Kidney 4: regulation of renal blood flow
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Two crucial regulatory systems maintain constant GFR over a wide range of normal systemic blood pressure. What are they?
renal autoregulation— intrinsic, myogenis response, tubuloglomerular feedback. Constriction of afferent and efferent vasculature.
renin angiotensin (aldosterone) system (RAS)— extrinsic
The portion of the distal tubule that sits closely appositioned to the glomerulus contains ______________ cells.
Macula Densa (MD)
What do MD cells do?
detect second-to-second changes in Na+ load within the distal tubule, which is a reflection of changes in GFR.
Na+ load is reduced when tubular flow is reduced.
Autoregulation is an intrinsic system within the renal corpuscle consisting of what two parts?
1. Myogenic response: mostly lowers GFR— afferent smooth muscle constrict
2. Tubuloglomerular feedback: mostly increases GFR—relax/dilate smooth muscle
• together they preserve constant renal blood flow and GFR in the face of alterations in systemic blood pressure
• specialized vascular smooth muscles of the afferent (and efferent) arteriole respond to autocrine factors (? not well-understood)
• moment-to-moment microadjustments of vessel diameter (vasoconstriction) of the afferent arteriole
• crucial in protecting glomerular capillaries against rapid and transient elevations in arterial blood pressure
What response is this describing?
Myogenic response (fast micro-seconds)
What response is fastest, myogenic response or tubuloglomerular feedback?
myogenic (micro-seconds) compared to more than a 20 second response in the tubuloglomerular feedback.
How does the tubuloglomerular feedback work?
• MD cells detect changes in NaCl load (indicating altered tubular flow)
• a decrease in NaCl load indicates low GFR
• microadjustments of vessel diameter (mostly vasodilation) of the afferent arteriole
• crucial in protecting glomerular capillaries against more sustained transient reductions in arterial blood pressure
• mainly acts to raise GFR
__________ may be regarded as the body's temporary
'quick fix' to preserve GFR in the face of transient alterations
in systemic blood pressure
Autoregulation
Autoregulation is ______ sufficient in the face of more chronic
deviations in arterial blood pressure
NOT
The ___________________system is the body's
longerm homeostatic mechanism to maintain renal blood flow
in the face of sustained alterations in arterial blood pressure
renin angiotensin system (RAS)
How long does it take for RAS to activate?
Longer— seconds to minutes
long term sustainability
Where in the renal corpuscle does the RAS system work?
Efferent arteriole
Vasoconstrict the efferent arteriole which causes a build up of back pressure in the gloms that will speed up GFR
The Juxtaglomerular Apparatus is comprised of what two things?
MD cells and granular Juxtaglomerular cells (JG cells) of the afferent arteriole
• note sympathetic innervation of JG cells
JG cells secrete the enzyme renin in response to what three things?
1. MD cells detection of reduced NaCl concentration (↓ GFR)
2. Baroreceptors (reduced stretch)
3. Sympathetic stimulation
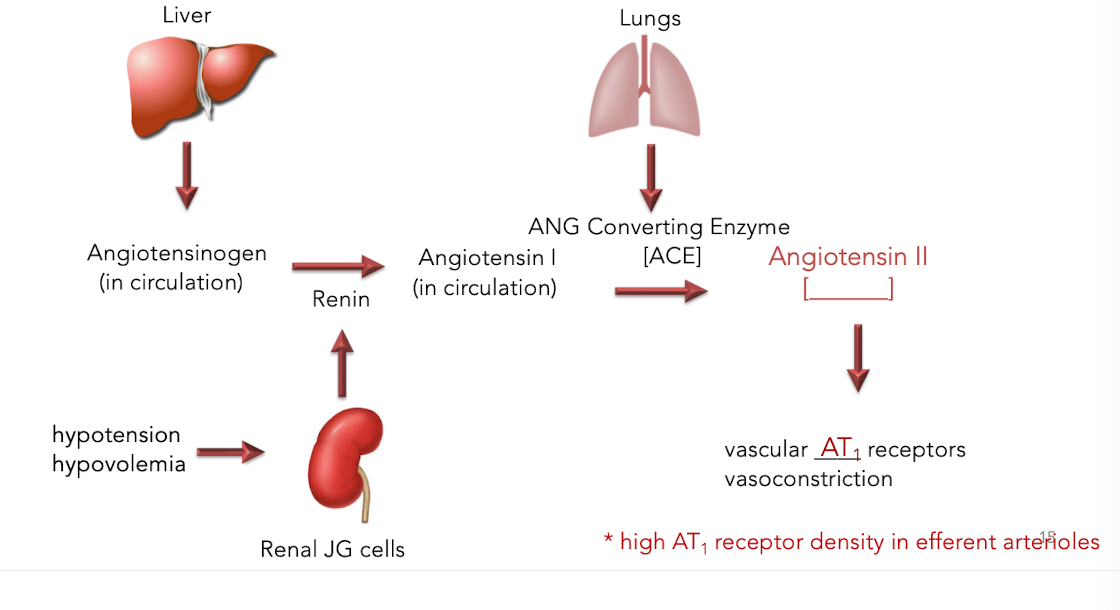
What does the renin secreted by the JG cells do?
converts angiotensinogen from the liver into angiotensin I.
What is the pathway of renin angiotensin system?
How do antihypertensives target RAS?
Together with diuretics, ACE inhibitors [captopril, enalopril] and ARBs [valsartan, losartan] are the front-line treatment for hypertension and congestive heart failure
By opposing the activity of ANGII, ACE inhibitors and ARBs induce systemic vasodilation, thus reducing cardiac load and arterial blood pressure
• ACE inhibitors prevent ANGII synthesis
• ARBs prevent ANGII binding of its cognate AT1 receptor on the efferent arteriole
• net effect: vasodilation of the efferent arteriole= decreased GFR
ANG II signals ____ to vasoconstrict.
ADH aka vasopressin
What is hypovolemic shock? What is the bodies response?
rapid fluid loss results in multiple organ failure due to inadequate perfusion with oxygenated blood.
• Progressively increasing hypotension= signal to constrict
• Tachycardia (sympathetic activation leads to norepinephrine secretion)
• Massive renal secretion of renin leading to very high systemic levels of ANGII
Without an opposing, vasodilatory mechanism, maximal RAS-mediated vasoconstriction could actually shut down blood flow completely, causing ________________________.
ischemic kidney injury and acute kidney injury (AKI)
The inner medulla is hypoxic under normal conditions and is particularly vulnerable to injury in AKI
To circumvent this catastrophe of ischemic kidney injury, ANGII activates _______________ synthesis and secretion in a dose-dependent manner
prostaglandin (PG)
What do prostaglandins do?
PGs vasodilate and combat affects to ANG II to maintain renal blood flow
How does ANG II produce prostaglandins?
stimulates the conversion of arachidonic acid into prostaglandins using the COX1/2
What role do NSAIDs play in the kidney?
NSAIDS (e.g. aspirin, ibuprofen) inhibit pro-inflammatory PG effects by inhibiting COX1/2. Prevents inflammation from prostaglandins but also takes away the battling mechanism against ANG II which is an issue for those experiencing hypovolemic shock. Would cause GFR and medullary blood flow leading to AKI and medullary necrosis.
____________________ are always contraindicated in patients with chronic kidney disease (CKD)
NSAIDS