Dermatology
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
What are key physiologic functions of equine skin?
Barrier protection, temperature regulation, shape & form, adnexa production, fluid reservoir, immunoregulation, and sensory perception.
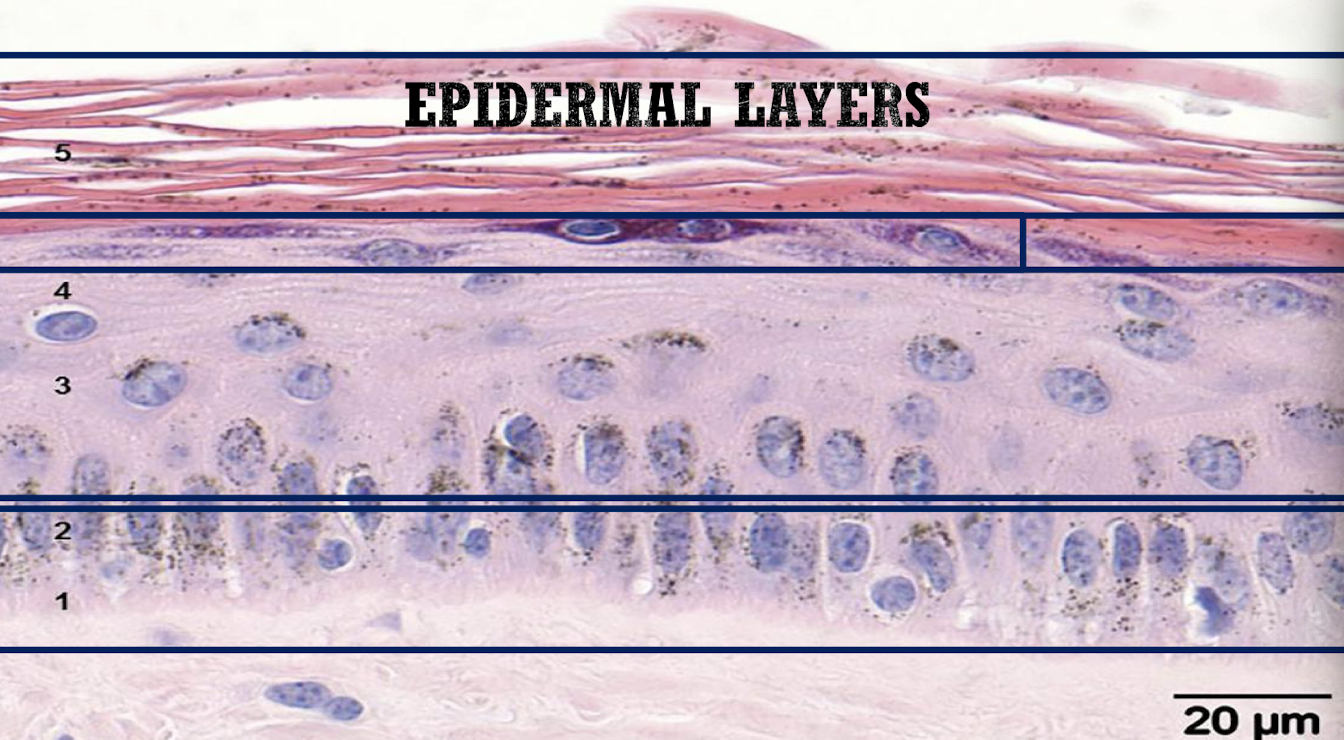
Name the layers of the equine epidermis from deep to superficial
Stratum basale → stratum spinosum → stratum granulosum → stratum lucidum (not in horses) → stratum corneum
What anchors epidermis to dermis and what structures exist in the dermis?
The basement membrane zone anchors them; dermis contains collagen & elastin, fibroblasts, dendrocytes, hair follicles, sebaceous/apocrine glands, blood & lymphatic vessels, and nerves.
What are the three hair-growth phases?
Anagen (growth), Catagen (transition), Telogen (rest). Mane/tail skin ≈ 2× thicker than body skin
What history elements are vital in skin cases?
Signalment, duration, lesion distribution, seasonality, pruritus, treatments & response, other animals affected, topical products, diet/environment, travel, preventive care, concurrent disease
What should you evaluate on exam?
Primary/secondary lesions, mucous membranes, mucocutaneous junctions, inguinal region, feathered limbs; record & measure lesions
Define leukoderma vs leukotrichia
Leukoderma = loss of skin pigment → pressure sores, burns, freezing, UV
Leukotrichia = loss of hair pigment → spotted, reticulated, hyperesthetic(more uncomfortable)

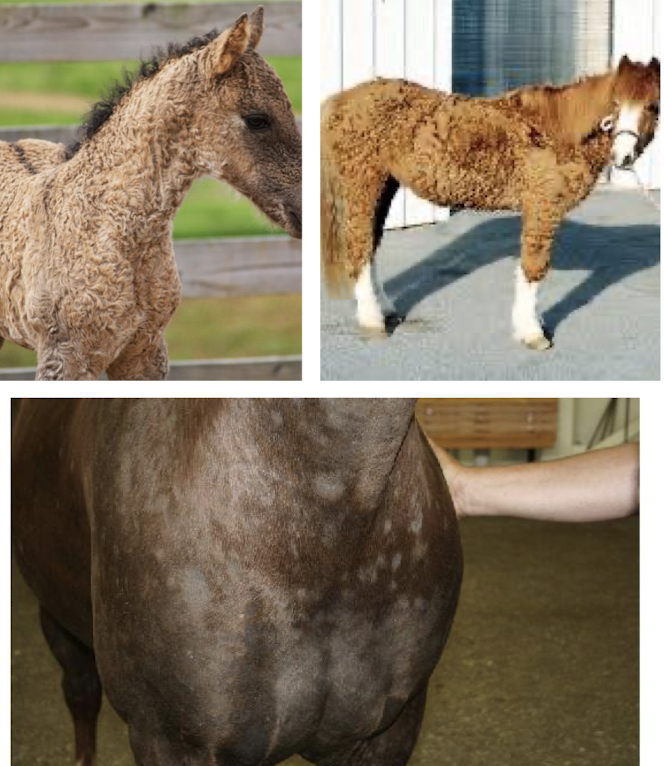
What conditions cause abnormal hair?
Hirsutism / hypertrichosis (PPID)
Alopecia areata (autoimmune)
Anagen/telogen defluxion (systemic illness or malnutrition)
What is exuberant granulation tissue and how is it managed?
Granulation = phase of wound healing.
Over-production of fibroblasts during healing (“proud flesh”), common on distal limbs; prevents closure; requires surgical debridement

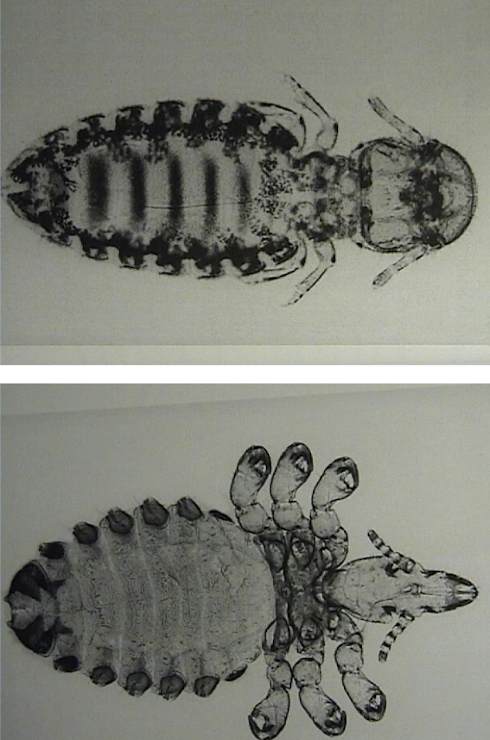
What causes pediculosis and how is it managed?
Damalinia equi (biting) and Haematopinus equi (sucking) lice; common in winter. Signs – pruritus, rubbing, dull coat. Treat: ivermectin 200 µg/kg PO q2 wk ×3 or topical eprinomectin weekly ×4 ± pyrethrin sprays. Clean tack and treat all horses.
How do these mites differ and what is the treatment?
Sarcoptes = burrowing, zoonotic; starts head/neck → generalized. Psoroptes = non-burrowing on face/ears. Both → severe pruritus and alopecia. Treat: ivermectin 200 µg/kg PO ×2 (14 days apart) or moxidectin 400 µg/kg once + environmental cleaning
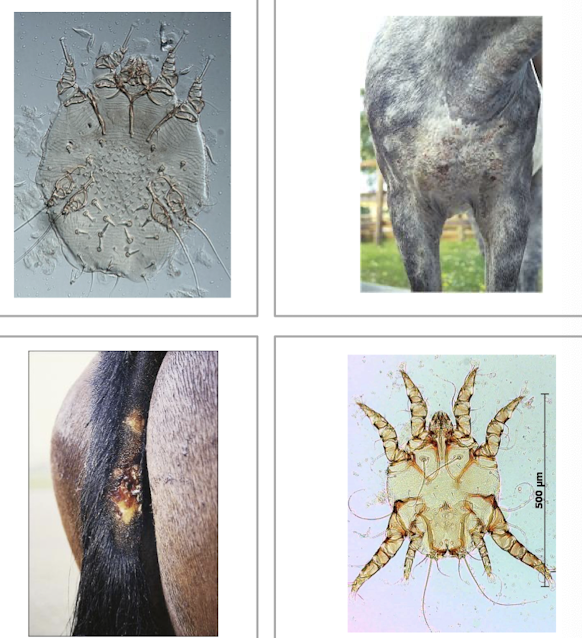
What are key features and management for Chorioptic mange?
Chorioptes bovis lives on feathered limbs, survives off host. Causes intense itching, erythema, crusting, lichenification. Diagnosis: superficial scrape. Treat: clip feathers, medicated wash, topical eprinomectin/fipronil, systemic ivermectin/moxidectin; clean premises.

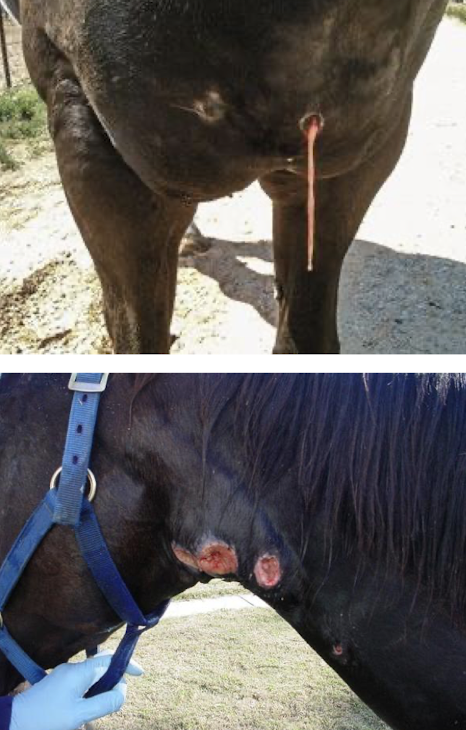
What causes summer sores and how do they appear?
Fly-transmitted Habronema/Draschia larvae invade wounds → ulcerated lesions, eosinophilic ulcer with yellow gritty “kunkers.” Occurs in spring & summer, esp. Arabians and greys. Diagnose: biopsy with larvae

How is Habronemiasis treated and prevented?
Treat: ivermectin/moxidectin PO + topical anti-inflammatory/antimicrobial + surgical debridement. Compounded ointment
Prevent: fly control, wound protection, manure management.
What is Onchocerca cervicalis and how does it cause skin lesions?
Adults in the ligamentum nuchae release microfilariae migrating in skin to ventral midline and face → hypersensitivity reaction with pruritic alopecia and crusts, mainly spring–summer.
What lesions and sites are typical of Onchocerciasis?
Alopecia, scaling, ulceration on face, neck, chest, ventrum. Diagnosis: skin biopsy showing microfilariae; seasonality supports it.

How is Onchocerciasis treated and what side effects can occur?
Ivermectin or moxidectin PO 2–3×/month. Microfilarial death may cause transient edema (ventral, umbilical, eyelids), pruritus, or fever. Cannot kill the female adult in the nuchae ligament

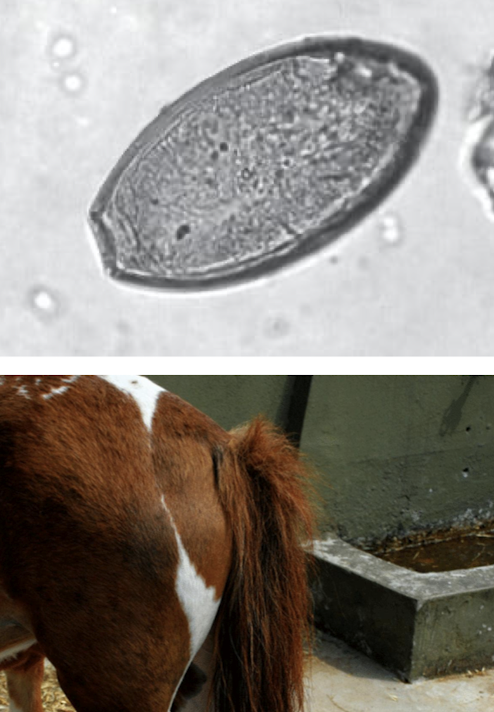
How do Oxyuris equi pinworms cause pruritus and how are they controlled?
Females lay sticky eggs on perineum → tail rubbing, irritation. Diagnosis: tape test.
Control: clean perineum/stall surfaces; deworm with ivermectin or moxidectin.
What are the main bacterial causes of equine skin disease?
Dermatophilus congolensis, Staphylococcus spp., Streptococcus spp., Corynebacterium pseudotuberculosis, Actinomyces, and Clostridium spp. They enter through wounds or moist skin and cause pyoderma, abscesses, and necrosis.
What causes Dermatophilosis (“rain rot”) and what conditions favor it?
Caused by Dermatophilus congolensis. Moisture, chronic damp coats, or damaged skin favor infection. Immunocompromised horses are more susceptible

What are typical signs of Dermatophilosis?
Crusted papules with “paintbrush” tufts of hair, often on the dorsum, face, neck, and distal limbs. In severe cases, lesions can become painful or secondarily infected

How is Dermatophilosis diagnosed and treated?
Diagnosis: saline slide smear or biopsy showing filamentous bacteria.
Treatment: dry environment, antibacterial shampoo, topical antibiotic cream, and disinfecting grooming tools

What causes superficial pyoderma and where do lesions appear?
Staphylococcus (coagulase +) or Streptococcus spp. infect disrupted skin. Lesions: crusting, pruritus, alopecia, often under tack or on pasterns → mud fever

How is superficial pyoderma diagnosed and managed?
Diagnosis: bacterial culture, cytology, or biopsy.
Treatment: mild = self-limiting; moderate = topical antimicrobial shampoo; severe = systemic antibiotics ± topical therapy

What organisms cause abscesses and how are they treated?
Streptococcus equi equi(strangles), C. pseudotuberculosis(pigeon fever), Actinomyces, Clostridium spp. or secondary trauma/injections.
Treatment: allow maturation and drainage, local limb therapy, and systemic antimicrobials.
What are the clinical forms and treatment for C. pseudotuberculosis infection?
Forms: external/internal abscesses, ulcerative lymphangitis, or pyoderma.
Diagnosis: appearance, culture
Treatment: drainage and long-term systemic antibiotics.

What causes clostridial necrosis and how is it treated? Clostridial Myo/Dermonecrosis
Occurs after wounds or intramuscular injections. Causes acute swelling and tissue sloughing. U/S → Gas under skin
Diagnose: culture ± histopathology
Treatment: surgical debridement and high-dose penicillin or metronidazole

What are key viral causes of equine dermatologic lesions?
Equine papillomavirus, vesicular stomatitis virus, and EHV-3 (coital exanthema). They cause warts, vesicles, or ulcerations; some are zoonotic or reportable
What causes equine warts and how are they transmitted?
Caused by Equus caballus papillomavirus. Spread by direct contact, fomites, or black flies. Seen in horses <4 years. Lesions regress spontaneously in 3–4 months

What are aural plaques and how are they managed?
Causes by Equine Papillomavirus Type 3 (EPV-3) → Smooth or raised white lesions on the inner ear pinna. They do not regress spontaneously.
Treatment: benign neglect, surgical excision, cryonecrosis(only for a couple lesions), or immunomodulators

What are key facts about vesicular stomatitis?
Caused by vesicular stomatitis virus; affects horses, ruminants, swine, and humans.
Transmission: flies or contact.
Signs: vesicles → ulcers around mouth. Will not want to eat
Note: reportable and zoonotic; self-limiting disease

What causes equine coital exanthema and how is it managed?
Caused by EHV-3; spread by breeding, fomites, or insects → reportable in some areas
Lesions: shallow ulcers on vulva, perineum, penis, or prepuce.
Treatment: isolate from breeding, avoid corticosteroids, supportive care.

What are the most common fungal causes of equine skin disease?
Trichophyton spp., Microsporum spp. (dermatophytes), and Pythium insidiosum. They cause alopecia, crusting, or ulcerated nodular lesions depending on depth and organism type.
What causes dermatophytosis (“ringworm”) and how is it transmitted?
Caused by Trichophyton equinum/mentagrophytes or Microsporum gypseum/canis. Spread by direct contact or contaminated tack, brushes, or stalls. Risk increases with poor hygiene and damp coats

What are the typical lesions of ringworm in horses?
Circular alopecic areas with scaling and crusting. Often on face, neck, or saddle area. May be mildly pruritic or asymptomatic
How is dermatophytosis diagnosed and treated?
Diagnosis: microscopic exam of hairs, fungal culture, or PCR.
Treatment: antifungal or accelerated H₂O₂ shampoo weekly 6–8 weeks, or 0.2% enilconazole rinse diluted 1:1. Isolate affected horses and disinfect environment → treat beyond visual resolution of lesions
Wear PPE
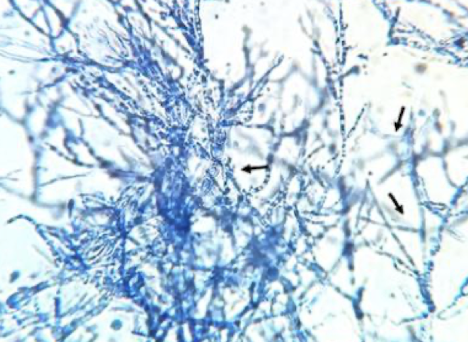
What causes pythiosis and what are the risk factors?
Caused by Pythium insidiosum, an aquatic oomycete. Risk increases in warm, wet regions where horses stand in stagnant water. Enters through wounds in submerged skin
How does cutaneous pythiosis appear clinically?
Forms granulomatous, ulcerated nodules resembling tumors with gray-yellow necrotic “kunkers.”(are pathognomonic) Common on limbs, chest, or abdomen. Lesions are locally invasive and non-healing
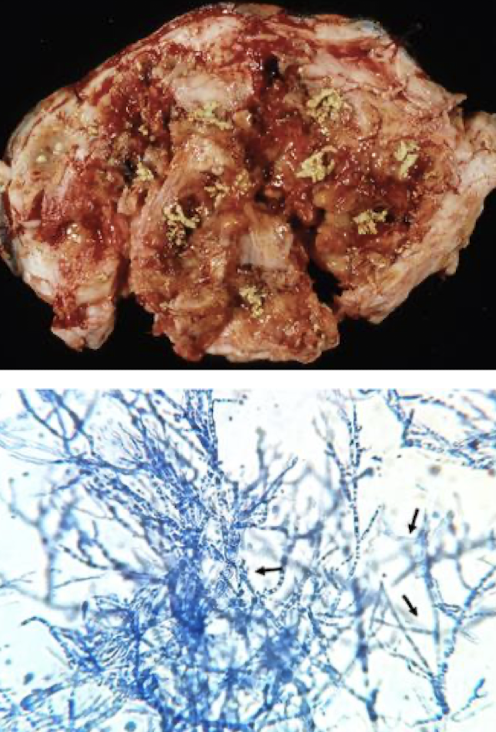
How is pythiosis diagnosed and treated?
Diagnosis: wet mount showing hyphae, serologic antibody tests, or PCR.
Treatment: complete surgical excision when possible, plus immunotherapy. Prognosis depends on lesion extent.
What is equine urticaria and what triggers it?
A Type I or II hypersensitivity reaction causing transient wheals or hives.
Triggers include feed, contact or inhalant allergens, drugs, temperature changes, exercise, insect bites, or idiopathic causes
How is urticaria identified and managed?
Based on sudden-onset raised, itchy welts.
Treatment: remove allergen if known, administer antihistamines or corticosteroids, and minimize stress or environmental triggers
What causes insect bite hypersensitivity and which breeds are predisposed?
Allergic response to Culicoides and other fly saliva.
Common in Icelandic, Friesian, Arabian, and Quarter Horses, especially over 3–4 years old. Often hereditary or worsened by importation
What are hallmark signs of insect bite hypersensitivity?
Severe pruritus with mane/tail rubbing, excoriations, alopecia, lichenification, pigment changes, and secondary bacterial infection. Distribution depends on insect species (black flies head, ears, ventral abdomen)

How is insect bite hypersensitivity diagnosed and treated?
Diagnosis: clinical exam, biopsy, or intradermal testing.
Treatment: allergen-specific immunotherapy, corticosteroids, antihistamines, and soothing topical shampoos (oatmeal/colloidal)
What are effective prevention strategies for insect bite hypersensitivity?
Avoid turnout during peak insect hours, use fans, move horses away from water, apply insect repellents, use misters/traps, and provide fly sheets or masks
What is immune-mediated vasculitis and what are common causes?
Type I–III hypersensitivity reaction of dermal vessels caused by infections (equine viral arteritis, influenza, C. pseudotuberculosis, Streptococcus equi most common) or idiopathic immune triggers

How does vasculitis present and how is it managed?
Signs: edema, erythema, petechiae, oral ulcers, bullae.
Diagnosis: titers or skin biopsy. Make sure they do not have strep equi before vaccinating
Treatment: address underlying cause, corticosteroids for immunosuppression, and supportive care (bandaging, hydrotherapy)
What are the most common equine skin tumors, and why are they important?
Sarcoids, squamous cell carcinoma (SCC), melanoma, and eosinophilic granuloma are most common. They can interfere with tack, ulcerate, or metastasize. Diagnosis via biopsy and treatment depends on tumor type and location
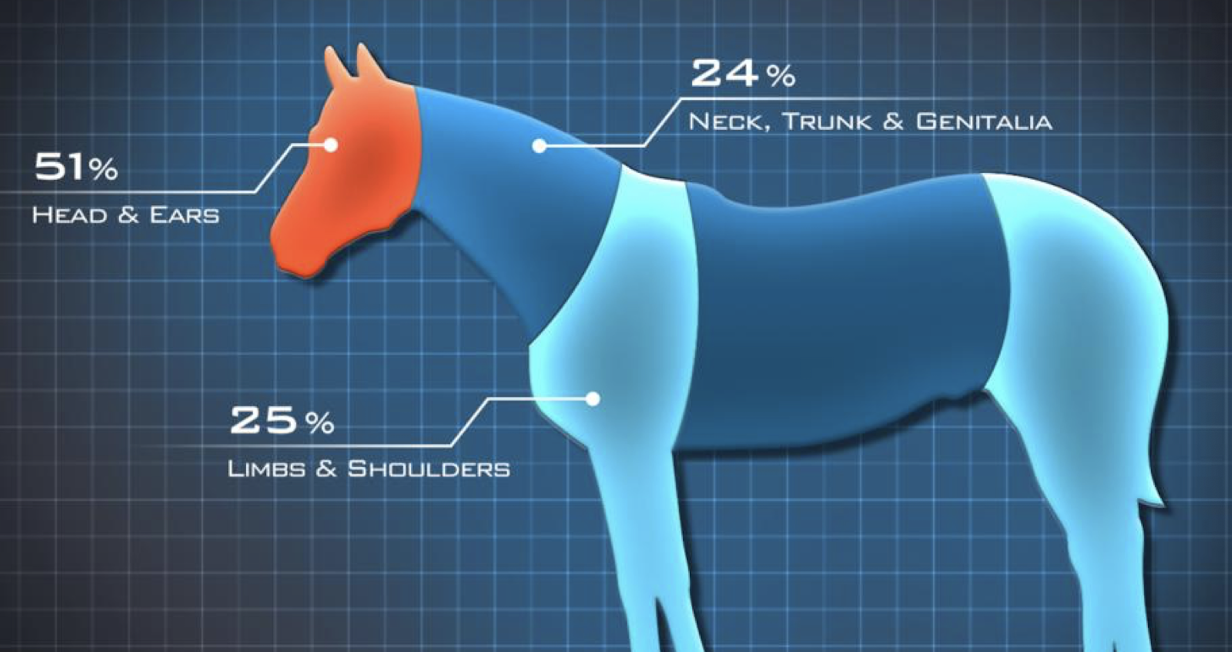
What causes sarcoids and what are risk factors?
Viral-induced tumors caused by bovine papillomavirus types 1 and 2. Risk factors include prior cattle contact, skin wounds, and familial predisposition. Usually occur in horses >1 year old
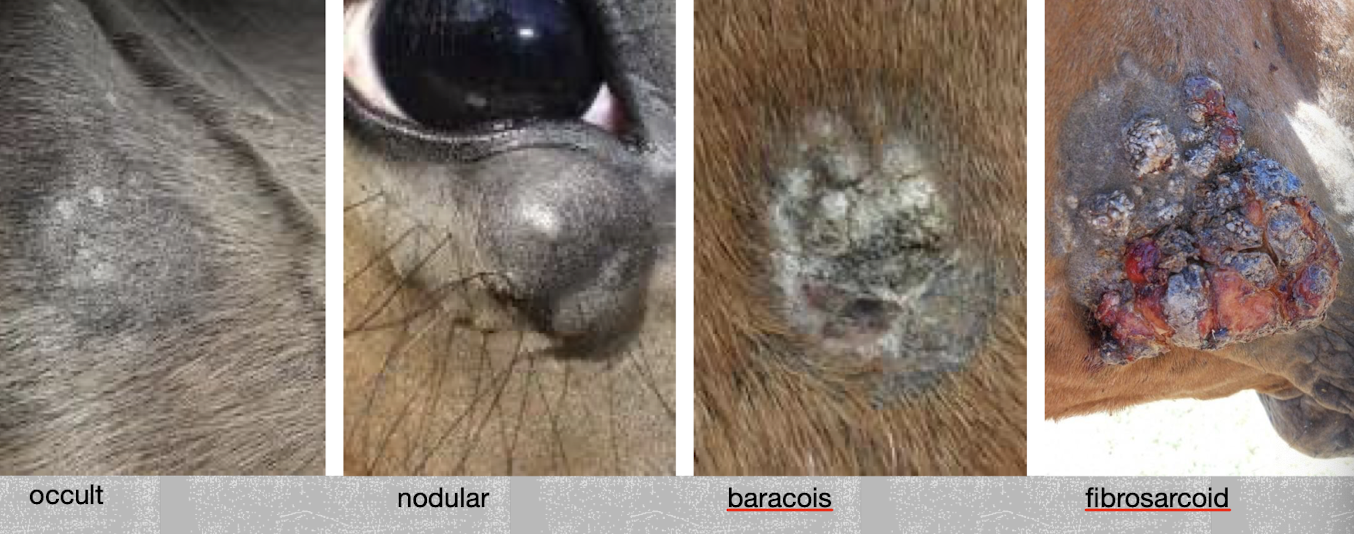
How are sarcoids identified and confirmed?
Diagnosis is usually by clinical appearance (wart-like, fibroblastic, or ulcerative lesions) and confirmed via biopsy and histopathology. Biopsy may risk local spread, so careful site selection is needed
What are treatment options for sarcoids?
Options include benign neglect (for small stable lesions), wide surgical excision, cryotherapy, CO₂ laser ablation, radiation, BCG immunotherapy, intralesional cisplatin or 5-fluorouracil, imiquimod cream, or herbal agents (e.g., Xxterra)
What causes equine SCC and which sites are most affected?
Caused by UV exposure, papillomavirus infection, or chronic irritation (smegma is carcinogenic). Affects unpigmented skin, mucocutaneous junctions—especially periocular and penile areas

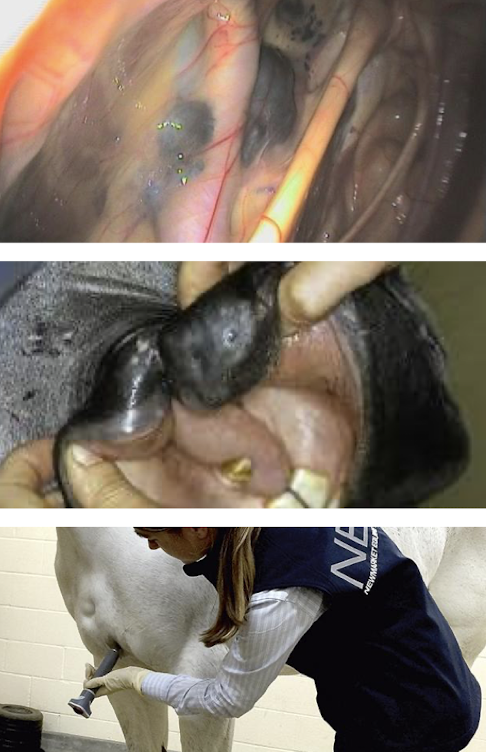
How does SCC behave and how is it managed?
Locally invasive but slow to metastasize.
Diagnosis: biopsy → take the whole thing
Treatment: wide surgical excision, cryotherapy, radiation, topical 5-fluorouracil, intralesional cisplatin, or NSAIDs like piroxicam to reduce recurrence
What are risk factors for equine melanoma and where do they occur?
Common in grey horses >15 years old; 67–80% affected. Also seen in Arabians, Thoroughbreds, and Percherons.
Sites: perineum, tail, genitalia, parotid region, and face

How do melanomas behave and how are they treated?
Progressive with age, locally aggressive, and often metastasize.
Diagnosis: appearance or biopsy.
Treatment: surgical removal, intralesional cisplatin, cimetidine (slows growth), or canine melanoma vaccine (Oncept)
What is eosinophilic granuloma and how is it treated?
Common, non-neoplastic nodules (0.5–10 cm) on withers, back, or neck due to hypersensitivity or trauma. Where the tack sits
Diagnosis: physical exam or biopsy.
Treatment: surgical removal or intralesional corticosteroid injection
What are the main categories of congenital and hereditary equine skin diseases?
Genetic connective-tissue and epidermal disorders causing fragile skin, poor healing, and joint or hoof abnormalities. Examples include HERDA, Warmblood Fragile Foal Syndrome, and Junctional Epidermolysis Bullosa. Most common in quarter horses

What is HERDA, which breeds are affected, and what are key features?
Autosomal recessive collagen defect in Quarter Horses, Paints, and Appaloosas. Skin is hyperextensible and tears easily, leading to scarring by age 2. Horses appear normal at birth. No treatment; DNA testing required for breeding
What are the characteristics of Warmblood Fragile Foal Syndrome?
Recessive genetic disorder causing thin, friable skin, severe joint laxity, and incomplete abdominal wall. Affected foals may be stillborn or unable to stand. Fatal; no treatment
What are the clinical signs and outcomes of Junctional Epidermolysis Bullosa?
Autosomal recessive blistering disease (Type 1 in Drafts, Type 2 in Saddlebreds). Causes skin and mucosal ulcers, dental enamel defects, and hoof sloughing soon after birth. No treatment; euthanasia often necessary

What general skin reactions result from chemical or physical injury in horses?
Photosensitization, burns, scalding, and pressure necrosis. These cause erythema, necrosis, or ulceration that may mimic infectious or immune diseases
What causes primary photosensitization and how is it treated?
Ingestion or contact with photodynamic agents (e.g., St. John’s wort, clovers, tetracyclines) in unpigmented skin.
Signs: erythema, edema, erosions.
Treatment: remove source and limit UV exposure

How are burns classified in horses and what determines prognosis?
1st degree: erythema, edema, desquamation
2nd degree: vesicles, necrosis, eschar
3rd degree: loss of sensation, deep eschar
Mortality increases if >50 % of skin affected. Full extent visible within ~14 days

How should thermal or chemical burns be managed?
Move horse to safety, cool area with water, give analgesics and IV fluids. Leave eschar intact, gently clean surrounding skin, apply occlusive dressing (honey or silver sulfadiazine), bandage lightly, and repeat as needed

What causes skin scalding and how is it prevented?
Due to diarrhea, urine scald, or neurologic dysfunction—especially in foals.
Treatment: clean area frequently, apply zinc oxide to affected skin and petroleum jelly to protect unaffected areas
What are the causes and treatments for pressure necrosis?
Caused by prolonged recumbency, tight bandages, casts, or ill-fitting tack.
Treatment: remove pressure source, improve bedding, rotate horse, clean and debride tissue, apply topical antimicrobials, and protect skin from further trauma
