NHP Infectious diseases
1/235
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
236 Terms
How do symptoms vary between macaques and marmosets with shigella?
Macaques: diarrhea
Marmosets: lethargy, deyhdration, depression
What is the etiologicaly agent for bacillary dysentary, and what are the clinical signs in macaques?
Bacillary dysentery is caused by Shigella spp. characterized by
foul-smelling, liquid stool containing mucus, frank
blood, and/or mucosal fragments.
What is the most common presentation of shigella in NHPs, chronic intermittent or acute?
A more common form of shigellosis is a subacute to
chronic diarrhea with liquid to semisoft stool that may
occur in colonies in which enzootic infections develop.
Diarrhea is intermittent to episodic.
What are some non-enteric forms of shigella in macaques?
Gingivitis, abortion, and air sac infections are non-enteric forms of shigella infections that may occur in rhesus monkeys.
Also a postinfective immune-mediated arthritis has
been observed and generally occurs 3–4 weeks following
resolution of intestinal signs (Urvater et al., 2000).
This particular aseptic arthritis often presents as a nonweight
bearing lameness accompanied by high fever
and responds to corticosteroids.
Where in the GI is pathology most common for Shigellosis and what are the pathologic signs?
Lesions of enteric shigellosis occur primarily
in the cecum and colon. The colonic mucosa is
usually covered with a fibrinopurulent exudate that
can progress to a pseudomembranous enterocolitis,
and the intestinal wall is edematous and hemorrhagic
with focal areas of ulceration.
Intussusception of the small intestine, rectal prolapse,
splenomegaly, and mesenteric lymphadenopathy may
occur
What is the best method for diagnosis of shigella, single culture or serial cultures?
To reduce this possibility, sequential
culture of samples taken from each of three successive
days is recommended.
Antibiotics used to treat shigellosis in NHPs?
Enrofloxacin and combination therapy with oral
trimethoprim-sulfamethoxazole, erythromycin, and tetra
cycline
Which bacterial pathogen is the most frequently isolated from clinical and nonclinical NHPs?
Campylobacter jejuni and C. coli are the
most frequent fecal bacterial isolates from subclinical, and clinically affected nonhuman primates
Clinical signs of campylobacterosis in NHPs?
Campylobacter infection usually presents
as watery diarrhea, although mucohemorrhagic diarrhea
has also been reported
Best stain for campylobacter spp?
Warfrin Starry Silver Stain
Why is treatment of NHPs for campylobacterosis controversial?
Because many infections are
self-limiting and reinfection is frequent (Russell et al.,
1987), the efficacy of antibiotic treatment for campylobacter diarrhea is debatable and should be determined on a case-by-case basis.
What are the four types of colibacillosis in NHPs?
Gram negative bacteria which is a frequent normal fecal isolate.
There are four recognized categories of diarrheagenic
E. coli: Shiga toxin-producing E. coli (STEC), also
known as enterohemorrhagic E. coli (EHEC), e.g., E. coli
O157; enterotoxigenic E. coli (ETEC), which produces
a heat labile or heat stable enterotoxin, or both; enteropathogenic
E. coli (EPEC), which are associated with
infantile diarrhea and are not known to produce enterotoxins
or Shiga toxin; and EIEC, which invades cells of
the colonic epithelium causing a watery and occasionally
bloody diarrhea
What form of colibacillosis are marmosets and tamarins susceptible to?
Common marmosets and Cotton-top tamarins are
also susceptible to disease with EPEC
Which bacteria is known to cause opportunistic disease in NHPs with SIV?
EPEC has also been recognized as an important and
common opportunistic pathogen of SIV-infected rhesus
macaques (M. mulatta) with immune deficiencies. infection was associated with persistent diarrhea and wasting, and was more frequent in animals that died at less than 1 year of age
What are the two most common species of salmonella found in NHPs?
two recognized species within the genus,
S. enterica and S. bongori
What are the enteric and nonenteric clinical signs of salmonella in NHPs?
Clinical signs of enteric salmonellosis
include watery diarrhea, sometimes with hemorrhage
or mucus. Animals are often pyrexic (Paul-Murphy,
1993). Other signs include neonatal septicemia, abortion,
osteomyelitis, and pyelonephritis
What on necropsy do you find with salmonella in NHPs in regards to the spleen in lymph nodes?
Enlargement of the spleen
and mesenteric lymph nodes may occur
What pathogen typically accompanies lymphocytic plasmacytic gastritis in NHPs?
H. pylori in the gastric mucosa of monkeys is often accompanied
by persistent lymphocytic plasmacytic gastritis
Common clinical signs of helicobacterosis in NHPs?
Clinical signs of gastric helicobacter infection
may include inappetence and occasional vomiting.
What has become a novel cause of IBD in cotton topped tamarins?
A novel Helicobacter has been isolated and characterized
from colons of cotton-top tamarins (S. oedipus), with
inflammatory bowel disease
Which bacterial disease has been associated with colonic adenocarcinoma in Rhesus?
Persistent infection of rhesus macaques with H. macacae associated with colonic adenocarcinoma has been described
Which bacterial enteric pathogen causes proliferative enteritis in juvenile macaques?
Lawsonia Intracellularis
Primary gross lesions of lawsonia in NHPs?
segmental thickening and pallor of the distal
5 cm of ileum
Which pathogen is the most devastating respiratory pathogen of NHPs?
Streptococcus pneumoniae. Streptococcal infections are acquired by aerosol via the upper respiratory tract, middle ear, or mouth
How does Streptococcus pneumoniae clinically progress in macaques and chimps?
In macaques, disease is usually rapidly
progressive; death may occur within hours of clinical
onset (Gilbert et al., 1987). In chimpanzees, clinical signs
are initially those of an upper respiratory infection:
coughing and a seromucoid to mucopurulent nasal discharge
are followed by neurological signs (Keeling and
McClure, 1974; Solleveld et al., 1984). Duration of clinical
illness can range from 2 to 14 days in chimpanzees.
What is likely the pathogen when you see degenerative neutrophils with intracullar gram positive cocci in the CSF from an NHP?
Streptococcus pneumoniae
What are the gross lesions of Streptococcal meningitis in NHPs?
Gross lesions include engorgement of the meningeal
vasculature, thickening and opacification of the leptomeninges,
and purulent exudation over the cortex
and/or the ventricles (Fox and Wikse, 1971; Solleveld
et al., 1984; Graczyk et al., 1995). Lesions may extend to
the spinal cord.
What pathogen is typically positive optochin test and a Kuellung rxn?
Streptococcal infection
Treatment of streptococcus in NHPs
S. pneumoniae remains sensitive to penicillin.
Treatment of animals with advanced clinical signs
indicating neurologic or systemic involvement is unlikely
to be successful
What are the clinical signs of Streptococcus pneumoniae?
Ataxia, muscle tremors, head pressing
What is the most common cause of meningitis in NHPs?
Streptococcus pneumoniae
What is the pathogen that is often found as part of the normal flora in the upper and lower gastrointestinal tracts of many nonhuman primates. Pathogenic strains associated with the upper respiratory tract are usually heavily encapsulated?
Klebsiella pneumoniae
Which pathogen uses fimbriae and capsules as virulence factors?
Many pathogenic strains possess fimbriae, which act as adhesins and a virulence factor that permits colonization of mucosal surfaces. The capsule also serves as a virulence factor by inhibiting phagocytosis. More virulent strains of K. pneumoniae with a hypermucoviscosity phenotype have been associated with severe disease in both human beings and nonhuman primates.
Clinical signs of Klebsiella in NHPs?
K. pneumoniae infection can result in pneumonia, meningitis, air sacculitis, septicemia, peritonitis, and enteritis in New and Old World primate species, and in apes. New World monkeys in particular may die from septicemia or peritonitis with no clinical signs. Young animals are more likely affected.
Which bacterial pathogen is a primary cause of respiratory death in chimps?
Klebsiella pneumonia
Most common pathology seen in callitrichids, marmosets and Owl monkeys with Klebsiella?
a. Fibrinous lobar pneumonia, purulent peritonitis, and mesenteric lymphadenopathy are the primary lesions reported in callitrichids infected with K. pneumoniae
b. Enteritis and hepatomegaly were reported in a colony of common marmosets
c. Purulent meningitis, consolidative pneumonia, intestinal hemorrhages, peritonitis, and air sacculitis occur in owl monkeys.
Antemortem diagnosis possible with Klebsiella?
Not typically because of the acute course of disease.
Is there a vaccine in NHPs for Klebsiella?
Vaccination utilizing autogenous bacterins has been effective in preventing infection and disease in marmosets, and owl and squirrel monkeys
What are common predisposing factors for Bordetella bronchisepticum infection in NHPs?
Bordetella bronchiseptica is carried as a commensal organism within the nasopharynx of many monkeys. Historically, disease has been associated with recent shipping, quarantine, poor condition, and overcrowding
Common clinical signs of Bordetella in NHPs?
Clinical signs in affected common marmosets included bilateral mucopurulent nasal discharge, dyspnea during handling, and pyrexia. Marmosets usually remained bright and alert and in good body condition. Death occurred in marmosets less than 1 year of age, but adults survived.
What is a common pathogen of shipping stress-related in squirrel and owl monkeys?
Pasteurella multocida
What are the clinical signs of P. multocida in squirrel monkeys?
Squirrel monkeys presented with unsteady gait, nystagmus, head tilt, and circling. Meningitis, otitis media, lymphadenitis, and myocarditis were diagnosed at necropsy Pneumonia, pleuritis, and meningitis occurred in affected owl monkeys.
What pathogen primarily causes Necrotizing, fibrinopurulent pneumonia with thrombosis of small blood vessels and severe, acute interstitial pneumonia with multifocal necrosis of alveolar septae?
Pasteurella multocida
What gram stain is nocardia?
Gram + acid fast
NHP presents with dypsnea and epistaxis, what is likely the pathogen?
Nocardia asteroides is the most common isolate in nonhuman primates. Infection occurs following contact with skin wounds, inhalation, or ingestion. Clinical signs include dyspnea and epistaxis
Which pathogen is indistinguishable from Tuberculosis on radiographs in NHPs?
Nocardia
NHP presents with Multifocal to coalescing pyogranulomas containing sulfur granules with large colonies of filamentous bacteria, what is the pathogen?
Nocardia
What is the gram stain of Moraxella catarrhalis?
Gram negative diplococcus
Cynomologous macaque presents with epistaxis, no other clinical signs seen, what is the pathogen?
Moraxella catarrhalis
What mycobacterium are common causes of TB in NHPS?
Tuberculosis is caused by Mycobacterium tuberculosis, M. bovis, or M. africanum, M. microti and M. canetti
Most common sources of transmission of TB in NHPs?
Epizootic tuberculosis in nonhuman primates usually takes place by aerosol transmission, but transmission has occurred by ingestion, direct contact, and contact with fomites, including contaminated thermometers
An NHP presents with unexplained cachexia? What diagnostic would you do first as a primary rule out?
TB test
What is a possible diagnosis of Lymphadenopathy of the tracheobronchiole lymph node in rhesus macaque?
TB
DDX of cavitary lesions in the lung?
Nocardia, cryptococcus, TB, Coccidioides and yersinia
What pathogen causes Scrofula and Potts DZ?
TB, Scrofula is cervical lymphadenopathy, Potts disease is spondylitis
Reasons for false positive on TB test?
a. Complete freuds adjuvant
b. Infection with non TB mycoplasma
c. Trauma
d. Rxn to TB test
Reasons for false negative?
a. Early or late measles disease
b. Given TB vaccine
c. Isoniazide treatment (treatment for TB)
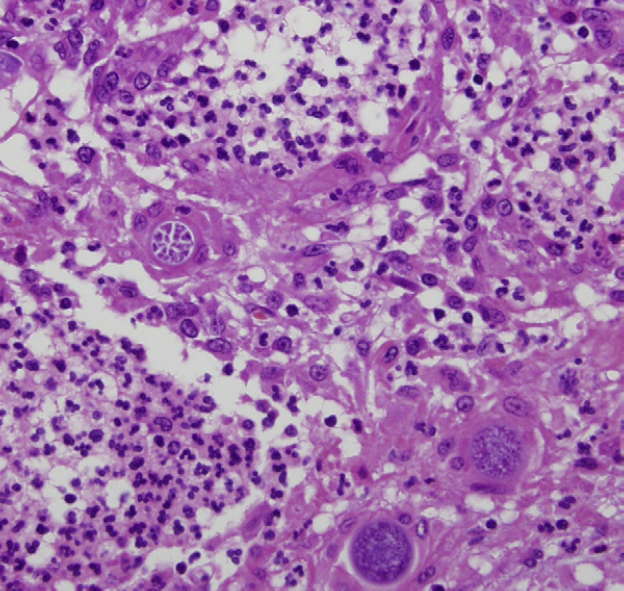
Most common microscopic findings for TB?
The typical microscopic lesions are un-encapsulated granulomas of varying size with a necrotic core. Surrounding the core is a layer of epithelioid macrophages and lesser numbers of neutrophils, with multinucleated Langhans’ giant cells at the periphery. Mineralization is uncommon. Acid-fast bacilli (AFB) can be demonstrated within the lesions both intra and extracellularly using an acid-fast stain; however, AFB are often rare or absent in clinical tuberculosis cases.
Which test is better for diagnosis of TB purified protein derivative or Mammalian Old Tuberculin?
MOT
What is the gold standard for TB diagnosis?
culture remains the gold standard for diagnosing tuberculosis.
What is the most common nonTB mycoplasma that afflicts NHPs?
Mycobacterium avium-intracellulare complex, also known as M. avium complex (MAC), consists of pathogenic, saprophytic, nontuberculous mycobacteria that are contracted through exposure to soil, water, or infected tissues
Which bacteria is most commonly seen as a secondary infection to Simian AIDs?
Mycobacterium avium-intracellulare
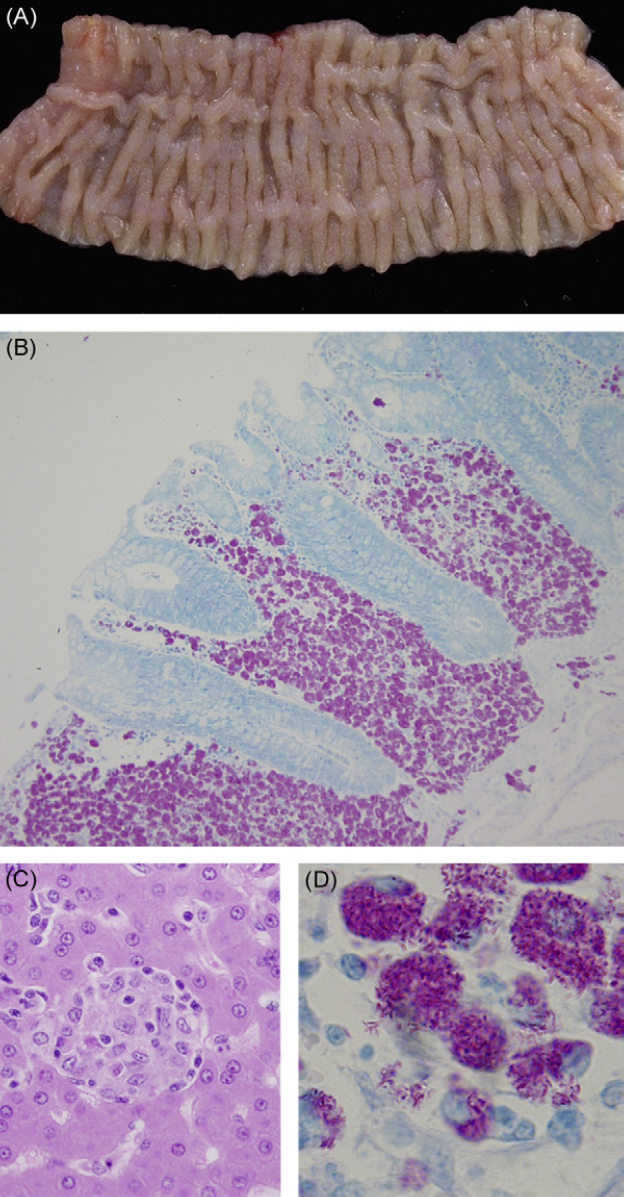
Which pathogen primarily involves the gastrointestinal tract and reticuloendothelial system?
Mycobacterium avium
Which pathogen particularly causes Diffuse granulomatous inflammation of the terminal ileum and proximal colon due to infiltration of large, foamy macrophages into the mucosa and submucosa was characteristic.
Mycobacterium avium
What is the cause of Hansens disease in NHPs?
Mycobacterium leprae
What pathogen causes Multiple, eroded, nodular skin lesions of the face and ears occurred in chimpanzees?
Mycobacterium leprae
What is the recommended treatment Mycobacterium leprae?
The currently recommended multidrug chemotherapy for treating humans includes daily dapsone and clofazimine, with monthly rifampicin treatments
What are the species that cause atypical mycobacterium in NHPs?
Mycobacterium kansasii and M. gordonae
What are the pathology findings of Mycobacterium kansasii?
pulmonary nodules, some containing yellow–green caseous material, and tuberculous-type lesions in the mediastinal lymph nodes
Mycobacterium avium
Is tetanus a problem in NHPs?
Yes, vaccine is common
Does a leptospirosis vaccine exist in NHPs?
yes
What is the most common isolate from wounds, catheter infections, and NHPs with arthritis?
S. aureus was the most frequent isolate from external wounds and joint specimens from monkeys with arthritis.
What is a common isolate from infection after radiation?
Methicillin-resistant S. aureus (MRSA) infections have been observed in rhesus macaques that have undergone irradiation
When does pneumocystis typically present in NHPs?
In nonhuman primates with debilitation due to recent importation, bacterial infection, neoplasia, or immunodeficiency associated with retroviral infection
NHP presents with SIV and a cough begins, a fungus is identified, what could be the pathogen?
Pneumocystis
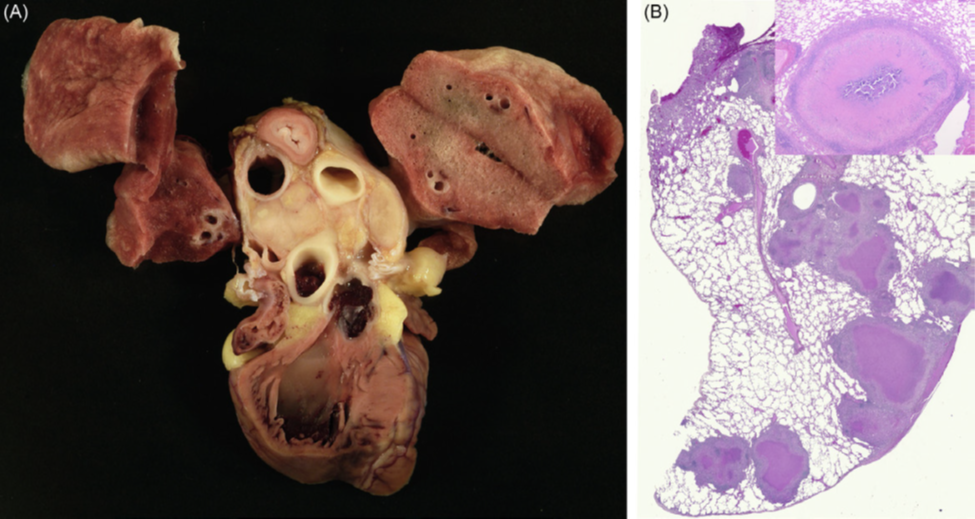
NHP necropsy findings include gross lesions of partial lung collapse; firm, rubbery lungs with multiple 1- to 2-mm gray nodules throughout the lungs?
pneumocystis
Pneumocystis
What is the most common opportunistic fungal infection of NHPs while having SIV?
Pneumocystis
NHP at a institute in southwest USA gets respiratory disease, what is a possible fungal disease?
Coccidoides immitis
Does Coccidioides typically disseminate or stay primarily in the lungs?
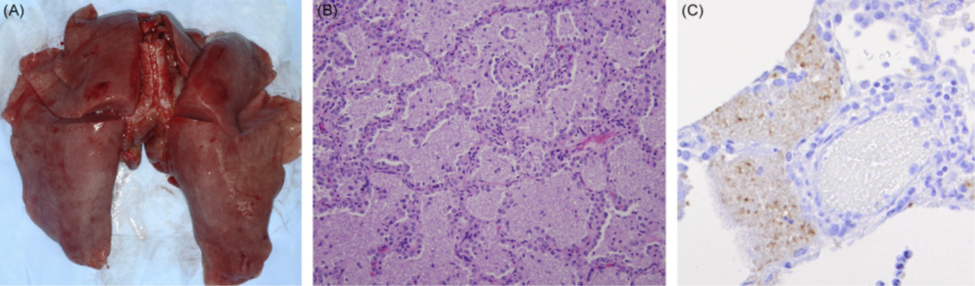
C. immitis infections usually result in disseminated disease, with lesions most frequently found in the lung and vertebrae
Common pathology of C. immitis?
Firm white nodules, partial or complete collapse of a lung lobe, pleural adhesions, and cavitations are common lesions
Coccidioides immitus
What fungus causes Disseminated microgranulomas with multinucleated Langhans’-type giant cells?
Histoplasma capsulatum
What is a pathogen that cause granulomatous lesions in the skin of baboons?
H. capsulatum var. duboisii is the etiological agent
What are predisposing factors for infection of Candida albicans?
a. Predisposing factors for clinical candidiasis include antibiotic therapy, recent importation, retroviral infection, routine oral gavage, or parasitism
b. Normal flora of NHPs
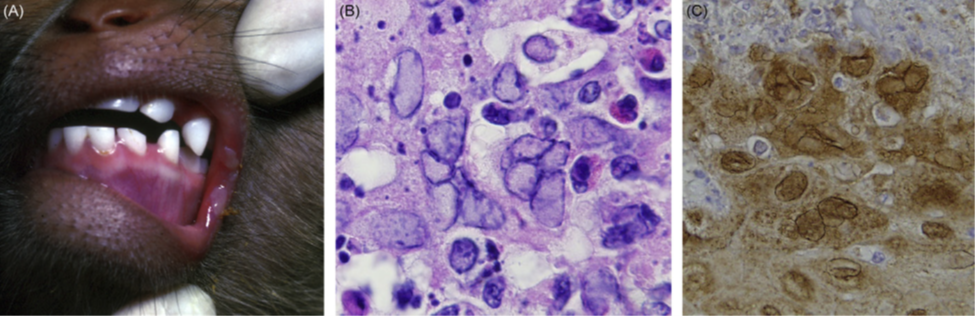
An NHP that just arrived at your institute presents with ulcers on the hard palate and infection of the nail beds?
Candida albicans
What is a pathologic feature of Candida albicans that you can grossly see?
Pseudomembrane formation results from candidial overgrowth. White or creamy plaques are found on the tongue, buccal cavity, esophagus, and intestine.
An NHP presents with seizures and blindness. On necropsy, there is a large gelatinous mass in the chest. What is likely the pathogen?
Cryptococcus neoformans
What organism do you use India-ink preparations allow visualization of the organism against a black background but are not diagnostic unless budding is observed?
Cryptococcus neoformans
What are the genetic and envelope features of herpesvirus?
DNA Enveloped
Which DNA Enveloped virus is persistent and latent resulting in life long infection?
Alphaherpes virus
Typical clinical presentation of alpha herpes virus in NHPs?
Clinical disease, when present, is usually self-limiting and consists of oral or genital vesicles that resolve over time
If NHPs get herpes from humans what tends to happen clinically?
Disease is much more severe when an alphaherpesvirus infects an aberrant host; often infection is fulminating, systemic, and fatal encephalitis.
What is the eitiology of simplex virus in NHPs?
Macacine herpesvirus 1 (McHV-1), also known as Cercopithecine herpesvirus 1, herpesvirus simiae, or B virus, causes a persistent, subclinical latent infection in macaques, the natural host species
Clinical presentation of Macacine herpesvirus 1?
primary infection may be associated with vesicular lesions at the site of exposure resulting frequently in stomatitis, conjunctivitis, vaginitis, or balanoposthitis.
Pathogenesis of Herpes B?
The virus invades axons and is transported retrograde to the associated sensory ganglion where a lifelong infection is established
NHP presents with vesicles in mouth and these microbiologic presentation?
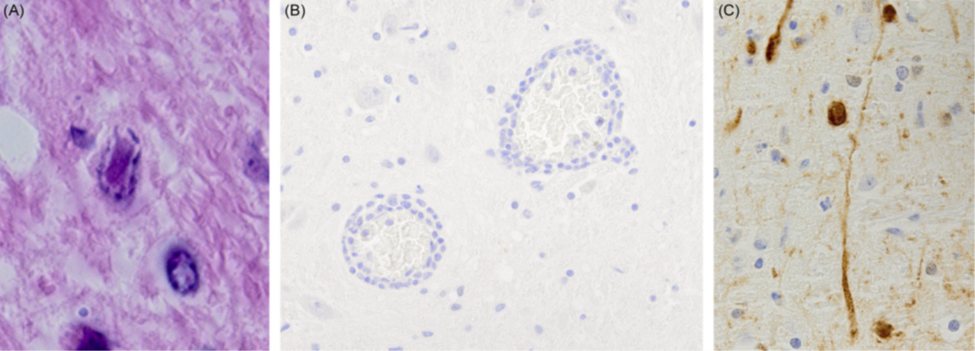
herpes B
Herpes B
Diagnosis of Cercopithecine herpesvirus 1?
Serology