Atrial Dysrhythmias: PACs, PAT, SVT, A Flutter, A Fib
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
94 Terms
Atrial Dysrhythmias
A dysrhythmia is any disturbance in the normal cardiac conduction pathway (P-QRS-T).
Ectopic Focus
An abnormal place in the atria, other than the sinus node, that initiates an impulse.
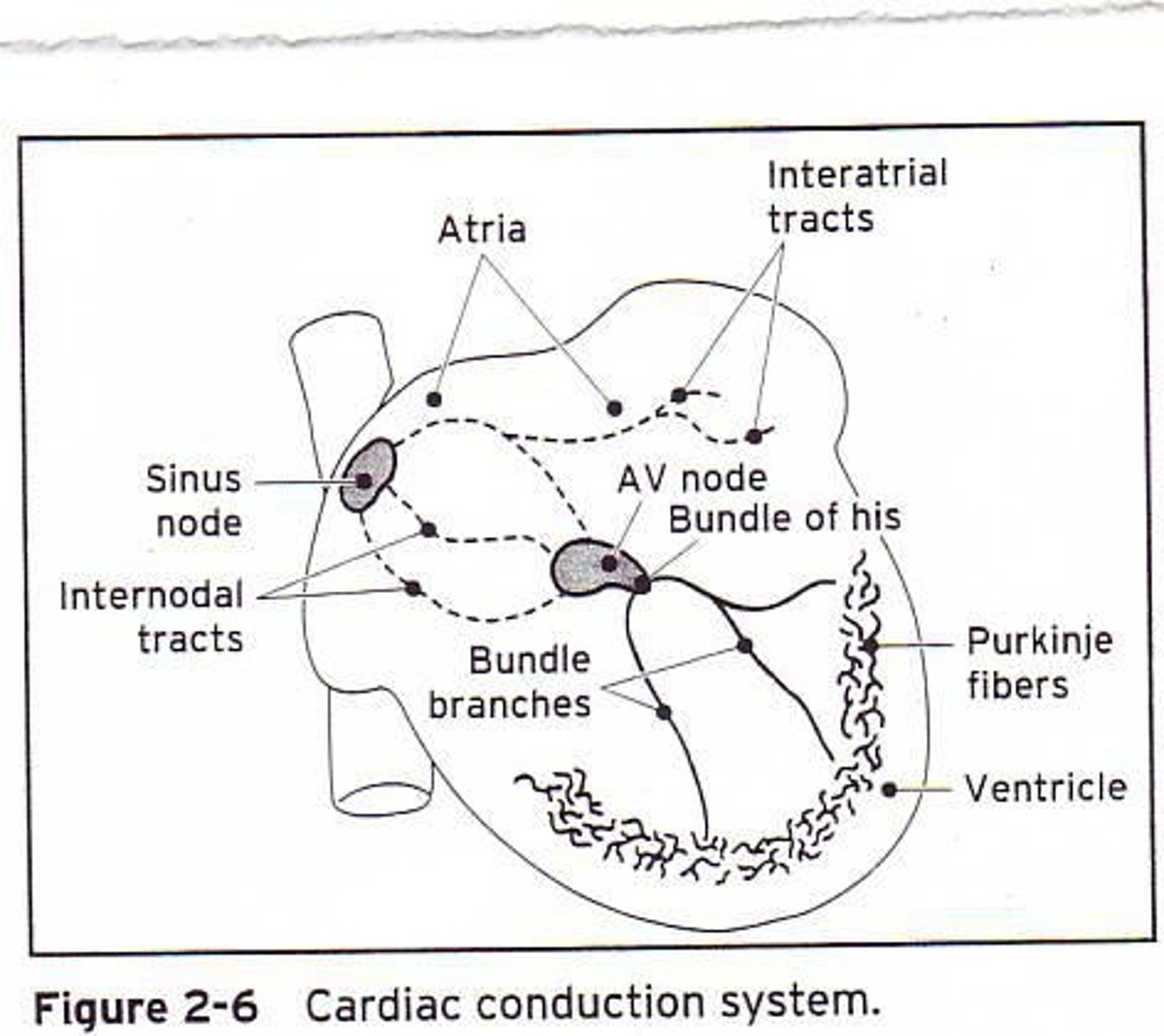
Normal Conduction Pathway
SA node begins the impulse, followed by the AV node, Bundle of His, Bundle Branches, and Purkinje Fibers.
Automaticity
The unique ability of the heart to self-generate an electrical impulse.
Premature Atrial Contraction (PAC)
Isolated, early beats from an ectopic focus in the atria, usually interrupting a regular sinus rhythm.
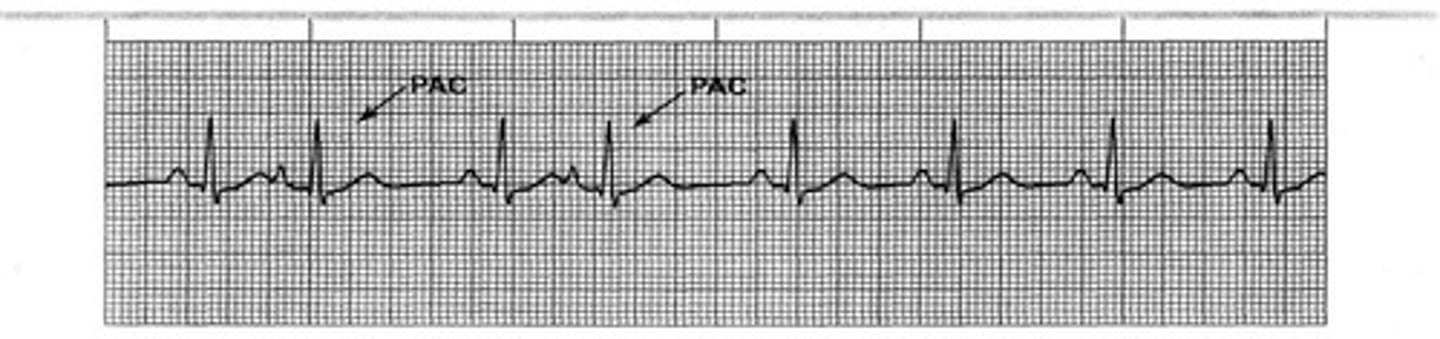
P-wave in PAC
May be inverted, hidden in T-wave, or have different morphology than the normal sinus impulse.
PR-interval in PAC
May be longer, shorter, or the same as the PR-interval of a sinus impulse.
QRS shape in PAC
Typically produces normal QRS or narrow QRS complex; depends on the health of the AV node, Bundle of His, & Bundle Branches.
PAC triggers
Can be accentuated by nicotine, caffeine, ETOH, strong emotions, myocardial ischemia, mitral valve prolapses, heart failure, and medications.
Electrolyte imbalances in PAC
Low potassium & low magnesium can predispose individuals to PAC.
PAC Treatment
No treatment is necessary in many cases; eliminate exposure to irritable conditions and manage underlying health issues.
Heart Palpitations in PAC
May be felt by the patient due to the interruption of the RR interval.
Rhythm in PAC
Underlying rhythm is regular but becomes irregular when PAC occurs.
P wave in PAC
Present, may be hidden in T-wave, or have a different shape.
PR interval in PAC
Varies in the PAC.
PAC occurrence
Can occur in individuals with normal hearts.
PAC and Myocardial Health
Recent MI may still present with PAC even with treatment.
Digoxin
New medication may need adjustment in patients with PAC.
PAC and Alcohol
Stopping/reducing alcohol consumption is recommended for PAC management.
PAC and Caffeine
Reducing caffeine consumption can help manage PAC.
PAC and Tobacco
Stopping tobacco consumption is advised for individuals experiencing PAC.
PAC and Emotional Stress
Alter emotions to reduce PAC occurrences.
Paroxysmal Atrial Tachycardia (PAT)
Sudden burst of 3 or more PAC's that becomes the rhythm for a short time.
Paroxysmal
Rhythm that starts and stops suddenly.
Causes of PAT
Emotions, nicotine, ETOH, caffeine, acute MI, and medications like digitalis.
Symptoms of PAT
May experience lightheadedness and palpitations, depending on the heart rate and duration.
Initial Rhythm of PAT
PAT usually begins with a PAC.
PAT Rate
Faster than sinus tachycardia with a rate of 160-250.
P Waves in PAT
P waves present but different than sinus P wave; can also be hidden in the T-wave.
PR Interval in PAT
PR interval is .12-.20 sec.
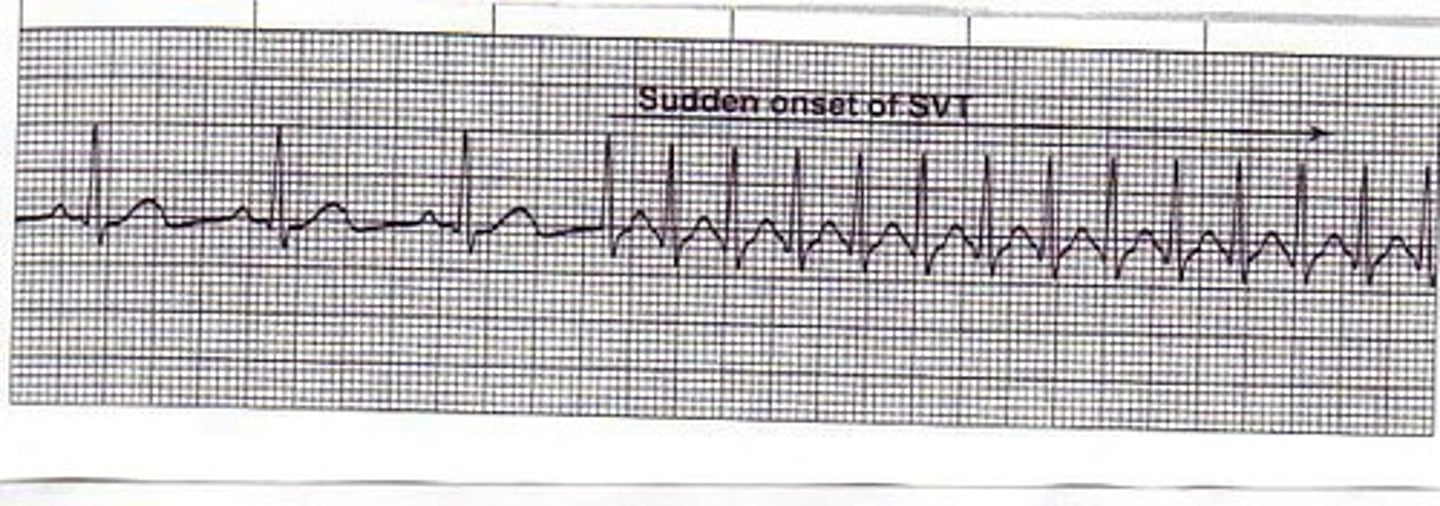
Supraventricular Tachycardia (SVT)
Describes a rapid, sustained atrial tachycardia when the mechanism is unknown.
Origin of SVT
Dysrhythmia that originates above the AV node.
Examples of Dysrhythmias Included in SVT
Sinus tachycardia, atrial flutter, atrial fibrillation.
CO Formula
CO = HR x SV.
Effects of Increased Rate in SVT
Decreases stroke volume, reduces diastolic fill time, and less coronary artery fill time.
SVT Rate
Rate is >130.
Rhythm in SVT
Regular and sustained; does not stop.
P Waves in SVT
Not identifiable; too fast and hidden in the T-wave.
PR Interval in SVT
Cannot be measured in the SVT portion.
QRS Duration in SVT
QRS < .12 narrow and very fast.
Adverse Effects of SVT
Decreased CO and hypotension.
SVT Treatment Focus
Directed towards heart rate reduction.
Valsalva Maneuver
First attempt to lower the heart rate.
Carotid Massage
Next attempt to lower heart rate; discouraged in the elderly due to increased stroke potential.
Adenosine
Medication that stops all electrical activity of the heart for 10 seconds.
Electrical Cardioversion
Delivery of an electrical shock on the 'R-wave' to convert the current dysrhythmia back to the normal QRS cycle.
Synchronized Cardioversion
Utilized to avoid shocking during the vulnerable repolarization phase of ventricular activity.
Shock Delivery in Cardioversion
Usually 200 joules delivered on the QRS complex.
Atrial Flutter (A Flutter)
A supraventricular tachycardia characterized by an atrial rate of around 300 beats/min.
Reentry Circular Pathway
Requires a reentry circular pathway around the SA node.
A-flutter ECG Recognition
Recognized on the ECG by the 'Sawtooth' atrial pattern.
F-waves
The sawtooth-shaped atrial waves are called 'F-waves' flutter waves.
AV Node Function
AV node fails to allow conduction of all atrial impulses to the ventricles (AV node acts as gatekeeper).
Ventricular Conduction Rate
Results in either a 2:1, 3:1, or 4:1 ventricular conduction rate.
Ventricular Response Rate (4:1)
Slower in 4:1 (75 beats/min) versus 2:1 (150 beats/min).
Atrial Rhythm
'F' flutter waves are regular, P waves are NOT present.
PR-Interval
Not measurable.
Atrial Rate
250-300 beats/min.
Ventricular Rhythm
Regular 4:1.
QRS Duration
QRS < .12 all usually.
A Flutter vs A Fib
A Flutter is regular due to the 4:1, 3:1, 2:1 ratio, while A Fib will be irregular.
Rapid Ventricular Rate (RVR)
Can decrease Cardiac Output (CO) and cause hypotension.
Atrial Kick Loss
Loss of 'Atrial-Kick' because the atrial contraction is not occurring (losing 20% of stroke volume).
Thrombi Formation
Without atrial contractions thrombi can form on the walls of the atria.
Pulmonary Embolus (PE)
Thrombi breaking off and going directly into the pulmonary circuit.
Cerebral Embolus (Stroke)
Thrombi can lead to a cerebral embolus.
Myocardial Infarction (MI)
Can occur from emboli.
Precursor to Atrial Fibrillation
Almost certainly a precursor to Atrial Fibrillation if left untreated.
Treatment Goal
Convert back to normal sinus rhythm (NSR) or achieve ventricular 'rate-control' (i.e. keep the HR <100).
Amiodarone
A chemical converter that helps to convert to Sinus Rhythm and control ventricular response.
Rate Control Medications
Beta-Blockers, Calcium Channel-Blockers, and digoxin control AV node and rate control.
Anticoagulation
Needed for long-term management, especially if we can't stop the A flutter.
Atrial Fibrillation (A Fib)
Is a rapid atrial ectopic rhythm occurring with an atrial rate of 350-500 beats/min.
P-waves in A Fib
Appear small, quivering fibrillatory waves.
Loss of atrial kick
Results in a 20% decrease in stroke-volume from the atria to ventricle.
Ventricular response (QRS) in A Fib
Is typically 'irregularly irregular'.
Ventricular response rate
Characterized as rapid (>100 beats/min) or controlled rate (<100 beats/min).
Conditions commonly associated with A Fib
Include heart failure, ischemic or CAD, pulmonary disease, after open heart surgery, and severe mitral valve disease.
Atrial Rhythm in A Fib
'P-waves' are indiscernible.
PR-interval in A Fib
Can't be measured.
Atrial rate in A Fib
350-500 beats/min.
Ventricular Rhythm in A Fib
Irregular RR intervals.
QRS duration in A Fib
<.12.
Goal of A Fib treatment
To convert back to normal sinus rhythm (NSR) or achieve ventricular 'rate-control' (i.e. keep the HR <100).
Amiodarone in A Fib treatment
Helps to convert to SR and control ventricular response.
Medications for AV node control
Include beta-blockers, calcium channel-blockers & digoxin.
Immediate treatment for symptomatic A Fib
May require immediate synchronized cardioversion.
Transesophageal Echocardiography (TEE)
Needed prior to cardioversion to rule out a clot in the atria.
Anticoagulation in A Fib
Heparin drip is needed during the acute phase.
Long-term anticoagulation for chronic AFib
Needed to prevent a stroke resulting from a tendency to form thrombi from the quivering action in the atria.
Coumadin (Warfarin)
Requires INR monitoring.
Xarelto (Rivaroxaban)
Used long-term to prevent embolic events with fewer adverse effects than Warfarin.
Ablation therapy
Uses radiofrequency energy to cause targeted localized cardiac lesion.
Effect of successful ablation therapy
Can prevent the initiation of the dysrhythmia ectopic area and disrupt the conduction pathway.