CMS I: PULM - EXAM #2 (ALL) | FROM KL QUIZLET
1/152
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
153 Terms
interstitial lung disease is an umbrella term for what diseases?
-idiopathic pulmonary fibrosis (most common one seen)
-sarcoidosis
-pneumoconiosis (asbestosis, silicosis, coal miner's)
chronic interstitial lung diseases can often lead to irreversible ____
interstitial fibrosis
-harder to get air in because lungs lose compliance; TLC decreases
-impaired gas exchange
interstitial lung diseases are diseases of the parenchyma that are commonly caused by
-autoimmune (anything autoimmune like lupus, RA, scleroderma can attack the lungs)
-infections
-drugs
-exposures to inhaled dusts (pneumoconiosis)
most have no specific cause
most common infection that causes interstitial lung diseases
myocplasma pneumonia
drug that can cause interstitial lung disease
amiodarone
insidious dry cough think
interstitial lung disease
-this is the most commonly seen symptom
-lungs are fibrotic/inflamed parenchyma so will be a dry cough; won't be producing anything to cough up
what is the best initial study for interstitial lung diseases? what would you do next?
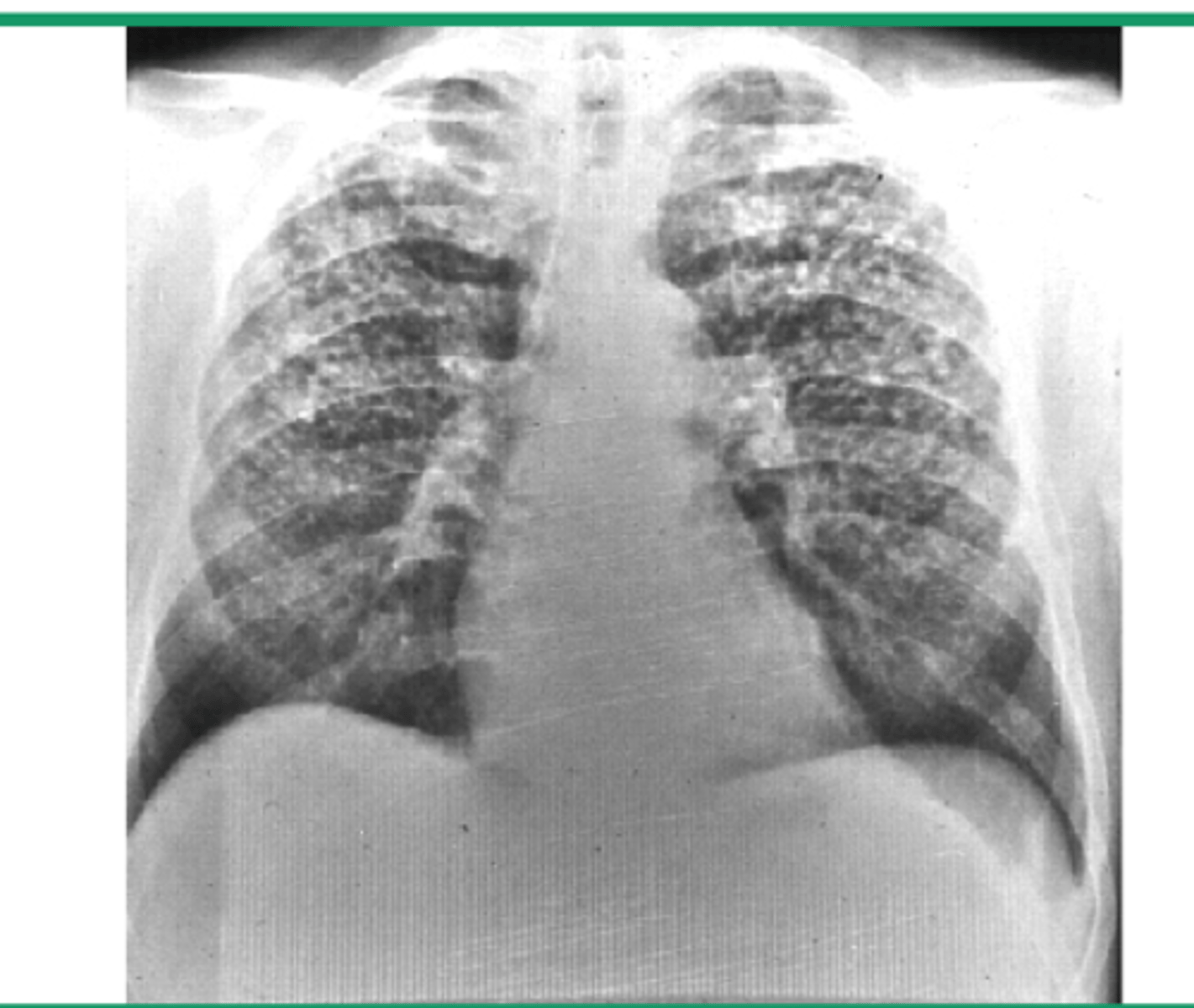
-CXR is always best intial study (would show reticulonodular infiltrates that may progress to honeycomb appearance)
-CT scan would be next to get more details
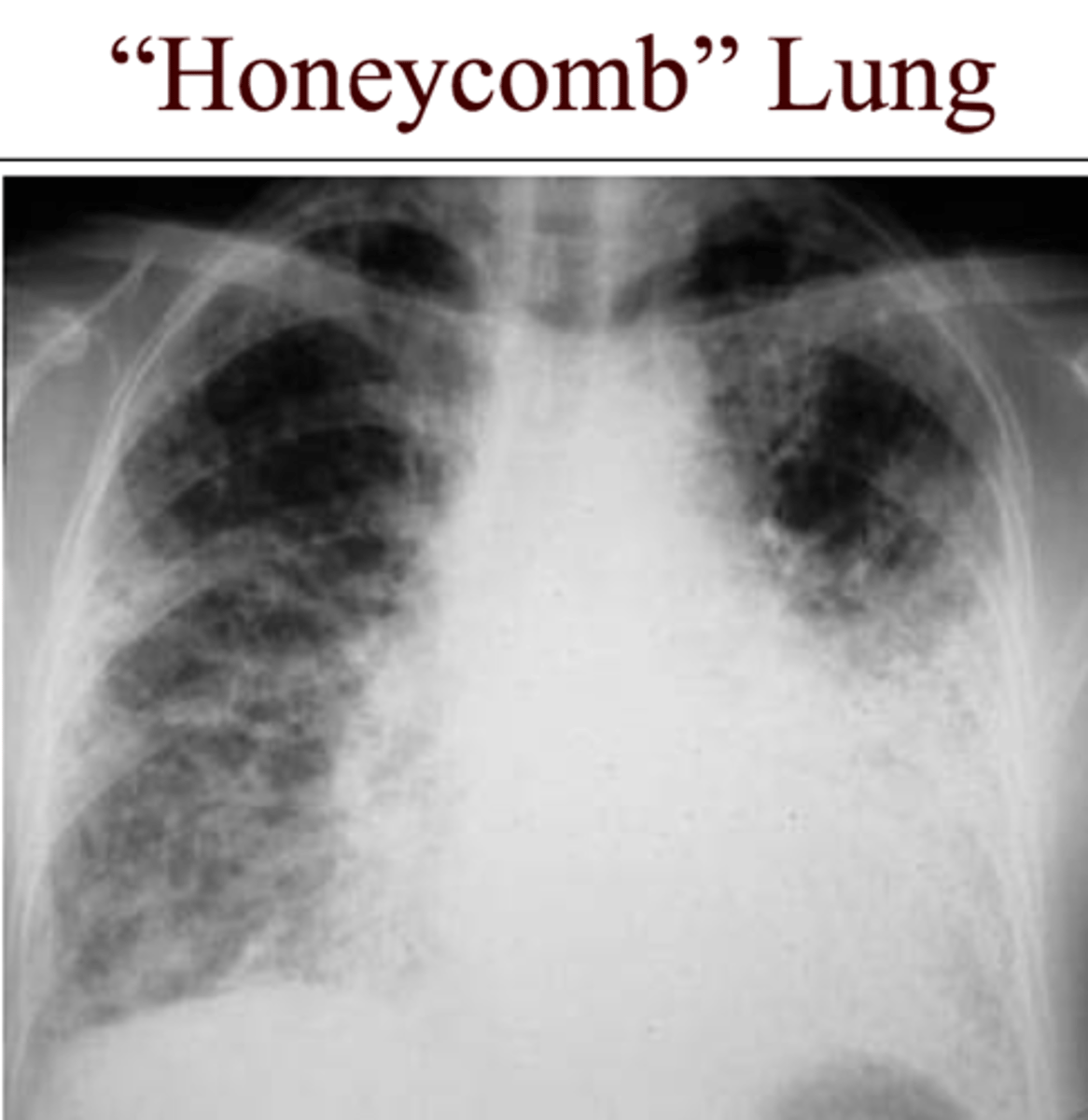
honeycomb/reticulonodular pattern on CXR or CT scan think
interstitial lung disease
common treatment for interstitial lung diseases
-steroids like prednisone/methylprednisolone (decrease inflammation)
-inhaled oxygen (improve symptoms and decrease stress)
-may also do immunosuppressants if you suspect autoimmune cause or antioxidants to help slow decline of the lungs
immunosuppressants vs antioxidants for interstitial lung diseases (know)
-immunosuppressants: azathioprine, cyclophosphamide, methotrexate
-antioxidant: N-acetylcystine (mucomyst); helps to slow decline of the lungs
most important risk factor for idiopathic pulmonary fibrosis
smoking
-not a cause, just a very important risk factor
-more common in men than women also
common physical exam finding for idiopathic pulmonary fibrosis
crackles
(because lung is fibrotic it has a hard time quietly getting air in and out; "crinkling up a water bottle")
-may also see cyanosis and clubbing with advanced diseases
best diagnostic tests for idiopathic pulmonary fibrosis
-CT scan
-PFTs will show decreased FVC and normal FEV1/FVC ratio
why is it important for idiopathic pulmonary fibrosis patients to get influenza and pneumococcal vaccines?
-these patients are immunocompromised and their lungs can't clear pathogens/pollutants as well
polycythemia is a common complication of what lung diseases? (know)
idiopathic pulmonary fibrosis and pulmonary hypertension
-high levels of RBCs form due to low blood O2 levels (hypoxia)
-will see increased hematocrit on CBC; body is trying to compensate by increasing O2 supply to tissues
young african american woman between age 20-40 with lung problem think
sarcoidosis
-also family members are 5x more susceptible to also having the diagnosis
difference between sarcoidosis and TB on CXR (know)
-sarcoidosis will show NON-CASEATING EPITHELIOID GRANULOMAS
-TB will show caseating-central necrosis
-fungal malignancy is also another DDX of sarcoidosis
why may someone with sarcoidosis have a false negative PPD reading for TB?
-depressed cellular immunity (anergy)
-sarcoid is an exaggerated T cell response to certain triggers so T cells being all used up so they won't be able to respond to the PPD---> false negative
Non-caseating granulomas think
Sarcoidosis
-granulomas form from accumulation of inflammatory response to "triggers" (infections, dusts, chemicals)
-overall good prognosis since most granulomas resolve on their own; BUT 20% of patients can develop chronic form
weight loss, fever, erythema nodosum, lupus pernio, uveitis think
sarcoidosis
-very similar presentation to TB except for the nonproductive cough, e. nodosum, and uveitis
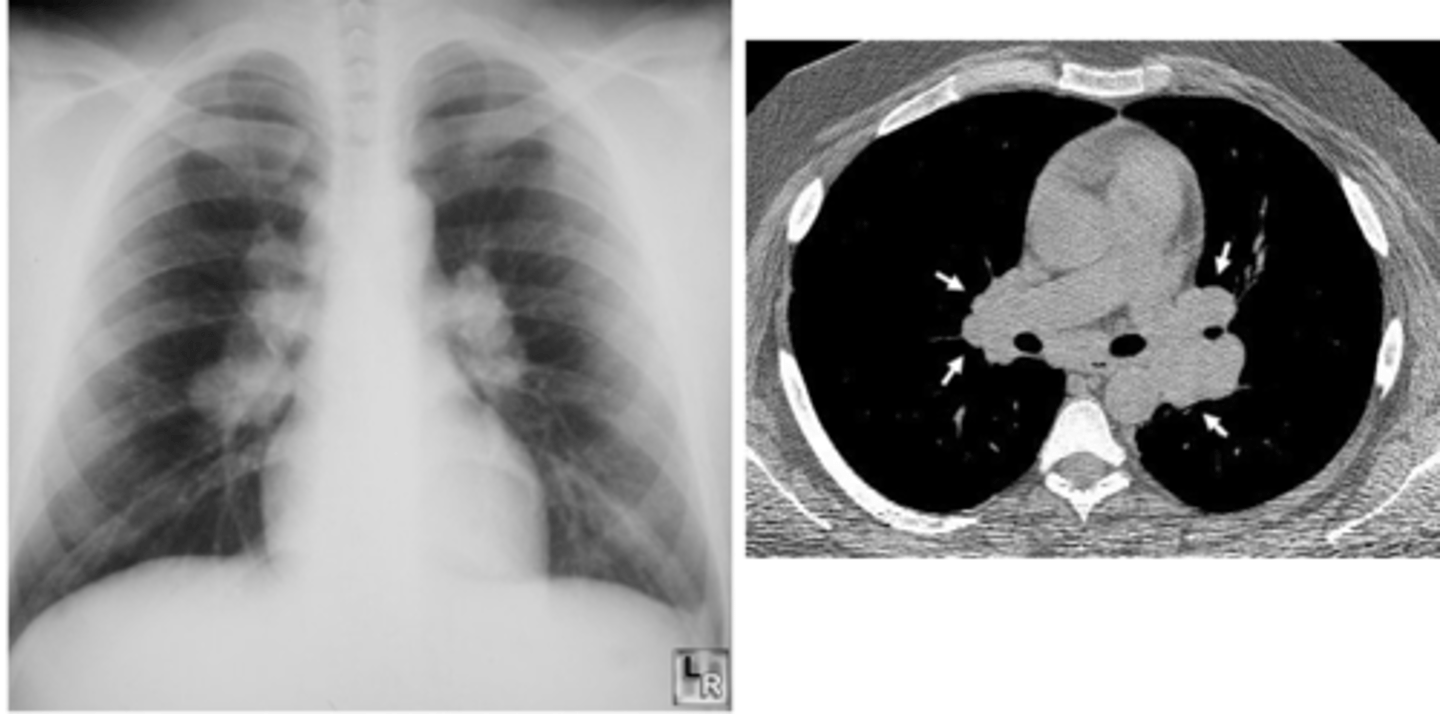
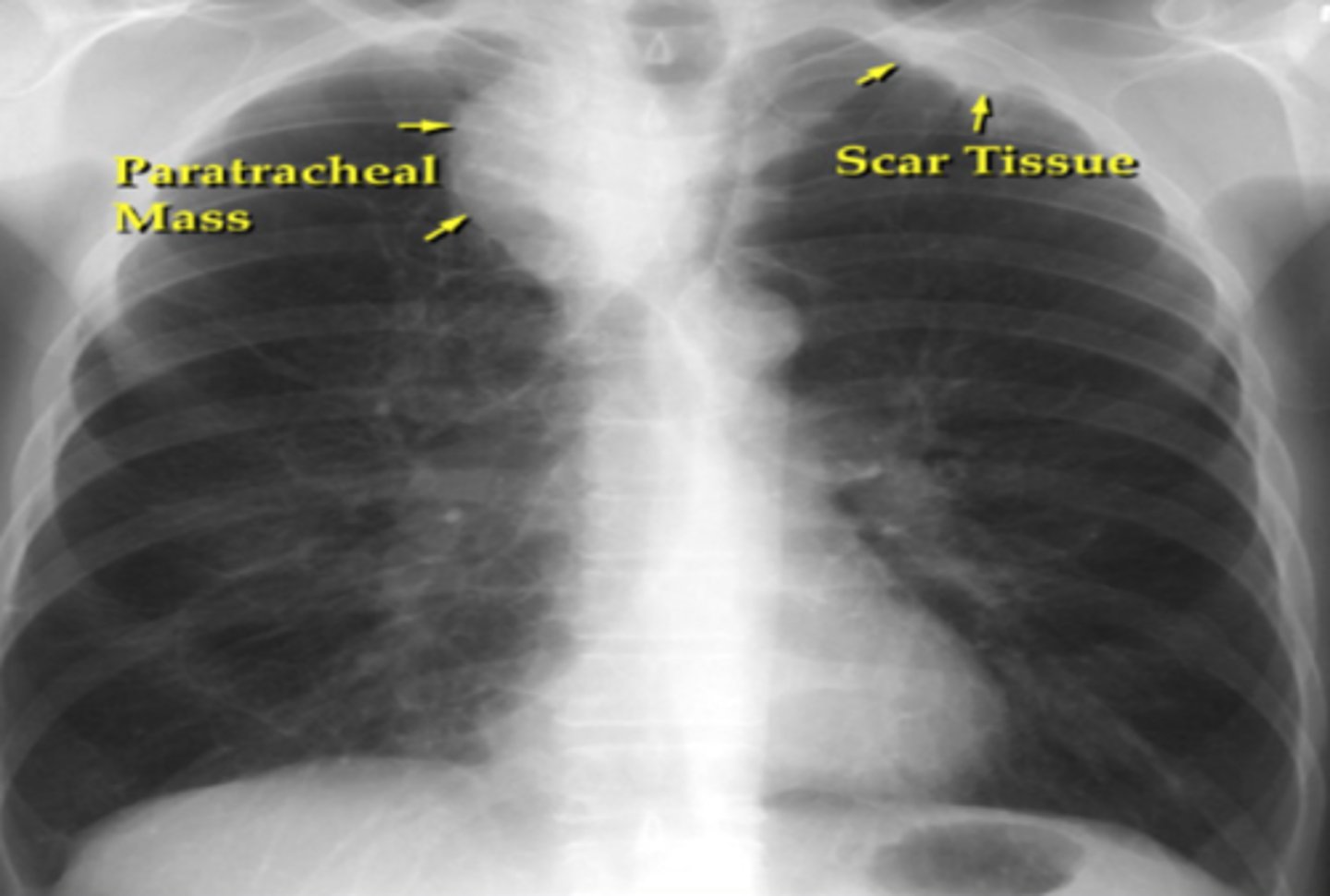
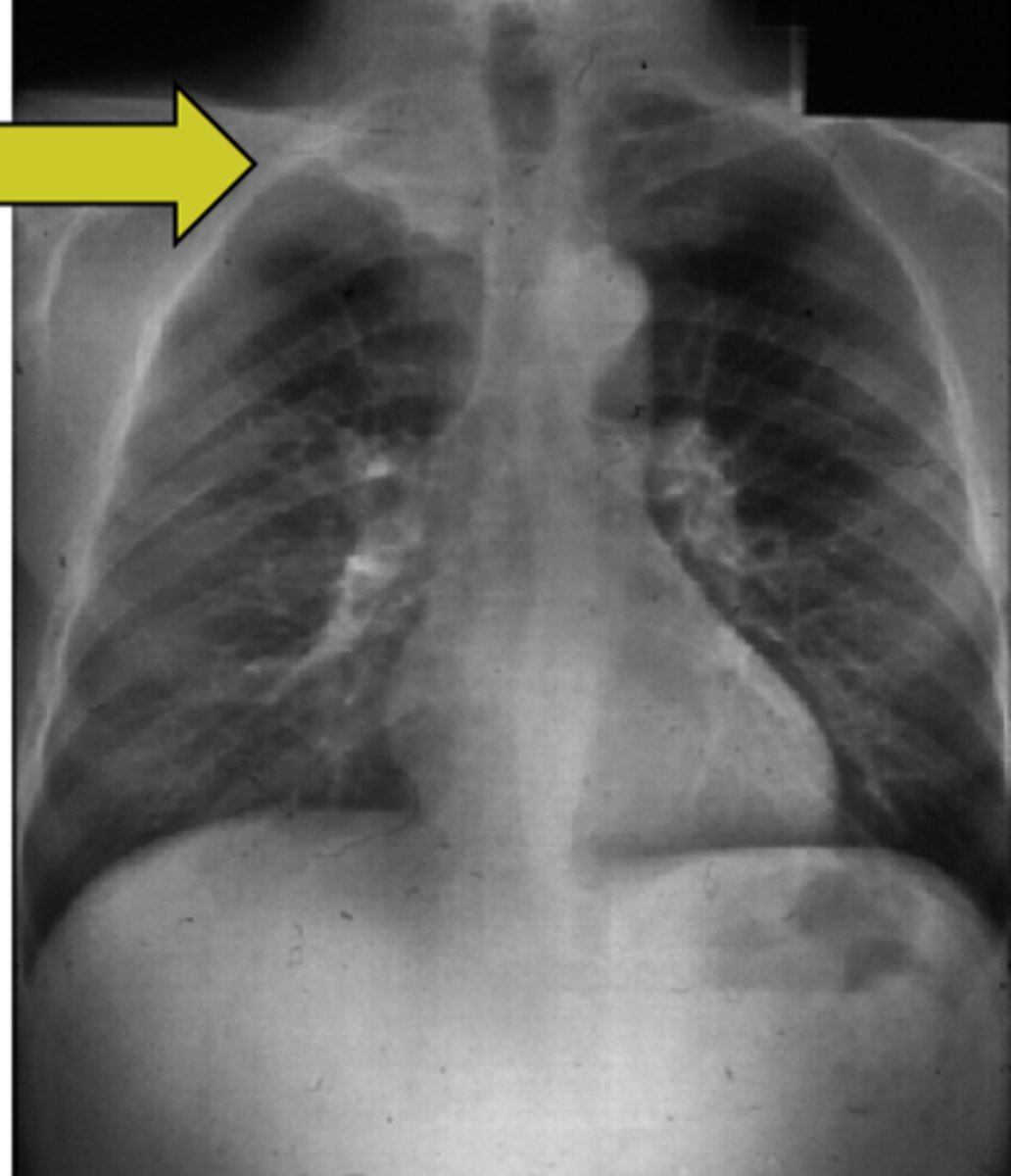
CXR showing bilateral hilar LAD (know)
sarcoidosis!
stage 1 usually
which lung disease will have increased calcium levels (hypercalcemia/hypercalciuria), increased ACE levels, decreased DLCO (diffusion capacity for carbon monoxide), increased bronchioalveolar lavage lymphocytes, and increased ESR (know)
sarcoidosis
-remember ACE is made in lungs and when these granulomas form they stimulate lungs to make more ACE
-exaggerated T cell response caused inc BAL lymphocytes
-inc ESR because inflammatory rxn
sarcoidosis can occur essentially in any organ but most commonly affects the _____
lungs! (2nd most common affected are the lymph nodes, then skin then eyes)
-this is an exaggerated cellular immune response to an unknown antigen
-waxes and wanes; 20% will be chronic so worse prognosis for that 20%
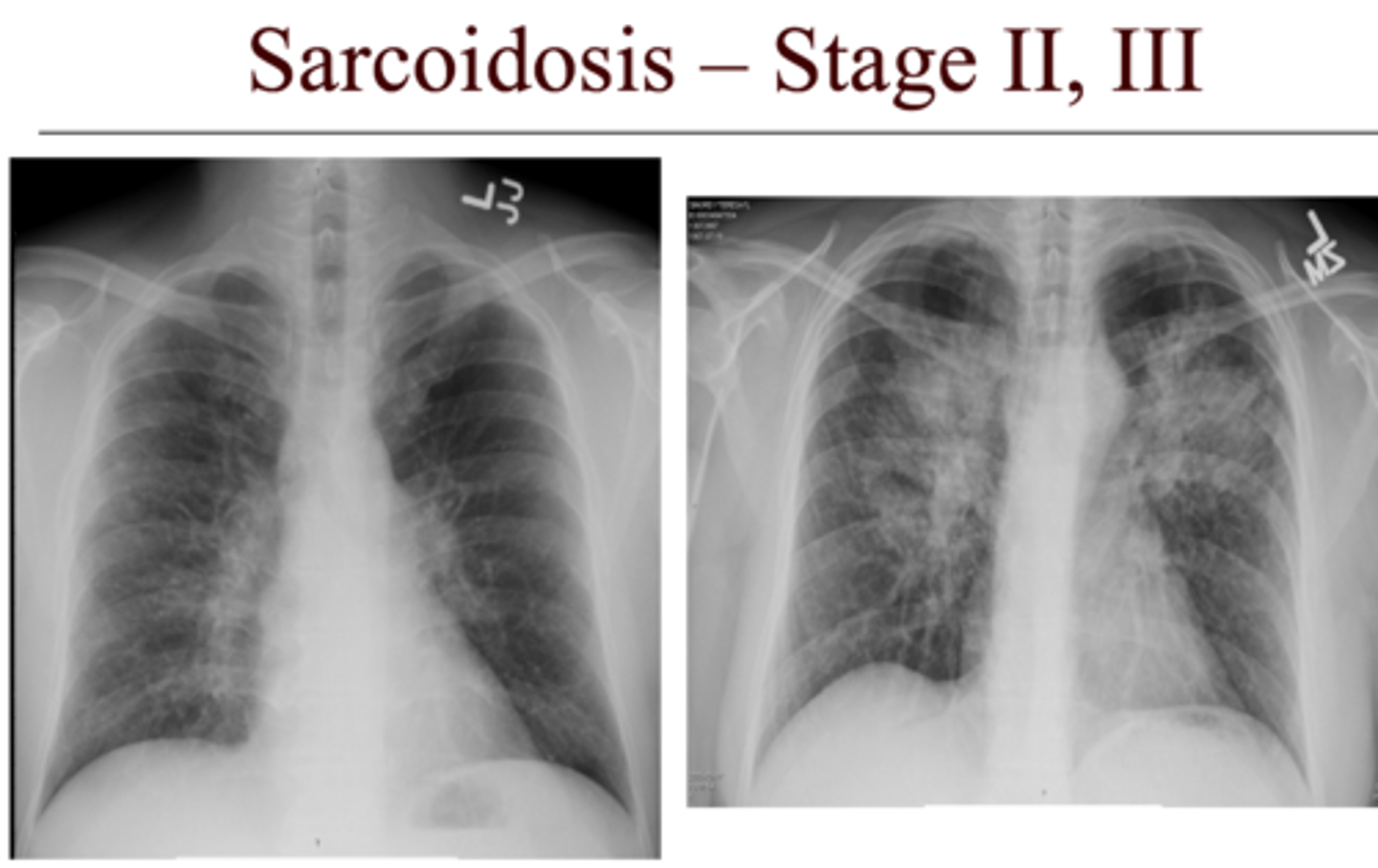
which stage of sarcoidosis in the lungs has the best prognosis? worst prognosis?
-stage 1=hilar adenopathy--> best prognosis
-stage 2= adenopathy + infiltrates
-stage 3= infiltrates (interstitial lung disease)
-stage 4=fibrosis--> worse prognosis
most sensitive test for interstitial lung disease?
-DLCO (diffusion of carbon monoxide in lungs)
would most likely be decreased
lupus pernio and erythema nodosum are skin conditions commonly associated with
sarcoidosis
-lupus pernio: plaques on nose, cheeks, ears---> worse prognosis if patient has this
-E. nodosum: red nodules on the anterior legs --> better prognosis than patients with lupus pernio
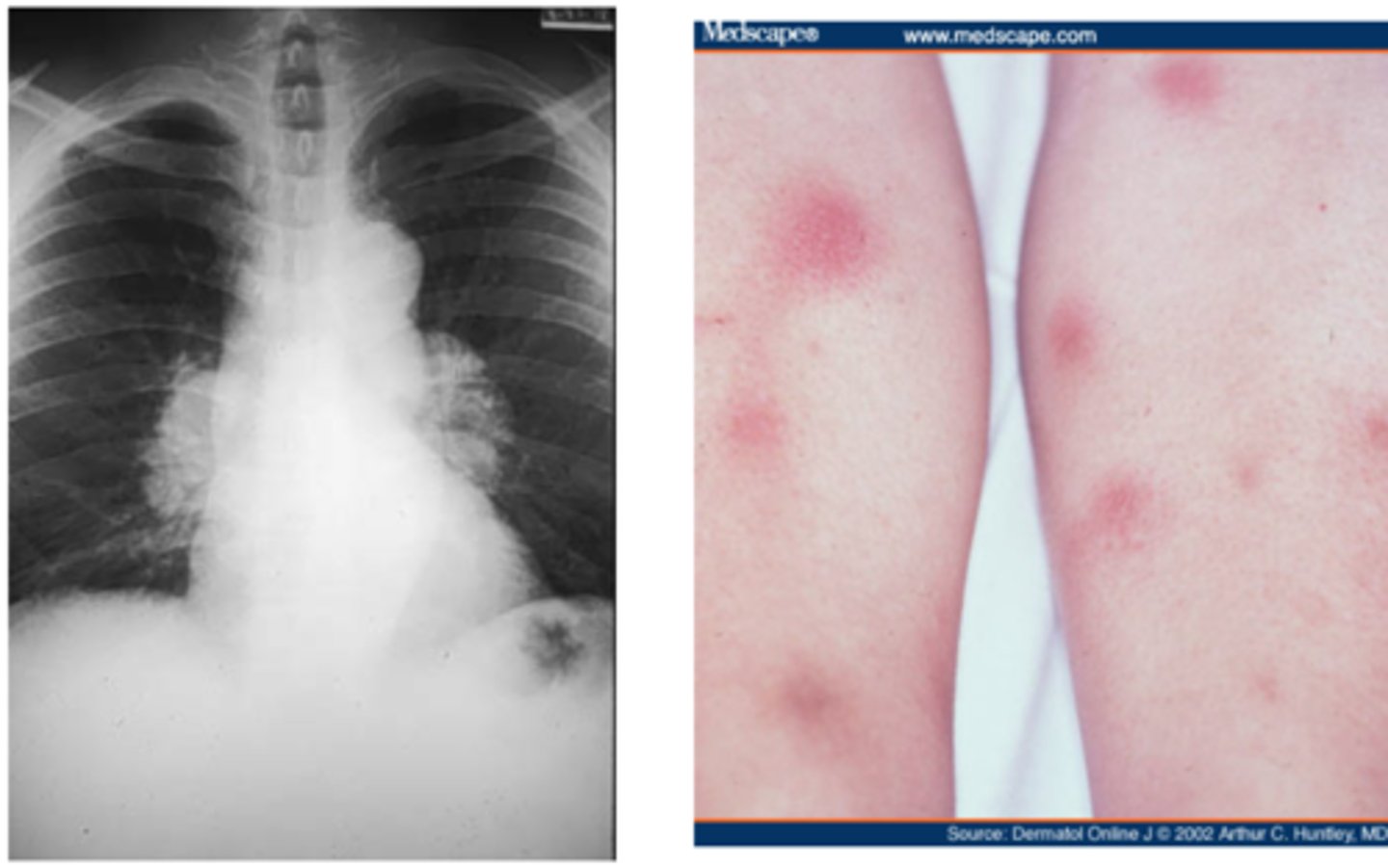
Lofgren's syndrome and Heerford's syndrome are most commonly associated with what lung disease?
sarcoidosis
-Lofgren's syndrome: bilateral hilar adenopathy, E. nodosum, uveitis, fever, arthritis-->good prognosis!!!
-Heerford's syndrome: facial palsy, chronic fever, uveitis, bilateral parotid swelling
cranial neuropathy seen with sarcoidosis
7th nerve: facial nerve paralysis
may also see 8th nerve so can affect hearing
-seen in Heerford's syndrome
how can sarcoidosis cause heart failure?
-can cause restrictive cardiomyopathy to form if granulomas get inside the heart!
-can also cause pulmonary hypertension which can lead to HF
treatment of sarcoidosis
corticosteroids for several months to 1 year
-if pt is diabetic or immune suppressed do steroid sparing agents (methotrexate, hydroxychloroquine)
pneumoconiosis are caused by inhalation of various dusts. The three most important pneumoconiosis include
asbestosis
silicosis
coal worker's
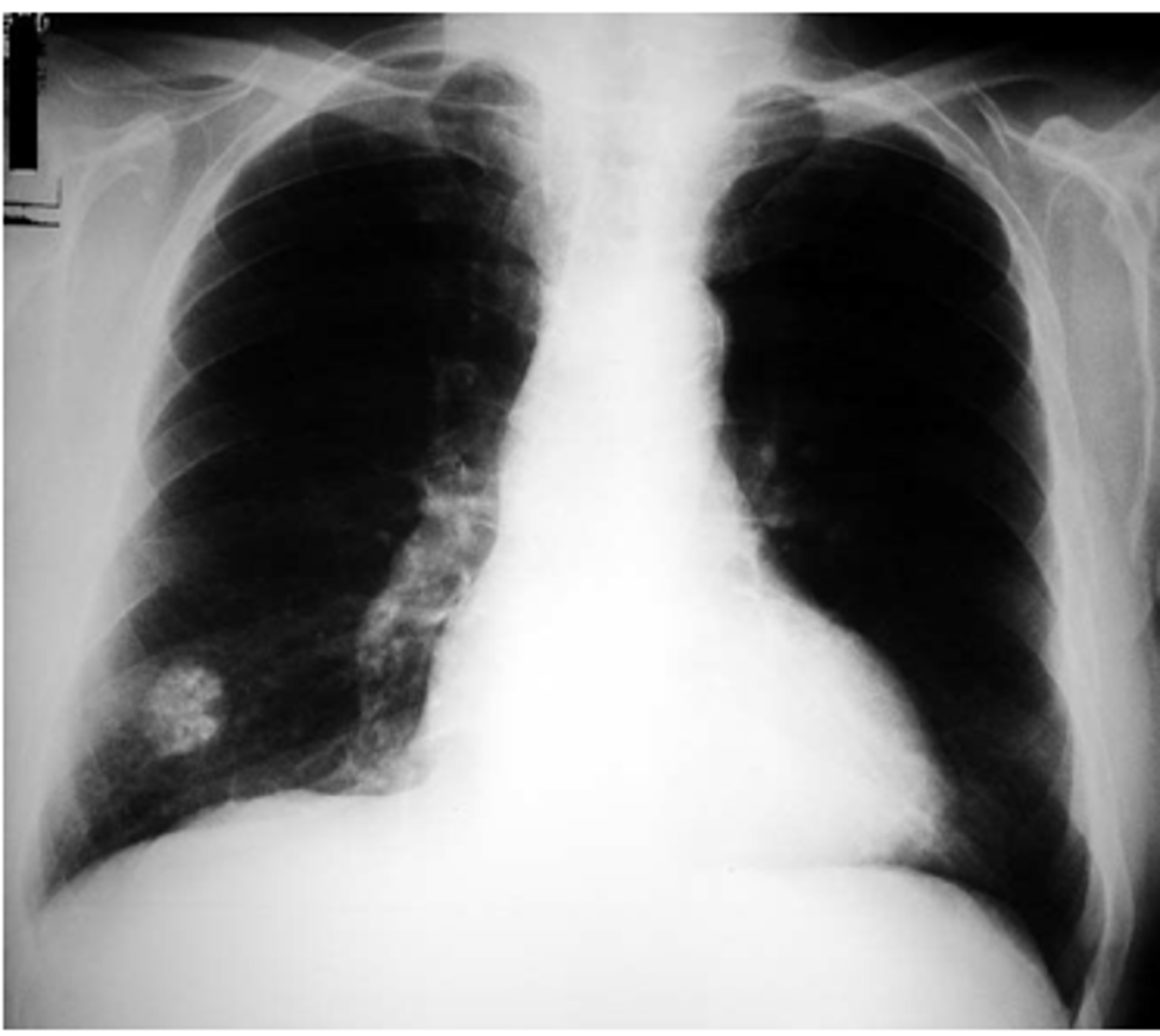
A 75 y/o male comes in presenting with progressive dyspnea, non-productive cough, and crackles on PE. He says that he worked as a ship-yard worker 20 years ago. What is the most likely diagnosis and what would you see on imaging studies?
asbestos! (exposure occurs in ship-yard workers, demolition workers, milling, etc); severity is directly related to intensity and duration of exposure
-minimum of 10 yrs before the disease starts to manifest
-CXR/CT would show honeycombing on BOTTOM PART OF LUNG or pleural plaques
-asbestosis always starts in lower lung but can end up in upper lung also

what is a severe consequence in the long run with any lung disease?
cor pulmonale
-often seen from asbestosis interstitial lung disease if left untreated
pleural plaques in lower lung fields (irregular thickening/calcification of parietal pleura) on CXR indicate
EXPOSURE to asbestosis not necessarily lung impairment
-these plaques are best evaluated by CT scan

1. what type of lung cancer can only be caused by asbestos exposure?
2. what is the most common cancers associated with asbestos?
1. mesothelioma (rare pleural malignancy only caused by asbestos exposure); mesothelioma and asbestos have a strong link
2. SCC and adenocarcinomas are the most commonly seen lung cancers in patients with asbestos exposure
patient who has a lung complaint that worked in sandblasting (exposure to silica/quartz), stone cutting, stone quarrying think
silicosis
what lung disease has a very high risk for TB and atypical mycobacterium disease? (know)
silicosis! (silica/quartz/granite exposure)
-30 x increase chance of TB in silicosis
what is the most common pneumoconiosis?
silicosis!
-silica is the MOST abundant mineral on earth; inhaling this puts you at risk for silicosis
nodules resembling onion skin think
silicosis!
-macrophages engulf silica--> macrophages die-->silca released into interstitial tissue--> nodules form around bronchioles--> "onion skin"
main way to tell the difference between silicosis and coal miner's
-CXR of silicosis will show EGG-SHELL CALCIFICATION on hilar lymph nodes
-both occur in top parts of lungs but egg shell appearance is specific to silicosis
eggshell calcifications in upper lobe of lung think
silicosis
patient who had years of exposure to coal dust think
coal worker's pneumoconiosis
-like silicosis, has high risk for TB
-looks similar to silicosis on CXR; but silicosis has egg shell calcifications
why are patients with silicosis and coal worker's pneumoconiosis are higher risk for TB?
-these diseases are in the upper lobes of the lung which is also where TB likes to be; these diseases destroy the lung tissue making it easier for TB to get into it
progressive massive fibrosis in the upper lung zones is a common complication of
coal worker's pneumoconiosis
-inhaled coal dust is ingested by alveolar macrophages which leads to formation of coal macules in upper lobes
which lung disease is associated with Caplan's syndrome? (know)
coal workers pneumoconiosis
-caplan's syndrome is seen in patients with rheumatoid arthritis and coal worker's
which type of cancer is the leading cause of cancer death in both men and women?
lung cancer
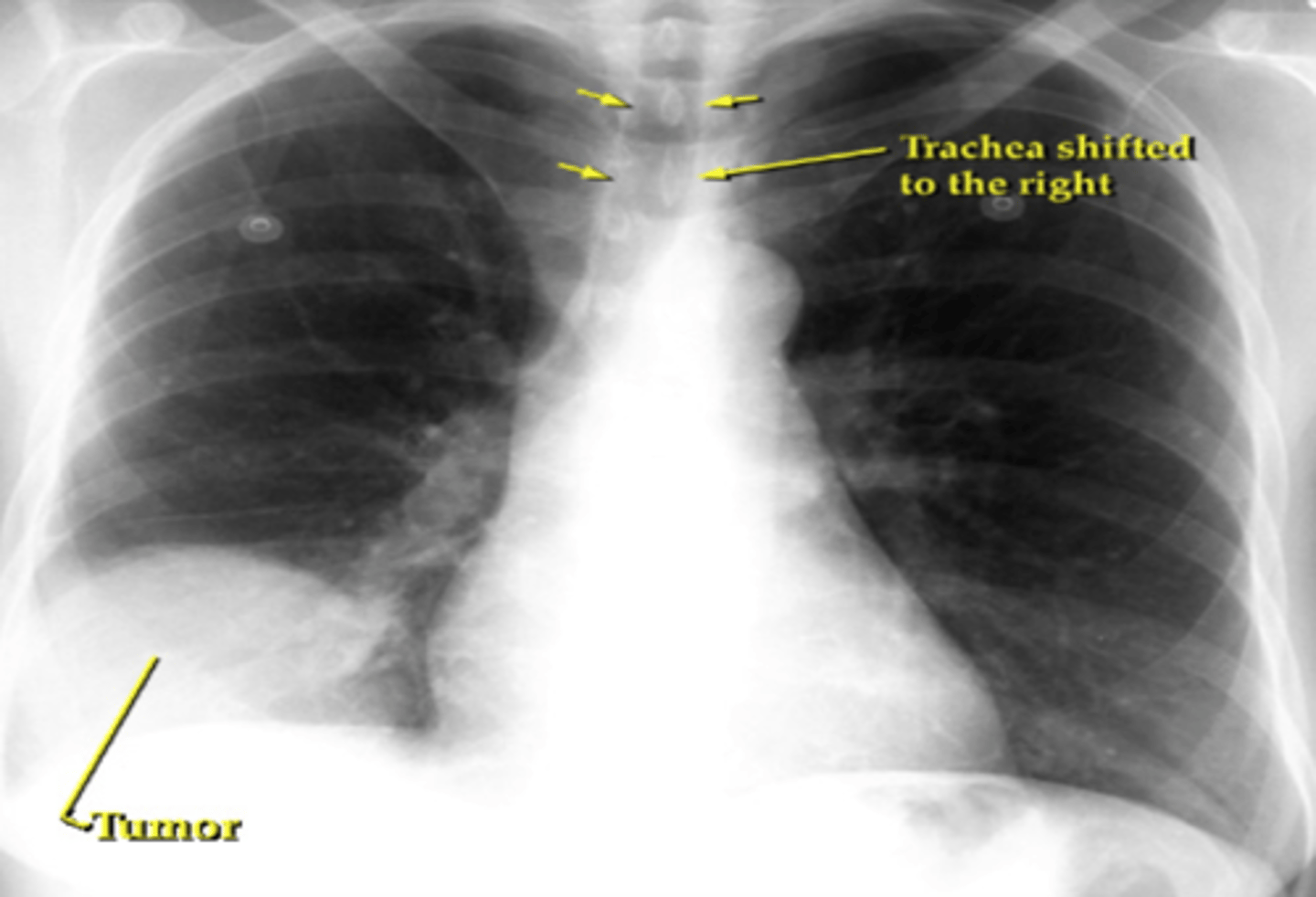
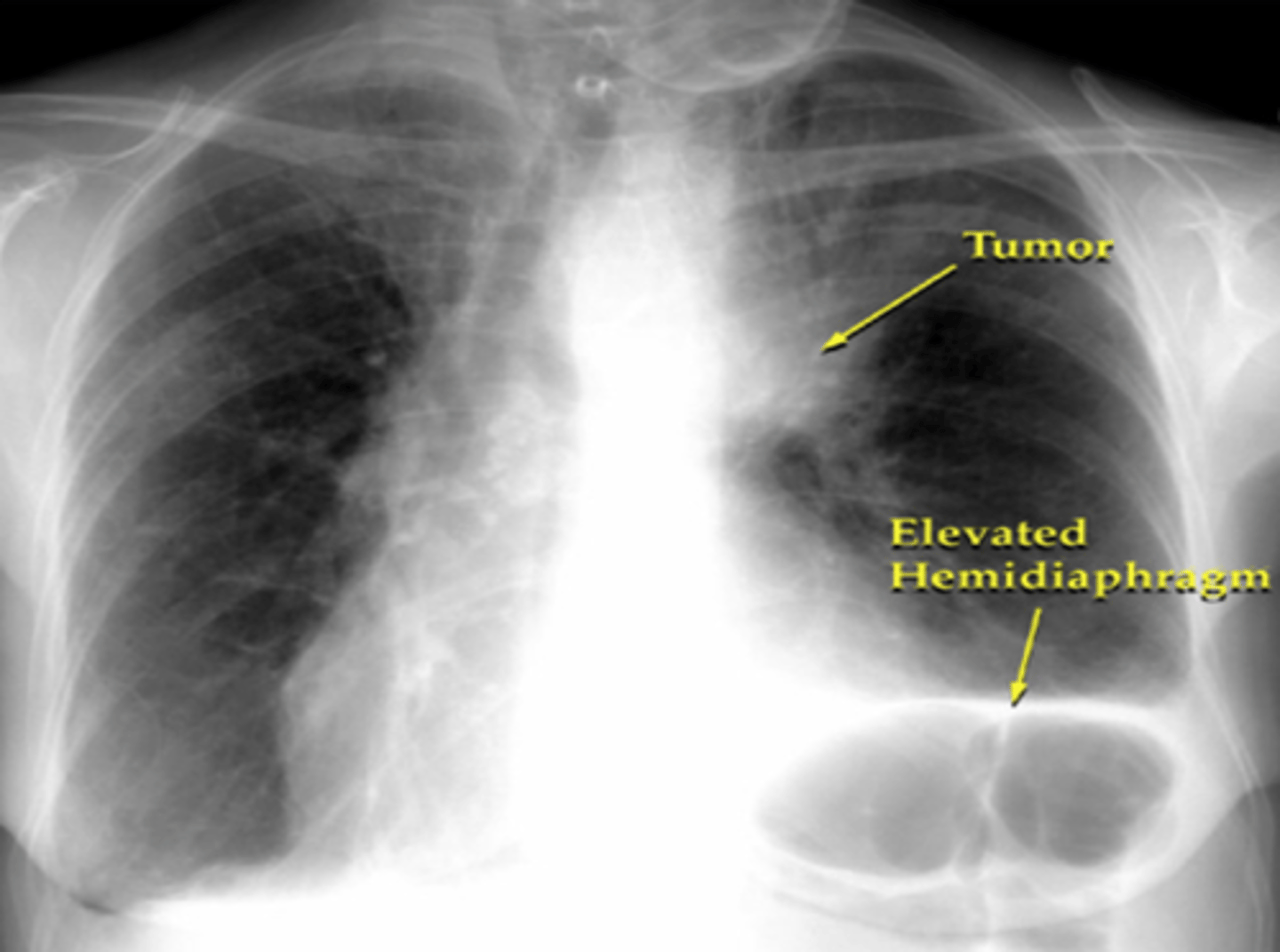
-4 types: adenocarcinoma, SCC or epidermoid carcinoma, small cell (oat cell), large cell carcinoma
-grouped as small cell and non-small cell which includes everything else
most common form of lung cancer and where is it found (know)
adenocarcinoma
-found in periphery of lungs
-small cell/scc usually found central
which type of adenocarcinoma is often mistaken for interstitial pneumonia and missed?
bronchioloalveolar carcinoma (BAC)
-subtype of adenocarcinoma
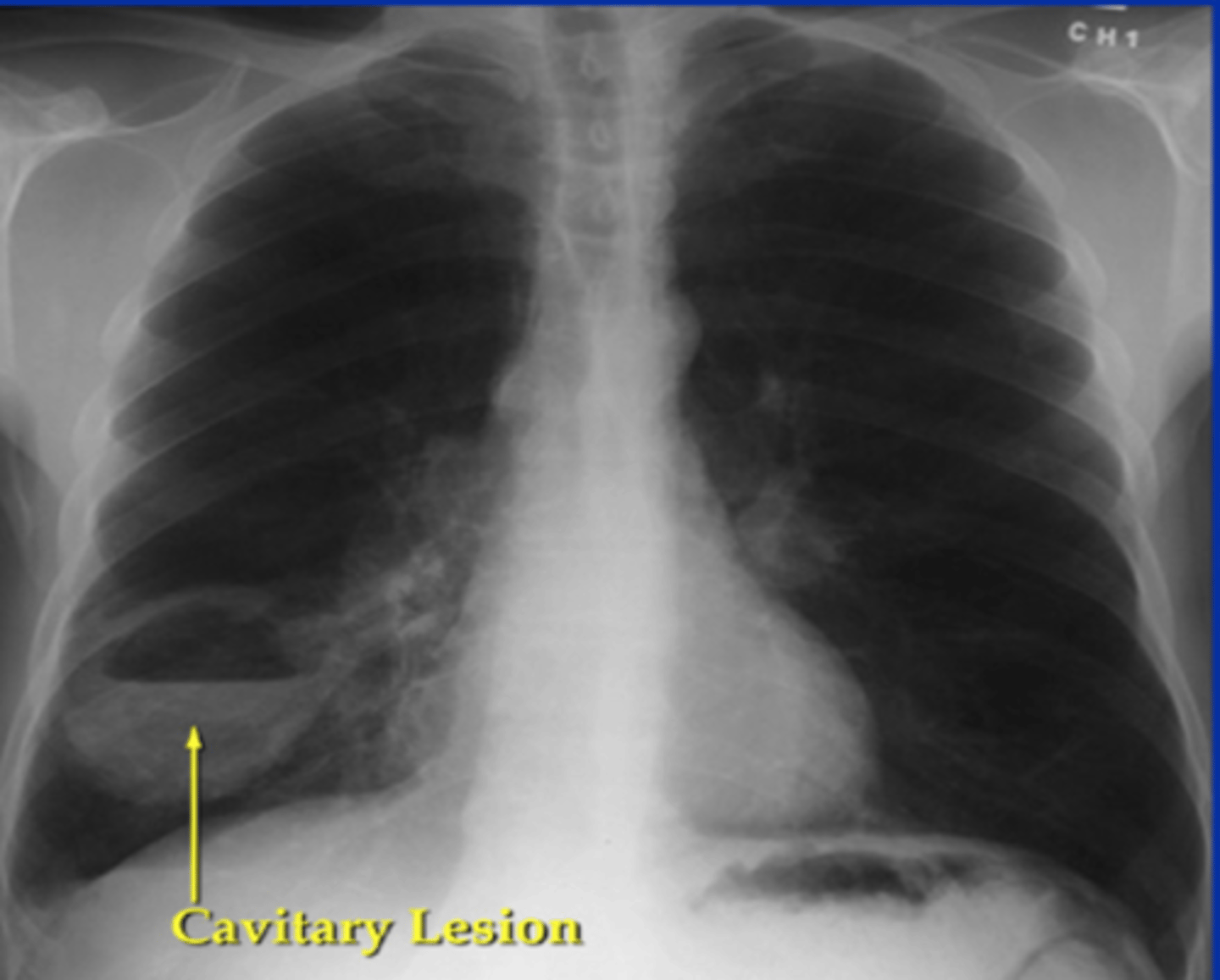
CCCP for recognizing SCC (know)
-Central
-Cavitary
-hyperCalcemia
-Pancoast syndrome (evolves from SCC usually, mass seen in apex of lungs)
high calcium always think
cancer!
what is the staging system for small cell carcinoma; why does it have this staging system?
2 stage system:
-limited-stage disease (30% of people; one hemithorax and regional lymph nodes involved)
-extensive-stage disease (70% of people; disease is beyond hemithorax and regional lymph node bounderies)
small cell has different type of staging because it is so aggressive compared to the other cancers; risk for early metastasis
lung cancer that can present as peripheral OR central; has rapid doubling time and very aggressive; may also cavitate
large cell
-not much is known about it
if a suspected lung cancer is shown as a cavitary lesion in the periphery of the lungs it is most likely a _____
large cell; can be peripheral or central
-remember SCC would cavitate but it is only centrally located
would have to get bx to know for sure!
common signs/symptoms of lung cancers
-weight loss, new or changing cough, hemoptysis, pain
-especially suspicious of cancer in a patient with these symptoms who smokes
1. metastasis is most commonly found in what lung cancer?
2. where do the mets typically spread?
1. small cell cancer
2. brain, liver, lymph nodes, bone, etc)
most common sign of secondary lung cancer
pleural effusion!
(exudative pleural fluid most likley cancer)
these paraneoplastic syndromes most commonly seen in what lung cancers: (KNOW)
1. syndrome of inappropriate secretion of antidiuretic hormone (SIADH)/hyponatremia
2.cushing's syndrome (hypercortisolism)
3. hypercalcemia
4. gynecomastia
5. eaton-lambert syndrome
1. small cell
2. small cell (due to ectopic ACTH production)
3. SCC
4. adenocarcinoma
5. small cell (neurologic-->decreased strength)
superior vena cava obstruction is most common in what lung cancer?
small cell
-tumor causes progressive obstruction of the venous drainage of the head, neck, and upper extremities
neuroendocrine tumor (NET) mostly found in GI tract but can also be found in lungs (know)
carcinoid tumors
atypical vs typical carcinoid tumors
-atypical: notorious for mets in 70% of cases
-typical: slow growth and low risk of mets-->BETTER PROGNOSIS
larger the NET, the poorer prognosis; overall these tumors have better prognosis compared to other cancers of lung
lung cancer that may have focal wheezing and flushing, diarrhea, hypotension
carcinoid tumors
-flushing, diarrhea, hypotension=carcinoid syndrome; due to a lot of serotonin being released from the neuroendocrine tumor!
pink/purple tumor that is well vascularized think
carcinoid tumor
-since these are so vascular, difficult to biopsy! always type and screen before taking biopsy if this tumor is expected
lung cancers that are RESISTANT to radiation and chemo and can ONLY be treated with surgery (know)
carcinoid tumors (surgical removal is only treatment)
lung cancer that can't be treated with surgery due to rapid metastasis (know)
small cell!
-therefore, radiation/chemo is ONLY treatment option
a patient comes in with pain in the lower part of the shoulder. You do a CXR and see a mass in the extreme apex of the lung. What is the most likely diagnosis
pancoast tumor (non-small cell tumor of the superior sulcus)
-tumor often presses on brachial plexus--> pain and sensory loss of shoulder/arm
-may also see patients with this cancer who have hoarse voice from tumor pushing on laryngeal nerve
what is horner's syndrome and which lung cancer is it seen in? (know)
Horner's syndrome= ptosis, miosis, anhydrosis
-seen with pancoast tumors; further neurological involvement
lung cancers that are treated with preop and postop radiotherapy
pancoast tumor
-preop RT to shrink the tumor before cutting it out
-postop RT to kill whatever may be left behind
what is used to get a definitive diagnosis for any cancer (know)
cytology (biopsy)
-knowing specific cancer type is ESSENTIAL in determining staging, treatment, prognosis
when performing a biopsy of a suspicious lesion, when would it be best to do a bronchoscopy? transthoracic needle biopsy? mediastinoscopy? (know)
-central lesions are better biopsied with bronchoscopy
-peripheral lesions are better obtained w/ transthoracic needle biopsy (adenocarcinoma)
-mediastinoscopy is reserved for harder to reach tumors
what imaging is best when looking for METs and recurrence
PET scan (positron, emission tomography)
-metabolically active areas will light up more
staging for non-small cell carcinomas (know)
TNM system
-T: tumor size
-N: nodal involvement
-M: metastases
stage I-IIIA (IIIA is where it is really bad)
2 major parts of staging lung cancer
1. anatomic staging (location)
2. physiological staging (assessing patient's immune system)
important for resectability (if you can remove the tumor or not) and operability (if patient can actually handle surgery)
in TNM staging what does MX, M0, and M1 mean?
MX: distant metastases cannot be assessed
M0: no distant metastases
M1: distant metastasis present(any time M1 is present means it is stage IV)
what tests should always be done before surgically removing lung cancer?
-remember surgery is tx of choice only for non-small cell cancers
-all surgical candidates should have PFTs and ABGs done before resection; need baseline pH and CO2 before affecting airway
if a patient has stage IV adenocarcinoma would surgery still be the treatment of choice?
no! although surgery is usually the tx of choice in non-small cell cancers, stage IV means metastasis are involved; therefore surgery is no longer an option; needs chemo/radiation
in which lung cancer should prophylactic cranial radiotherapy be done?
small cell (don't want to risk cancer spreading to the brain)
-combo of chemo + radiation=treatment of choice!
-can NOT do surgery on this type
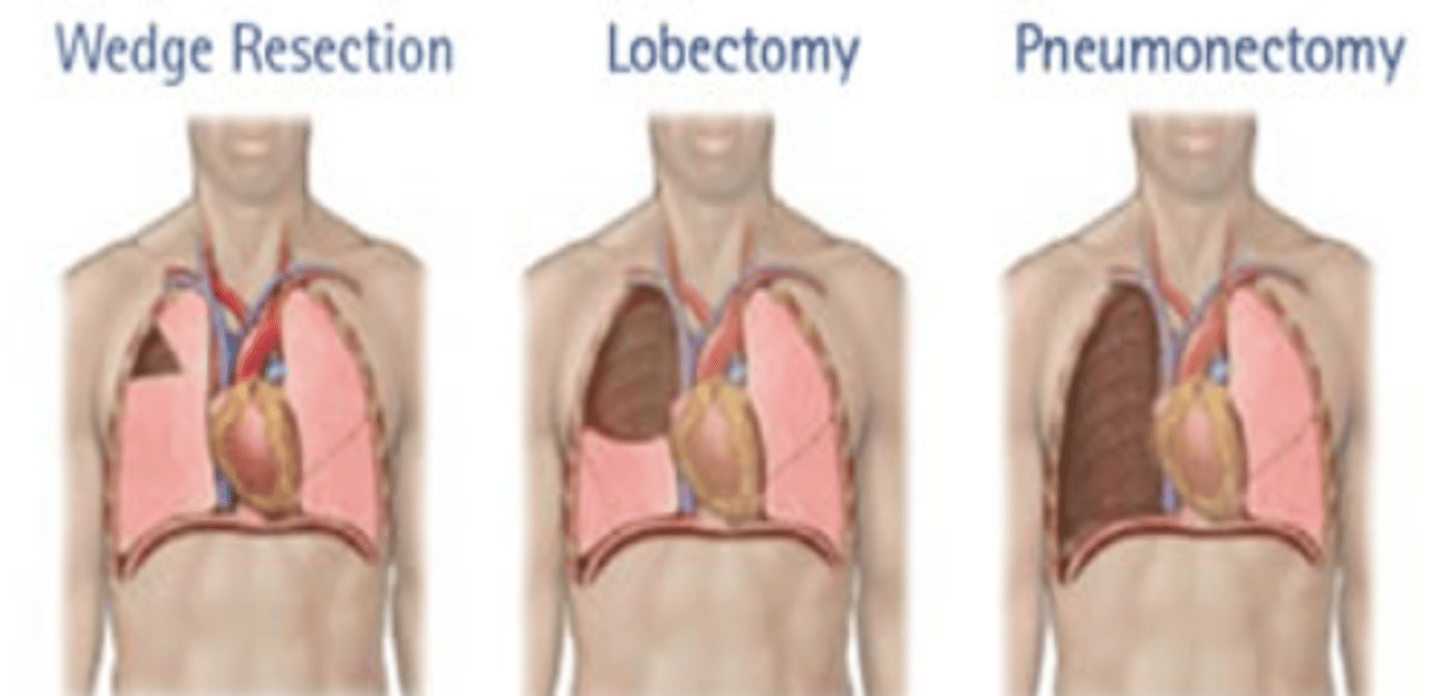
procedure of choice for most lung cancer surgical resections
lobectomy
-lobectomy superior to wedge resection may also be done (for patients with limited reserve)
which type of non-small cell cancer does best with resection?
SCC!
-better survival compared to adenocarcinoma or large cell
what population should receive annual screening for lung cancer with a low dose CT scan
individuals with at least a 30 pack year smoking history starting at age 55-80
-if it has been > 15 years since the patient has smoked-->no CT
-if patient has other comorbidities that could shorten their lifespan--> no CT
sputum cytology and CXR are NOT routine for screening
characteristics of a benign pulmonary nodule (know)
- < 8 mm in size
- dense central calcification
- sharply circumscribed
- isolated
- pt is less than 30 yrs old
- non smoker
most common benign lung tumor and what will it show on CXR?
hamartomas
peripheral popcorn calcifications on CXR
-only tx is surgery but HIGHLY VASCULAR so only remove if causing problems!
-other common benign mass are bronchial adenomas
most benign pulmonary nodules are
granulomas!
first and most important step of diagnosing a pulmonary nodule? (know)
comparison with old films!!
a 20 yr old patient presents with a 5 mm pulmonary nodule with sharp borders. The patient has no history of smoking or any other comorbidities. What should be done?
pt is under 35 and has no prev smoking history= low probability for malignancy
-serial CXR q 3 months x 1 year then q 6 months x 1 year
treatment of pulmonary nodules in low, intermediate, and high risk patients
low (under 30, no smoking hx)
-serial CXR q 3 mos x 1 yr then q 6 mos x 1 yr; if still no change can stop following
intermediate
-bronchoscopy, trans thoracic biopsy, PET scan
high
-resection
risk of malignancy of pulmonary nodule increases with
-size (> 1-2 cm)
-age (>35)
-smoking hx
-absence of calcification
lack of growth for over 2 years of observation by CT scanning--> no further work up needed
most common source of pulmonary embolism
lower extremities; deep calf veins (anterior/posterior tibial veins and peroneal veins) (DVT)
-greater risk with proximal thrombus since easier to miss this when doing venography
Virchow's triad (know)
1. venous stasis (long car rides, flights, bed ridden)
2. hypercoaguable state (cancer, pregnancy, OCPs, Estrogen therapy, smoking)
3. vascular injury/inflammation (surgical procedures)
**pt also at risk if prev DVT/PE or if they have had trauma/surgery in the last 4 weeks
Saddle embolus
sudden death due to clot in between the right and left pulmonary arteries
a patient with a PE may retain more CO2 due to impaired gas exchange. What happens to compensate for this?
patients will increase minute ventilation--->hyperventilation--> relative hypocapnea--> respiratory alkalosis
-may also see increased pulmonary vascular resistance due to vascular obstruction and/or neurohormonal agents (surge of catecholamines)
why is hypotension and tachycardia often seen with pulmonary embolism
-inc pulmonary vascular resistance and pulmonary vasoconstriction--> decrease in RV output--> RV failure-->dec CO/SV-->hypotension; tachycardia occurs to compensate to hypotension; still trying to get blood to organs
obstruction of vascular bed and reflex vasoconstriction are a hemodynamic effect of
pulmonary embolism
-this results in inc pulm vascular resistance and can cause pulm HTN and RVF
what should you expect if a patient with a PE is experiencing respiratory acidosis and hypercapnea
shock!
Hampton's hump and westermark's sign on CXR think
PE
-Westermark's sign= collapse of vasculature distal to the embolus and dilation of vasculature proximal to the embolus
-Hampton's Hump= wedge shaped infarct
-may also see atelectasis at bases or pleural effusion

normal CXR + hypoxia think
PE!
-often won't cause CXR findings unless it's very big
-CXR usually just done to r/o other causes for presenting symptoms
-CXR is NOT used to diagnose PE
most common symptom of PE
sudden onset of dyspnea
-may be with exertion or at rest
other common symptoms include pulse ox < 95% and unilateral extremity discomfort
a 25 yr old caucasian female who is a non-smoker, not on OCP/estrogen therapy, no prev surgeries/trauma, no pregnancy, and no obesity presents with symptoms of a pulmonary embolism. How is this possible?
the patient most likely has Factor V Leiden deficiency
-this is the most common inherited cause of PE in caucasians
-normally factor V leiden breaks down clots
pulmonary embolism rule-out criteria (PERC)
-age < 50
-HR < 100 bpm
-no prior DVT/PE
-no recent trauma/surgery (last 4 weeks)
-no hemoptysis
-no exogenous estrogen
-no clinical signs suggestive of DVT
**if all 8 present only 1 % risk of PE
Homan's sign
used to assess DVT
-calf pain with passive, forcible, dorsiflexion of foot with knee flexed
-non-specific!!
most common EKG finding with pulmonary embolism
sinus tachycardia!!
-compensating for hypotension
may also see T wave inversion in V1-V4