(22.7) Transport of Respiratory Gasses by Blood
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Describe how oxygen is transported in blood
1.5% is dissolved in plasma
98.5% is loosely bound to each Fe of hemoglobin (Hb) in RBCs
T/F: O2 is highly soluble in the blood
→ FASLE
O2 is POORLY SOLUBLE in the blood → only 1.5% is dissolved in plasma, remaining 98.5% must be carried on hemoglobin
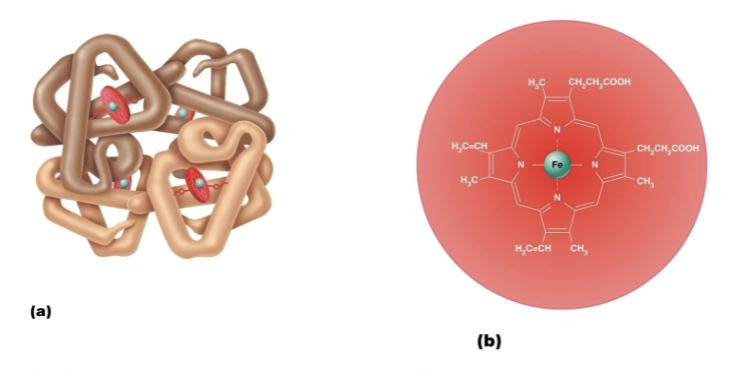
How many O2 molecules can be reversibly bound to a molecule of hemoglobin?
Each Hb molecule is composed of 4 polypeptide chains, each with an iron-containing heme group → so each Hb can transport 4 oxygen molecules
Distinguish between Oxyhemoglobin & Deoxyhemoglobin
Oxyhemoglobin (HbO2)
Hemoglobin-O2 combination
Deoxyhemoglobin (HHb)
Hemoglobin that has released O2
Reduced hemoglobin
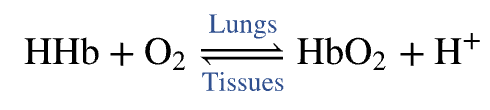
Explain Influence of O2 on Hemoglobin Shape
Loading and unloading of O2 is facilitated by change in shape of Hb
O2 binds, Hb changes shape → INCREASING its affinity for O2 increases
O2 is released, Hb shape change → causes a DECREASE in affinity of O2
Explain Influence of O2 on Hemoglobin Saturation
FULLY saturated (100%)
ALL 4 heme groups carry O2
PARTIALLY saturated
ONLY 1 to 3 hemes carry O2
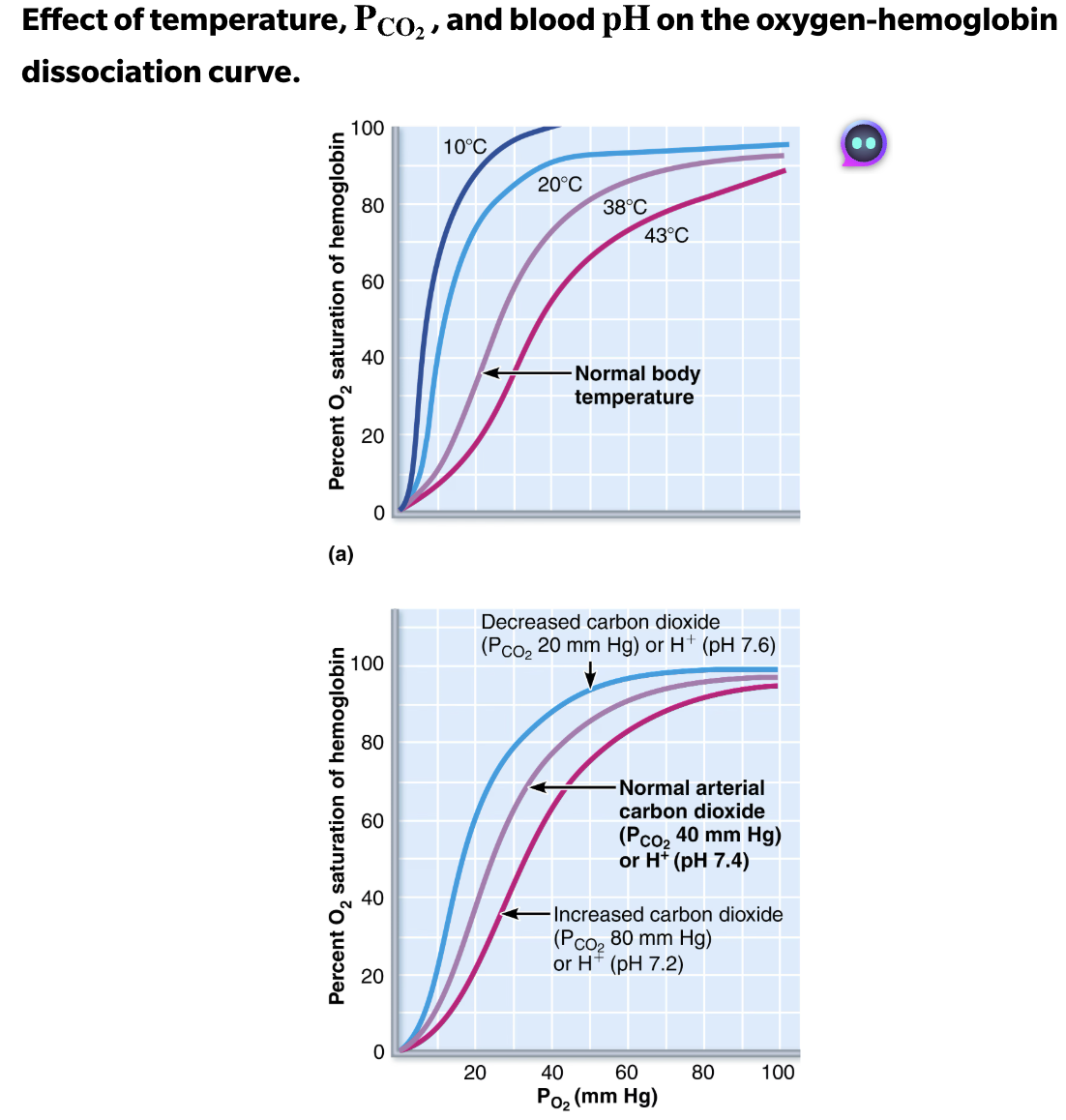
Factors regulating oxygen loading and unloading from hemoglobin
Rate of loading and unloading of O2 is regulated to ensure adequate oxygen delivery to cells
PO2
Temperature
pH
BPG
PCO2
Explain Influence of PO2 on Hemoglobin Saturation
HIGH plasma partial pressure of O2 → hemoglobin unloads little oxygen
DROP plasma partial pressure of O2 → more oxygen can be unloaded to the tissues
T/F: Increased temperature results in decreased O2 unloading from hemoglobin.
→ FALSE
Increased temperature results in INCREASED O2 unloading from hemoglobin
Decrease the affinity (binding strength) of hemoglobin for oxygen.
T/F: If your core temperature becomes colder, it is more difficult for oxygen to dissociate from hemoglobin at any
→ TRUE
Decrease in temperature increases hemoglobin's binding affinity for O2, making it more difficult to dissociate (unload) O2from hemoglobin
Which of the following would induce the loss of oxygen from hemoglobin and the blood?
A.) a decrease in plasma carbon dioxide
B.) an increase in hemoglobin that already has one or more oxygen molecules bound to it
C.) a drop in blood pH
D.) a decrease in blood temperature
→ C.) a drop in blood pH
Lower pH (more acidic) → Bohr effect → reduced hemoglobin affinity for O₂ → more O₂ released.
Less CO₂ → fewer H⁺ ions → higher pH, which increases hemoglobin’s affinity for O₂
Hemoglobin the more O₂ it carries, the higher its affinity becomes
Lower temperature shifts the dissociation curve left, increasing O₂ affinity
T/F: As carbon dioxide enters systemic blood, it causes more oxygen to dissociate from hemoglobin (the Haldane effect), which in turn allows more CO2 to combine with hemoglobin and more bicarbonate ions to be generated (the Bohr effect).
→ FALSE
CO₂ (and H⁺) → O₂ unloading
Bohr effect
As carbon dioxide enters systemic blood, it forms carbonic acid → H⁺.
These H⁺ ions decrease hemoglobin’s affinity for O₂, causing more oxygen to dissociate from hemoglobin
Deoxygenated Hb → increased CO₂ uptake and bicarbonate formation
Haldane effect
Explain Cause and Effect of Hypoxia
CAUSE
Inadequate O2 delivery to tissues
EFFECT
Cyanosis

List and explain causes of Hypoxia
Anemic hypoxia
Too few RBCs or abnormal or too little Hb
Ischemic hypoxia
Impaired or blocked circulation
Histotoxic hypoxia
Cells unable to use O2, as in metabolic poisons
SUMMARY how PO2, temperature, pH, BPG, and PCO2 affect oxygen loading and unloading from hemoglobin
ALL of these factors influence Hb saturation by modifying hemoglobin’s three-dimensional structure, thereby changing its affinity for O2
Increase in temperature, PCO2, H+, or BPG levels in blood lowers Hb’s affinity for O2, enhancing oxygen unloading from the blood
Decrease in any of these factors increases hemoglobin’s affinity for oxygen, decreasing oxygen unloading
Carbon Monoxide Poisoning Affect in Hb
Hb has 200x greater affinity for carbon monoxide than oxygen
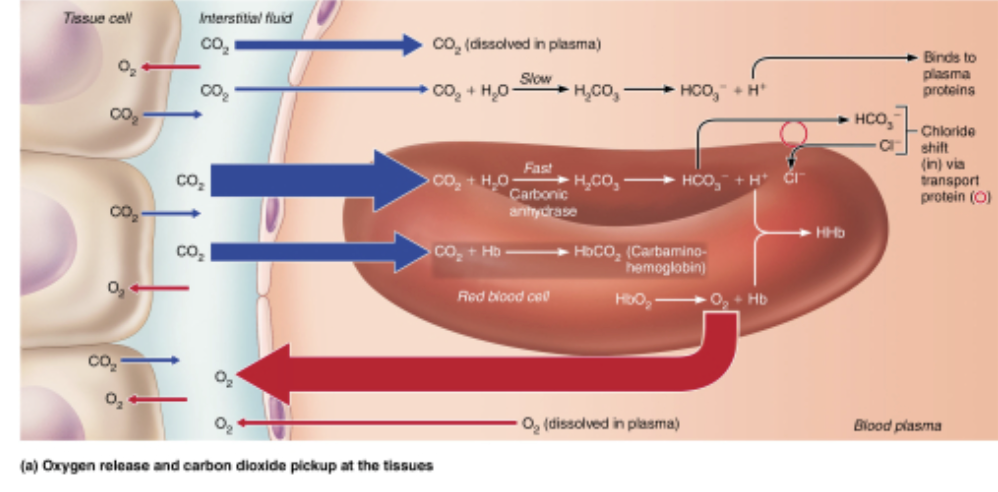
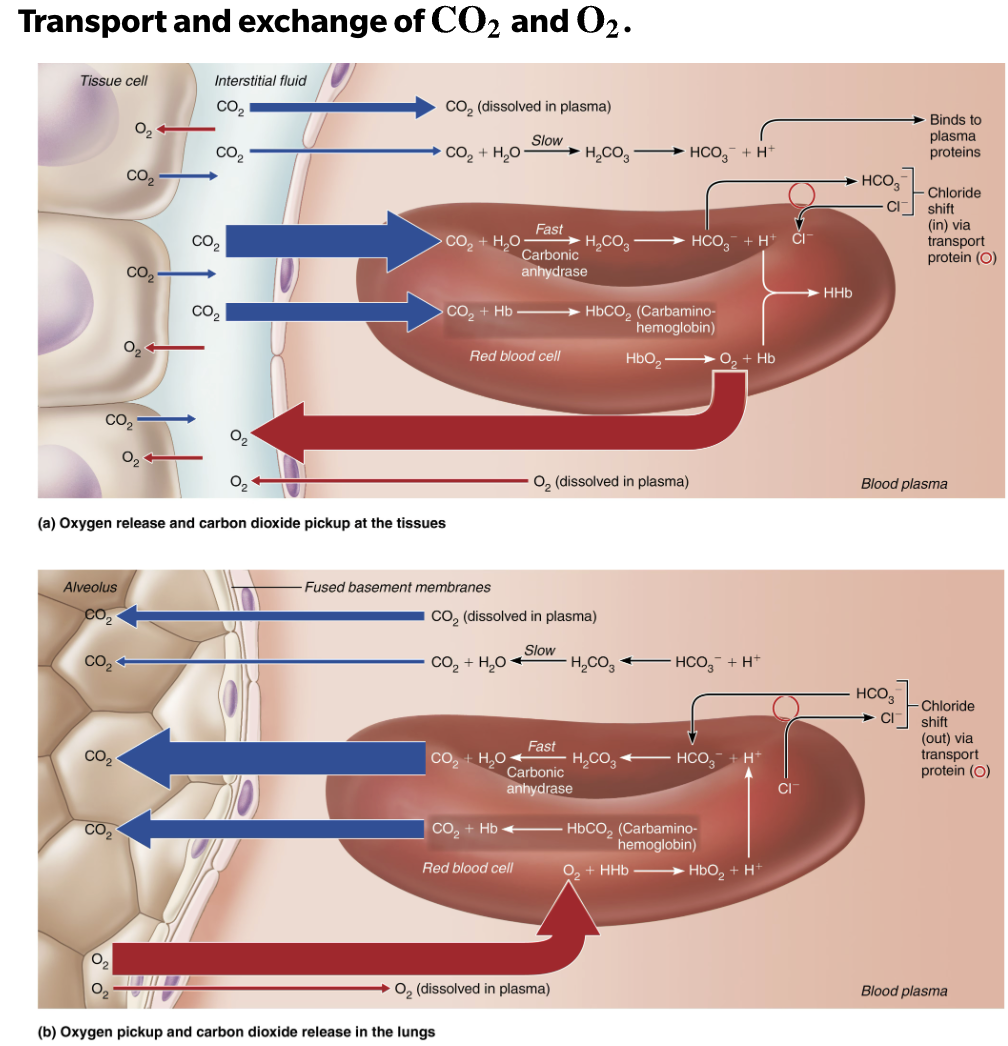
Describe carbon dioxide transport in the blood
7-10% is dissolved in plasma as PCO2
20% of CO2 is bound to the globin part of hemoglobin (carbaminohemoglobin)
70% is transported as bicarbonate ions (HCO3-) in plasma
T/F: The largest amount of carbon dioxide is transported in the bloodstream in the form of carbonic anhydrase.
→ FALSE
7-10% is dissolved in plasma as PCO2
20% of CO2 is bound to the globin part of hemoglobin (carbaminohemoglobin)
70% is transported as bicarbonate ions (HCO3-) in plasma
Role of Bicarbonate
Important buffer of blood pH
Explain Formation of Bicarbonate
Occurs primarily in RBCs, where enzyme carbonic anhydrase reversibly and rapidly catalyzes this reaction
Involves CO2 combining with water to form carbonic acid (H2CO3) → which quickly dissociates into bicarbonate and H+
In capillaries, after HCO3- is created → it quickly diffuses from RBCs into plasma
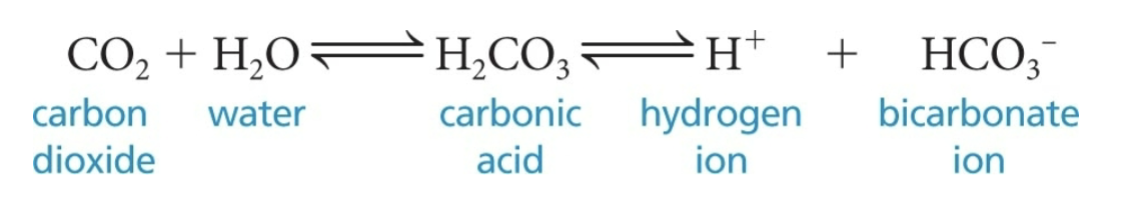
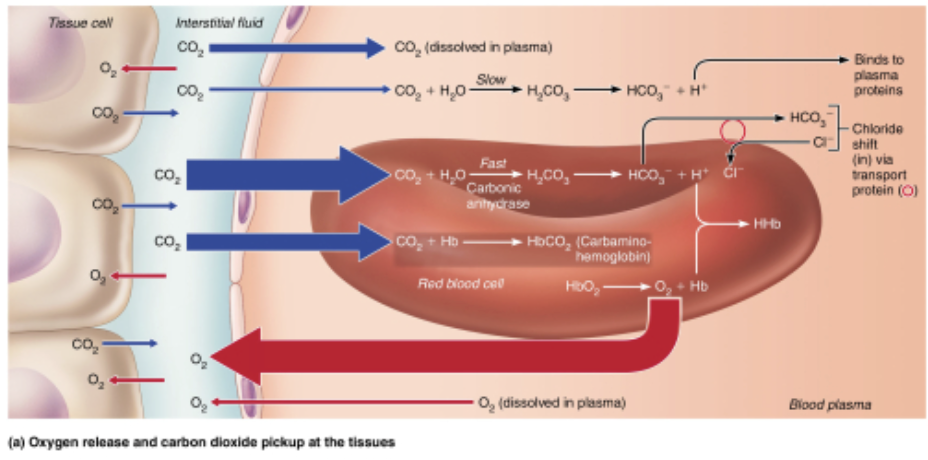
Which of the following best describes the chloride shift as seen in the figure?
Chloride ions rush into RBCs to counterbalance the outflow of bicarbonate ions (HCO3-)
The outflow of negatively charged bicarbonate ions from RBCs is balanced by the inflow of negatively charged chloride ions
Explain Influence of CO2 on Blood pH
Carbonic acid-bicarbonate buffer system → helps blood resist changes in pH
If H+ concentration in blood rises → excess H+ is removed by combining with HCO3- to form H2CO3 which dissociates into CO2 and H2O
If H+ concentration drops→ H2CO3 dissociates, releasing H+
CO₂ + H₂O ⇌ H₂CO₃ ⇌ H⁺ + HCO₃⁻
List Factors the Affect Blood pH
Rapid, deep breathing causes a DECREASE in CO2 in blood → resulting in a RISE in pH
Respiratory rate
Depth
T/F: Breathing plays a major role in acid-base balance of body
→ TRUE
Your patient has several cracked ribs from a car accident, which of these would you expect from his or her blood gases?
A.) Decreased PCO2 and decreased pH
B.) Elevated PCO2 and decreased pH
C.) Decreased PCO2 and increased pH
D.) Elevated PCO2 and increased pH
→ B.) Elevated PCO2 and decreased pH
Cannot take a deep breath, their PCO2 will elevate leading to respiratory acidosis.
Effect and Cause of Hyperventilation
EFFECT
Increased depth and rate of breathing that exceeds body’s need to remove CO2
DECREASE in CO2 in the blood → HYPOCAPNIA
CAUSE
Anxiety attacks
Effect, Cause, and Treatment of Hypocapnia
EFFECT
DECREASE in CO2 in the blood
SYMPTOMS → tingling and involuntary muscle spasms in hands and face
CAUSE
Cerebral vasoconstriction and cerebral ischemia → resulting in dizziness and fainting
TREATMENT
Breathing into paper bag increases CO2 levels being inspired
SUMMARY of Transport & Exchange of CO2 and O2
At the tissues:
O₂ leaves the blood → goes into tissues (where it’s needed)
CO₂ leaves tissues → enters the blood (to be carried away)
In the lungs:
INSPIRATION: O₂ enters from alveoli to blood (to be delivered to the body)
EXPIRATION:CO₂ leaves the blood goes into alveoli (to be exhaled)
Summary of O2 and CO2 Transport
O2
Air enters through the nose or mouth
Air travels down the trachea and then enters the bronchi
Air travels down smaller and smaller bronchioles
Air reaches small sacs (alveoli)
CO2
CO₂ is released from the mitochondria
CO₂ diffuses into a capillary
CO₂ is carried to the lungs
CO₂ diffuses into an alveolus
Air exits through nose or mouth
Summary of O2 Loading & Unloading
Increased Loading
Increased PO2 in the alveoli
Increased surface area of respiratory membrane
Decreased Loading
Decreased ventilation alveoli
Increased thickness of the respiratory membrane
Decreased atm
Increased Unloading
Increased PCO2 in the tissues
Decreased pH in the tissues
Decreased PO2 in the tissues
Decreasing Unloading
Decreased temperature in the tissues
Decreased concentration of BPG
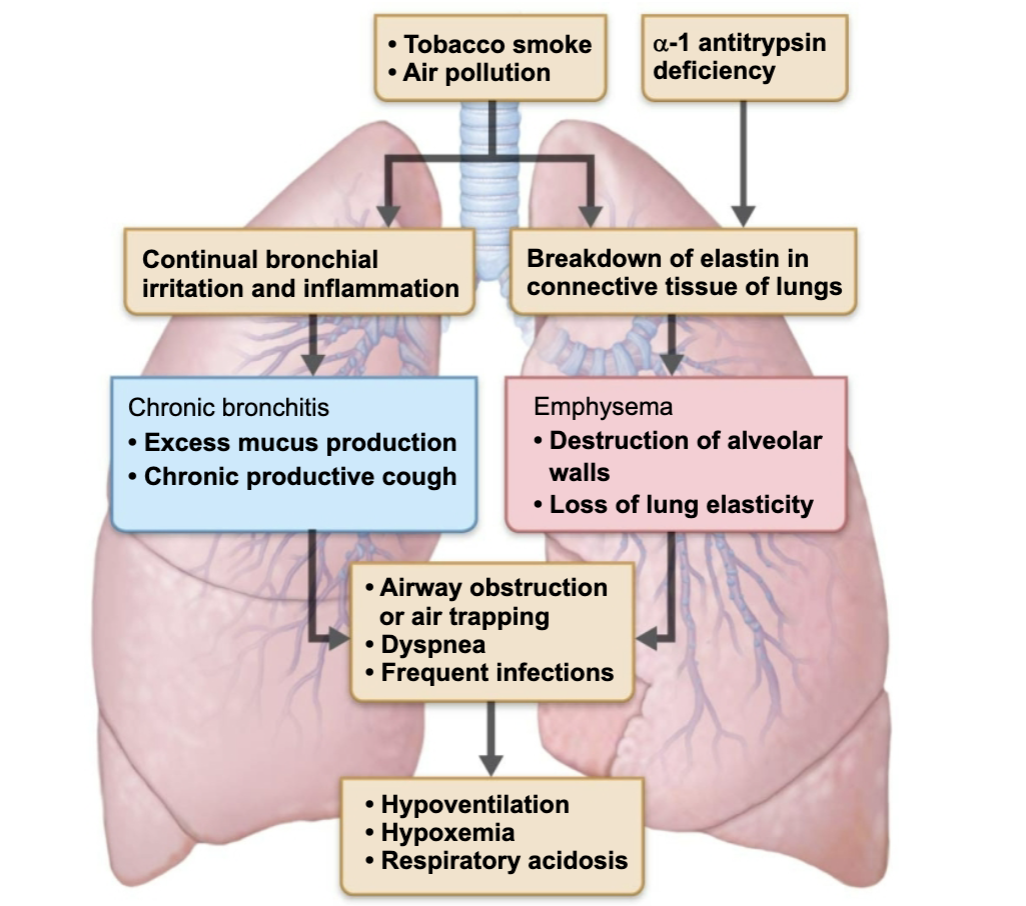
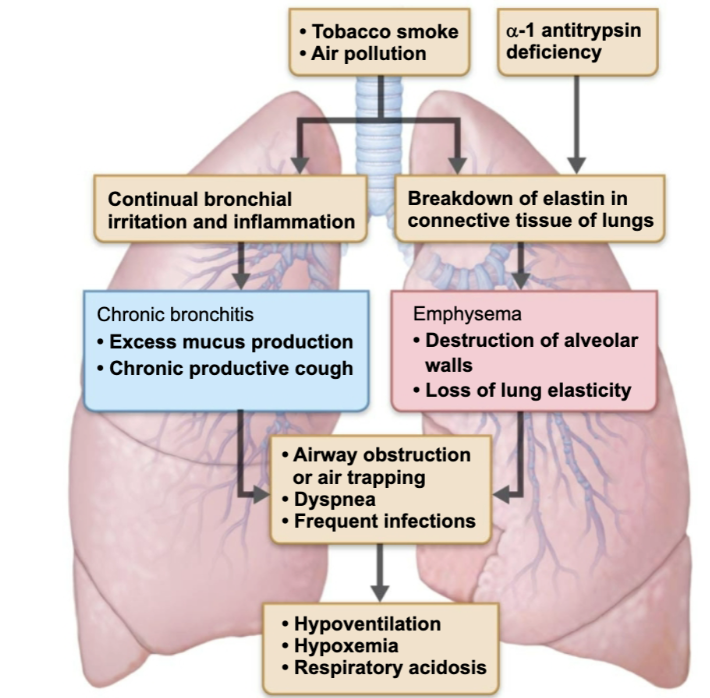
Effect and Cause of COPD
Chronic Obstructive Pulmonary Diseases
EFFECT
Emphysema
Chronic bronchitis
CAUSE
Seen in patients that have history of smoking → result in progressive dyspnea, coughing, and frequent pulmonary infections
Distinguish between Emphysema & Chronic bronchitis
Chronic Obstructive Pulmonary Diseases
Emphysema
Permanently enlarged alveoli and deterioration of alveolar walls
Chronic bronchitis
Results in excessive mucus production, inflammation and fibrosis of the lover respiratory mucosa
Effect and Cause of Asthma
EFFECT
Coughing
Dyspnea
Wheezing
Chest tightness
CAUSE
Active inflammation of the airways
Cause and Effect of Tuberculosis (TB)
CAUSE
Infectious disease caused by the bacterium Mycobacterium tuberculosis
EFFECT
Spread by coughing and inhalation
Effect and Cause of Lung Cancer
EFFECT
In both sexes, long cancer is the most common type of malignancy
CAUSE
Strongly correlated with smoking
SUMMARY of Lung Diseases