IHD W5 - Allergy and Hypersensitivity
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
Definitions
Atopy: genetic predisposition to make IgE in response to allergen exposure
Atopic March: natural history of allergic diseases and how they develop/progress. The initial manifestation in infancy is followed by staggered development of additional manifestations later in life.
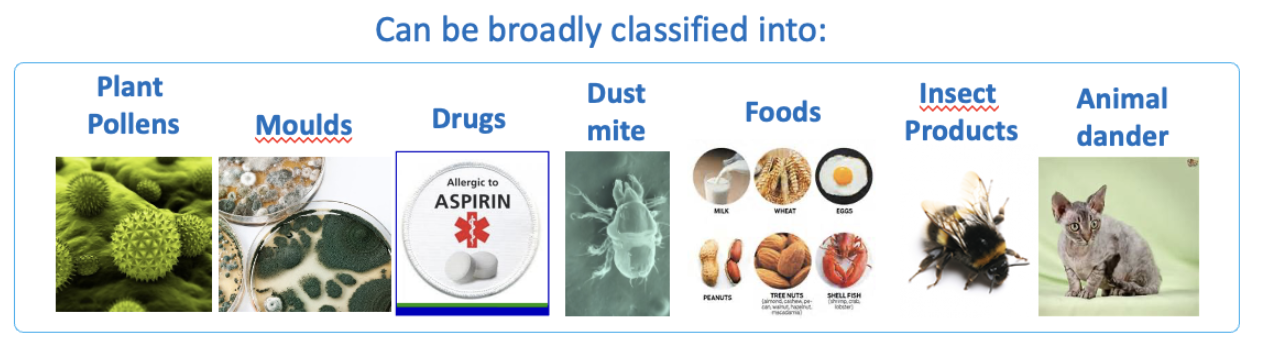
Allergen: any antigen that can cause allergic reaction
Asthma: type of Type I IgE-Th2 driven immune response in the airways.
Non-IgE allergic diseases
Type II, III, IV Gell and Coombs
mediated by TH1 cells and cytotoxic CD8 cells
Non-IgE drug dependent drug-induced hypersensitivity reactions in susceptible individuals occur by binding of the drug to the surface of circulating blood cells.
Systemic disease caused by immune-complex formation can follow the administration of large quantities of poorly catabolised antigens.
Gell and Coombs Classification mechanisms
Pros | Cons |
Only successful attempt to classify disease by mechanism Useful framework to describe and understand various diseases. | Not useful clinically Oversimplified - many diseases (particularly chronic) utilise multiple components of the immune system and don't fit into this classification. |
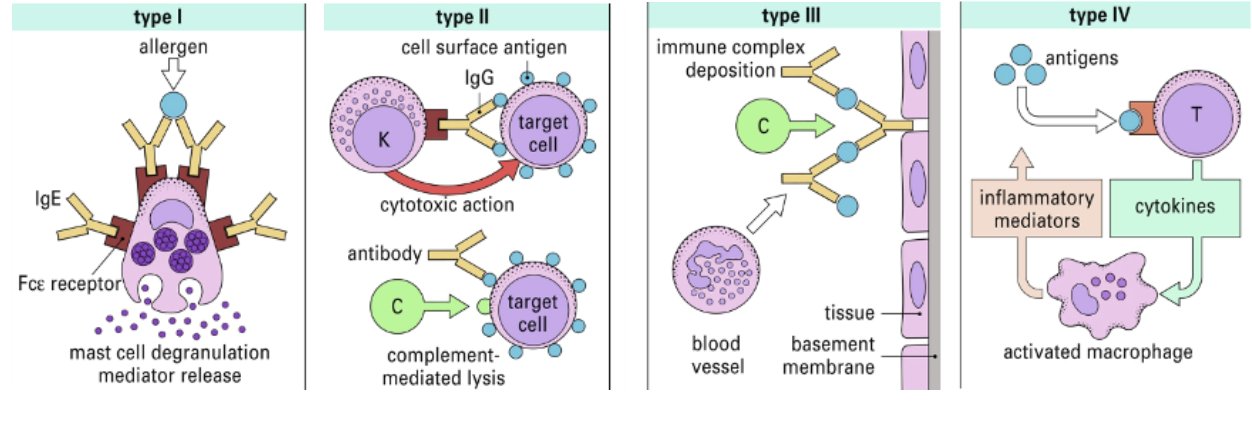
Type I, II and III similarities
reactions can be transferred by serum
Type IV does not involve antibodies and requires the transfer of antigen-specific Th1 clones that orchestrate macrophage response.
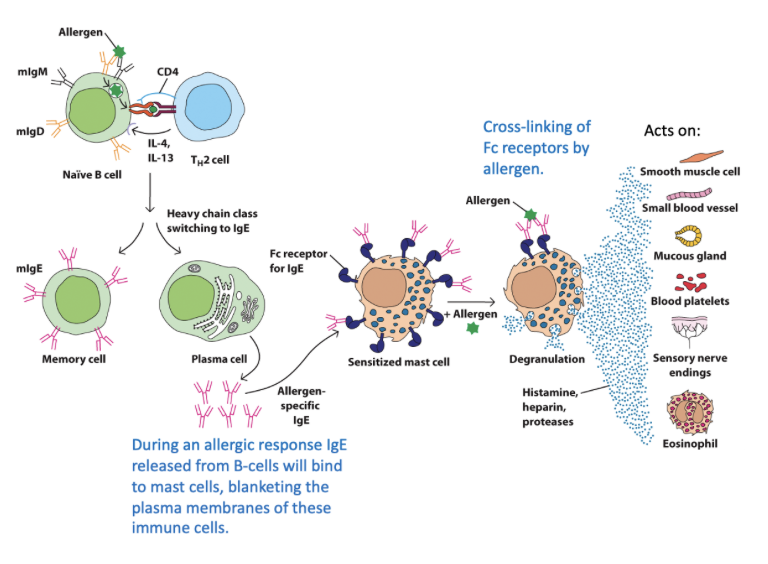
Type I immediate ‘allergic’ hypersensitivity - classic allergy
IgE dependent
atopic individuals produce IgE against environmental antigens (allergens)
IgE cross-links Fcε receptors on innate cell surface
granule content from innate cells are released (histamine, proteases, heparin, leukotrienes, prostaglandins, chemokine) - symptom inducing
Systemic exposure to Type I allergic response
catastrophic, systemic release of inflammatory mediators via IgE cross linking on peri-vascular mast cells which manifests as Anaphylactic Shock
Local exposure to Type I response
localised release of inflammatory mediators
epidermal: Urticaria
inhalation: Asthma
ingestion: Diarrhoea
Type II mechanism
Cytotoxic response - mediated by IgM and IgG targeting membrane associated antigens
etiology: hapten-carrier, molecular mimicry or idiopathic (unknown)
IgM/IgG binds to antigen on host tissue/cells which causes damage via 3 routes:
antibody-dependent cell mediated cytotoxicity (cellular destruction)
activation of classical complement and cell lysis (inflammation)
cellular dysfunction (blocking normal receptor function)
Type III mechanism
Immune complex deposition - Ab-Ag complexes form in circulation, and are deposited into susceptible tissues - may also form directly in the tissue (Arthus reaction)
in healthy individuals, Ag-Ab complexes are soluble and removed by macrophages in the spleen/liver
etiology: antigens that can induce complexes are either endogenous or exogenous, Type III response occurs in cases where the antigen cannot be easily destroyed eg. autoimmunity
immune complex deposition is a prominent feature of several autoimmune diseases
Type III damage
Damage by immune complexes:
precipitate and deposit into tissues if clearance system becomes overwhelmed
leads to complement activation and inflammatory cell recruitment
may trigger release of inflammatory and vasoactive mediators
proteases may damage connective tissue - clots formation as immune complexes activate platelets
Particularly affects blood vessels and the kidney:
3 steps to damage:
immune complex formation
immune complex deposition
inflammatory reaction - classical complement, macrophages, neutrophil recruitement
Type III reaction types
Systemic reaction - serum sickness
7-14 days post exposure
rash, fever, joint pain, lymph node enlargement, proteinuria
vasculitis if in blood vessel
glomerulnephirtis if in kidneys
arthritis if in joints
Local reaction - Arthus reaction
acute, local, typically after vaccination or insect bite
high inflammatory reaction, induced by injection of an antigen in an individual with high levels of circulating antibodies specific to it
swelling and localised bleeding at injection site
also seen when boosters are administered in individuals with high antibody titres
Diagnosing and treating Type III
immune complexes in blood are fragile and hard to quantify
can be detected in tissue biopsies - however this is not simple
relevant antibodies are observed and amount of complement activation is measured
complement factors in the blood decrease in systemic conditions, as they are being used up in hypersensitivity III reactions
main therapy is avoidance where possible, corticosteroids and immunosuppression
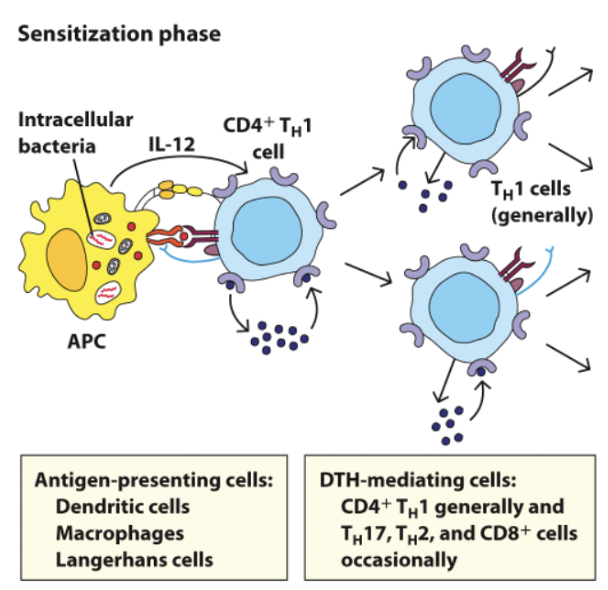
Type IV mechanism
delayed type - not humoral, cell mediated, initiated by T cells
required delay to develop
characterised by recruitment of macrophages at inflammation site
involves sensitisation and effector phases
Type IV Phases - Sensitisation phase
initiation involves sensitisation by an antigen, initial exposure triggers production of a T cell response
often CD4+ TH1 subset
Type IV Phases - Effector phase
induced by second exposure to sensitising Ag.
induces production of TH1 inflammatory cytokines (IFNy, TNF-a, IL-2, IL-3 etc.) these rescue and help macrophage activation
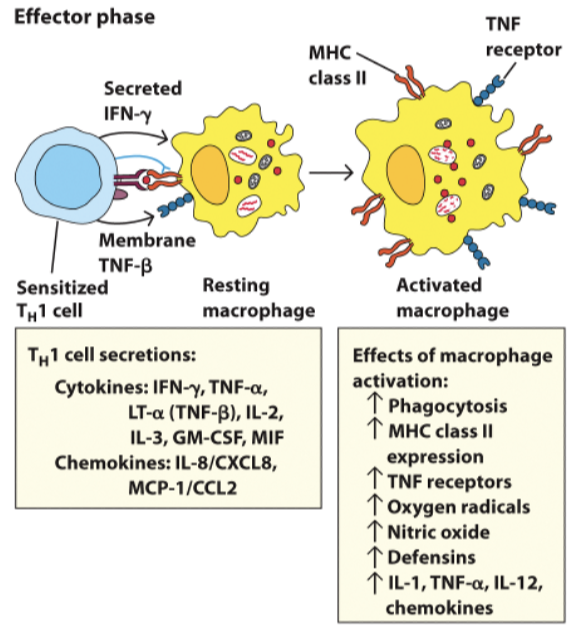
Type IV management
avoidance where possible
immunosuppression via blocking T cell activation or ablate T cells with anti-lymphocyte antibodies
corticosteroids
Type I eitology and mechanism
Etiology: IgE mediated hypersensitivity may have evolved because of their protective roles against helminth worms and animal venoms
allergies initiated by an interaction between IgE and multivalent antigen
free circulating IgE is usually low in serum
global concern of allergy
postulated hypotheses for increasing allergy prevelance
allergen exposure
biodiversity (overuse of antibiotics on gut flora)
immune and metabolic homeostasis
diet
Allergen features
proteins or glycoproteins (bind MHC)
possess many antigenic sites (epitopes) per molecule
often have intrinsic enzymatic properties (favour transition into body)
may contain potential PAMPs, stimulating innate immunity
may enter mucosal tissues at low concentrations, including IgE-stimulating Th2 response
self protein homology
seasonal or perennial
IgE and FCE receptors
IgE cross-links FCE receptors on innate cell surfaces causing degranulation and release of symptom causing molecules
IgE Abs are not themselves harmful
High affinity: FCEI - constitutively expressed on mast cells and basophils
Low affinity: FCEII - regulated IgE levels
proteins as allergen components - example Der p1
Der p 1 is a cysteine protease, a major house dust mite allergen, promoting IgE/Th2 response via protease activity
disrupts epithelial barrier
biased Th1/Th2 polarisation; triggers IL-6 and cleaves IL-2 - reduces inflammation and promotes Th2
excessive IgE: Der p 1 can cleave FCERII (low affinity) on B cells, regulation of IgE
cleave surfactant: reduced allergen clearance
Classic Th2 cytokine profile - in Type I response
IL-4: stimulates/maintains Th2 response B cell class switching
IL-5: recruitment and activation of eosinophils, primes basophils for histamine and leukotriene release
IL-9: stimulates proliferation of mast cells
IL-13: promotes mucus secretion, airway hyperesponsivness
Preformed (primary) Type I mediators
histamine: smooth muscle contraction, increased vasopermeability/vasodilation, enhanced mucus production, pruritus ,gastric acid secretion
proteases: eg. Tryptase, contributes to airway remodelling
Proteoglycans: eg. Heparin, an anticoagulant
De novo synthesised mediators (secondary):
eicosanoids (leukotrienes/prostaglandins): bronchoconstriction, vascular permeability,vasoconstruction, vasodilation, inflammation
Platelet activating factor (PAF): vascular permeability, bronchoconstriction, chemotaxis, degranulation of eosinophils
bradykinin: vasoperability, vasodilation, hypotension, smooth muscle contraction, activation of arachnidonic acid metabolites.
Eicosanoids - bioactive lipids, role in inflammation
comprise prostanoid, leukotrienes (LTs), and lipoxins, which have pro- and anti-inflammatory effects in asthma
potent, short half life, act locally
In asthma, NSAIDs inhibit COX enzymes, leading to reduced prostaglandins and LT overproduction
LT overproduction can worsen asthma
Early and late phase allergic reaction - Type I
Type I hypersensitivities are characterised by both early and late phase responses:
Early response occurs within minutes of allergen exposure
Late responses, hours later, result of recruited cells
A third phase has been described involving basophils and fibroblasts
Late-phase response is caused by continued production of these histamine and lipid mediators, and by recruitment of lymphocytes and myeloid cells
Late phase reaction is mediated by Th2 cells and eosinophils
Late responses, hours later, as a result of recruited cells.
Cytokines released from mast cells increased expression of chemokines and cell adhesion molecules (CAMs) on endothelium facilitating influx of neutrophils, eosinophils and Th2 cells.
Eosinophils play a large role in late phase, recruiting neutrophils and degranulation.