conjunctiva I - infective conjunctivitis
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
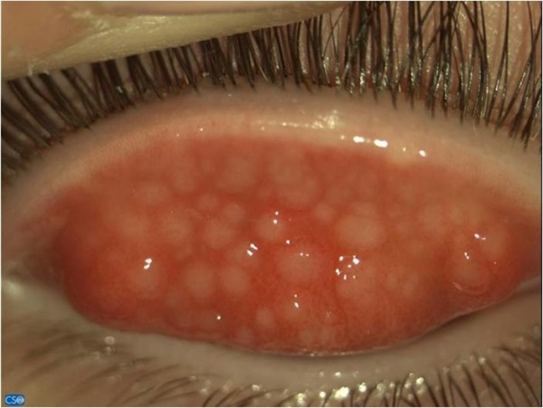
define follicles and describe their appearance (4)
accumulation of WBC’s
Raised white/pinkish, round elevations
Whitish-grey centres surrounded by small vessels
Tarsal or forniceal conjunctiva (uncommonly on bulbar conjunctiva)

why do follicles form (2)
response to viral or chlamydial infection
also seen in toxic conjunctivitis
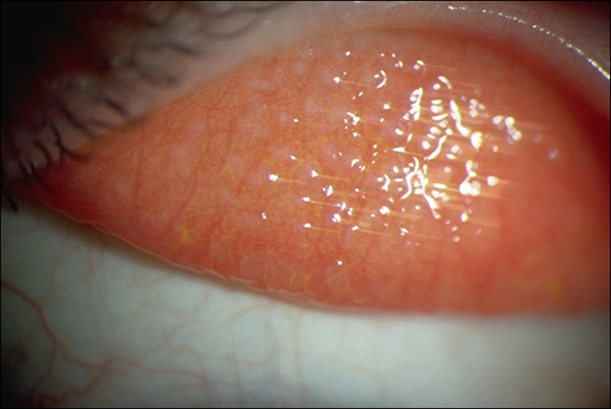
define papillae and describe their appearance (4)
elevated areas of inflammation
Raised swellings in the tarsal conjunctiva
May be visible blood vessel in centre (vascular tuft)
Classified by size - Small appear velvety - may be a normal finding // Large - ‘giant’ - cobblestone appearance

what are papillae indicative of
of an allergy or a bacterial infection
what are the 3 categories/types of infective conjunctivitis
viral
bacterial
chlamydial
explain the aetiology of viral conjunctivitis (4:3:6)
can be caused by adenovirus: most common cause
> 30 serotypes (types) capable of affecting eye
commonest acute infective conjunctivitis (75%) - 3/4 cases are adenoviral
presentation varies - mild-severe
can be acute haemorrhagic:
rare epidemics
enterovirus & coxsackievirus - conjunctiva primary site of infection
others: primary site not necessarily conjunctiva
Molluscum contagiosum
Papilloma
SARS-CoV-2 coronavirus
Herpes simplex (see cornea lecture)
Mumps and measles

explain the symptoms of viral conjunctivitis (4:2)
Acute onset (3-7 days):
•Redness
•Watery discharge
•Crustiness of eye lids
•Discomfort - burning or grittiness
Progression:
•Unilateral becomes bilateral
•Blurred vision if cornea involved

what are the predisposing factors of viral conjunctivitis (4)
•Recent cold/upper respiratory tract infection
•Poor hygiene - failure washing hands
•Crowded conditions (school, camps, clinics) - can be passed on easily
•Eye clinic - passed on between px’s
describe the signs of viral conjunctivitis (7)
•Watery discharge
•Conjunctival hyperaemia (redness)
•Follicles - upon lid eversion
•Pin-pick (petechial) subconjunctival haemorrhages (tiny dot-like red spots on conjunctiva when small blood vessels break)
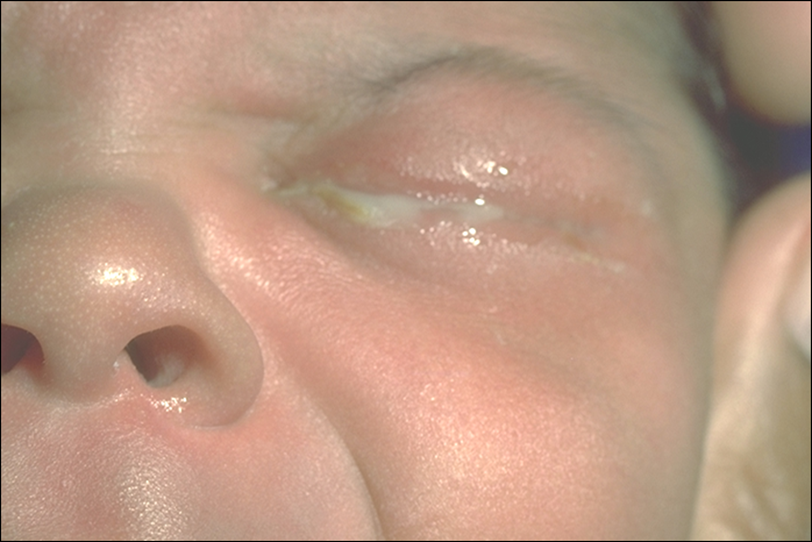
•Psuedomembranes (if severe) - layer of fibrin, inflammatory cells and exudates - coats surface of tarsal conjunctiva - white/yellow soft membrane sitting on conjunctiva
•Lid oedema - swelling (variable extent)
•Watch for corneal involvement (keratitis) - check if clear - if not serious infection

describe the optometric management of viral conjunctivitis (8)
Highly contagious - wash hands and clean equipment - reduce risk of cross infection
Patient advice:
Self-limiting condition (gets better on its own)
Usually resolves in 1-2 weeks - 8-10 weeks to completely clear
Highly contagious (family, friends, colleagues) - explain risk of passing it on - hand hygiene, not sharing towels etc.
Temporarily avoid contact lenses
Do not usually need to refer: however refer urgently if:
pain
Sight-compromising corneal involvement
Psuedomembrane
what is the treatment for viral conjunctivitis (3)
•Cold compress - symptomatic relief
•Ocular lubricants
•Painkillers
what are the secondary care options for viral conjunctivitis (5)
•Antibiotics ineffective against viruses
•Generally no effective antiviral - however - viral culture - conjunctival swab - if effective against that then antiviral may be offered but not routinely
•Topical antihistamines - severe itching
•Weak topical steroid - used with care (membranous or risk of scarring) - suppress immune response BUT can make infection more likely + delay wound healing
•Adenovirus necessitates 2 weeks off work/school - reduce risk of contamination

describe the aetiology of bacterial infective conjunctivitis (3)
Very common
Self-limiting infection (gets better on its own)
caused by various bacteria:
•Staphylococcus species
•Streptococcus pneumoniae
•Haemophilus influenzae
•Moraxella catarrhalis
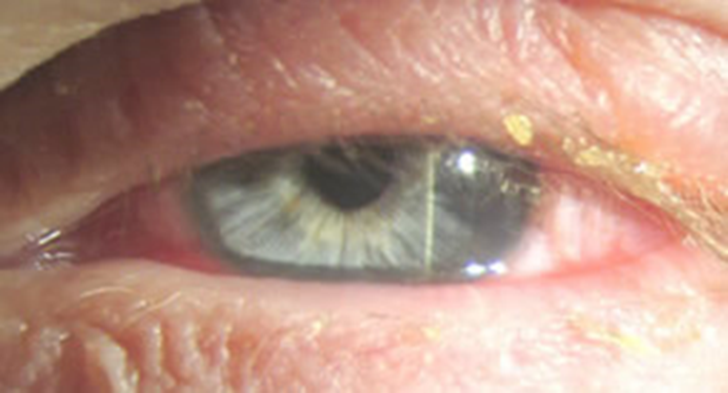
what are the predisposing factors of bacterial infective conjunctivitis (7)
•Contamination of conjunctival surface
•Blepharitis
•Trauma
•Contact lens wearer - way in for bacteria - make infection more likely
•Recent cold/upper respiratory tract infection or sinusitis (inflammation of the mucosa lining the paranasal sinuses)
•Immune compromise (including diabetes)
•Steroids (systemic or topical)
describe the symptoms of bacterial infective conjunctivitis (6)
Acute onset (24-48 hours)
Redness
Discomfort - burning or grittiness (no pain - unless cornea is involved)
Discharge - purulent or mucopurulent (sticky)
Lids may be stuck together on waking
Usually bilateral (can be asymmetrical - then may pass onto other eye)

what are the signs of bacterial infective conjunctivitis (5)
•Purulent or Mucopurulent discharge
•Conjunctival hyperaemia (redness)
•Mild papillary conjunctivitis (tarsal conj)
•May be lid oedema
•+/- epithelial punctate staining due to tear film instability

describe the management of bacterial infective conjunctivitis (7)
Self limiting condition - resolves spontaneously without treatment within 5-7 days - for MOST px’s
Highly contagious (e.g. through sharing towels) - advise px’s on this
Bathe/clean the eyes with sterile wipes, lint or damp cotton wool
Cease contact lens wear until resolved - throw away potential contaminated lenses and contact lens case
May not need treatment, but… chloramphenicol drops or ointment (drops 2 hourly for first 48 hours then 4 hourly for 5 days)
Contact lens wearers - risk of acanthamoeba - CHECK
Conjunctival swab if resistant to treatment or recurrent - referral if pain persists and if necessary
explain the aetiology of chlamydial infective conjunctivitis (5)
almost always sexually transmitted disease (rare eye to eye infection)
Chlamydia trachomatis is an intracellular parasite (type of bacteria)
Serotypes (strains) A-C:
•Trachoma
•a leading cause of worldwide blindness
Serotypes (strains) D-K:
•Chlamydial (adult inclusion) conjunctivitis
•Ophthalmia neonatorum - STD
Uncommon compared to bacterial and viral conjunctivitis
what are the predisposing factors of chlamydial infective conjunctivitis (2)
•Young adulthood (15-35 years) - sexually active years
•STD C. Trachomatis
symptoms of chlamydial infective conjunctivitis (5)
•History > 2 weeks (subacute)
•Gritty irritation
•Sticky discharge
•Often unilateral - can be bilateral
•Droopy lid(s)

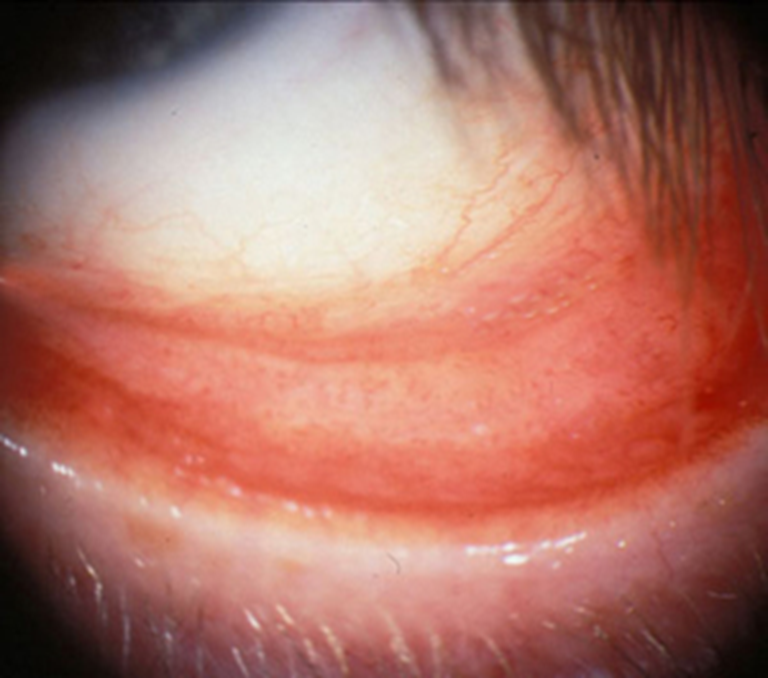
what are the signs of chlamydial infective conjunctivitis (6)
Lid oedema & mechanical ptosis
Mucopurulent discharge
Conjunctival hyperaemia (redness) and chemosis (swelling)
Large follicles in upper and lower fornices
+/- limbal and/or bulbar follicles
Keratitis (superior “micropannus”)
describe the optometric management of chlamydial infective conjunctivitis (3)
•Advise against CL wear
•Ocular lubricants
•Liaise with GP/Ophthalmologist
what are the secondary care options for chlamydial infective conjunctivitis (3)
•Lab tests to confirm diagnosis (swab)
•Systemic antibiotics
•May need referral to Genitourinary clinic
describe what ophthalmia neonatorum is (3)
•Any conjunctivitis within first month of life - born with it/develops early on
•Infection of the maternal birth canal (STD)
•Since April 2010 is no longer a notifiable disease in the UK
what are the different types/causes of ophthalmia neonatorum (5)
•Chlamydial (5-14 days)
•Gonococcal (3-5 days)
•Staphylococcal
•Haemophilus spp
•Herpes simplex virus
symptoms and management of ophthalmia neonatorum (3)
•Bilateral redness, discharge, lid oedema
•At risk of corneal perforation (full-thickness hole in cornea - allowing contents of anterior chamber to leak out)
Same day referral to ophthalmologist
what is chlamydial (trachoma) conjunctivitis (3)
•Second leading cause of blindness world wide (visual impairment in 1.8 million) - occurs in third world countries
•Fomite transmission (flies & person-to-person)
-not a sexually transmitted disease
what are the signs of chlamydial (trachoma) conjunctivitis (4)
Conjunctival scarring
trichiasis (misdirected eyelashes that turn inward and rub against cornea + conjunctiva)
corneal ulcers
Infiltrates, superior pannus, Herbert’s pits (scarred limbal follicles), 2° corneal infections

what are the risk factors of chlamydial (trachoma) conjunctivitis (3)
Poverty
crowded living conditions
poor sanitation
treatment options for chlamydial (trachoma) conjunctivitis (4)
•Public health measures, hygiene
•Systemic & topical antibiotics
•Lubricants
•Consider lid surgery - correct scarring and placement of lids to prevent further corneal infections