Feeding tube placement
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms

Naso-oesophageal Tube placement - Equipment (image of NO tube)
Soft rubber (preferably silicone) nasogastric tube
Local anaesthetic drops (used in the eye) - proxymetacaine
Water-soluble lubricant
Gloves
Tissue glue
Elastoplast
Syringe and sterile water
Pen

Naso-oesophageal tube placement
Measure the tube between 7-9th rib and mark the length
Administer local anaesthetic into the nose
Insert the feeding tube ventro-medially into the nostril
Check placement
Secure in place

Naso-oesophageal tube placement - Measurement
Make sure the tube is sat in the oesophagus not through the pylorex sphincter - can get reflux of stomach acid
Mark with pen or tape
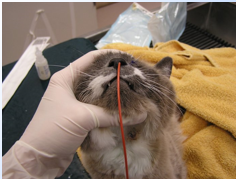
Naso-oesophageal tube placement - Local anaesthetic
Local into the nose → Tilt head back with nose towards the sealing
Goes down the nasal cavity
Wait for this to work (5-10 mins)

Naso-oesophageal tube placement - Aim vento-medial direction
If there is resistance, stop and try again
Swallowing indicates correct placement
Once the marker has been reached, check the placement
Draw back with empty syringe - negative pressure = in oesophagus, instill sterile water
If in the wrong place = coughing

Securing naso-oesophageal tube
Comfortable - tape not interfering with vision
Can use tape, glue or sutures to hold in place

Oesophagostomy placement - Equipment needed
Anaesthetic equipment
Clippers
Surgical scrub/spirt
Long curved arty forceps
Scalpel blade and handle
Suture material, needle and needle holders
Tube of suitable size

Oesophagostomy feeding tube placement
Surgically prep the area - measure the tube
Measure the feeding tube to the 7th to 8th intercostal space and mark the length
Placed curved artery forceps into the mouth and down the oesophagus - incise over the end of the forceps
Grip the end of the feeding tube with the forceps through the incision and draw this out through the mouth
Redirect the feeding tube down into the oesophagus until it reaches the marker made
Secure in place with a Chinese fingertrap suture
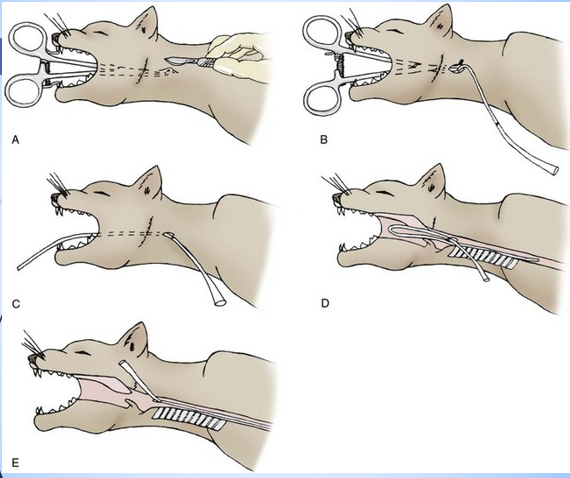

Oesophagostomy placement
A ‘special vet’ is available for use costing around £200; Van Noort Technique
The Van Noort set makes the procedure easier as the tube is introduced into a sheath directly into the oesophagus in the right direction from the start
This means it doesn’t need redirecting from the mouth
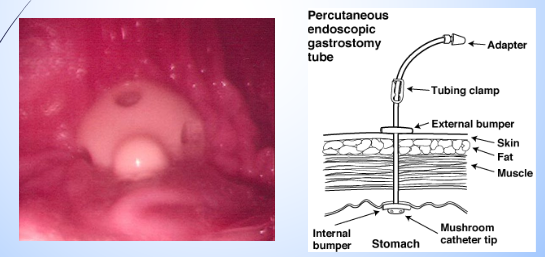
Gastronomy placement
Patient positioned in right lateral
Endoscope used to to into the stomach - pushed against the stomach wall and light seen externally
Placed on the left-hand side

Jejunostomy tube
Not frequently used
Used where the upper GI tract needs to be bypassed
Needs to be on a constant rate infusion (CRI) as no holding capacity in the jejunum like there would be in the stomach
Must be a liquid diet
Suffer from diarrhoea with this as its not fully digested, difficult to meet energy requirements
Minimum 4-day placement
Feeding tube care
Patient must wear a buster collar
Care of stoma site
Flush the tube before and after each meal
If blockages - flushing with carbonated drink or flush and suction with warm water
Keep tube clean
Ensure correct RER calculated
Gradual feeding 1st 3 days
Ensure food is appropriate and warmed or at room temperature
Do not allows dried food to accumulate around the opening
The feeding tube will be dressed with a non-adhesive dressing, this needs to be ..
Changed daily and cleaned with chlorhexidine - wear gloves and hand hygiene
Why is flush used when caring for the feeding tube?
Check the placement
Prevent blockages
May need replacing
We should ensure that the food is the correct consistency to put down the tube, it may be necessary to add more water to some diets when using smaller tubes. However, what must be taken int account if doing this?
The loss of nutritional valve when adding more water, making more meals necessary per day to give the patient the correct RER

Complications
Tube obstruction
Premature tube removal or dislodgement by patient
Food contamination
Vomiting
Diarrhoea
Site infection
Peritonitis
Electrolyse changes
Refeeding syndrome
Refeeding syndrome - patients at risk
Anorexic >3-5 days
Metabolic condition (diabetic ketoacidosis or hepatic lipidosis)
Metabolic disturbances due to nutrition being reinstated
Refeeding syndrome
Get metabolic disturbances due to reinstitution of nutrition
Change from protein digestion (catabolic state) to carbohydrate digestion (anabolic state)
Shift of electrolytes leading to clinical signs
Go from protein digestion for energy - catabolic state to carb digestion - anabolic state
Releases insulin and causes electrolytes and glucose to shift from extracellular space to intracellular space - shift of electrolytes
Muscle weakness, cardiac arrhythmias, respiratory depression, haemolysis and death
How to avoid refeeding syndrome
Recognise ‘at risk’ patients
Do not exceed RER → feed 1/3 day one, 2/3 day two and full amount day three/four. Monitor patient closely!
Feed high fat, low carb diet is patient has not eaten from more than 5 days
Monitor phosphorus, potassium, magnesium and PCV/TS twice daily
Supplement electrolytes if needed (IV or oral)
Monitor patient closely

Parental nutrition
Parental nutrition is the provision of an animals nutritional requirement intravenously
It use is becoming more common in referral veterinary hospitals
Usually use a central line
Central catheter is used i.e. Jugular catheter
Possibility of septicaemia so good sterile catheter care is essential
Good care of catheter site and environment needed - food prime for bacterial growth is contaminated

If the patient is on parental nutrition , what must they have done?
Blood samples need to be taken tice daily perhaps more often depending on the patients condition and checked for blood glucose, acid base and biochemistry
Partial parental nutrition
It is difficult to meet the total energy requirements, so often Partial parental nutrition is used rather than total parental nutrition
What is parental nutrition comprised of?
Solutions of sugared, fatty acids and amino acids are used all of which are highly osmotically active so they can only be ‘tricked’ in - must be on a CRI