacteria that are catalase-positive and coagulase-positive cocci in clusters. They commonly colonize the nares, ears, axilla, and groin and can cause various inflammatory and toxin-mediated diseases.
Staphylococcus epidermidis
Gram-positive, catalase-positive, coagulase-negative cocci in clusters, not ferment mannitol. They are normal microbiota of the skin but can infect prosthetic devices and IV catheters by producing adherent biofilms (synthesis of an extracellular polysaccharide matrix). Novobiocin sensitive.
Staphylococcus saprophyticus
Gram-positive, catalase-positive, coagulase-negative cocci in clusters. They are normal microbiota of the female genital tract and perineum and are the second most common cause of uncomplicated urinary tract infections in young females.
Streptococcus pneumoniae
Gram-positive, α-hemolytic, cathalase negative, lancet-shaped diplococci that are encapsulated. They are sensitive to optochin and bile soluble. They commonly cause meningitis, otitis media, pneumonia, and sinusitis.
Viridans group streptococci
Gram-positive, α-hemolytic cocci that are optochin resistant and bile insoluble. They are normal microbiota of the oropharynx and can cause dental caries and infective endocarditis.
Streptococcus pyogenes (group A streptococci)
Gram-positive cocci in chains, beta-hemolytic, bicitracin sensitive. They cause various pyogenic, toxigenic, and immunologic diseases, including pharyngitis, cellulitis, impetigo, scarlet fever, toxic shock-like syndrome, necrotizing fasciitis, rheumatic fever, and glomerulonephritis.
Scarlet fever
Condition characterized by a blanching, sandpaper-like body rash, strawberry tongue, and circumoral pallor, usually occurring in the setting of group A streptococcal pharyngitis. It is caused by the production of erythrogenic toxin by Streptococcus pyogenes.
Streptococcus agalactiae
Gram-positive cocci that colonizes the vagina and causes pneumonia, meningitis, and sepsis, mainly in babies. It has a polysaccharide capsule that confers virulence and produces CAMP factor.
Streptococcus bovis
Gram-positive cocci that colonizes the gut. S. gallolyticus (S. bovis biotype 1) can cause bacteremia and infective endocarditis. Patients with S. bovis endocarditis have an increased incidence of colon cancer.
Enterococci
Gram-positive cocci that are normal colonic microbiota. Enterococci (E. faecalis and E. faecium) are penicillin G resistant and can cause UTI, biliary tract infections, and infective endocarditis. VRE (vancomycin-resistant enterococci) are an important cause of healthcare-associated infection. Gamma hemolysis (no hemolysis) on blood agar.
Bacillus anthracis
Gram-positive, spore-forming rod that produces anthrax toxin. It has a polypeptide capsule and colonies show a halo of projections. Cutaneous anthrax presents as a painless papule surrounded by vesicles and ulcer with a black eschar. Pulmonary anthrax is caused by inhalation of spores and presents with flulike symptoms that rapidly progress to fever, pulmonary hemorrhage, mediastinitis, and shock.
Bacillus cereus
Gram-positive rod that causes food poisoning. It can survive cooking rice and causes two types of food poisoning:emetic type (nausea and vomiting within 1-5 hours) and diarrheal type (watery, nonbloody diarrhea and GI pain within 8-18 hours).
Clostridia
Gram-positive, spore-forming, obligate anaerobic rods. Clostridium tetani produces tetanospasmin, an exotoxin causing tetanus. Clostridium botulinum produces a heat-labile toxin that inhibits ACh release at the neuromuscular junction, causing botulism. Clostridium perfringens produces α-toxin that can cause myonecrosis and hemolysis. Clostridioides difficile produces toxins A and B, which damage enterocytes and can lead to pseudomembranous colitis.
Tetanus
Disease caused by Clostridium tetani, characterized by spastic paralysis, trismus (lockjaw), risus sardonicus (raised eyebrows and open grin), and opisthotonos (spasms of spinal extensors). It is preventable with tetanus vaccine and treated with antitoxin, antibiotics, diazepam, and wound debridement.
Botulism
Disease caused by Clostridium botulinum, characterized by diplopia, dysarthria, dysphagia, dyspnea, and descending flaccid paralysis. It does not present with sensory deficits. Treatment includes human botulinum immunoglobulin.
Clostridium perfringens
Bacterium that produces α-toxin and can cause myonecrosis (gas gangrene) and hemolysis. It can also cause late-onset food poisoning symptoms if heavily spore-contaminated food is cooked but left standing too long at <60°C.
Clostridioides difficile
Bacterium that produces toxins A and B, leading to watery diarrhea, abdominal pain and pseudomembranous colitis. It is often associated with antibiotic use and can cause fulminant infection. Diagnosis: Nucleic acid amplification test (NAAT) → PCR to detect toxigenic strains. Treatment includes oral vancomycin or fidaxomicin.
Corynebacterium diphtheriae
Gram-positive rod ocurring in angular arrangements that causes diphtheria, a respiratory infection characterized by a thick grayish coating in the throat, transmitted through respiratory droplets. + Elek test for toxin. Grow in Cystine-tellurite agar (appear as black colonies), and Löffler medium is an alternative culture (intracellular metachromatic granules).
Corynebacterium diphtheriae treatment
Diphtheria antitoxin ± erythromycin or penicilin
Toxoid vaccine
Vaccine that contains inactivated toxins, used to stimulate an immune response and provide immunity against a specific toxin.
Listeria monocytogenes
Gram-positive facultitive intracellular rod, acquired by ingestion of unpasteurized diary products and cold deli meats, transplacental transmission. Cold enrichment, forms rocket tails. Generates pores in phagosomes allowing its scape into cytoplasm. Can cause amnionitis, sepcticemia, and spontaneus abortion in pregnant, granulomatosis infantiseptica, meningitis in immunocompromised patients, neonates and older adults, mild-self limited gastroenteritis in healthy individuals. Treatment: Ampicilin.
Nocardia
Gram-positive bacteria that forms branching filaments that can cause pulmonary and cutaneous infections. Can spread to CNS. Immunocompromised. Treatment: Sulfonamides (TMP-SMX).
Actinomyces
Gram-positive bacteria that forms branching filaments that can cause oral and facial abscesses. Can also cause PID with IUDs. Treatment: Penicilin.
Mycobacterium tuberculosis
Acid-fast rod that causes tuberculosis, a respiratory infection that primarily affects the lungs. Cord factor, which is a glycolipid on the surface of the cell wall, protects the bacteria from phagocytic killing and is directly cytotoxic to macrophages
Ghon complex
Combination of a primary tuberculosis lesion in the lung and associated lymph node involvement.
Miliary tuberculosis
Form of tuberculosis in which the infection spreads throughout the body, affecting multiple organs.
Interferon-γ release assay (IGRA)
Blood test used to detect tuberculosis infection by measuring the release of interferon-γ in response to specific antigens.
Leprosy
Chronic infectious disease caused by Mycobacterium leprae, an acid fast bacillus, characterized by skin lesions and nerve damage.
Lepromatous Form - Leprosy
Present diffusely over the skin, with leonine facies, and is comunicable (high bacterial load), characterized by low cell-mediated immunity with a largely Th2 response. Can be lethal. Treatment: Dapsone, rifampin, and clofazimine.
Tuberculoid Form - Leprosy
Limited to a few hypoesthetic, hairless skin plaques, caractherized by high cell-mediated immunity with a largely Th1 reponse and low bacterial load. Treatment: Dapsone, and rifampin,
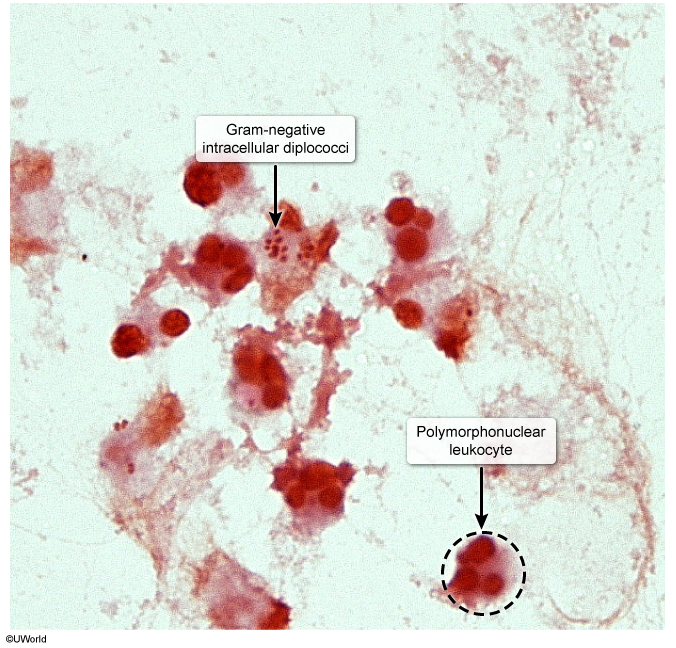
Neisseria gonorrhoeae
Gram-negative diplococci that metabolize glucose and produce IgA proteases. Contain lipooligosaccharides (LOS) with strong endotoxin activity. No polysaccharide capsule, no maltose acid detection. Often intracellular, sexually or perinatally transmitted. Causes gonorrhea, septic arthritis, neonatal conjunctivitis, pelvic inflammatory disease (PID), and Fitz-Hugh-Curtis syndrome. Disseminated disease present with the triad of polyarthralgia, tenosynovitis, and dermatitis or purulent arthritis. Diagnosis: NAAT, chocolate agar. Treatment: Single dose IM ceftriaxone, if coinfection with chlamidial add doxycycline.
Neisseria meningitidis
Gram-negative diplococci that metabolize glucose and maltose, produce IgA proteases. It have a polysaccharide capsule and it’s trasmitted vi respiratory and oral secretions (army barracks, college dorms). Causes meningococcemia with petechial hemorrhages and gangrene of toes, meningitis, and Waterhouse-Friderichsen syndrome (acute hemorrhagic adrenal insufficiency). Diagnosis: Culture-based tests or PCR, maltose acid detection. Tretament: Ceftriazone or penicilin G.
Haemophilus influenzae
Small gram-negative (coccobacillary) rod that is transmitted via aerosol. Nontypeable strains are the most common cause of mucosal infections (otitis media, conjunctivitis, bronchitis) as well as invasive infections. It causes epiglottitis (inspiratory stridor, patient tripo positioning), meningitis, otitis media, and pneumonia. Produce IgA protease. Culture on chocolate agar with S aureus (produce X-hematin and V-NAD+ factors). The vaccine contains type b capsular polysaccharide conjugated to diphtheria toxoid or other protein (2-18 months of age). Treatment: Amoxicilin +/- clavulanate for mucosal infection, ceftriaxone for meningitis, rifampin prophylaxis for close contacts.
Burkholderia cepacia complex
Aerobic, catalase-positive, gram-negative rod that causes pneumonia in and can be transmitted between patients with cystic fibrosis. It is often multidrug resistant and is a relative contraindication to undergoing lung transplant.
Bordetella pertussis
Gram-negative, aerobic coccobacillus that produces adenylate cyclase toxin (inhibit phagocyte activity), and tracheal cytotoxin (destroy ciliated epithelial cells). Presents with cough associated with turning red in the face, inspiratory whoop, or posttussive emesis, lack of fever, and lymphocytosis. Progresses through three clinical stages: catarrhal, paroxysmal, and convalescent. Prevented by Tdap and DTaP vaccines. Treatment: Macrolides (azythromicin), if allergic TMP-SMX.
Brucella
Gram-negative, aerobic coccobacillus that is transmitted via ingestion of contaminated animal products. It survives in macrophages in the reticuloendothelial system and can form non-caseating granulomas. It typically presents with undulant fever, night sweats, and arthralgia. Treatment: doxycycline + rifampin or streptomycin.
Legionella pneumophila
Gram-negative rod (use silver stain) that causes Legionnaires' disease (severe pneumonia - unilateral and lobar, fever, GI and CNS symtomps) and Pontiac fever (mild flulike symptoms, bradicardia, headache, confussion, watery diarrhea). It is transmitted via aerosol from environmental water sources and grows on charcoal yeast extract medium with iron and cysteine. It is detected by the presence of antigen in urine. Labs may show hyponatremia. Outbreaks associasted with cruise ships, nursing homes. Treatment: Macrolide or quinolone.
Pseudomonas aeruginosa
Aerobic, motile, catalase-positive, gram-negative rod that is frequently found in water. It has a grapelike odor and is associated with various infections, including pneumonia, sepsis, UTIs, ecthyma gangrenosum, osteomyelitis, hot tub folliculitis, and otitis externa. It produces a mucoid polysaccharide capsule (may contribute to chronic pneumonia in cystic fibrosis due biofilm production) and various virulence factors such as phospholipase C, endotoxin, exotoxin A, and pigments (green). It can cause corneal ulcers/keratitis in contact lens wearers or minor eye trauma.
Salmonella and Shigella
Gram-negative rods that are non-lactose fermenters, oxidase-negative, and can invade the GI tract via M cells of Peyer patches.
Yersinia enterocolitica
Gram-negative pleomorphic rod/coccobacillus that is usually transmitted from pet feces, contaminated milk, or pork. Cause bloody diarrhea, pseudoappendicitis (due to mesenteric adenitis and/or terminal ileitis, reactive arthritis in adults.
Lactose-fermenting enteric bacteria
Bacteria that can ferment lactose and produce pink colonies on MacConkey agar. Examples: Citobacter, E coli, Enterobacter, Klebsiella, Serratia.