1/2- bone bio + occlusal forces
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
definition of bone
specialized connective tissue hardened by mineralization w/ calcium phosphate in the form of hydroxyapatite
5 functions of bone
support
protection
movement
mineral storage: calcium + phosphates
hematopoiesis: major site of blood cell formation in adults, within marrow spaces
2 components of bone
extracellular matrix
cellular component
2 components of the extracellular matrix of bone
inorganic matrix (67%): mainly hydroxyapatite crystals
organic matrix (33%): collagen type I
4 cell types that are in the cellular component of bone
osteocytes: maintains bone tissue
osteoblasts
osteogenic cell: stem cell
osteoclast
2 components of mineralized bone structure
compact (cortical)
trabecular (spongy)
3 components of non-mineralized bone structure
marrow
cells
connective tissue
what’s the alveolar process
forms + supports the tooth sockets (alveoli)
alveolar process is formed by which cells
cells from dental follicle (alveolar bone proper) + cells independent of tooth development
when does the alveolar process form
when the tooth erupts to provide the osseous attachment to the forming PDL
T/F: the alveolar process remains after a tooth is extracted
false, it gradually disappears after the tooth is lost
3 components of the alveolar process
compact bone
trabecular bone
alveolar bone proper
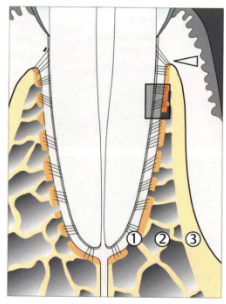
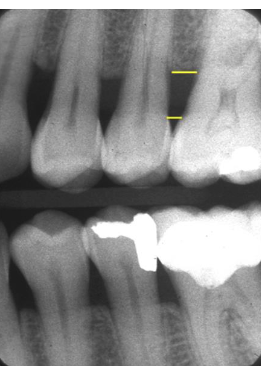
what are the numbers
alveolar bone
spongy (trabecular) bone
cortical plate
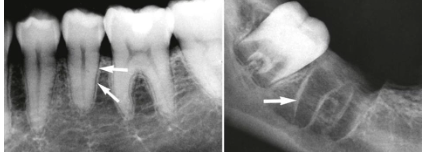
what are the arrows pointing to
lamina dura/cribriform plate
T/F: lamina dura/cribriform plate is compact
false, it has many perforations that allow it to have neurovascular bundles link to the PDL
how is cementum connected to alveolar bone
Sharpey’s (collagen) fibers from cementum reach across PDL space and insert into alveolar bone proper
what determines the morphology of alveolar processes
size, shape, location, function of teeth
what are 2 alveolar bone defects
fenestration: exposed root due to absence of lingual/buccal alveolar bone lamina
dehiscence: roots extending through marginal bone
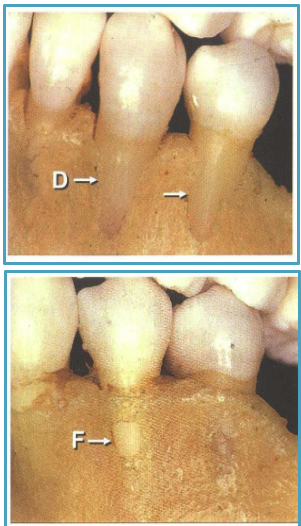
alveolar bone defects are more common on facial or lingual
facial
common areas of fenestrations vs. dehiscence
fenestration: maxilla
dehiscence: mandible
alveolar bone level runs ___ to the levels of the 2 CEJs
parallel
healthy distance from CEJ → alveolar bone
2-3 mm
what does an implant lack compared to a real tooth
implant does not have:
PDL
cementum
Sharpey’s fibers (true CT attachment)
what’s the biologic width (supracrestal attached tissue width) for implants
4-4.5 mm
T/F: periodontal bone will adapt to strong occlusal forces
true
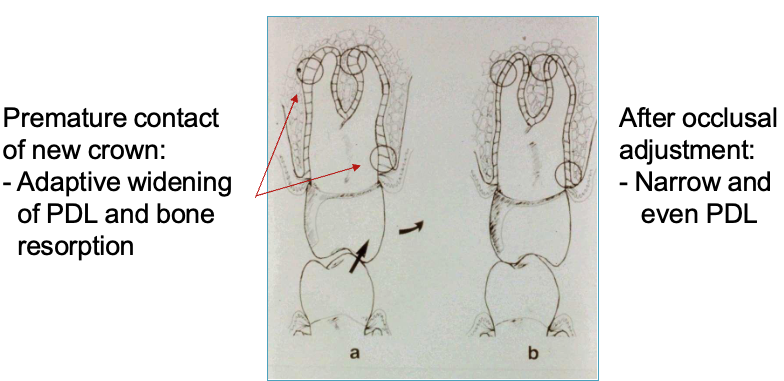
describe 2 characteristics of periodontal bone when it's adapting to strong occlusal forces
narrow + even thickness of PDL
widened PDL space: hour glass shape of marginal + peri-apical bone
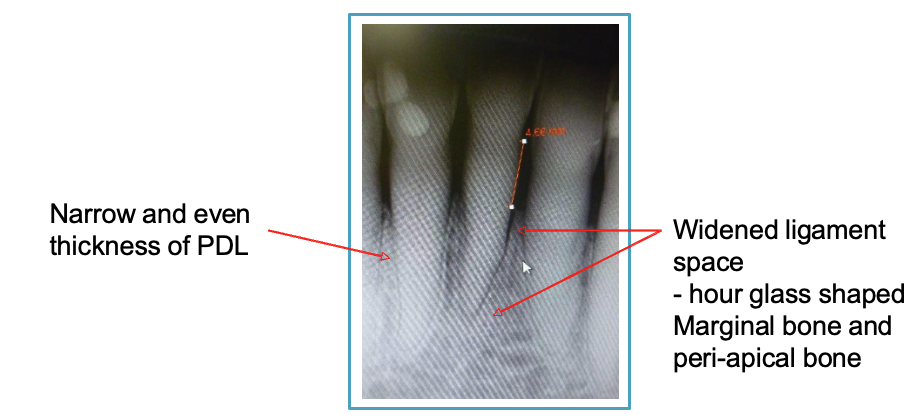
T/F: adaptation of periodontal bone to heavy occlusion is reversible
true
3 types of perio pockets
normal: apical termination of junctional epithelium is at CEJ
supraboney: proliferating pocket epithelium + remnant of junction epithelium persists
infraboney: extends beyond alveolar crest

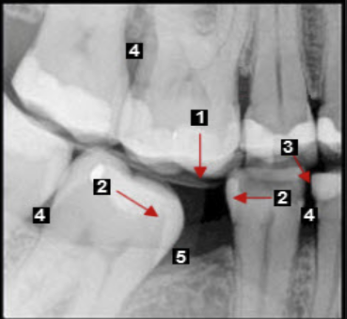
describe what’s being circled
vertical bone loss: furcation involvement
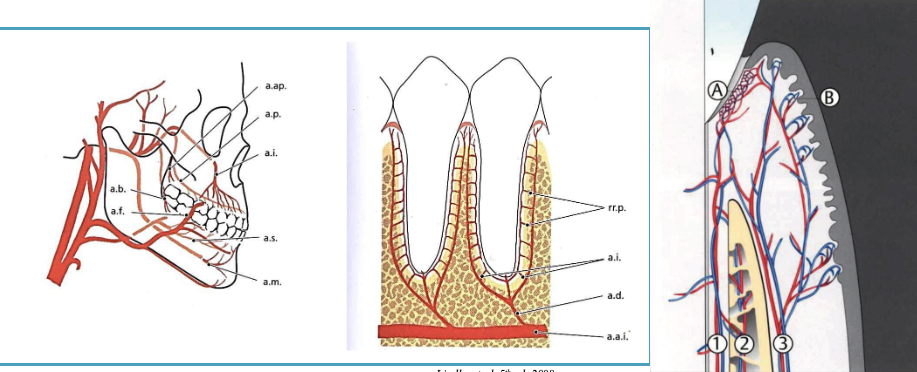
2 functions of the PDL that relate to occlusion
shock absorption
transmission of forces to bone
PDL adapts + remodels to which 2 forces
occlusal + orthodontic forces
normal vs. excessive amount of occlusal load in newtons
70-150 N vs. 300-500 N
normal vs. excessive angle of occlusal load in newtons
axial w/ limited lateral component vs. 30o
5 structures that can be damaged under occlusal load
tooth + restorations
root
periodontium + alveolar bone
masticatory muscles
TMJ
2 effects of occlusal trauma on periodontium
widened PDL space
tooth mobility
what’s the Irving Glickman (Tufts) concept of occlusal trauma
occlusal trauma jiggles the tooth + “pumps” the infection apically along the PDL → vertical bone loss from occlusal trauma + inflammation and horizontal bone loss from inflammation
suggesting occlusal trauma as a co-destructive factor of bone loss

what’s Waerhaug’s concept
occlusal trauma is not a contributing factor to vertical bone loss:
thin bone + inflammation → horizontal bone loss
thick bone inflammation → vertical bone loss
what’s the relationship between active periodontitis + occlusal trauma
occlusal trauma can accelerate existing periodontal disease
acute vs. chronic occlusal trauma
acute: acute injury → toothache, percussion sensitivity, tooth mobility
chronic: chronic overload (ex: bruxism, faulty restorations, insufficient # of teeth) → tooth mobility
primary vs. secondary occlusal trauma
primary: from excessive occlusal forces
secondary: from normal occlusal forces on a weakened (reduced) periodontium
4 histological signs of occlusal trauma
resorption of collagen, bone, cementum
widened PDL
increased mobility
no attachment loss
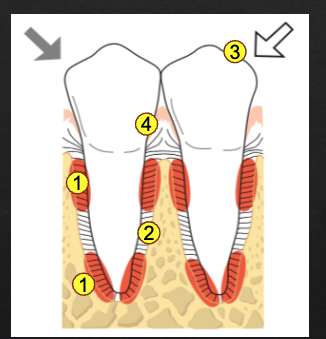
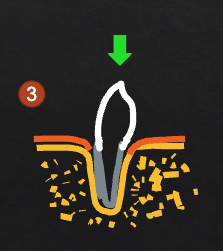
what are the numbers
resorption of collagen, bone, cementum
widened PDL
increased mobility
no attachment loss
Occlusal trauma may be due to:
A. Accidentally biting on a hard object
B. Clenching while asleep
C. Chewing with just a few teeth left
D. All of the above
D. All of the above
Occlusal trauma can cause:
A. Attachment loss
B. Increased mobility
C.Vertical bone loss
D. Tooth loss
B. Increased mobility
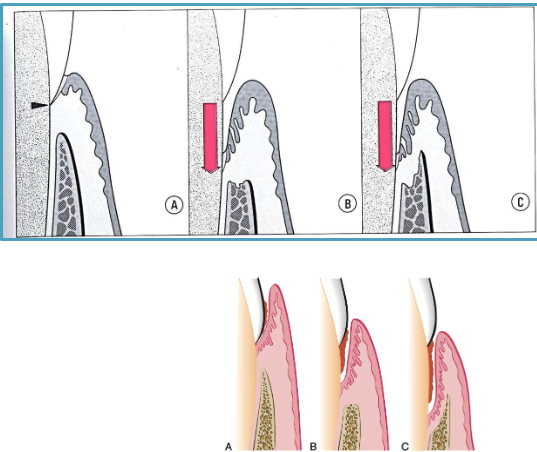
3 stages of tissue response to acute occlusal trauma
stage I: injury
stage II: repair
stage III: adaptation
I R A
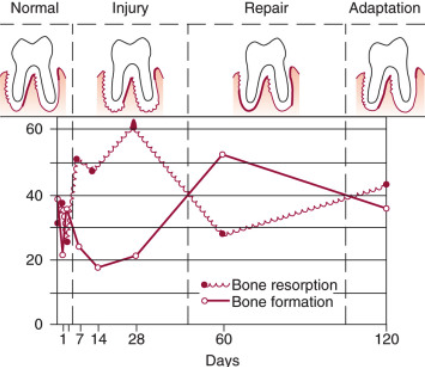
describe what happens during stage I of tissue response to acute occlusal trauma
PDL inflammation (microscopic)
bone resorption (microscopic, not clinical)
widened PDL
increased tooth mobility
describe what happens during stage II of tissue response to acute occlusal trauma
no more inflammation
foundation of new PDL, bone, cementum
describe what happens during stage III of tissue response to acute occlusal trauma
widened PDL + tooth mobility remains
no pocketing/attachment loss
what are the consequences of secondary occlusal trauma
same as primary occlusal trauma (widened PDL + increased mobility) but NO progression in attachment loss
what’s pathologic tooth migration
form of secondary occlusal trauma: normal occlusal forces acting on reduced periodontium → tooth mobility + migration
4 clinical signs of pathologic tooth migration
periodontitis
increased mobility
new interproximal gaps
tooth extrusion

what was the conclusion of Burgett 1992 “clinical trial to assess occlusal adjustment”
occlusal adjustment resulted in minimal but measurable (0.5mm) increase in attachment gain
T/F: tx of periodontitis is necessary + tx of occlusal trauma is of secondary importance
true
T/F: occlusal trauma by itself causes perio attachment loss + bone loss
false
what’s the physiological mobility of teeth under normal forces
100 microns (0.1mm)
T/F: physiological mobility varies from tooth to tooth → larger on single-rooted anterior teeth + less on multi-rooted molars
true
3 factors that determine tooth mobility
height of alveolar bone in relation to length of root: more bone loss = more mobility
width of PDL space: wider PDL = more mobility
shape + # of roots: more + thicker roots = less mobility
what’s the Miller classification
no mobility: <0.1 mm
grade I: 0.1-1mm
grade II: 1mm<
grade III: vertical or twist mobility
T/F: tx of occlusal trauma depends on cause of mobility
true
4 causes of tooth mobility + their tx
occlusal trauma: occlusal adjustment or distribution occlusal forces
periodontal abscess: elimination of cause (SRP/RCT)
periodontitis: STP, splinting for pt comfort
root fracture: EXT
what’s splinting
mechanical stabilization of teeth

when is splinting indicated
for pt comfort on mobile teeth
pathologic tooth migration
guided tissue regeneration on mobile teeth
prosthetics where multiple abutments needed
5 consequences of lack of occlusion
thin PDL
reduction in bone density
supra-eruption
apparent attachment loss
furcation exposure
posterior bite collapse leads to what
super-eruption → root + furcation exposure
molar tipping → pseudopocket (5)
open contact
NCCLs are caused by a combination of which 2 things
abrasion from brushing
chemical erosion due to acidic foods/drinks
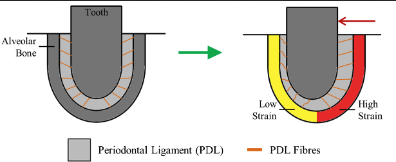
how does the PDL adapt to orthodontic forces
low PDL fiber strain → bone resorption
high PDL fiber strain → bone formation
T/F: orthodontic tx can be done on a periodontitis pt
true, but they must have NO inflammation
what happens to the periodontium if the tooth is moved through cortical bone
creates boney defect (dehiscence)

what happens to the periodontium if the tooth is extruded
bone + gingiva will follow (beneficial for implant planning)

what happens to the periodontium if the tooth is intruded
unlikely to create new attachment; may create deeper pocket
what happens to the periodontium if a molar is uprighted
mesial pocketing can be eliminated; may expose furcation

Tooth #24 can be moved bucco-lingually more than 1mm but not in any other direction. What is the grade of mobility?
A. 0
B. I
C. II
D. III
C. II
Which of the following root exposures is caused PRIMARILY by inflammation?
A. Non-carious cervical lesion
B. Periodontitis
C. Orthodontic extrusion
D. Tooth super-eruption
B. Periodontitis