P1 Final Test Questions / Study Guide
1/158
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
159 Terms
When instrumenting tooth # 13 mesial buccal you will be in the __________ o'clock position with the patients head turned______________ you.
right handed operator- 11 or 12, toward; left handed operator- 4, away
When instrumenting tooth # 18 mesial lingual you will be in the __________ o'clock position with the patients head turned______________ you.
right handed operator- 8, away; left handed operator- 4, toward
When instrumenting tooth # 30 mesial lingual you will be in the __________ o'clock position with the patients head turned______________ you.
right handed operator- 11 or 12, toward, left handed operator- 4, away
When instrumenting tooth # 8 mesial lingual you will be in the __________ o'clock position with the patients head turned______________ you.
right handed operator- 11 or 12, neutral ; left handed operator- 1 or 12, neutral
When instrumenting tooth #3 distal buccal you will be in the _________ o'clock position with the patients head turned_____________ you.
right handed operator- 8, away; left handed operator- 1, toward
When working on the maxillary arch; the patient’s head should be in a _______ position .
Tilted up
When working on the mandibular arch; the patient’s head should be in a _______ position .
Chin down
The cllinician is ____ from patient’s mouth
15’’‐22”
True or false: You should always inform patient of change in position and never move the patient’s head yourself!
True
Your upper arm should be at a ____ angle to body
20‐45°
When in the maxillary arch, the position of the chair back :
should be nearly parallel to the floor
When in the mandibular arch, the position of the chair back :
should be slightly raised above the parallel position at a 15‐20 degree angle to the floor
When in the mandibular arch, the position of the light :
should be over the patient’s head
When in the maxillary arch, the position of the light :
should be over the patients chest and tilted toward mouth
persistent fear in which an object or situation is avoided or endured with intense anxiety or interferes with normal routines
Dental Phobia
unpleasant mental, emotional or physiologic sensation derived from a dental-related stimulus
Dental Fear
nonspecific unease, apprehension or negative thoughts about what may happen at appointment
Dental Anxiety
these patients are not able to cope and will typically avoid the dental experience
Dental Phobia
support the flight or fight response when a patient is exposed to a stressor -Cortisol (steroid) is produced -Epinepherine or adrenaline is produced
This is an example of:
Physiologic effects of dental fear/anxiety
Behavioral Effect: how a person acts during a signficant fearful episode Impulsiveness Nervous laughter -Emotional outbursts -Excessive drinking -Smoking - Children: acting out, crying, screaming
This is an example of:
Behavioral effects of dental fear/anxiety
how a person feels emotionally during periods of stress: - Irritability -Guilt - Anger - Anxiety - May also lead to lowered self esteem and depression or sensitivity to constructive criticism
this is an example of:
Phycological effects of dental fear/anxiety
the point at which an uncomfortable stimulus is perceived as painful……anxiety lowers the threshold of pain
Pain Threshold
the amount of pain that is the most an individual can bear….this decreases when an individual is fearful of treatment
Pain Tolerance
The Use(s) of a dental mirror are:
All of the above
Light reflected off the mirror, passing upward through the teeth is an example of:
Transillumination
Transillumination helps to detect:
All of the above
True or false: you can clean the mirror with the patient’s buccal mucosa.
False
When the clinician is instrumenting tooth #30 distal buccal, will the mirror be on the cheek side or the tongue side?
the mirror will be on the cheek or buccal side
A thorough summary of all the components of the assessment- required for routine maintenance
Complete exam
A Brief preliminary exam ;Used for initial assessment and triage to determine priority
Screening exam
Emergency situation
Limited exam
To check healing ; Remove sutures/dressing
Follow-up exam
Complete reassessment to develop new treatment plan
Maintenance/Reevaluation exam
Direct Observation • Radiographic Examination • Transillumination
Visual examination
Starts in the Reception: • Physical deformities • Abnormal movements • Facial form & expression • Color • Stature • Hair • Hearing & other senses • Speech • Breath odor • Extraoral lesions
Direct Observation
True or false: Radiographic Examination is a type of Visual examination?
True
Examination using touch through tissue manipulation or pressure on an area with the fingers of one or both hands • Types of Palpation • Digital • Bidigital • Manual/Bimanual • Bilateral • Circular
Palpation
Use of a single finger • Example- determine the presence of tori
Digital
• Use of finger and thumb (same hand) • Example: palpation of the lip
Bidigital
Use of finger or fingers and thumb from each hand applied simultaneously in coordination • Example: floor of mouth • Manual is use of one hand
Bimanual
Two hands at the same time on corresponding structure on opposite sides of the body • Example- TMJ, submandibular lymph nodes
Bilateral
Overlapping circular palpation • Example- anterior superior, superficial cervical
Circular
Examination instruments, such as a periodontal probe and an explorer are used for specific examination of the teeth and periodontal tissues • Probe can be used to measure lesions
Instrumentation
• The act of tapping a surface or a tooth with the fingers or an instrument • Example- tapping on the crown of a tooth to detect fractures or apical lesions
Percussion
Pulp testing- Tests the presence or absence of vital pulp tissue
Electrical Test
The use of sound • Example- TMJ for crepitus, grinding or popping • Blood Pressure
Auscultation
• Detect mucogingival involvement- lip is pulled to see if there is pulling of the periodontium
Tension test
Usually soft and translucent
Blisterform
small circumscribed lesion with a thin surface covering. May contain serum and appear white
Vesicle
more or less than 5mm in diameter, contains pus that gives pustule a yellow color
Pustule
a circumscribed elevated lesion that is more than 5mm in diameter, usually contains serous fluid, and looks like a blister
Bulla
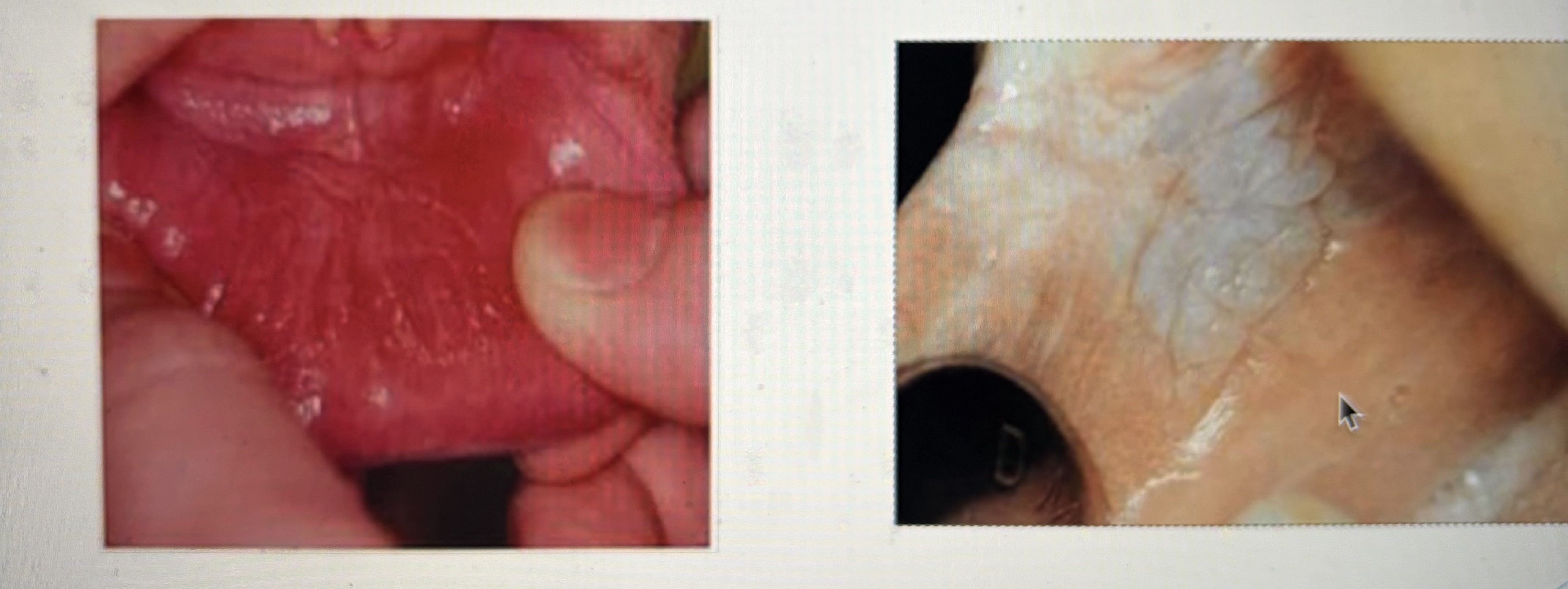
Solid and do not contain fluid base can be sessile or pedunculated
Nonblisterform
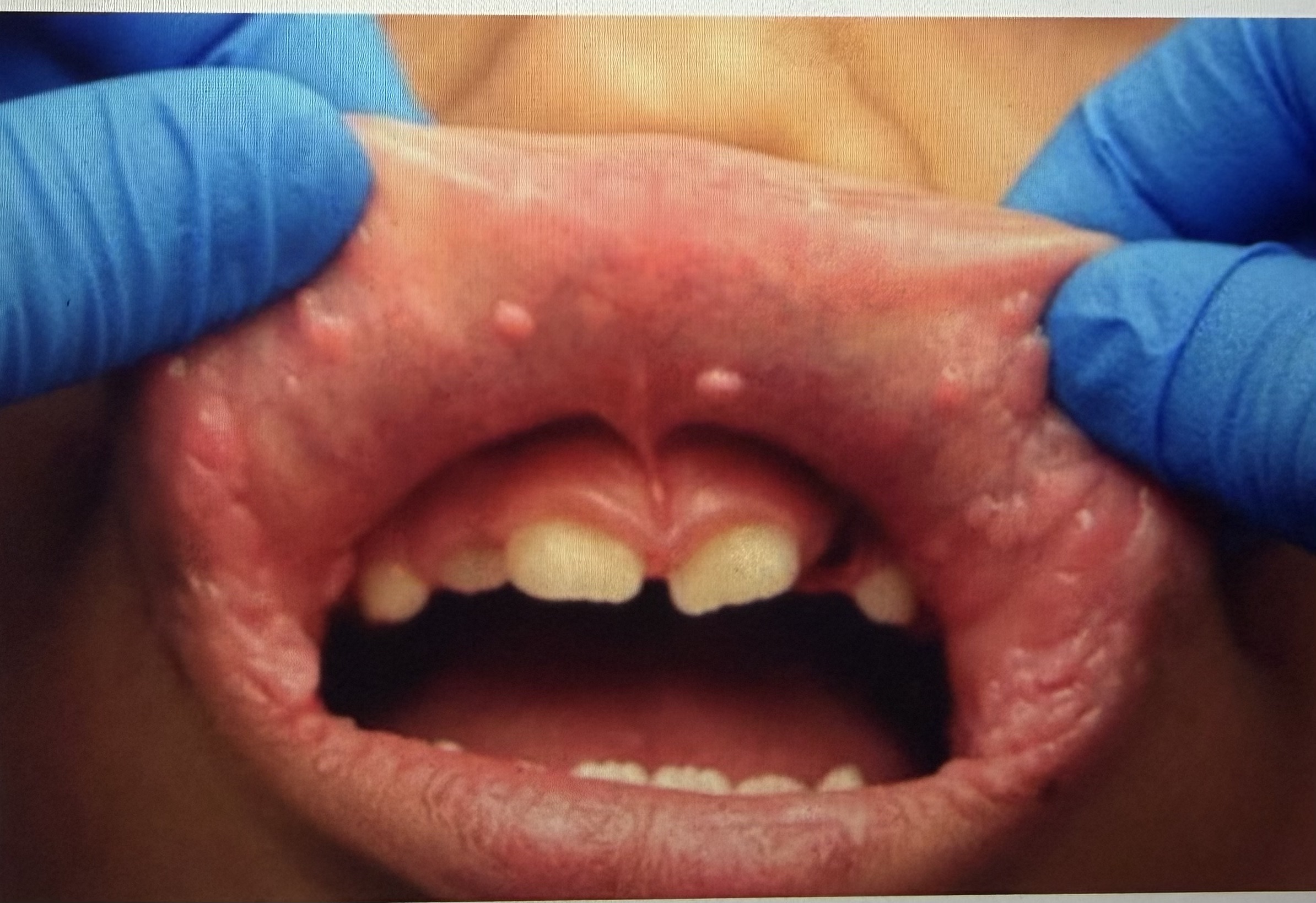
A small, circumscribed lesion usually less than 1 cm in diameter that is elevated or protrudes above the surface of the normal surrounding tissue. May be pointed, rounded, or flat topped.
Papule
A papable lesion up to 1 cm in diameter found in the soft tissue; it can occur above, level with, or below the skin surface.
Nodule
A tumor is 2 cm or greater in width. In this context, means a general swelling or enlargement and does not refer to a neoplasm, either benign or malignant.
Tumor
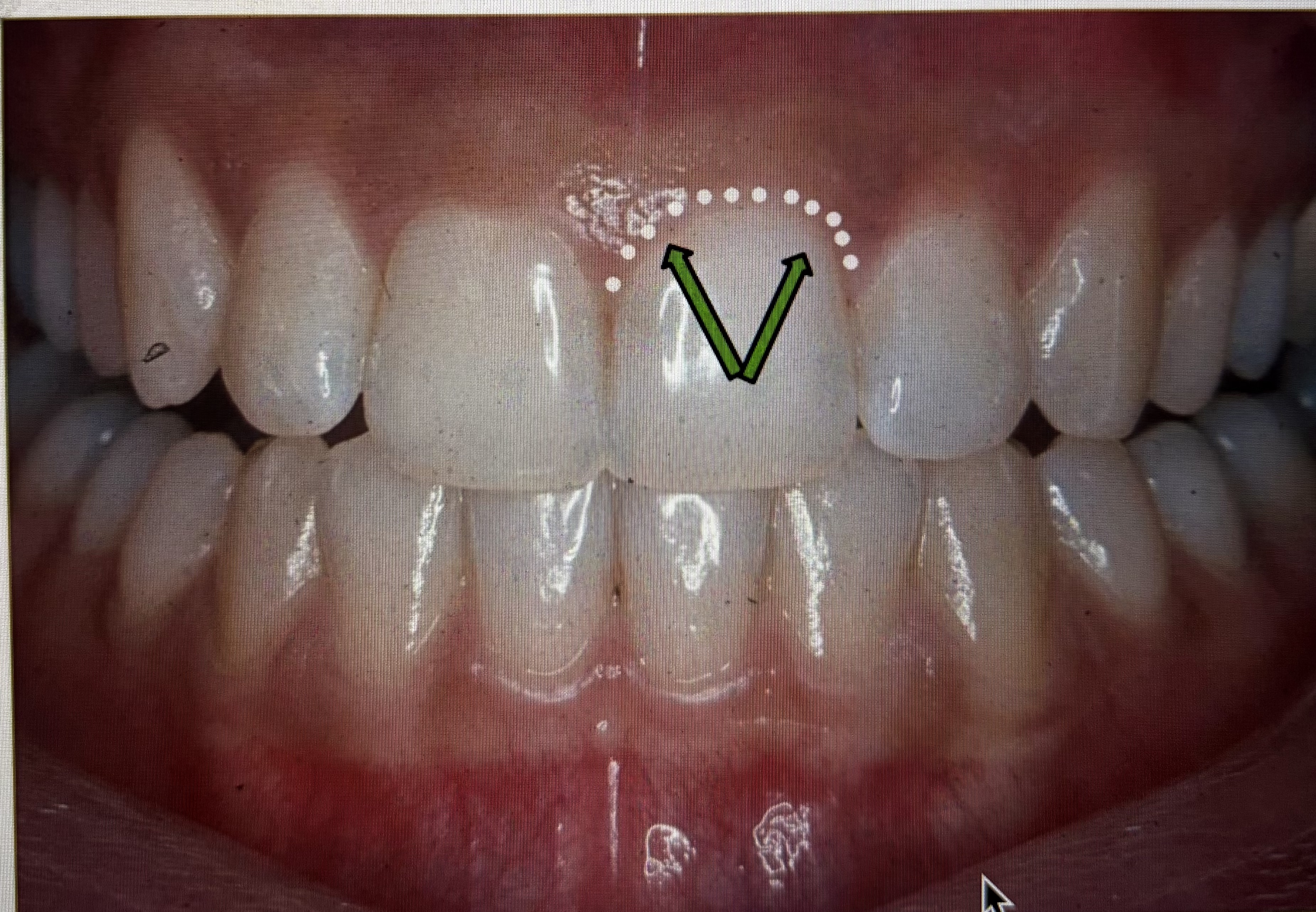
A plaque is a slightly raised lesion with broad, flat top. Usually larger that 5 mm in diameter, with a “pasted on” appearance
Plaque
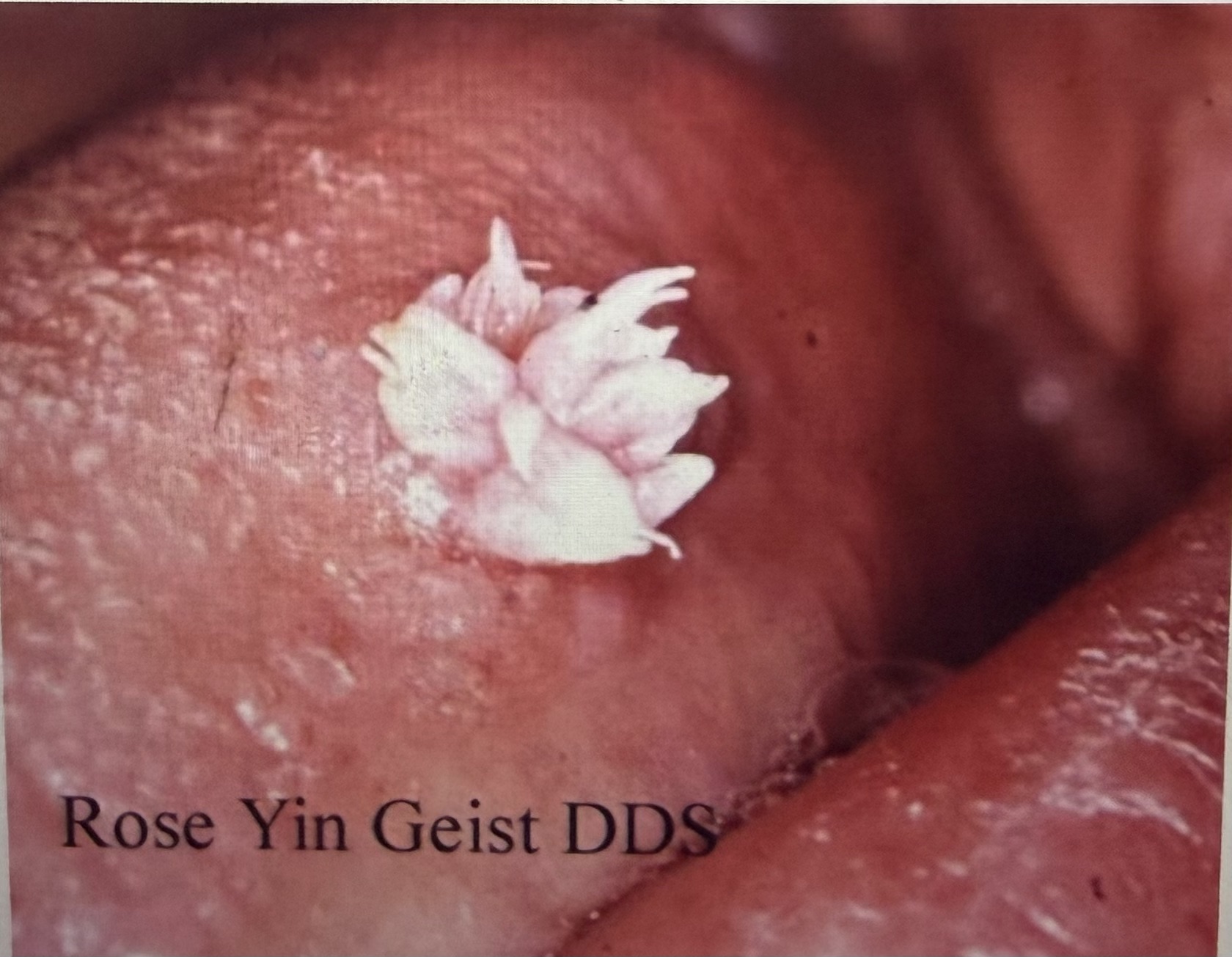
Verrucus or Wartlike

Papillary
Corrugated
Nodule

Tumor
What does Coalesced
Multiple small lesions close together
True or False: Bartholin’s duct drains saliva into the oral cavity through the sublingual caruncle and the sublingual fold
True
What part of the gingiva is the arrow pointing to?
marginal gingiva

Which part of the gingiva is the arrow pointing to?
attached gingiva

Which part of the gingiva is the arrow pointing to?
mucogingival junction

Which part of the gingiva is the arrow pointing to?
interdental papilla
knife edged, flat, rolled or rounded, enlarged
marginal gingiva (shape/contour)
pointed, pyramidal, flat, blunted, cratered, bulbous
interdental gingiva (shape/contour)
Coral, Pink, pigmented, red, cyanotic, magenta
Color
Firm, spongy, soft, edematous, fibrotic, keratinized
Consistency
stippled, smooth, shiny
Texture
The end of a probe is called the:
Nib
Used to determine furcation • Curved working end • Blunt tip • Depth of insertion determines the furcation
Naber’s Probe
up to 1 mm horizontal displacement in a facial‐lingual direction
Class I mobility
greater than 1 mm but less than 2 mm of horizontal displacement in a facial‐lingual direction
Class II mobility
greater than 2 mm displacement in a facial‐lingual direction OR vertical movement in socket
Class III mobility
When the gingival margin is ______ to the CEJ, the CAL is calculated by subtracting the gingival margin level from the probing depth
coronal
When _____ is present, the clinical attachment is calculated by adding the probing depth to the measurement of the gingival recession.
recession
Probing measurement is 4mm Gingival margin has 2mm recession What is the clinical attachment level (CAL)?
6mm
Probing measurement is 9mm Gingival margin is 3mm coronal to the CEJ What is the clinical attachment level (CAL)?
6mm
Probing measurement is 6mm Gingival margin is at the CEJ What is the CAL?
6mm
Probe depth (PD) = 8mm
Gingival Margin
(GM) = +3mm
What is the CAL?
5mm
The patient presents with a periodontal pocket reading of 8mm. There is 2mm of attachment loss. What can you tell me about this patient?
The gingiva is 6mm coronal to the CEJ
The patient has a pocket depth of 4mm and 8mm of attachment loss. What can you tell me about this patient?
There is 4mm of recession
How many basic measurements are made on each tooth in periodontal charting?
6
Most periodontal pocket depths up to what depth are usually related to a normal, healthy sulcus?
3 mm
When measuring the depth of a periodontal pocket, the measurement is made from the base of the pocket or the attached periodontal tissue to
the height of the gingival margin
The depression between the lingual and facial papillae that conforms with the proximal contact area is termed
col
Supragingival exam of margins of restorations;
Gets its name because it resembles the long hook with the curved end that was used by shepherds to catch sheep
Shepards hook
Supragingival exam of margins of restorations
Short curved terminal shank
Straight Explorer
The clinician wants to explore tooth # 30 buccal. How should the clinician begin?
Place the tip on the distofacial line angle and work back onto the distal surface
To determine the correct working end the terminal shank will be _______________ to the tooth surface.
parallel
When using the 11/12 explorer __________________ of the tip remains on the tooth at all times.
:1/3 side of the tip or the terminal 1-2 mm side of the tip
Explorers are made of strong, rigid metal that does not bend easily. Explorers are circular in cross section.
The first statement is false; the second statement is true.
The clinician should not use a shepherd hook explorer for subgingival calculus detection because _____.
The sharp point is directed toward the junctional epithelium
To select the correct working end of an explorer for use on a molar. Which of the visual clues should you use?
Both posterior = parallel and functional shank up and over the tooth
Which instrument should be used to help determine the amount of subgingival calculus on the teeth?
11/12 explorer
Straight Scaler internal angles are:
Internal angles 70°-80°
Curved Anterior Scaler internal angles are:
70°-80°