Anti-arrhythmics
1/59
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
ATP (maintain gradient, energy for muscles), Ca2+
What does the heart need to contract?
Site of origin (SA or ectopic), Conduction (rate, regularity, blockages)
Arrhythmias are caused by 1+ abnormalities in
Ischemia, cardiomyopathy, LVH, Long QT, medications, digitalis toxicity, electrolyte imbalances, increased catecholamines, pulmonary diseases, hypoxia, alcohol
What are some predisposing or exacerbating factors with arrhthymias?
Na+ influx
What is phase 0 in the depolarization of cardiac cells?
Ca2+ influx (L-type)
What is phase 2 in the depolarization of cardiac cells?
K+ efflux (repolarization)
What is phase 3 in the depolarization of cardiac cells?
Na+ channel blockade (decreased automacity)
What does a class I act on
IC > IA > IB (based of association/dissociation speed)
Which class Is are most potent
disopyramide, quinidine, procainamide
What are the IAs (double quarter pounder)?
lidocaine, mexiletine, tocainide
What are the IBs (lettuce, mayo, tomato)?
Flecainide, propafenone
What are the ICs (Fries please)?
Decrease sympathetics and ectopic automaticity, decrease conduction rate, prolongs refractory period, inhibits phase 0, decrease the heart rate
What is the MOA for class II anti-arrhythmics?
atrial tachyarrythmias, prevention, decreases mortality post-MI
What are the class IIs used for?
Beta blockers
What are the class IIs?
blocks K+ channel (prolongs phase 3)
What is the MOA for the class IIIs?
Amio, dronedarone, ibutilide, dofetilide, sotalol, bretylium
What are examples of class IIIs?
calcium channel blockade (depresses action potential, slows AV node conduction)
What is the MOA for the class IVs?
dilitiazem, verapamil (no DHPs since reflex tach is what we’re NOT trying to do)
What are examples of class IVs?
Amio (III, IA, II, IV), Sotalol (II, III), Digitalis, Adenosine, Vernakalant (I, III, IV)
What are the special anti-arrhythmics that kinda break the Vaughan Williams Classification system?
His/Purkinje fibers, contractile tissue
The fast action potentials (which depend on Na+) are found where?
SA/AV nodal tissue
The slow action potentials (the ones that rely on calcium) are found in
Bind to A receptor, hyperpolarized (open K+ channel), dilate coronaries
What is the MOA for adenosine?
PSVT
What is adenosine used for
onset in 10-30 sec, IV only, t1/2 less than 10 seconds (broken down by RBCs)
Tell me about adenosine
dyspnea, flushing, bronchoconstriction, burning chest sensation
ADRs for adenosine that no one cares about because they last like 10 seconds
acts on K+Na+ATPase on myocytes (increase vagal tone, decrease ventricular rate)
What is the MOA for Digoxin?
arrhythmias, fatigue, weakness, anorexia, NVD, dizziness, green/yellow visual color disturbances, DDI
What are the ADRs for digoxin?
anticholinergic (use the tachycardic effect to treat brady)
What is the MOA for atropine
blurred vision, dry mouth, constipation, urinary retention
ADRs for atropine
Amio
What is the most effective anti-arrhythmics drug for atrial and ventricular arrhythmias - used for V tach and V fib?
~53 day t1/2 (loading dose), huge Vd (super lipophillic), CYP3A4 inhibitor
Tell me about Amio
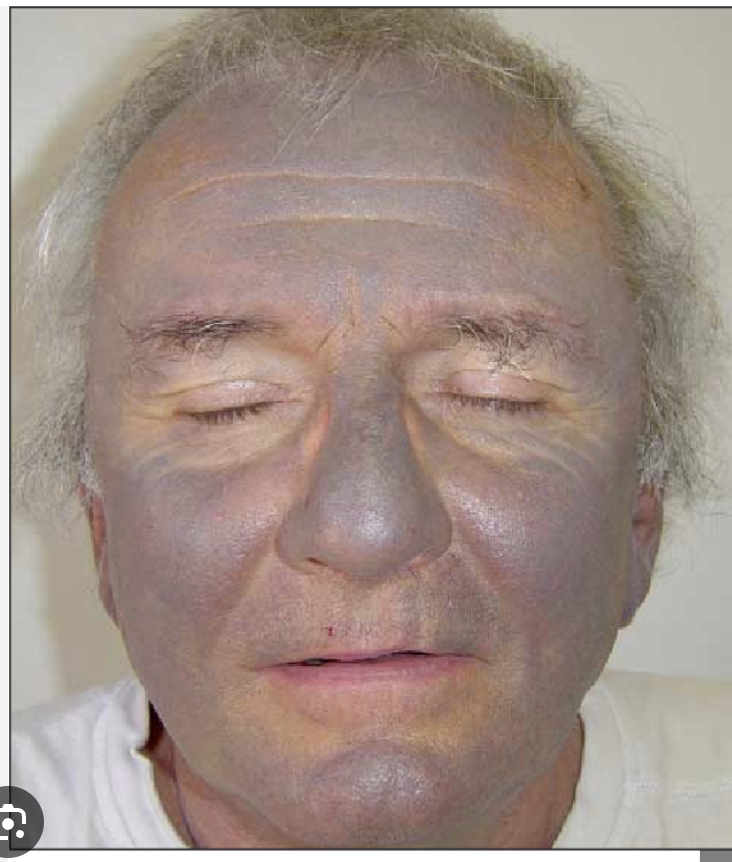
hypotension, decrease HR, heart block, pulmonary fibrosis, thyroid abnormalities, (iodine), corneal deposits, blue skin discoloration, peripheral neuropathy, photosensitivity, hepatotoxicity
ADRs of Amio
Dronedarone
So scientists being scientists decided to take the iodine out of amio and mod it so it’s less toxic - what did they end up with?
t1/2 24 hours, inhibits 3A4 and 2D6
Tell me about dronedarone?
prolongs QT, increase mortality in A fib
ADRs for dronedarone
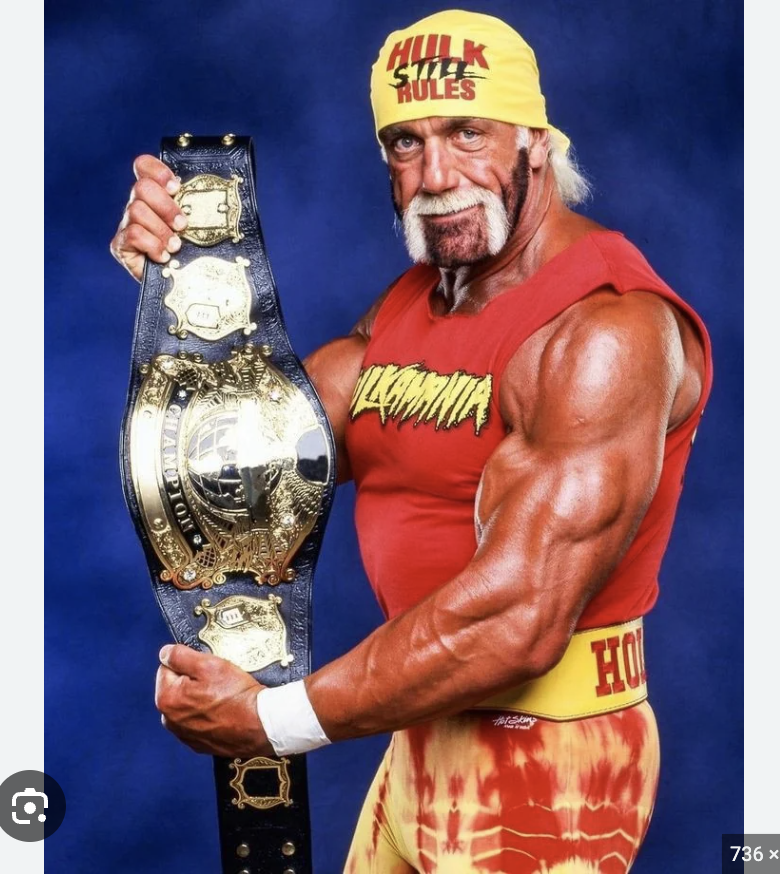
Potential to cause serious arrhythmias especially Vtach or Vfib (Hell yeah brother)
What is the down side to all anti-arrhythmics?
IAs, Sotalol, IIIs, macrolides, fluroquinolones, psychotrophics, terfenadine, astemizole, 5HT3 antagonists, methadone
What are some examples of drugs that prolong QT (block HERG channels)?
prolonged QT
What is the ADRs for ALL IAs?
cinchonism (tinnitus, HA, psychosis), cramping, decrease BP, increase chance of digitalis toxicity, most potent 2D6 inhibitor on the planet, anti-cholinergic
ADRs for Quinidine (specifically)
lupus like syndrome
ADRs for Procainamide (specifically)
negative inotrope, anticholinergic
ADRs for Disopyramide (specifically)
tremor, AMS, Seizures (at high IV doses)
ADRs for Lidocaine
pulmonary fibrosis, agranulocytosis
ADRs for tocainide
heart failure, pro-arrhythmic
ADRs for ICs
hypotension, brady, AV block
ADRs for class IIs
short onset, short t1/2, short lived ADRs
Tell me about esmolol
torsades
ADRs for sotalol (specifically)
V tach
ADRs for ibutilide and dofelitide
complete AV block, negtive inotropic, constipation (verapamil)
ADRs for class IVs
ventricular arrhythmia, torsades, brady
ADRs for Vernakalant
A fib
What is multiple foci of reentrant pathways that cause rapid and disorganized atrial depolarization (atria having a party, ventricular not invited, AV node is the bouncer)?
cardiovert if unstable, AVN blockers to control ventricular response rate, Prophylactically give anti-thrombotics (warfarin, DOACs, etc), rate vs. rhythm control
What are the treatment approaches to A fib?
minor skin burns, post-cardiovert arrhythmia, emboli (give blood thinners beforehand)
What are the ADRs for cardioversions?
Digoxin (not super effective - use with concurrent HF), CCBs, beta blockers (esmolol for acute, propanolol/metoprolol for maintenance), Vernakalant (atrial selective)
What AV node blockers can we use for rate control in A fib
elderly, concurrent CV disease
Which peeps should we probably rate control
symptomatic despite rate control,
Who we should we consider rhythm control in?
Ibutilide (watch your QT)
What medication is approved for the conversion of stable, recent onset Afib/flutter?
dofetilide (watch QT, long term use) Amio, ICs (proarrythmic)
What medications other than ibutilide can be used for chemical cardioversion?
dofetilide, amio, sotalol (anything more than 320 causes torsades)
What medications can we use for the maintenance of normal sinus - reserved for symptomatic recurrent Atrial fib?
no (may increase mortality)
Do we treat each and every PVC?