GI 6: Small + Large Intestine Motility and Secretion
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
Physiological anatomy of small intestine
− mucosa of the intestine is organized into finger-like villi with the associated villus crypts (between adjacent villi)

Villi
projections into the lumen
- covered predominantly with mature, absorptive enterocytes
o Function: absorption
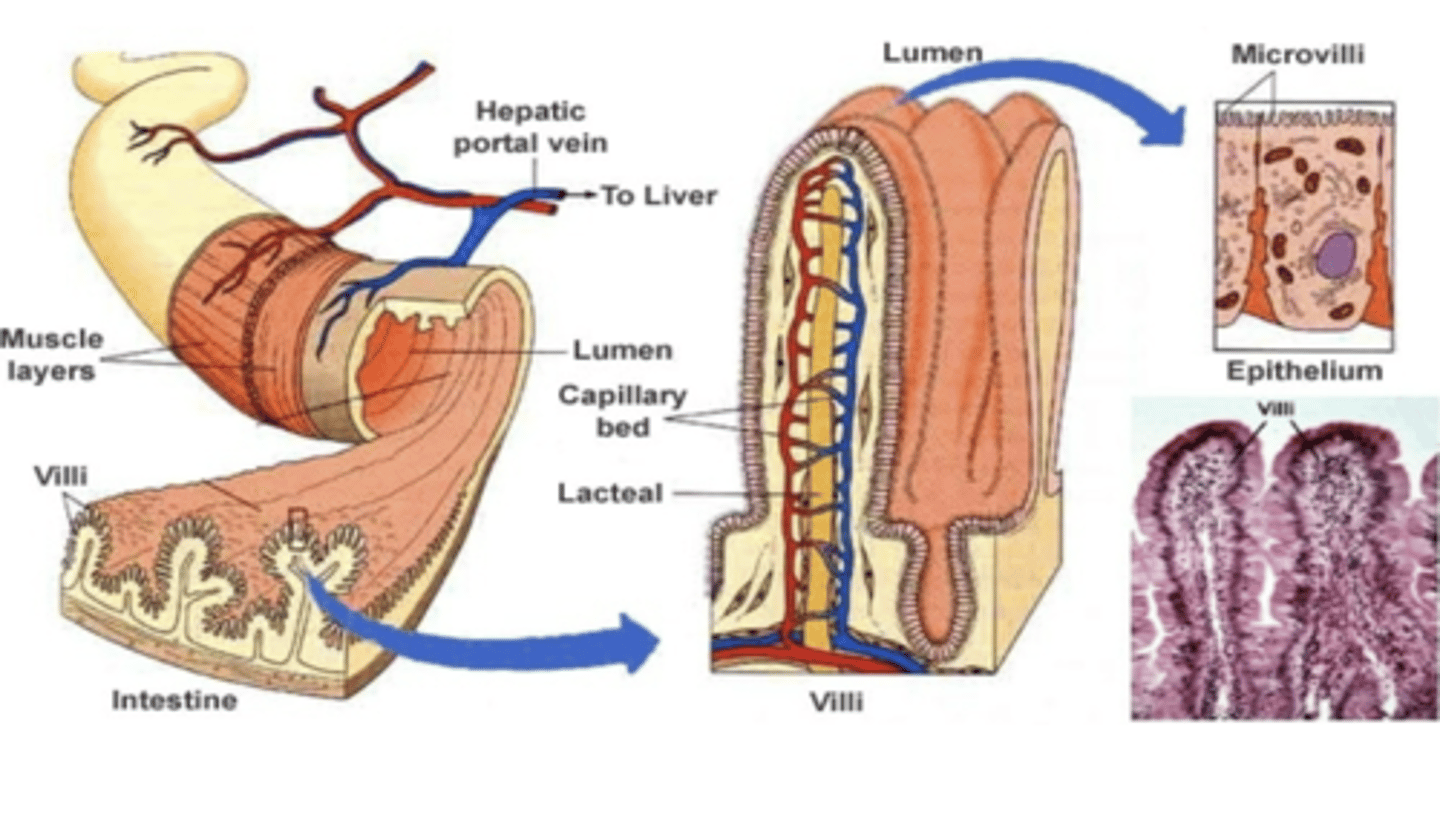
Crypts (of Lieberkuhn)
tubular invaginations in the epithelium around the villi
- lined largely with younger epithelial cells, which are involved primarily in secretion
- at the base are stem cells, which continually divide and provide the source of all the epithelial cells
SI Secretion
Secretion of fluid and electrolytes into the intestinal Lumen
- carried out mainly by cells located within the Crypts of the mucosa
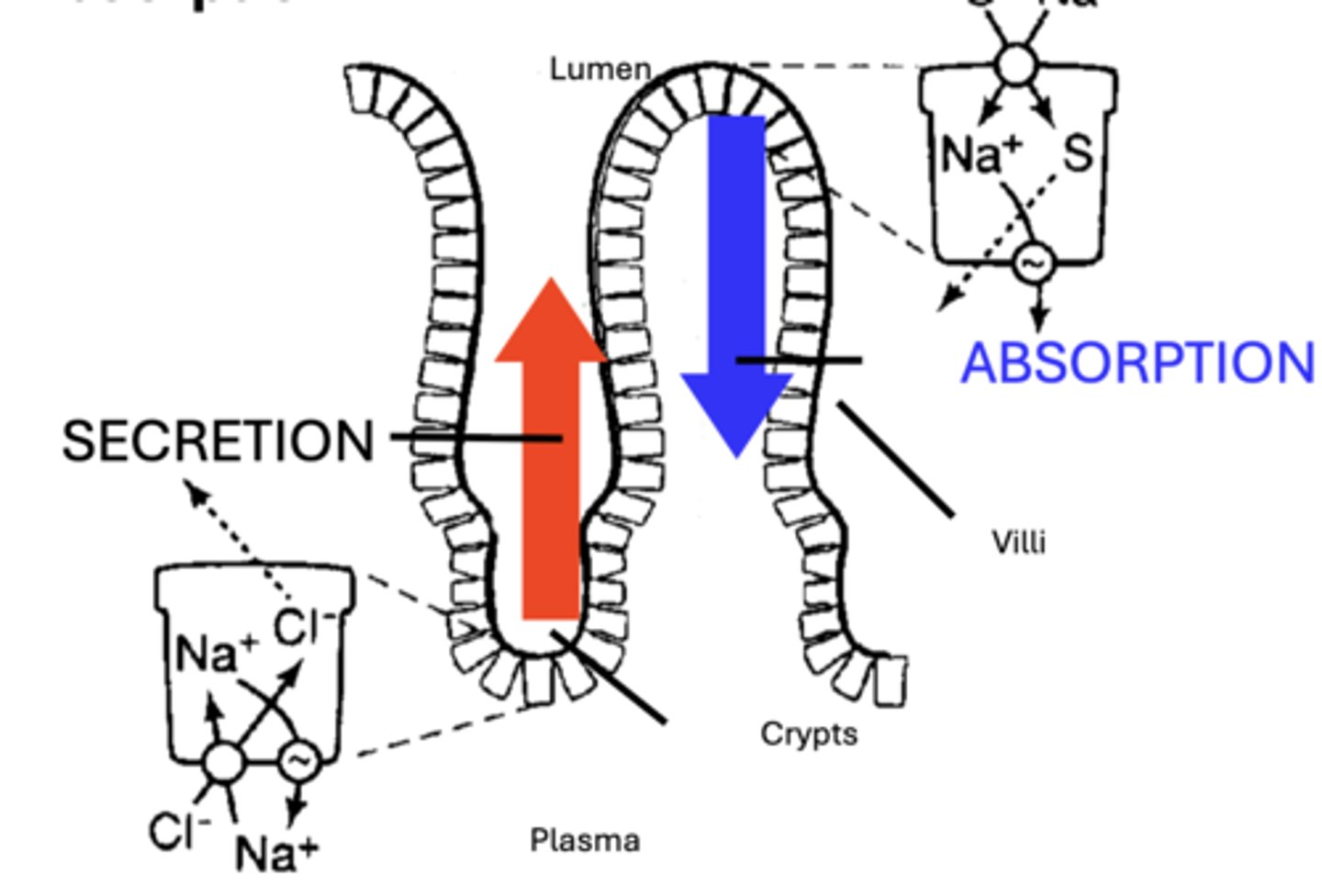
SI Absorption
Absorption from the Lumen into the Plasma
- performed primarily by enterocytes located within the upper 2/3 of the Villus
Secretions of small intestine
• 1-2 L/day of intestinal juice
• Secretions are typically Isotonic and slightly Alkaline due to a relatively high HCO3- component
Composed mainly of:
• H2O
• Electrolytes (Na+, K+, Cl-, HCO3-)
• Mucus
Secretions of Colon
secretes a similar, but lower volume (0.2 L/day) fluid as compared to the SI
• generally richer in Mucus
• possess higher concentration of K+ & HCO3-
Functions of Intestinal secretions
1. Maintain Chyme Fluidity
- facilitates digestion, absorption & motility
2. Play a role in diluting ingested noxious agents & microorganisms
3. High HCO3- aids in Buffering
- Acid Chyme (sm. intestine)
- bacterially produced acids (colon).
4. Mucus component protects the intestinal lining from mechanical abrasions
Regulation of secretions of small intestine
major physiological stimuli of intestinal secretions:
- tactile stimulation of mucosal cells
- distension of the intestinal wall
• most secretions are normally reabsorbed by the intestines themselves
Toxins effect on secretion
Clinically, a few toxins (e.g. Cholera toxin) may greatly stimulate intestinal secretion to levels that exceed the reabsorptive capacity of the intestines
- causes production of a watery diarrhea that can lead to dehydration, electrolyte imbalance and perhaps death
Components of Intestinal Secretion: SI
• 1-2 L/day
• H2O
• Na+, K+, Cl-, HCO3-
• Mucus
• Alkaline
• Isotonic
Components of Intestinal Secretion: Colon
• Similar Sm. Int.
• 0.2 L/day
• ↑ Mucus
• ↑ K+; HCO3-
Overview of Secretion Function and Regulation
Function:
• Chyme Fluidity:
- Dig./Absorp.
- Motility
- Dilute Toxins
• Abrasion
• Acid Buffer
Regulation:
• Tactile (Mucosa)
• Distention (Wall)
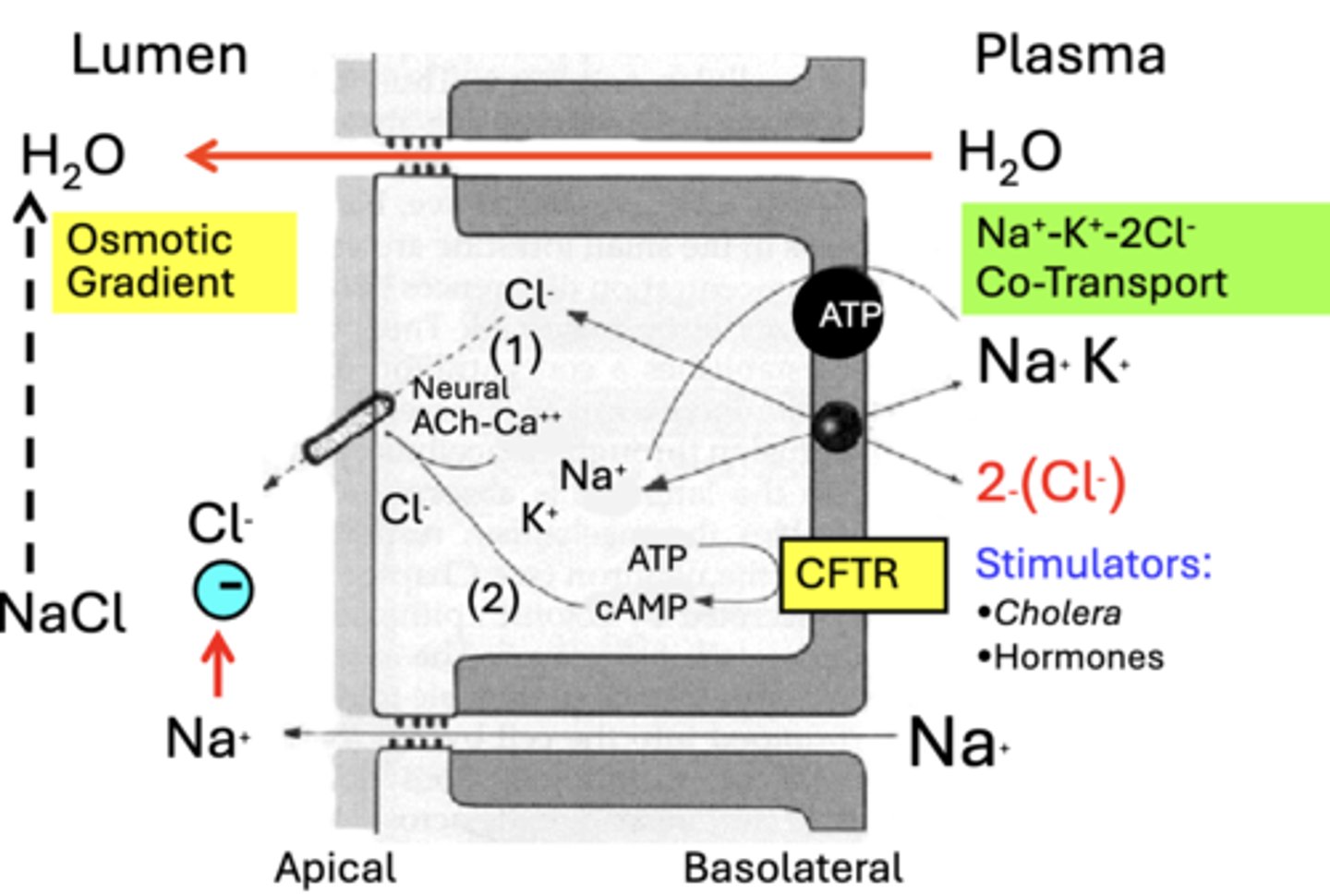
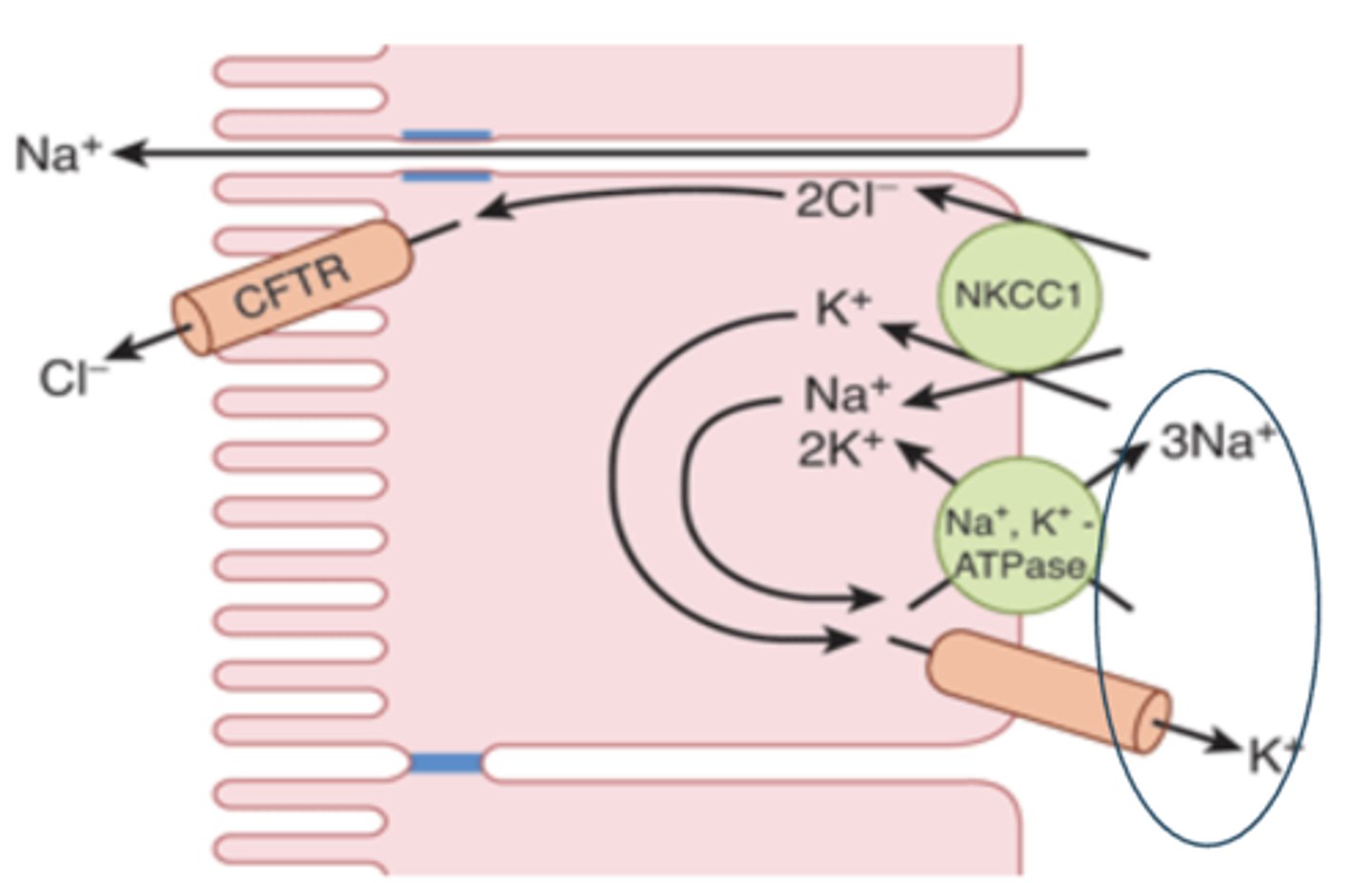
Chloride secretion
- Cl– normally enters enterocytes from the interstitial fluid via Na+–K+–2 Cl– cotransporters in their basolateral membranes
- secreted into the intestinal lumen via channels that are regulated by various protein kinases
Chloride Apical Fluid Secretion
Cl- transport across the Apical membrane occurs through two types of Cl-Channels:
1. Cl- channel activated via a cAMP-dependent phosphorylation pathway
2. Cl- channel activated by increased intracellular Ca++ levels (Ca++)
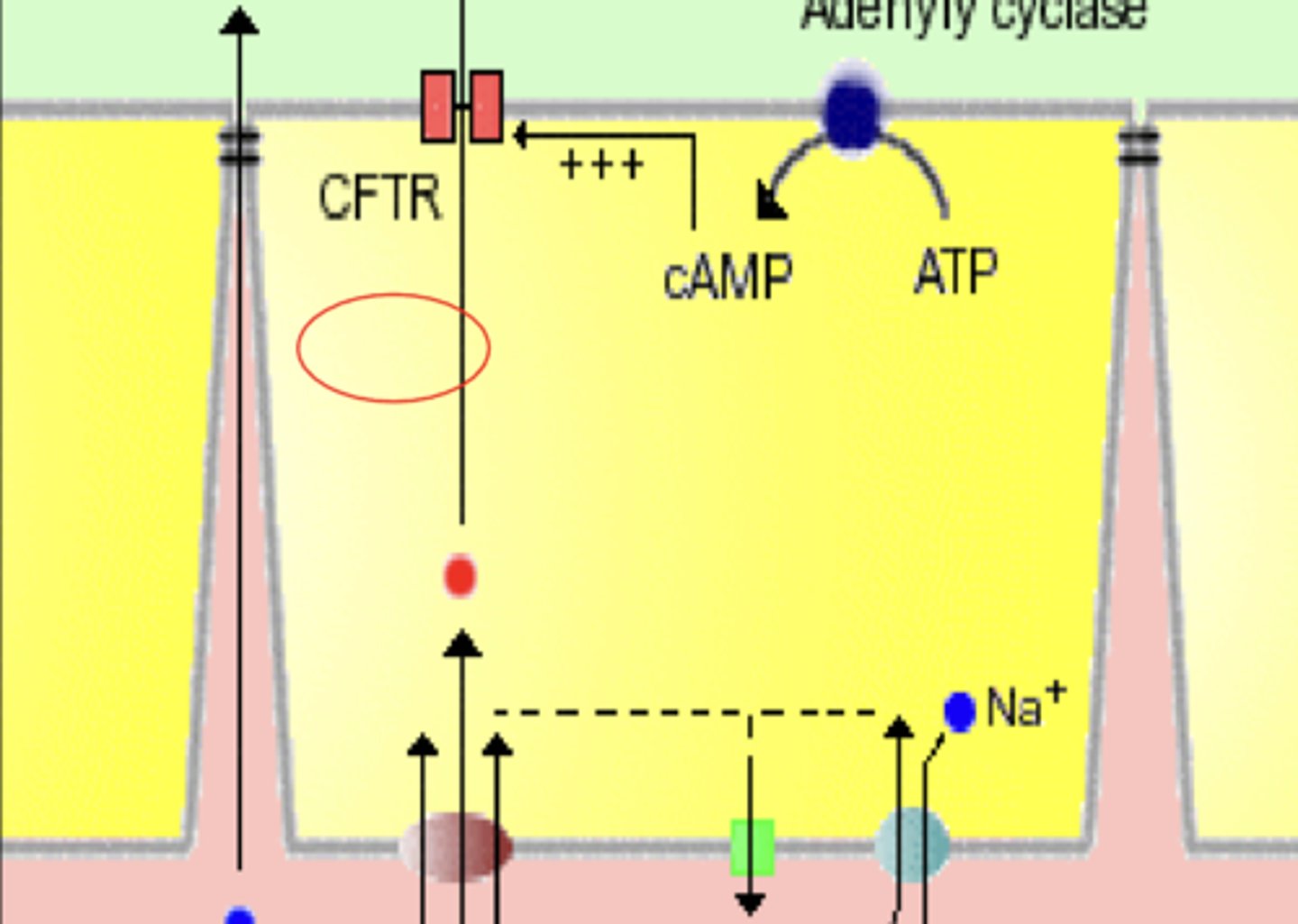
CTFR
Cystic Fibrosis Transmembrane Conductance Rectifier
- Cl- channel activated via a cAMP-dependent phosphorylation pathway
- stimulated by a variety of secretagogues, including Cholera toxin and a number of Hormones
found:
- salivary glands
- pancreatic ducts
- pulmonary airways
- implicated in Cystic Fibrosis
Cl- channel activated by increased intracellular Ca++ levels (Ca++)
- Parasympathetic Neural stimulation of intestinal fluid secretion acts through activation of this type of Cl- channel
- Stimulation is mediated by acetylcholine (ACh) through the enteric nervous system
Sodium secretion
- when stimulated, one or both channels secrete Cl- into the Lumen
- negative electrical potential (-) created by the luminal movement of Cl- acts as a driving force for the paracellular movement of Na+ into the Lumen
- result is the secretion of NaCl into the Lumen
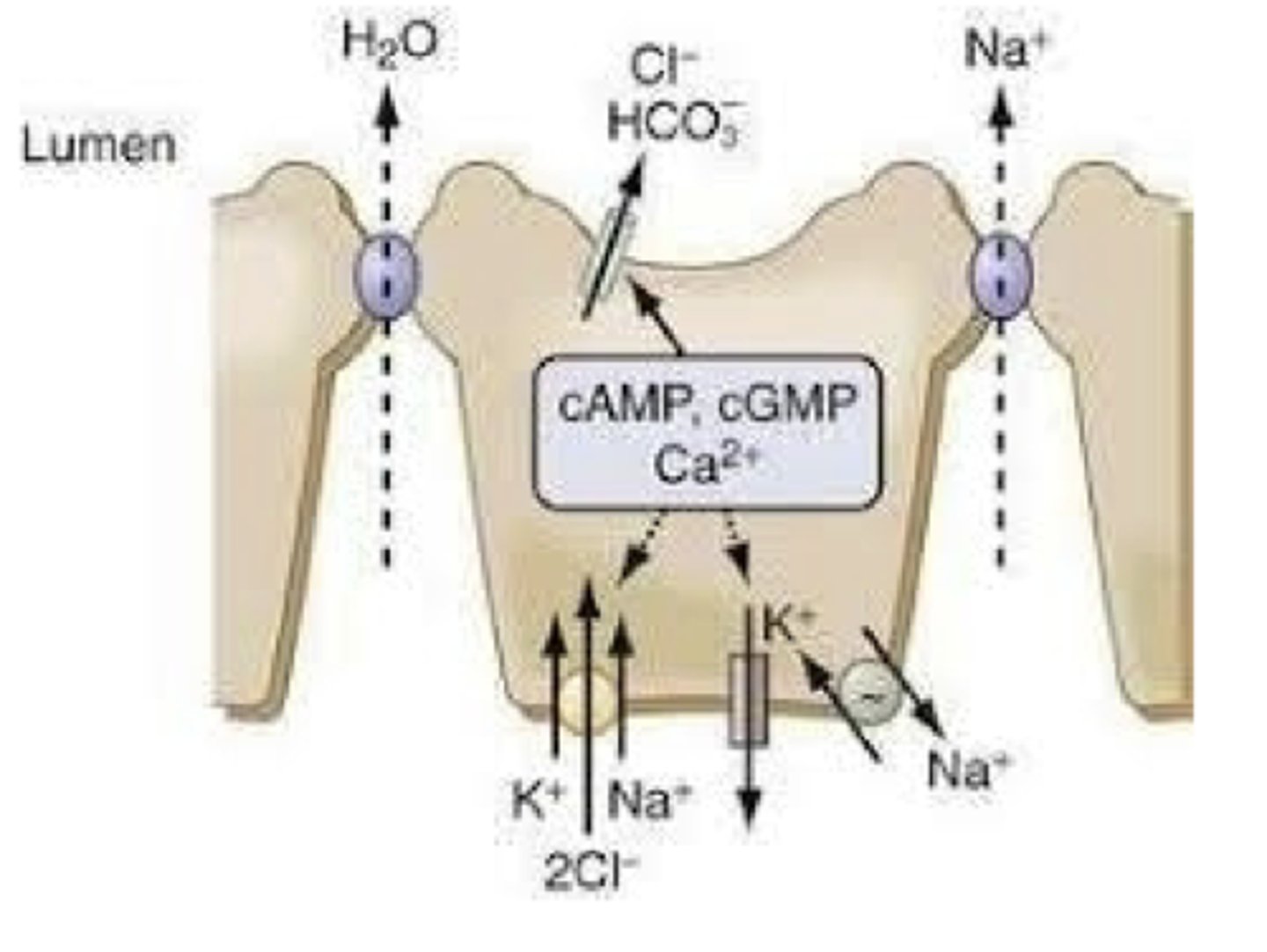
Water secretion
- secretion of NaCl into the Lumen creates an Osmotic Gradient that attracts the passive movement of H2O into the Lumen
- net result is the secretion of an Isotonic Fluid (NaCl & H2O) into the intestinal crypts and Lumen
Physiological anatomy of the Large Intestine (Colon)
- marked proximally by the Ileocecal Sphincter & Valve
- marked distally by the External Anal Sphincter
anatomically distinguished (orad → caudad) into the:
- Cecum
- Ascending
- Transverse
- Descending
- Sigmoid Colon
- Rectum
- Anal Canal
- colorectal Sphincter separates the rectum and anal canal
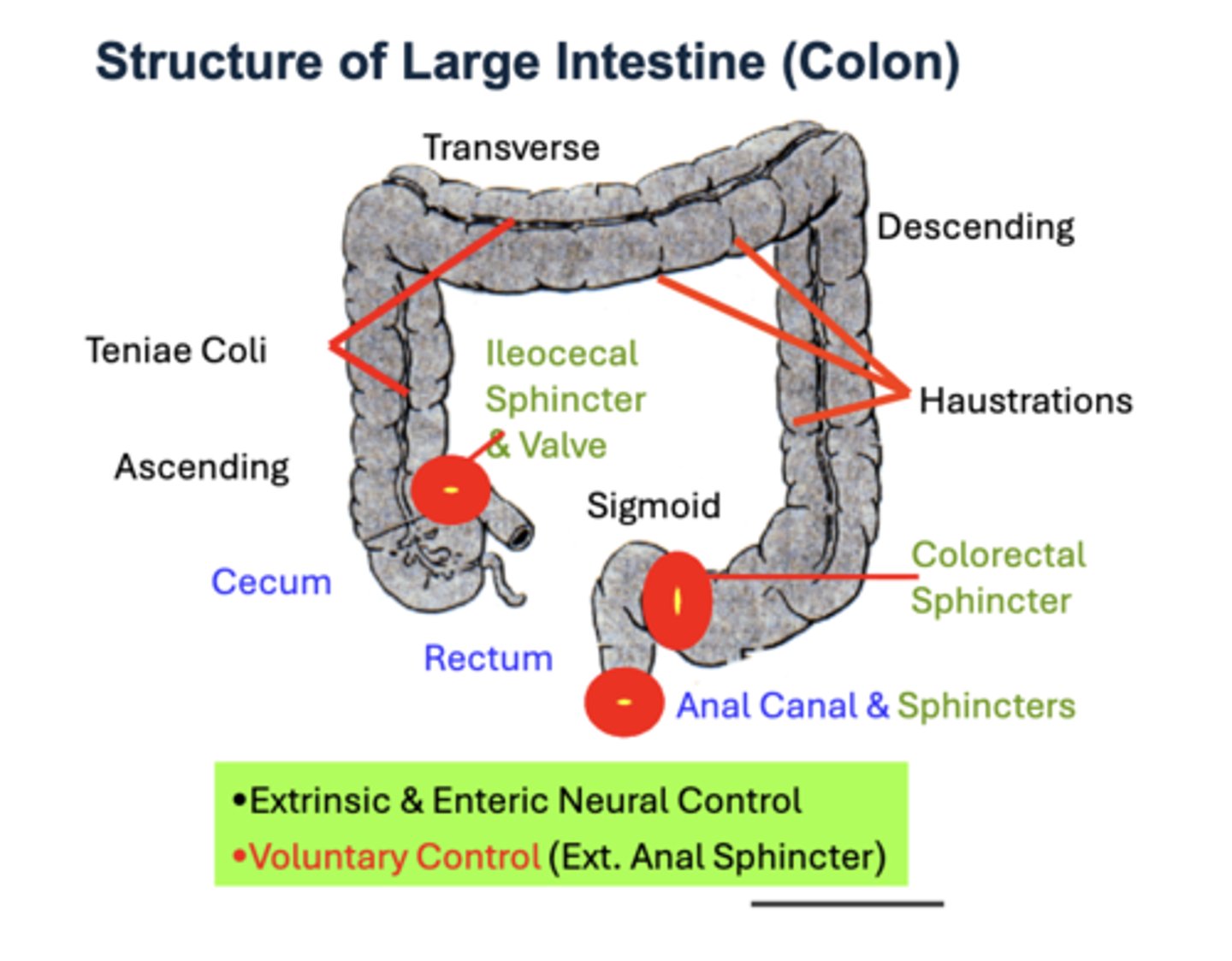
Colon motility
relies on the actions of its thick smooth muscle layers
1. outer longitudinal layer is organized into three distinct flat bands called Teniae Coli
2. inner circular layer is continuous through the anal canal, where it increases in thickness to form the internal anal sphincter
3. smooth-striated muscle transition region leads to purely Striated Muscle bundles that comprise the external anal sphincter
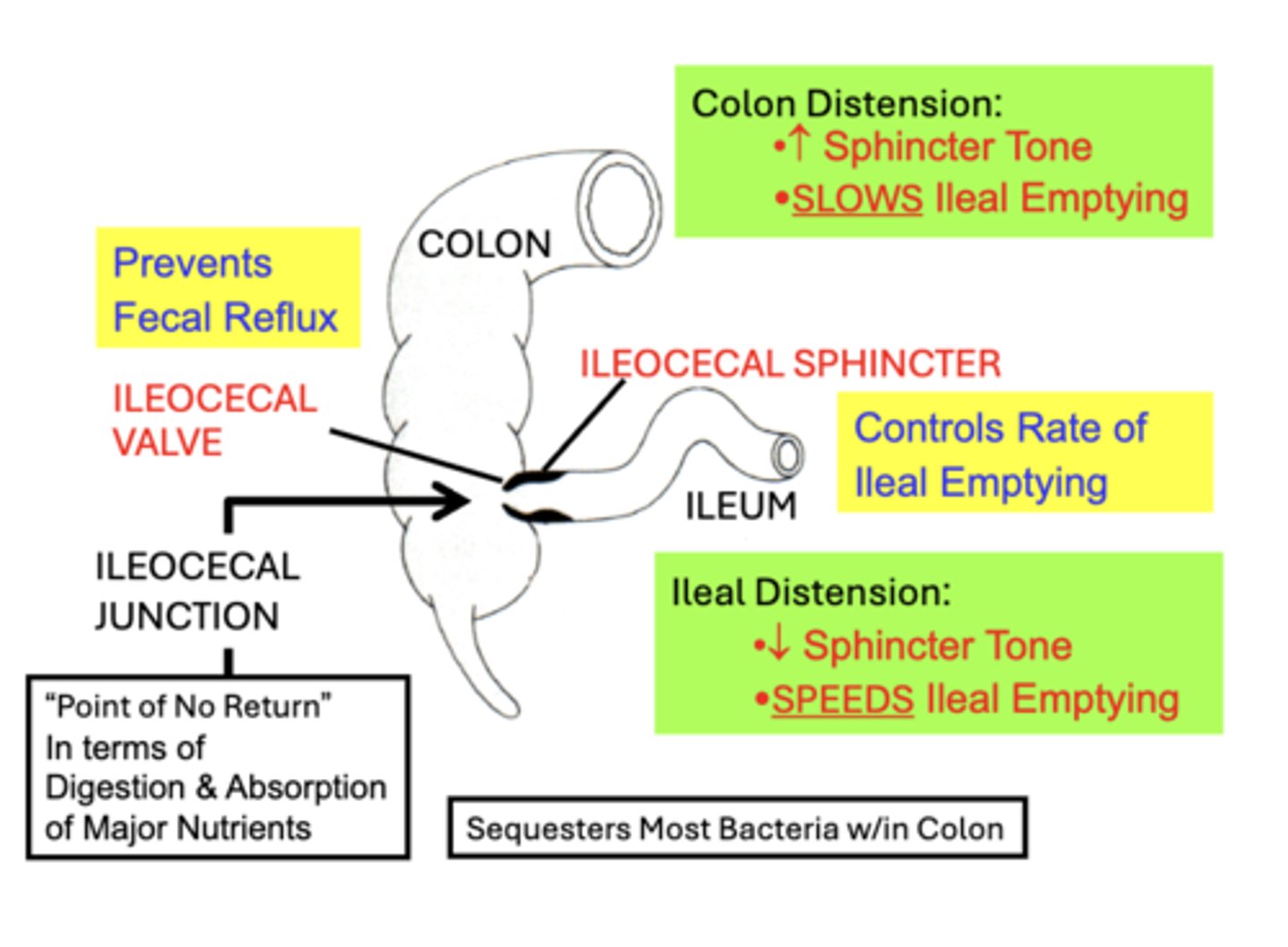
Entry of food from SI to LI: Ileocecal Valve
mainly functions to Prevent Fecal Reflux from the colon into the ileum
- its lips protrude into the lumen, acting as a one-way valve
- when colon pressure pushes fecal contents backward, the valve closes, preventing reflux into the ileum
- physiologically, this is important in order to the maintain Sequestration of Most Bacteria within the Colon
Entry of food from SI to LI: Ileocecal Sphincter
primarily functions to Control Ileal Emptying Rate into the colon
- normally remains mildly constricted, causing a general slowing of ileal emptying into the cecum
- physiologically, this is important because the ileum is the “Point of No Return” in terms of Digestion & Absorption of Major Nutrients since the colon does not largely participate in nutrient digestion or absorption.
- basal constrictive tone of the ileocecal sphincter is maintained by intrinsic myogenic control
Entry of food from SI to LI: Distension
distension of adjacent proximal (Ileum) or distal (Colon) intestinal regions modulate sphincter tone and ileal emptying rate:
Ileal Distension:
- decreases Sphincter Tone
- SPEEDS Ileal Emptying Rate into the colon
- prevents build-up of material in the ileum
Colon Distension:
- increases Sphincter Tone
- SLOWS Ileal Emptying Rate into the colon
- prevents excess filling of the colon
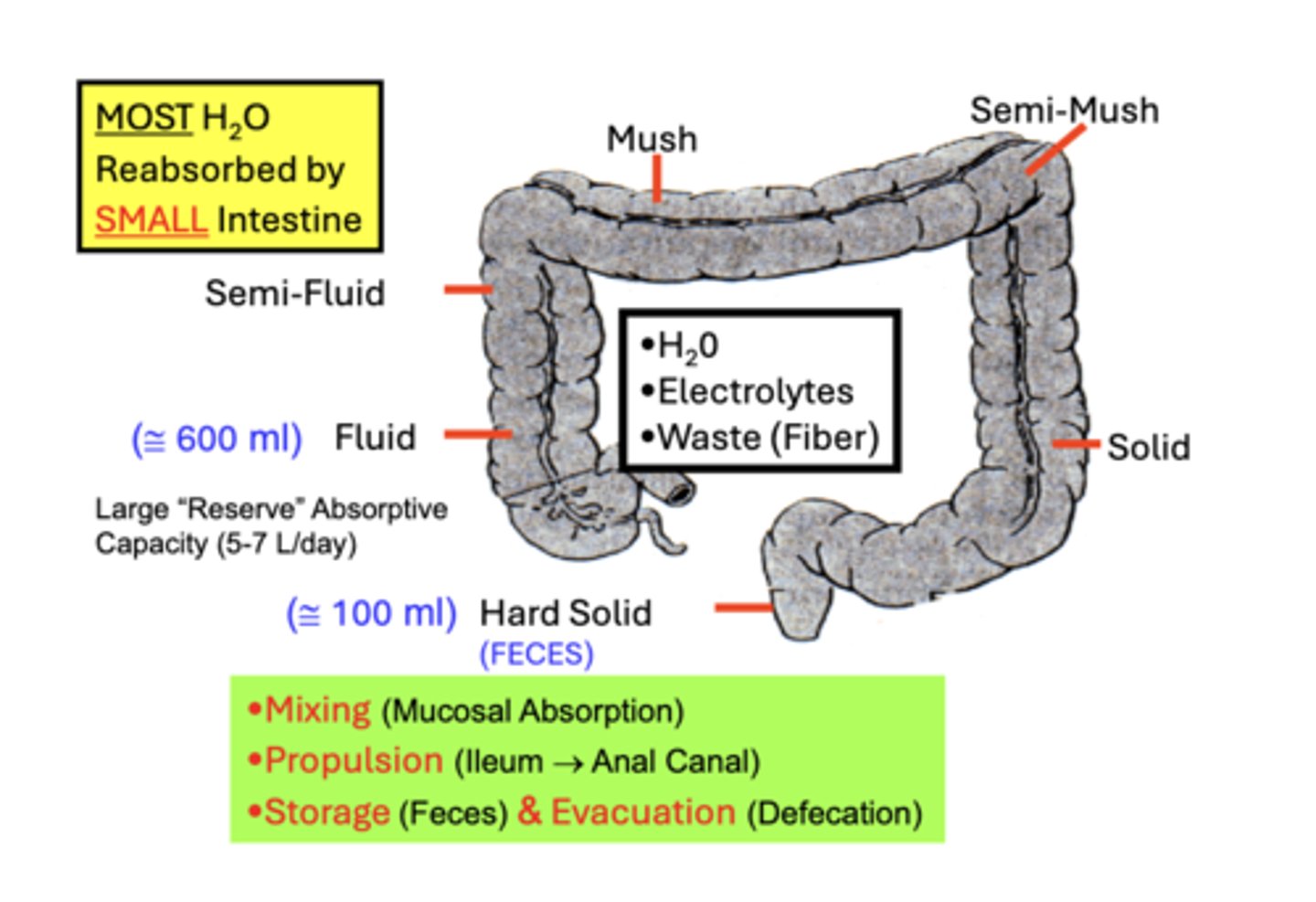
Absorption in Large Intestine
digestion and absorption of most nutrients is almost complete by the time intestinal material enters the colon
- however, significant amounts of H2O & Electrolytes, remain to be absorbed
- in addition, Waste material that is indigestible (Fiber) or produced within the tract (bacteria; mucus) must be transported, stored, and then eliminated from the colon
H2O Absorption
While the large bowel is important for optimal H2O absorption, MOST H2O entering the tract is actually absorbed by the SMALL Intestine
- 7-10 L of ingested or secreted H2O enter the GI tract/day, but only 600 ml is reabsorbed the colon
- however, colonic material still remains highly Fluid
Total Absorption in Large Intestine
reabsorbs all but 100 ml
- causes a relatively Hard Solid material (Feces) to normally reach the rectum for evacuation
- in spite of the relatively small amount of fluid normally reabsorbed, the colon has a large absorptive capacity (5-7 L/day)
- acting as a “reserve capacity” when small intestinal absorption and/or secretion become impaired
Motility Functions of Large Intestine
Colonic motility actions function in the:
• Mixing of material for Mucosal Absorption (H2O & electrolytes)
• Propulsion of contents from the Ileum → Rectum → Anal Canal
• Storage (Feces)
• Evacuation (Defecation) of waste material
Motility Functions of Large Intestine: Haustrations
Segmenting Contractions
• the most common colonic motility action
• local constricting contractions
• act to Mix intestinal contents with little net propulsion of material
• Colonic segmenting contractions exert Greater Force
• 2-4x Longer in Duration (12-60 sec.) than those of the small intestine.
• Contractions deeply constrict the lumen, causing the characteristic Haustrations
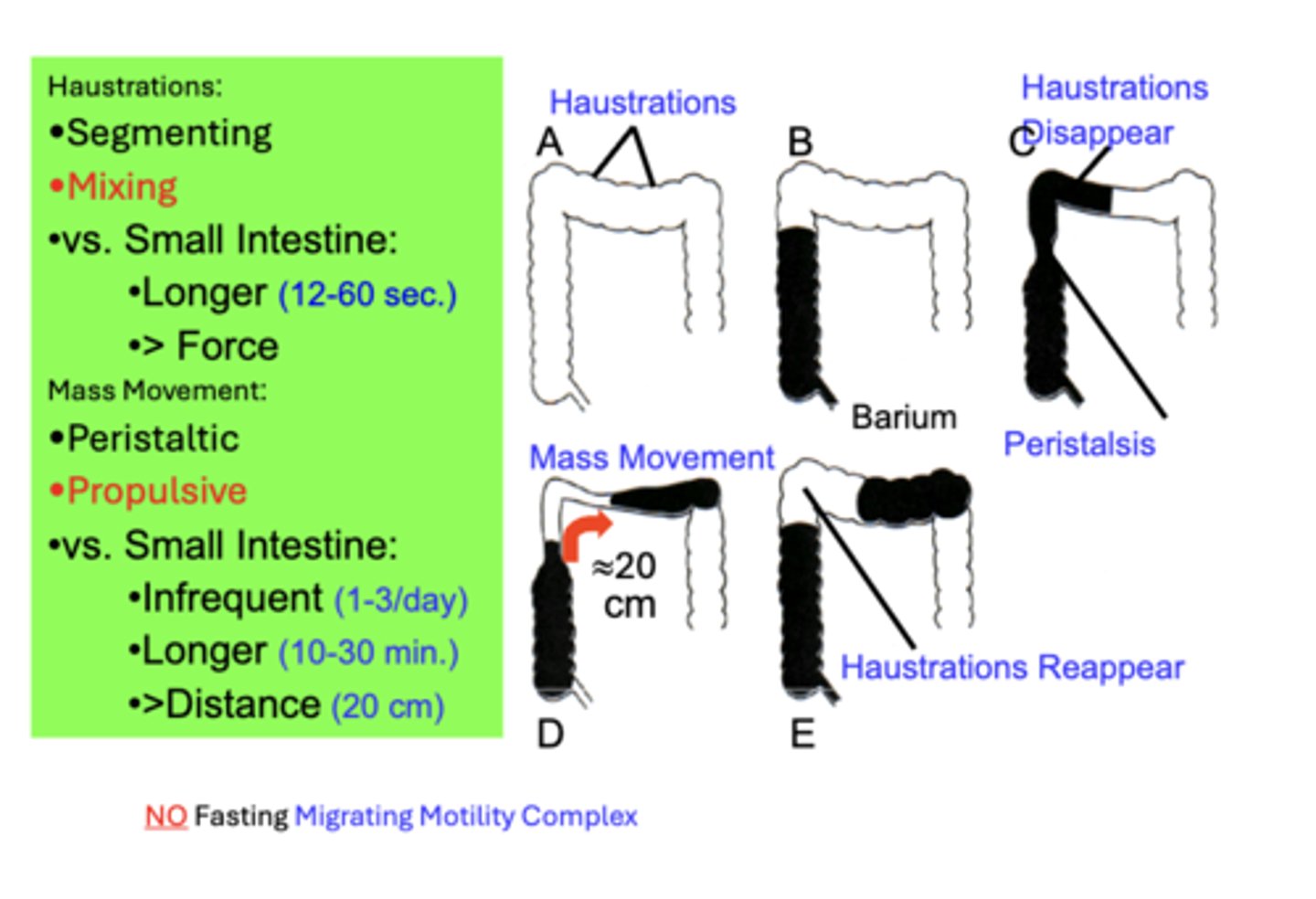
Motility Functions of Large Intestine: Mass Movements
Peristaltic Contractions
- serve in the Propulsion of intestinal contents toward the rectum
compared to small intestine peristalsis (8-12x/min; 4-5 sec., 1-4 cm):
- Less Frequent (1-3x/day)
- Longer in Duration (10-30 min.)
- propel material a Greater Distance (20 cm)
Large Intestine: Neural Reflexes
GASTROCOLIC REFLEX:
• Stomach Distension (e.g. After a Meal)
• Colon Mass Movement
• Coordinated w/ Gastroileal Reflex
DUODENALCOLIC REFLEX:
• Duodenal Distension (e.g. After Meal)
• Colon Mass Movement
• Augments Gastrocolic & Gastroileal
• Defecation Sensation After Eating
Large Intestine: Inter-regional Neural Reflexes
All reflexes are mainly regulated Extrinsically and are largely responsible for the Defecation Sensation that commonly develops shortly after eating a meal
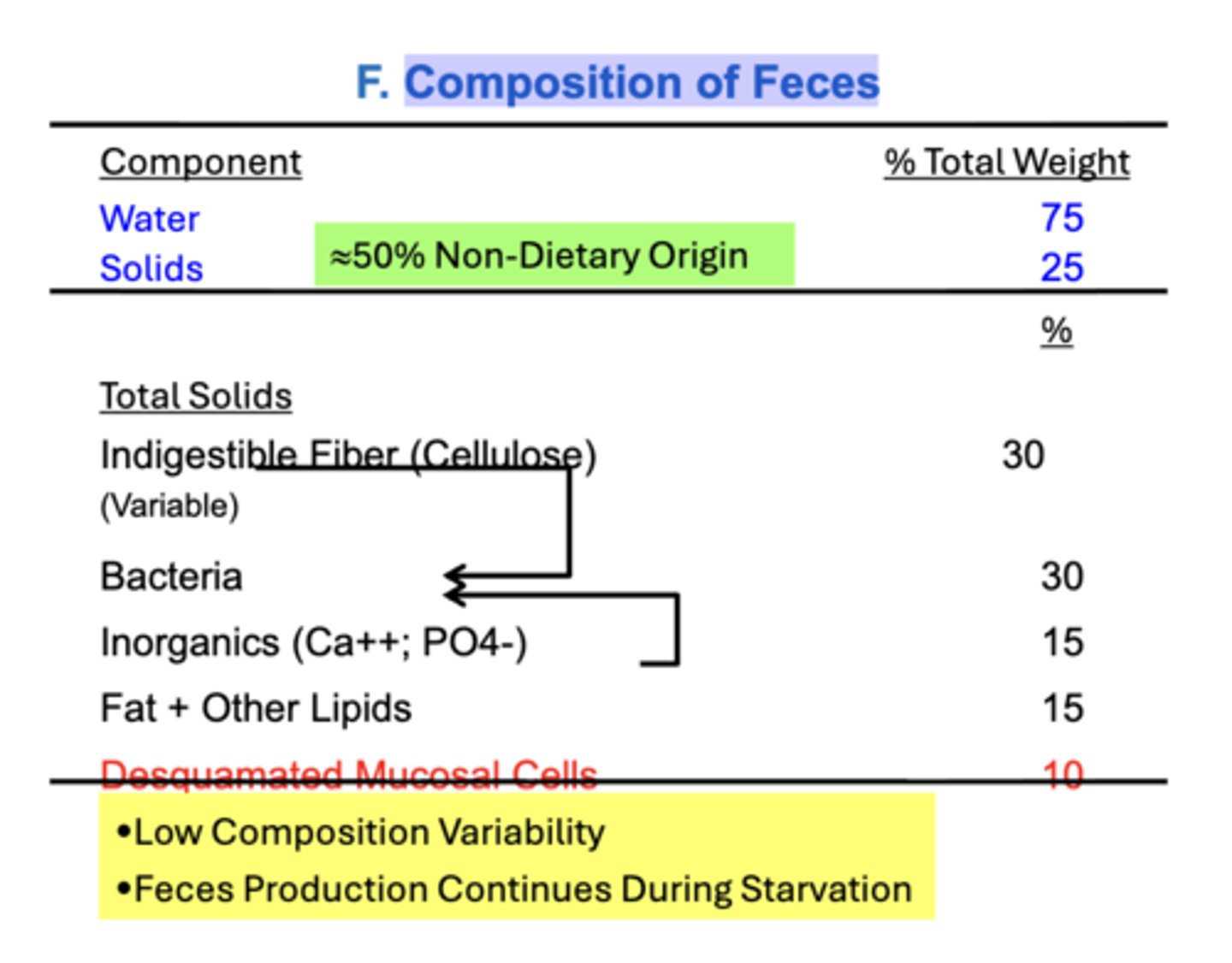
Composition of Feces
Normal Human Feces is about 75% Water and 25% Solids
Note: more than half of the components of feces is of Non-Dietary Origin
- most dietary carbohydrates, fats & protein are digested & absorbed
- there is a relatively Low Composition Variability of feces despite significant variability in diet composition