1 - The Organization of the Respiratory System and Principles of Ventilation
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
Cellular respiration Definition
Intracellular metabolic processes that uses O2 and produces CO2
External respiration (pulmonary physiology) Definition
All the events involved in the exchange of O2 and CO2 between the external environment and tissues
Parts of Upper airways or respiratory tract
Larynx and above (nose, nasal cavity, pharynx, larynx)
Parts of Lower airways or respiratory tract
Trachea and below
Two sections of the respiratory tract
Conducting zone
Respiratory zone
Parts of the conducting zone
Trachea to terminal bronchioles
Parts of respiratory zone
Respiratory bronchioles to alveolar sacs
Function of respiratory zone
Have at least one alveolus on the wall
Gas exchange
What are the functions of the conducting zone
Conduit for air movement
Humidify the air
Warm the air
Remove particulate material
Components of the respiratory epithelium (6)
Periciliary fluid layer (Watery fluid)
Lumen
Epithelial cell
Cilia
Goblet cell
Mucus layer
How does the conducting zone of the lower respiratory tract (and the nasal cavity) help remove inhaled particulate material (dust, pollutants, microbes, etc)?
Mucus traps foreign particles
Cilia beat and move the mucus and trapped particles toward the throat
What happens to any particulate material that escapes being cleared by the respiratory epithelium and gets into the alveoli?
Phagocytosed by macrophages in the alveoli
Alveolar sacs are in which part of the respiratory tract?
A. Conducting zone of the upper respiratory tract
B. Conducting zone of the lower respiratory tract
C. Respiratory zone of the upper respiratory tract
D. Respiratory zone of the lower respiratory tract
D. Respiratory zone of the lower respiratory tract
Cystic fibrosis is caused by mutations in a Cl- channel that results in a decreased ability to secrete Cl-, which enhances Na+ and water absorption by airway epithelial cells, causing a reduction in the volume of periciliary fluid. This will most likely cause: (pick 2)
A. A more watery mucus layer
B. A more viscous mucus layer
C. Reduced mucociliary transport
D. Enhanced mucociliary transport
B. A more viscous mucus layer
C. Reduced mucociliary transport
A smoker develops a lower respiratory tract infection and has been coughing up mucus. What put him at risk for this infection?
A. Recruitment and increased activity of lung macrophages
B. Decreased mucus production
C. Increased activity (more contraction) of bronchiolar smooth muscle
D. Paralysis or decreased activity of the cilia in the respiratory epithelium
E. Increased production of watery fluids by the respiratory epithelium
D. Paralysis or decreased activity of the cilia in the respiratory epithelium
What aspect of an alveoli facilitates gas exchange? (2)
Thin wall
Alveoli are close to the capillaries
Type I and Type II cells
Type I cell - Makes up most of the alveolar wall
Type II cell - Produce surfactant
Functions of the intrapleural fluid (3)
Lubrication
Holds the parietal and visceral pleural membranes together
It has an intrapleural pressure (Pip) which is needed for ventilation
What are the 2 phases of ventilation or breathing?
Inspiration and expiration
What causes air to flow into and out of the lungs?
Pressure gradient
What prevents or resists flow?
Resistance of conducting airways
What is the Flow formula for airflow?
Flow = (Palv-Patm)/R
(Palv-Patm) = Pressure gradient
Patm value
Atmospheric pressure (760 mm Hg at sea level, but we will set it at zero)
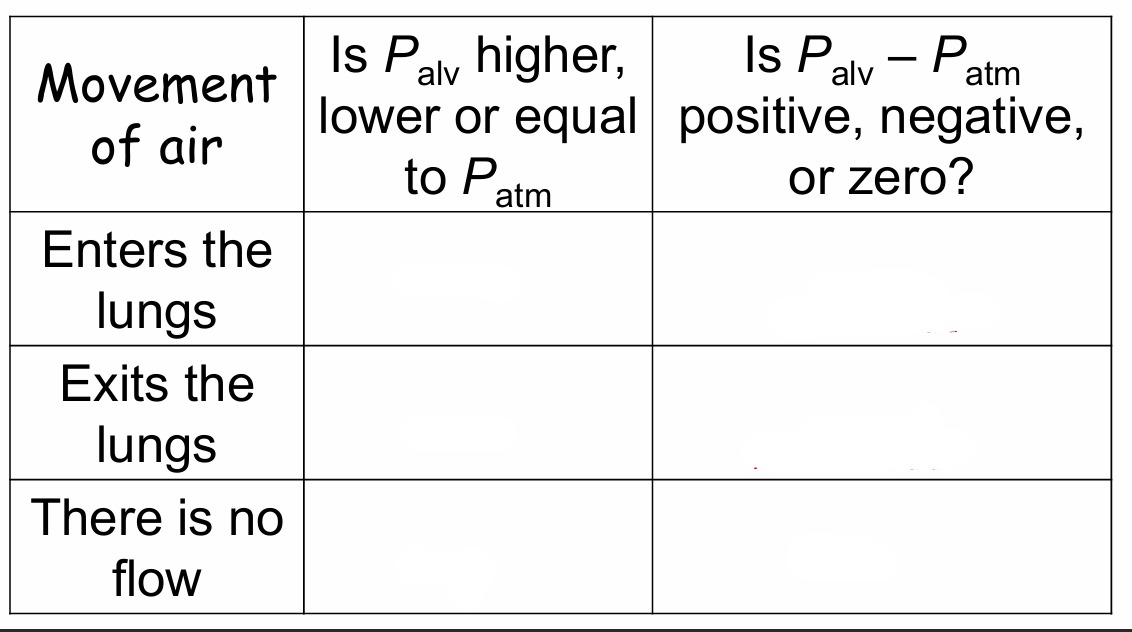
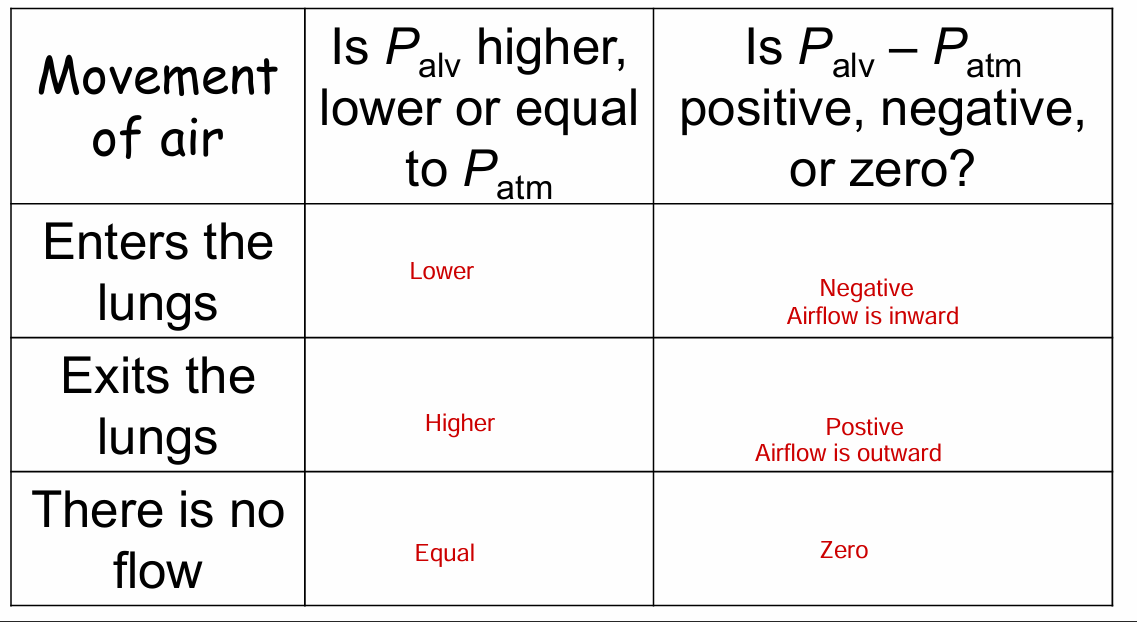
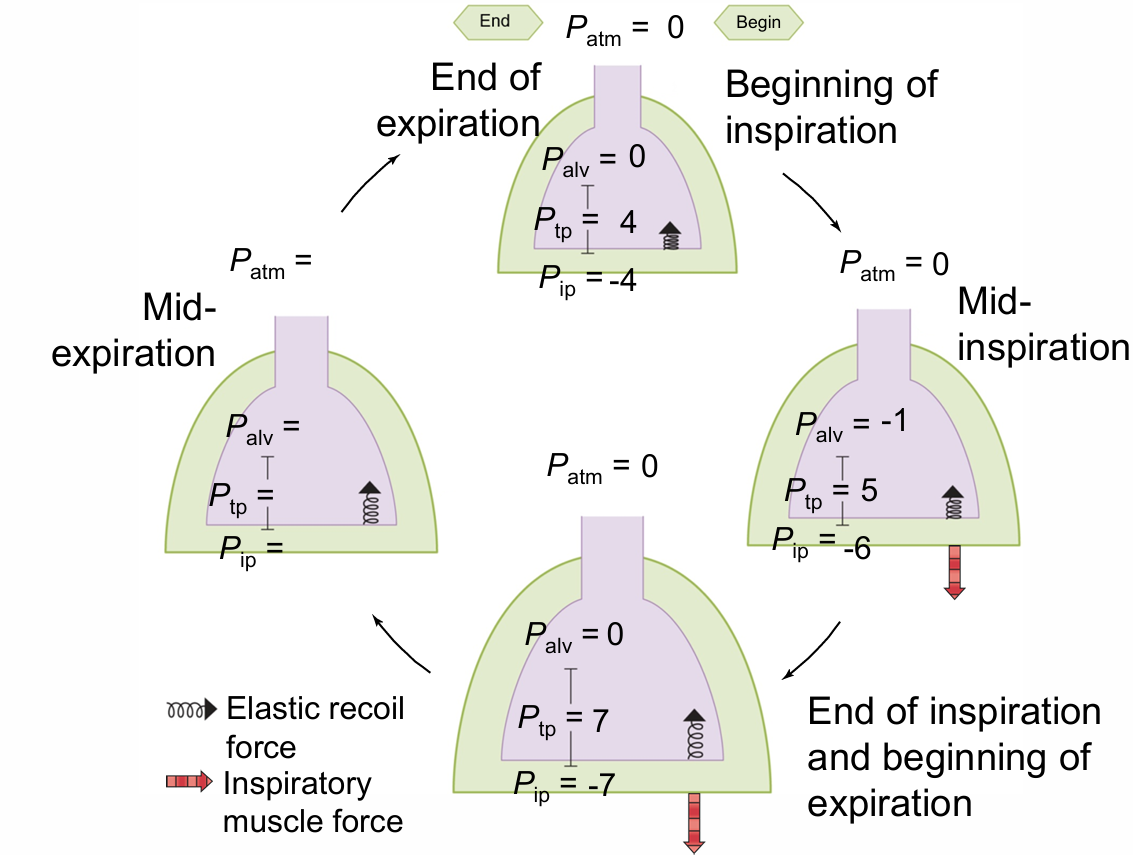
Fill out the table
Ptp equation
Pressure difference between the alveolus and intrapleural fluid
Ptp= Palv - Pip
Pip definition
Pip - Elastic recoil of the lung and chest wall
Ptp relationship to elastic recoil
Ptp is equal and opposite to the elastic recoil of the lungs
Before insp (Ptp= Palv - Pip)
4 = 0 - -4
If just Pip changes (Ptp= Palv - Pip)
5 = 0 - -5
If both Palv and Pip changes (Ptp= Palv - Pip)
5 = -1 - -6
What happens with a pneumothorax/ collapsed lung
If the pleura is punctured, air can enter the pleural cavity.
The pressure in the pleural cavity will then be equal to atmospheric pressure (Pip will be 0)
Transpulmonary pressure will then be 0
There isn’t anything to oppose the elastic recoil of the alveoli and they collapse
In order for inspiration and expiration to occur, the volume of the thoracic cavity needs to change. What causes this change in volume?
Muscle contraction and relaxation
muscles of inspiration
Diaphragm
More muscles recruited during labored breathing
Muscles of expiration
Only used during forced expirations (labored breathing)
How does muscle contraction during inspiration affect the size (i.e. volume) of the thoracic cavity, and how does this affect Pip?
Contraction of inspiratory muscles causes:
Volume of thoracic cavity will increase
Pip will be More negative (Creating a larger vacuum)
During inspiration (mid inspiration), how does the change in Pip, affect Ptp, and lung or alveolar volume?
Pip is more negative
Ptp increases (Greater than elastic recoil)
Alveolar volume increases
During inspiration (mid inspiration), if alveolar volume increases, what happens to Palv?
Palv more negative (or < 0
During inspiration (mid inspiration), what happens to air?
Flows from an area of higher pressure (atmospheric pressure outside the body) to an area of lower pressure (alveolar pressure)
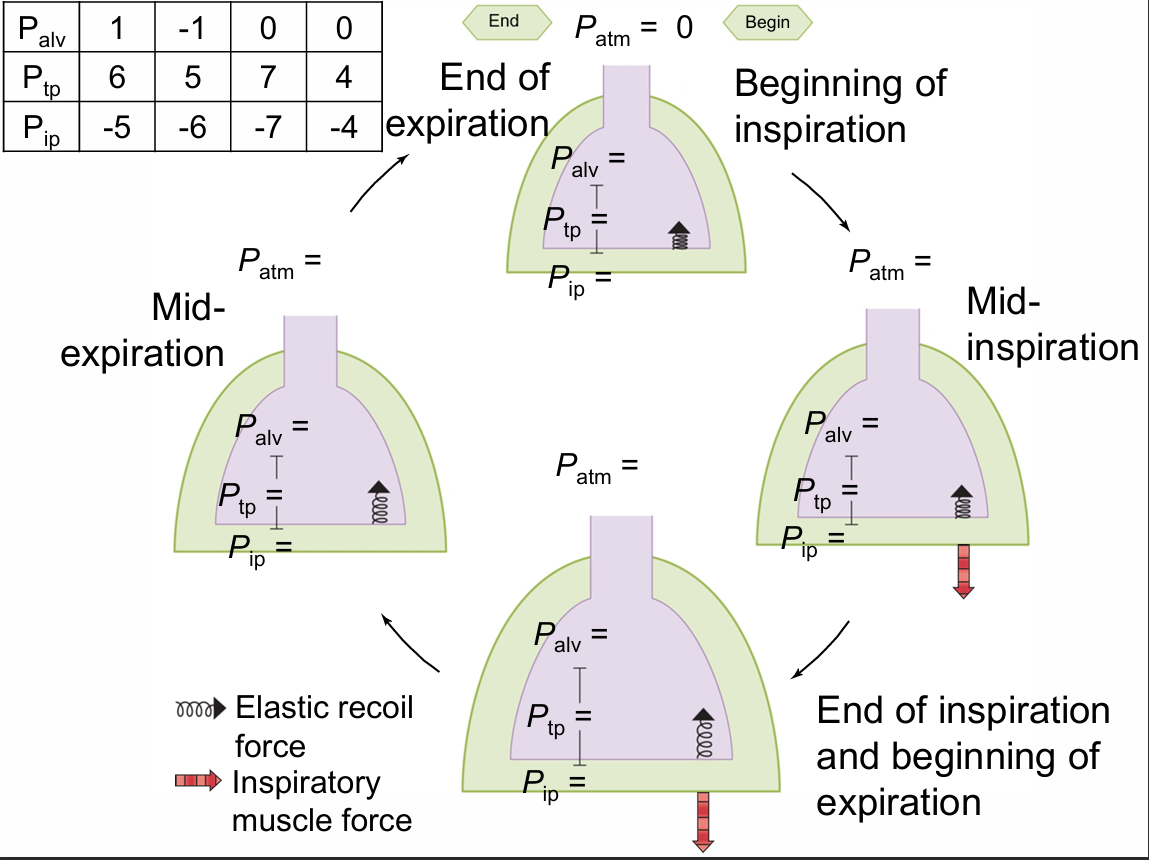
DRAW THIS OUT using numbers
What happens to Pip, Ptp, alveolar volume and Palv during expiration (mid expiration)?
Pip becomes less negative
Ptp decreases
Alveolar volume decreases
Palv increases
Air flows out (From high to low pressure)
Take home message: When breathing in (mid inspiration)
Thoracic cavity and alveoli get bigger
Both Pip and Palv become more negative (same direction)
Take home message: When breathing out (mid expiration)
Thoracic cavity and alveoli get smaller
Both Pip and Palv become more positive (same direction)
Pressure at the end of an unforced expiration
Air movement
Alveolar pressure
No movement of air
Alveolar pressure = atmospheric pressure
Pressure During inspiration when Inspiratory muscles contract (7)
Diaphragm
Ribs
Thorax
Alveolar volume
Alveolar pressure
Air movement
Diaphragm moves down to make chest cavity bigger
Ribs move up and out
Thorax expands (more of a vacuum = decreased Pip)
Alveolar volume increases
Alveolar pressure is less than atmospheric pressure
Air moves inward
Pressure at the end of inspiration
Air movement
Alveolar pressure
No air movement
Alveolar pressure = atmospheric pressure
Pressure During expiration
Diaphragm
Inspiratory muscles
Thorax
Alveolar pressure
Alveolar volume
Air movement
Diaphragm relaxes and moves up
Inspiratory muscles relax/ recoil
Thorax - less of a vacuum in thoracic cavity = increased IP
Alveolar pressure greater than atmospheric pressure
Alveolar volume decreases
Air moves outward
A person started choking and was administered the Heimlich maneuver (you do an abdominal thrust or push on their abdomen). Why did this work to expel the food out of the throat?
A. There is an increase in Palv without affecting Pip
B. Pip becomes more positive leading to a decrease in Palv
C. Pip becomes more positive leading to an increase in Palv
D. Pip becomes more negative leading to an increase in Palv
E. Pip becomes more negative leading to a decrease in Palv
C. Pip becomes more positive leading to an increase in Palv
In order for air to enter the lungs during inspiration, what needs to happen to Palv and Pip? Compared to at the end of an unforced expiration:
A. There is no change in Palv or Pip
B. Palv needs to be more positive and Pip need to be more negative
C. Palv needs to be more negative and Pip need to be more positive
D. Both Palv and Pip need to be more positive
E. Both Palv and Pip need to be more negative
E. Both Palv and Pip need to be more negative
A person has a stab wound to the chest which causes their lungs to collapse (pneumothorax). What happened to Pip?
A. Pip > 0
B. Pip < 0
C. Pip = 0
C. Pip = 0
This causes the transpulmonary pressure gradient (P tp) to be lost
Besides the transpulmonary pressure (Ptp), what else affects the change in volume (i.e. size) of the lungs or alveoli when breathing?
A. Lung compliance
B. Airway resistance
A. Lung compliance
Lung compliance definition
How well the lungs (alveoli) can stretch
change in lung volume produced by a given change in Ptp
Airway resistance defintion
Resisting flow in the tube → Viscosity of air, length of tube, radius of the tube
What 2 factors determine the compliance of the lungs?
The ability of the lung tissue to stretch
Surface tension of the liquid on the alveolar wall
What is the purpose of surfactant production?
Acts like a detergent which lowers surface tension
What is the benefit of surfactant? (2)
It increases compliance
Don’t need as great of an increase in Ptp to expand the lungs with inspiration
Benefit of surfactant when Pip decreases
Ptp increases
Alveoli stretch
Much easier to do with surfactant
Now let’s look at airway resistance. How can the body change the resistance of the airways? By changing the:
A. Size of the alveoli
B. Compliance of the alveoli
C. Viscosity of the air
D. Radius of the tube (trachea, bronchi, bronchioles)
E. Length of the tube (trachea, bronchi etc)
D. Radius of the tube (trachea, bronchi, bronchioles)
Purpose of trachea, bronchii
Cartilage keep the airways open
Purpose of bronchioles
Smooth muscle/ no cartilage
The same forces that open up alveoli, open up bronchioles!
can also contact and relax the smooth muscle
There are several hormones (e.g. epinephrine), neurotransmitters (e.g. acetylcholine), paracrine factors (e.g. histamine, leukotrienes) that affect airway resistance. For example, epinephrine decreases airway resistance by activating:
A. a1 receptors which relaxes bronchiolar smooth muscle
B. B2 receptors which contracts bronchiolar smooth muscle
C. a1 receptors which contracts bronchiolar smooth muscle
D. B2 receptors which relaxes bronchiolar smooth muscle
D. B2 receptors which relaxes bronchiolar smooth muscle
NO SYMPATHETIC INERVATION
Respiratory distress syndrome of the newborn occurs in premature infants (< 37 weeks gestation) in which the alveoli collapse. Which of the following contributes to this lung collapse?
A. Decreased lung compliance
B. Excessive production of surfactant by type II alveolar cells
C. Increased lung resistance
D. Decreased lung resistance
E. Deceased surface tension in the alveoli
A. Decreased lung compliance
What happens with less surfactant?
The force to keep alveoli open and expand the lungs during inspiration needs to be greater
Asthma is an inflammatory disease. But, during an attack, one reason why a person has difficulty breathing is because smooth muscle in the lungs is hyperactive with excessive broncho constriction. How will this affect respiration
A. Decrease lung compliance
B. Decrease airway resistance
C. Increase elastic recoil
D. Increase lung compliance
E. Increase airway resistance
E. Increase airway resistance
The increased airway resistance makes it difficult to exhale.
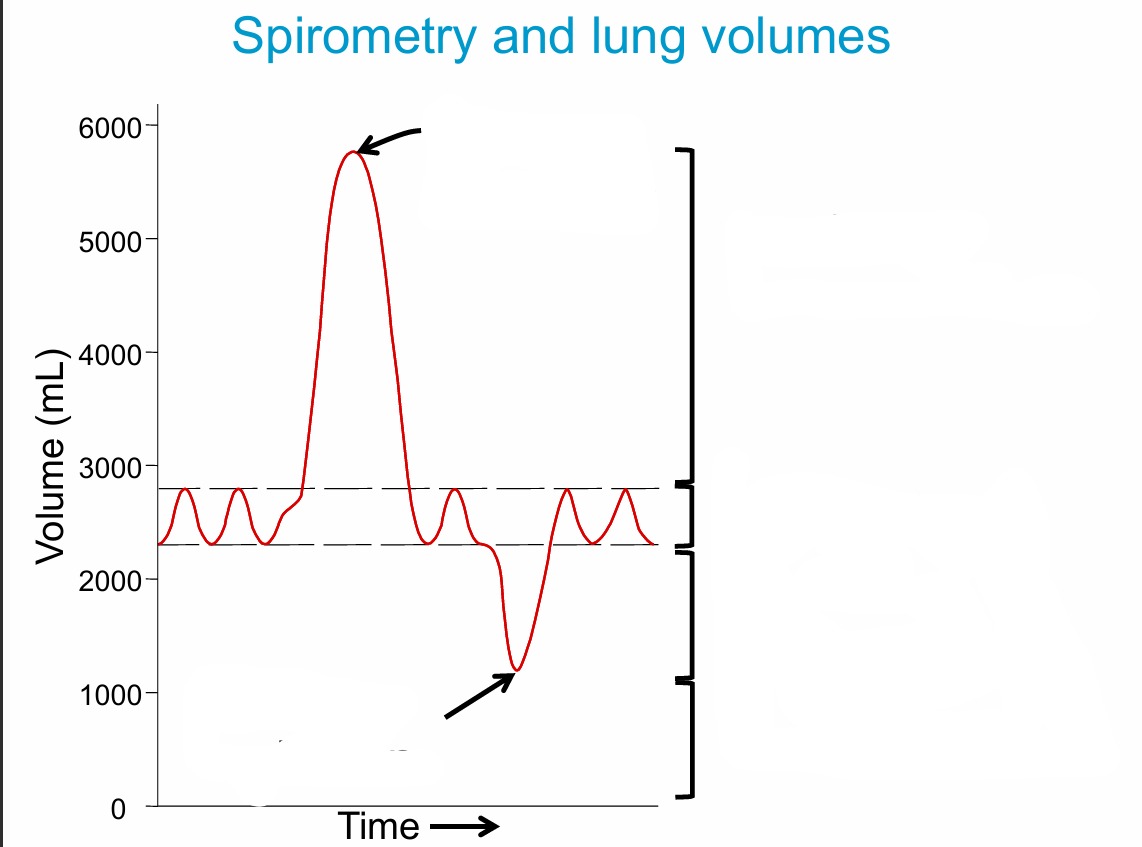
Draw and lable
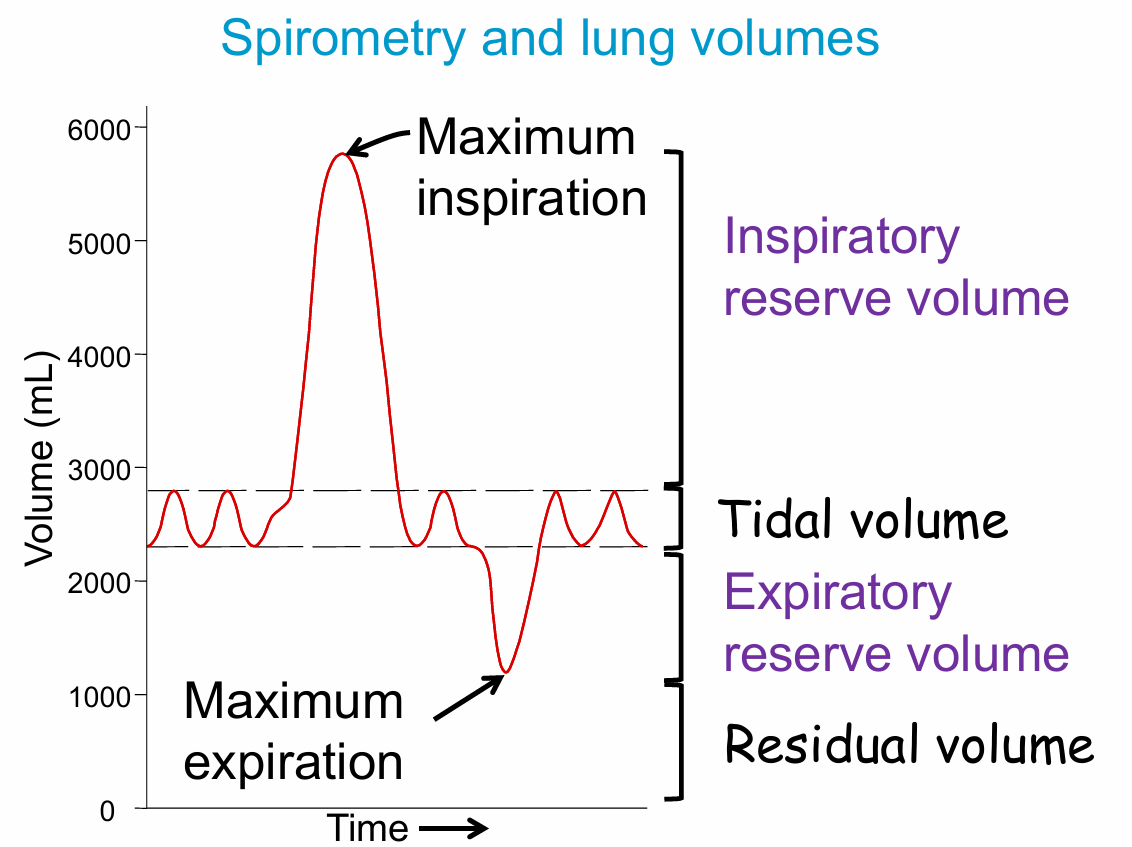
During exercise, which of the following changes occur? (select all that are correct)
A. Tidal volume increase
B. Tidal volume stays the same
C. Inspiratory reserve volume increases
D. Inspiratory reserve volume decreases
E. Expiratory reserve volume decreases
F. Expiratory reserve volume stays the same
G. Residual volume decrease
H. Residual volume stays the same
A. Tidal volume increase
D. Inspiratory reserve volume decreases
E. Expiratory reserve volume decreases
H. Residual volume stays the same
What is vital capacity?
Maximum amount that you can expel from the respiratory tract after a maximum inspiration
How is vital capacity measured?
Inhale maximally, then exhale maximally into a spirometer as fast as possible
Forced expiratory vital capacity (FVC)
Forced expiratory volume in 1 second (FEV1)
What is Forced expiratory vital capacity (FVC)? What is Forced expiratory volume in 1 second (FEV1)?
How much you can inhale
How fast or easy it is to exhale
A person has muscular dystrophy where their diaphragm is weak. How will this effect their vital capacity?
C. No effect
D. Increased
E. Decreased
E. Decreased
Reduced compliance can also reduce vital capacity
A person has emphysema. (with emphysema the elastic recoil of the lungs is reduced). How will this affect their FEV1?
A. Not have any effect
B. Decreased
C. Increased
B. Decreased
FEV1 can also be reduced by asthma/ bronchoconstriction