CLASS 6 (Postpartum Period)
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
92 Terms
define the postpartum period
Postpartum period = interval between birth and the return of reproductive organs to the nonpregnant state.
how long is the post partum period roughly
Duration: roughly 6–12 weeks.
what happens during this time? what is the process called?
During this time, all body systems that adapted to pregnancy gradually readjust to pre-pregnancy physiology.
Key process: involution – the body’s internal “reversal” of pregnancy changes.
how is the UTERUS affected during involution? when does it begin? when does it end?
Involution: return of uterus to nonpregnant size and condition.
Begins immediately after delivery of the placenta.
At ~12 hours postpartum, the uterus is at the level of the umbilicus.
It then descends 1–2 cm every 24 hours.
By 2 weeks postpartum, it’s no longer palpable abdominally.
Returns to pre-pregnancy size by 6 weeks.
how do uterus contractions help the involutions process?
Purpose: maintain hemostasis (prevent bleeding) after delivery.
The uterus cannot form clots like a cut on the skin — instead, it contracts to clamp down on blood vessels.
Oxytocin, released from the posterior pituitary, stimulates these contractions
The same hormone responsible for labor contractions now prevents postpartum hemorrhage (PPH).\
Exogenous oxytocin is often administered after birth to assist this process.
Pain from uterine contractions (“afterpains”) may be stronger in multiparous women due to less uterine tone.
what is lochia? whta does it look like immediately after birth?
Postpartum Uterine Discharge)
Composed of blood, tissue debris, leukocytes, and remnants from the uterus.
Immediately after birth: bright red, similar to a heavy menstrual flow, may contain small clots.
what are the 3 stages of lochia? what is the duration?
Progresses through three stages:
Lochia Rubra (days 1–3/4): bright red, blood + trophoblastic tissue.
Lochia Serosa (days 4–14): pink/brown, old blood, serum, leukocytes, tissue debris.
Lochia Alba (2–4+ weeks): yellow-white, mostly leukocytes and mucus.
Total duration: up to 6 weeks.
what are some abnormal findings for lochia?
Abnormal findings: foul odor, large clots, or return to bright red bleeding after it has lightened may signal complications (e.g., subinvolution, infection).
how is the CERVIX affected during involution? what does it loook like?
Immediately postpartum: soft, may appear bruised or edematous.
Gradually closes — about 1 cm dilated at 1 week.
The external os never returns to its pre-pregnant circular shape; it becomes slit-like after vaginal birth.
If C-section without labor → cervical os remains largely unchanged.
how is the VAGINA affected during involution? what drops? what are some methods to promote healing?
Estrogen levels drop postpartum → vaginal wall thinning and loss of rugae (smooth appearance).
Rugae typically return within 3 weeks, though tone and elasticity may not fully return to baseline.
Perineum: often edematous and tender, especially with lacerations or episiotomy.
Initial healing: 2–3 weeks.
Complete healing: up to 4–6 months depending on severity and care.
Good hygiene, ice packs, and sitz baths promote healing.
how is the ABDOMEN affected during involution?
For the first days/weeks, the abdomen may still appear pregnant due to stretched muscles and enlarged uterus.
Returns to pre-pregnancy state in ~6 weeks, though muscle tone may take longer, especially without exercise.
Diastasis recti (separation of abdominal muscles) may persist temporarily.
the delivery of the placenta cause a decrease in which HORMONES during involution?
Human placental lactogen (hPL)
Estrogens and progesterone
Cortisol
Insulinase
what are the consequences of this
Reversal of gestational diabetes (insulin resistance resolves quickly).
Diuresis (fluid loss) as estrogen and progesterone fall.
hCG persists in tissues for 3–4 weeks, though drops rapidly in circulation.
which pituitary HORMONES arise during involution? difference between lactating and non lactating mothers?
Prolactin rises throughout pregnancy and surges postpartum:
When estrogen and progesterone levels drop, prolactin rises further.
Breast/chestfeeding individuals: high prolactin maintained as long as feeding continues.
Non-lactating individuals: prolactin declines to normal within 2 weeks.
what does OVULATION AND MENSES look like during the involution period for non lactating mothers?
Ovulation can return as early as 27 days postpartum.
Mean time: 7–9 weeks.
70% resume menstruating by 12 weeks.
→ Important for contraception teaching: pregnancy is possible even before the first period.
what does OVULATION AND MENSES look like during the involution period for lactating mothers?
Average ovulation return: ~6 months (if exclusively breastfeeding).
Breastfeeding suppresses ovulation via prolactin, but it’s not fully reliable contraception.
how is the URINARY system affected during involution? what is there in increase of in the urine?
Temporary changes common postpartum (Usually resolve within 6 weeks):
Glycosuria (presence of excess glucose in the urine) – from altered carbohydrate metabolism.
Lactosuria (the presence of lactose in the urine) – may persist while lactating.
↑ BUN (Blood Urea Nitrogen) – due to uterine muscle breakdown (autolysis).
Proteinuria (high level of protein in your urine) and ketonuria (abnormally large amounts of ketone bodies) – from dehydration or prolonged labor.
what is compensatory mechanism in term of FLUID LOSS during involution period?
Postpartum diuresis within the first 12 hours due to hormonal shifts.
Helps eliminate extra plasma volume from pregnancy.
what are some factors decreasing the urge/ability to void?
Trauma (especially from forceps/vacuum delivery).
Effects of anesthesia (reduced sensation).
Increased bladder capacity during pregnancy.
what is the risk of a full bladder? what is the nursing care to help this?
Full bladder → impedes uterine contraction → ↑ risk of postpartum hemorrhage (PPH).
Nursing care: encourage voiding, assess bladder fullness, catheterize if necessary.
how is APPETITE affected during involution?
Usually increased after delivery; most can resume a regular diet as tolerated.
Encourage culturally preferred foods if desired.
how is BOWEL MOVEMENTS affected during involution? why?
Often delayed 2–3 days postpartum due to:
↓ intestinal tone
Dehydration
Lack of food during labor
Effects of anesthesia or narcotics
Fear of pain from episiotomy/laceration
what are some special considerations and interventions for GI system?
Special considerations:
Operative vaginal delivery (forceps, vacuum): assess for anal sphincter injury or incontinence.
C-section: risk for gas buildup and shoulder pain (referred gas pain).
Nursing interventions: encourage hydration, fiber, and ambulation.
how is the BREASTS affected during involution for non lactating mothers??
Milk will still come in → breasts may feel tense and engorged.
Do not express or stimulate nipples, as this prolongs milk production.
Wear a tight-fitting bra, use cold compresses, and avoid stimulation.
Engorgement typically resolves spontaneously in several days.
how is the BREASTS affected during involution for lactating mothers??
First 24 hours: breasts feel soft; colostrum (thick, yellow, nutrient-rich fluid) is produced in small amounts.
Milk “comes in” 72–96 hours postpartum → breasts become fuller and heavier.
Encourage frequent feeds to maintain supply and prevent engorgement.
how is CARDIOVASCULAR affected during involution? vag vs c/s?
Hypervolemia of pregnancy (~40–45% ↑ blood volume) enables the mother to tolerate normal blood loss:
Vaginal birth: 300–500 mL
Cesarean birth: 500–1000 mL
Cardiac output gradually returns to normal over several weeks.
how is RESPIRATORY affected during involution?
Immediate decrease in intra-abdominal pressure post-delivery → lungs expand more easily.
Progesterone declines, causing a rise in PaCO₂ to pre-pregnancy levels.
Respiratory function returns rapidly to normal.
how is NEUROLOGICAL affected during involution?
Most pregnancy-induced changes reverse postpartum.
Carpal tunnel (from edema and nerve compression) often resolves quickly.
Headaches require careful assessment → could indicate hypertension or preeclampsia.
how is MUSCULOSKELETAL affected during involution?
Pelvic joints and ligaments stabilize within 6–8 weeks.
Foot size may remain larger post-pregnancy.
Encourage gentle core exercises when appropriate.
how is INTEGUMENTARY affected during involution?
Chloasma (mask of pregnancy) and linea nigra fade gradually.
Striae gravidarum (stretch marks) lighten but don’t disappear.
Hair/nail growth slows back to normal rates.
how is IMMUNE affected during involution?
Pregnancy induces immunosuppression to tolerate the fetus.
Postpartum → immune system rebounds to pre-pregnant state.
Watch for autoimmune flare-ups (e.g., lupus).
Postpartum follow-up is often required for those with autoimmune conditions.
how is VITAL SIGNS affected during involution?
Usually stable and near pre-pregnancy baseline.
Heart rate and BP normalize within a few days.
Respiratory rate and temperature return rapidly to pre-pregnancy values.
Any deviations (e.g., tachycardia, fever) should be investigated for infection or hemorrhage.
what is the time from labout to post partum ward?
When: After delivery of placenta → 1–2 hours on labour ward (4th stage of labour) → transfer to postpartum/mother–baby unit if mother + baby stable.
what is the purpose of a TOA?
Purpose: Transfer of accountability (TOA) — give concise, focused report from recovery nurse to postpartum team so care continues safely.
what are the 8 things relevent to include in a TOA?
Type of labour & birth: spontaneous / vacuum / forceps / C-section; fetal presentation; time of ROM.
GTPAL, maternal age, gestational age.
Anaesthesia/analgesia: epidural/spinal/general; time of last catheterization (important for voiding expectations).
Perineum condition: intact / episiotomy / lacerations (degree) / repaired.
Events since birth: vitals, fundus location/firmness, lochia description, input/output, medications (name, dose, time, effect), oxytocin/PPH drugs, IV status (rate, meds), skin-to-skin time, parental responses, family interactions/siblings.
Newborn summary: time of birth, sex, weight, Apgar 1 & 5, feeding method, prophylaxis (vit K, eye), blood glucose if needed.
Relevant prenatal info: rubella immunity, hep B/HIV, blood type/Rh, GBS status + intrapartum antibiotics, maternal infections, preexisting conditions/meds.
Social factors: adoption plans, visitor preferences, social risks.
why is an toa important?
Why this order matters: rapid, structured TOA prevents missed treatments (e.g., oxytocin continuation, GBS prophylaxis) and flags safety/social needs before discharge planning.
ROUTINE MONITORING IN FIRST 24 HOURS — what is the minimum stay asnd frequency of monitoring?
Minimum stay: typically ≥24 hours after vaginal birth (longer if C-section or complications).
Frequency: hospital policy guides vitals & checks; fundus/lochia frequently in immediate postpartum to detect hemorrhage early.
which assesment framework is used?
Main assessment framework used in class: BUBBLLEE
Breasts
Uterus (fundus)
Bladder
Bowel / Abdomen
Lochia
Legs (DVT assessment)
Episiotomy / incision (C-section)
Emotions / energy (perinatal mood)
+vitals signs**
Vital signs — expected values + bedside reasoning
BP: baseline similar to pregnancy/prepregnant. Orthostatic hypotension possible for ~48 hr.
High BP → anxiety, essential HTN, or preeclampsia (if new or persistent).
Low BP → possible hemorrhage (think volume loss).
Temp: 36.2–38°C normal early. >38°C after 24 hr → suspect infection (endometritis, wound infection, UTI).
Pulse: 60–100 bpm normal. Tachycardia → pain, fever, dehydration, hemorrhage (esp. with low BP).
Respirations: 12–24 breaths/min normal. Tachypnea → anxiety, PE; bradypnea → narcotic effect.
Breath sounds clear. Crackles → consider fluid overload (rare but important — e.g., preeclampsia + fluid shifts).
Clinical link: Early detection of hemorrhage often is through rising pulse + falling BP before dramatic visible bleeding — monitor trends.
Breasts — expected values + bedside reasoning
Timeline:
Days 1–2: soft (colostrum)
Days 2–3: filling
Days 3–5: full; soften after breastfeeding
Normal: nipples intact, soft → firm with feeding.
Red flags: firmness, heat, focal redness, severe pain, systemic fever → mastitis or blocked duct.
Nipple trauma (cracks, blisters) → poor latch; immediate latch support and education indicated.
Example: Client with unilateral breast warmth + fever + pain → assess for mastitis; encourage frequent emptying, analgesia, consider antibiotics if systemic.
Uterus (fundus) — expected values + bedside reasoning
Expected: firm, midline, at level of umbilicus in first 12–24 hr, then descends 1–2 cm/day.
What to palpate: height, tone, position (midline vs deviated), presence of bogginess.
Red flags:
Soft/boggy fundus → uterine atony → major cause of postpartum hemorrhage (PPH).
Fundus deviated laterally → bladder distension (empty bladder to allow contraction).
High fundal height or heavy bleeding → retained tissue or uterine subinvolution.
Clinical action: If boggy → massage until firm, assess lochia, call provider; check bladder; give uterotonic per protocol (oxytocin, ergots, etc.).
Bladder — expected values + bedside reasoning
Expectations: spontaneous void within 6–8 hours after last catheter removal (timing may vary by hospital). Postpartum diuresis common (first 12 hr).
Concerns: retention or overdistended bladder → prevents uterine contraction → increases bleeding. Dysuria, frequency, urgency → consider UTI.
Assessment: bladder scan or catheterize if unable to void and fundus deviated.
Example: Patient with boggy uterus + fundus shifted to right → encourage void, bladder scan showing 600 mL → catheterize → fundus firms up.
Bowel & Abdomen — expected values + bedside reasoning
Expect: bowel movement usually 2–3 days postpartum; abdomen soft; bowel sounds present (especially important post C-section).
Factors delaying BM: decreased intestinal motility (pregnancy/anesthesia), dehydration, analgesia, fear of pain (episiotomy).
Special: C-section → watch for gas pain, encourage ambulation and early feeding to prevent ileus; shoulder pain often referred gas pain.
Red flags: absent bowel sounds, severe abdominal distension, persistent constipation/obstruction.
Nursing tips: stool softeners, fiber, fluids, ambulation; check for perineal pain that prevents bowel movement.
Lochia (postpartum vaginal discharge) — expected values + bedside reasoning
Stages & timing:
Lochia Rubra (days 1–3/4): bright red, blood + trophoblastic tissue.
Lochia Serosa (days 4–14): pink/brown, old blood, serum, leukocytes, tissue debris.
Lochia Alba (2–4+ weeks): yellow-white, mostly leukocytes and mucus.
Volume: scant → moderate; small clots fine.
Red flags: Large amount of bleeding, passage of large clots, foul odor → PPH, retained tissue, or infection (endometritis). Return to rubra after becoming serosa → suspect re-bleed.
Quantify: know what hospital defines as scant / moderate / heavy; gauge pad saturation timing (e.g., saturating a pad in <1 hour is concerning).
Legs (VTE risk) — expected values + bedside reasoning
Normal: peripheral edema may be present.
Red flags: unilateral redness, swelling, tenderness, increased warmth → evaluate for venous thromboembolism (DVT).
Link: pregnancy/postpartum is hypercoagulable (increased tendency for blood to form clots) → high index of suspicion, especially with C-section, immobility, obesity, personal/family history of clotting disorders.
Action: immobilize, physician notification, ultrasound Doppler as ordered, anticoagulation if confirmed.
Episiotomy / C-section incision — expected values + bedside reasoning
Perineum: minimal edema; laceration/episiotomy edges well-approximated; manage with ice, sitz baths, analgesia, pelvic floor exercises.
C-section incision: dry, clean, intact sutures.
Red flags: pronounced edema, hematoma, warmth, erythema, purulent drainage → wound infection or hematoma requiring intervention.
Emotions / Energy (Perinatal mood) — expected values + bedside reasoning
Normal: able to care for self & infant; may have baby blues (tearfulness, mood swings) days 3–14, resolves by 2 weeks.
Red flags: persistent sadness, severe anxiety, inability to care for infant → perinatal mood disorder (PMD) (depression, anxiety, or psychosis).
PERINATAL MOOD SPECTRUM — what is baby blues?
Baby blues: 50–80% incidence; tearfulness, mood swings, mild sleep/appetite change; resolves ≤2 weeks. Nursing: validation, rest, support, monitor.
PERINATAL MOOD SPECTRUM — what is Perinatal Mood Disorders?
Perinatal Anxiety Disorders: ~1 in 5; includes GAD, OCD, panic, PTSD; treat with CBT/ERP, SSRIs if needed (take ~2 weeks).
PERINATAL MOOD SPECTRUM — what is Perinatal Depression (PPD)?
Perinatal Depression (PPD): 10–15% (likely underreported); intense sadness, guilt, irritability, ruminations; persists beyond 2 weeks. Collaborative care: psychotherapy + meds (SSRI) + social supports.
PERINATAL MOOD SPECTRUM — what is Postpartum psychosis?
Postpartum psychosis: 0.1% — emergency within 2 weeks; rapid onset bizarre behaviour, hallucination, delusions; high association with bipolar disorder → urgent hospitalization, antipsychotics, mood stabilizers.
what are risk factors for perinatal mood disorders
Risk factors (box 24.4):
STRONG: prior psychiatric illness, prenatal anxiety, prior perinatal depression.
MODERATE: stressful life events, refugee/immigrant status, low support, adverse obstetrical outcomes, history of abuse, intimate partner violence, reproductive trauma.
WEAK: low SES, single parent, unplanned pregnancy, breastfeeding problems, substance use.
Clinical link: screening (EPDS), early education, and referral pathways are critical. Involve family supports; safety planning if suicidal or intrusive thoughts of harming baby.
what are POSTPARTUM NURSING ROLES
Postpartum nursing focuses on prevention, promotion, and education to support recovery after birth. Nurses assess maternal recovery, prevent complications, and promote comfort, rest, and readiness for future pregnancy.
POSTPARTUM NURSING ROLES (prevention) - what roles do nurses play in prevention of excessive bleeding? what are the primary intervention?
Most frequent cause: Uterine atony (uterus not contracting effectively).
Primary interventions:
Maintain uterine tone – ensure uterus contracts properly.
Prevent bladder distension – a full bladder prevents effective uterine contraction, increasing risk of postpartum hemorrhage (PPH).
POSTPARTUM NURSING ROLES (prevention) - what assesment can be done to watch for excessive bleeding?
Assessment of blood loss:
Visual assessment often underestimates blood loss.
Most accurate: weigh peripads → 1 gram = 1 mL of blood.
POSTPARTUM NURSING ROLES (prevention) - what are some bladder care interventions?
Bladder care interventions:
Encourage frequent voiding.
Techniques: running tap water, sitz bath, pour water over perineum.
Address pain and provide privacy to facilitate voiding.
POSTPARTUM NURSING ROLES (prevention) - what are some ipac method postpartum?
Infection prevention:
Maintain hygiene and a clean environment.
Change pads frequently.
Wash hands before perineal care.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of painmanagement
Pain management: Believe patient’s description; use pharmacological (Tylenol, ibuprofen) and nonpharmacological interventions. Encourage routine dosing to prevent pain escalation.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of fatigue
Fatigue: Encourage rest as tolerated. Fatigue is common due to labor, delivery, and newborn care.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of ambulation
Ambulation & exercise: Helps regain strength and prevents venous thromboembolism (VTE). Even in-bed exercises are beneficial.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of nutrition
Nutrition:
Non-lactating: ~1800–2000 kcal/day.
Lactating: +350–400 kcal/day to support milk production.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of bowl and bladder
Bowel and bladder function: Prevent constipation using ambulation, fluids, and fiber. Gas pain is common after cesarean section.
POSTPARTUM NURSING ROLES (promotion) - what are some promotion of breastfeeding
Breastfeeding: Initiate as early as possible, ideally in the first hour post-delivery.
what is important to note to the mother about RUBELLA in terms of future preg
Rubella (MMR)
Check immunity during pregnancy.
If non-immune: give subcutaneous MMR postpartum, safe while breastfeeding.
Avoid pregnancy for 4 weeks due to live attenuated vaccine.
Contraindications: immunocompromised patient or household members.
what is important to note to the mother about RH in terms of future preg
Rh Isoimmunization
For Rh-negative patients, administer Rh immune globulin within 72 hours postpartum to prevent maternal sensitization affecting future pregnancies.
POSTPARTUM COMPLICATIONS - Postpartum Hemorrhage (PPH): what is classified as hemorrhage
Definition: 500 mL after vaginal birth OR 1000 mL after cesarean section
POSTPARTUM COMPLICATIONS - Postpartum Hemorrhage (PPH): what are the diff between pri and second
Timing:
Primary: within 24 hours
Secondary: after 24 hours, up to 12 weeks postpartum
POSTPARTUM COMPLICATIONS - Postpartum Hemorrhage (PPH): what are the four T risk factors?
TONE (UTERINE ATONY):
Overdistended uterus (large fetus, twins, hydramnios)
Anesthesia/analgesia (e.g., conduction anesthesia)
High parity, prolonged labor, oxytocin use
Magnesium sulfate administration
Chorioamnionitis, obesity, subinvolution
TRAUMA:
Birth canal lacerations
Forceps or vacuum-assisted delivery
Cesarean birth
Ruptured/inverted uterus, manual placenta removal
TISSUE:
Retained placental fragments
Placenta accreta/increta/percreta
Placental abruption or previa
THROMBIN :
Thrombin, also known as Factor IIa, is a critical enzyme in the blood clotting process that converts fibrinogen into fibrin, forming a clot to stop bleeding
Coagulation disorders (don't have enough thrombin)
POSTPARTUM COMPLICATIONS - Postpartum Hemorrhage (PPH): what are the 9 assesments and interventions for PPH
Assess bleeding and signs of shock
Check fundus: firm or boggy
Boggy → massage fundus continuously
Do not leave patient; call for help immediately
Empty bladder
Administer uterotonics as ordered (e.g., oxytocin, ergonovine, misoprostol, Hemabate)
Monitor vital signs and hemodynamic status continuously
Laboratory studies: CBC, coagulation profile, blood type/crossmatch
Fluid and blood replacement therapy as needed
Surgical intervention if bleeding persists
Collaborative care: physicians, midwives, and nurses coordinate medication, fluids, and documentation
POSTPARTUM COMPLICATIONS - Venous Thromboembolism (VTE): what is VTE? what are the main types?
the medical term for blood clots that form in veins
Types: Superficial, DVT, PE
POSTPARTUM COMPLICATIONS - Venous Thromboembolism (VTE): what is vte a risk factors for pregnancy?
Risk: Pregnancy/postpartum increases risk 15-fold due to hypercoagulable state
POSTPARTUM COMPLICATIONS - Venous Thromboembolism (VTE): what are symptoms of dvt and pe?
Symptoms:
DVT: unilateral leg pain, calf tenderness, swelling, redness, warmth
PE: dyspnea, tachycardia, apprehension, cough, hemoptysis, fever, syncope, restlessness/anxiety
POSTPARTUM COMPLICATIONS - Venous Thromboembolism (VTE): what are ways to treat superficial, dvt, and pe?
Superficial: analgesia, rest with elevation, compression stockings, heat
DVT: anticoagulants, rest, elevation, compression stockings, 3 months of oral anticoagulants
PE: continuous heparin infusion followed by anticoagulants for up to 6 months
POSTPARTUM COMPLICATIONS - Postpartum Infections: what is it?
Definition: any infection within 42 days postpartum
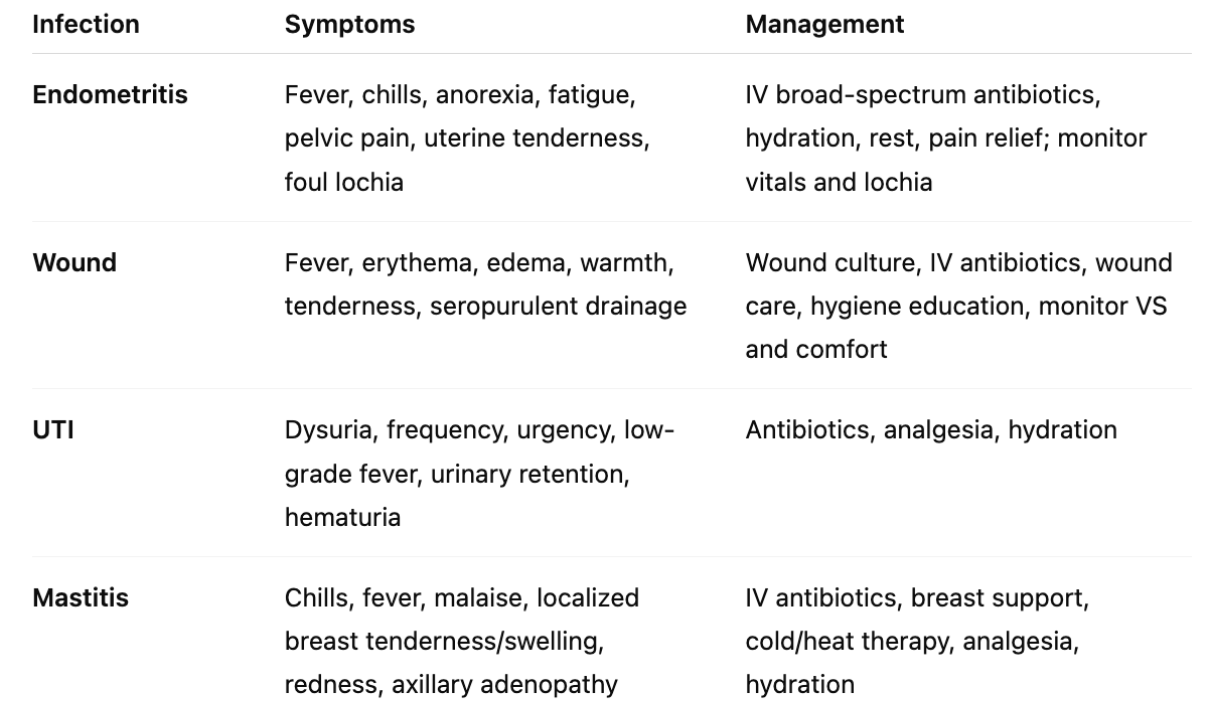
POSTPARTUM COMPLICATIONS - Postpartum Infections: what are the four common types of infections? what are they
?
endometritis = an inflammation of the inner lining of the uterus, called the endometrium, usually caused by an infection
wound infection (C-section) = occurs when bacteria enter the surgical incision, leading to symptoms like increased pain, redness, swelling, fever, and discharge from the wound
urinary tract infection (UTI) = occur when bacteria enter the urinary tract through the urethra and begin to spread in the bladder.
mastitis = swelling and redness, called inflammation, of breast tissue
POSTPARTUM COMPLICATIONS - Postpartum Infections: what are some symtoms and management for each?
what is the BABY-FRIENDLY HOSPITAL INITIATIVE (BFHI)
A joint initiative by WHO and UNICEF aimed at promoting optimal breastfeeding and infant care practices in hospitals.
Hospitals can receive a “Baby-Friendly” designation if they implement 10 evidence-based steps to support breastfeeding families.
what are benefits of breastfeeding for the BABY
Reduced mortality (fewer infant deaths).
Immune support: Enhances gastrointestinal and immune maturation.
Reduced disease risk:
Gastroenteritis, celiac disease, Crohn disease, necrotizing enterocolitis (especially preterm infants).
Respiratory illnesses (RSV, pneumonia), otitis media, urinary tract infections, bacterial meningitis.
Certain allergies (esp. in high-risk families).
Lower SIDS risk.
Possible long-term protection against lymphoma and type 1 & 2 diabetes.
Dental development: Decreased malocclusions.
Cognitive development: Enhanced in term and preterm infants.
Pain relief during procedures (e.g., heel prick, injections).
what are benefits of breastfeeding for the MOM
Physical health:
Decreased postpartum bleeding and faster uterine involution.
Reduced risk of breast & ovarian cancer, rheumatoid arthritis, hypertension, cardiovascular disease, type 2 diabetes.
More rapid postpartum weight loss; protection against osteoporosis.
Reproductive health: Delayed return of menses.
Psychosocial:
Unique bonding experience.
Increased maternal role attainment.
May reduce risk of perinatal mood disorders when breastfeeding difficulties are properly addressed.
what are benefits of breastfeeding for the FAMILY
Convenience: Ready-to-feed; no bottles or special equipment required.
Cost-effective: Less expensive than formula; reduces healthcare costs.
Work & social impact: Reduced parental absence due to infant illness.
Environmental impact: Lower waste from formula packaging.
what are some contraindications to breastfeeding for the MOM
Cancer therapy, radioactive isotopes/iodine.
Active untreated tuberculosis.
HIV-positive in high-income countries (risk of viral transmission).
Maternal HTLV I/II infection.
Certain medications (e.g., antineoplastics, some anticonvulsants).
Substance use: managed methadone is not a contraindication.
what are some contraindications to breastfeeding for the BABY
Galactosemia (cannot metabolize galactose).
what are best practices in breatfeeding?
Immediate skin-to-skin contact for 1–2 hours after birth.
First feed:
Assess breast/nipple appearance.
Evaluate parent’s understanding of breastfeeding.
Provide assistance and education (responsive, cue-based feeding).
Before discharge:
Assess positioning and latch.
Teaching tip: Normalize challenges—breastfeeding is natural but not always easy. Support is crucial to prevent postpartum stress and anxiety.
what are some key postpartum health teachings?
Self-care & signs of complications: Nutrition, rest, exercise after six-week checkup.
Medications: Finish prenatal vitamins; continue any prescribed medications.
Sexual activity & contraception: Generally wait six weeks; menses may return sooner in non-breastfeeding parents.
Coping with visitors: Encourage asserting needs; prioritize rest and bonding.
Routine checkups:
Mother: 6 weeks postpartum.
Infant: 3–5 days (or earlier depending on risk).
Community support: Home visits, telehealth lines (breastfeeding support), support groups.
what is the transition to parenthood described as?
Described as a developmental transition, not a crisis.
Can involve disorder, disequilibrium, and satisfaction.
Usual coping methods may be insufficient.
Opportunity for developing new coping strategies.
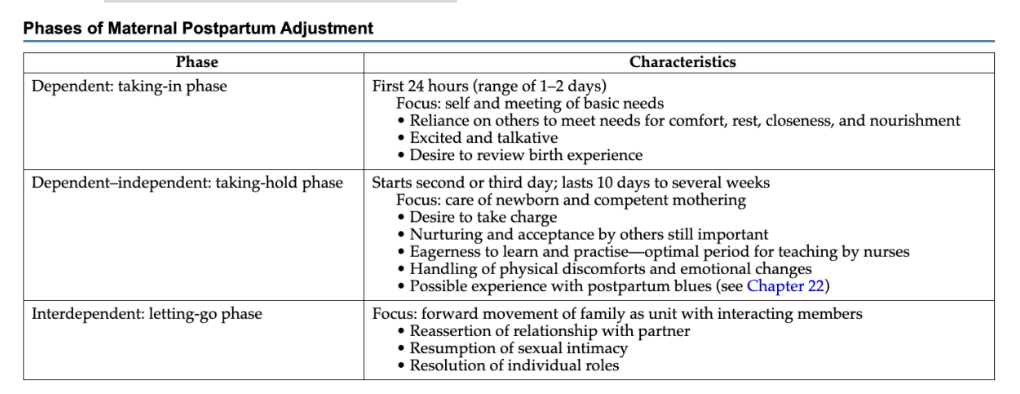
what are the 3 STAGES OF MATERNAL POSTPARTUM ADJUSTMENT according to RUBIN
Dependent (Taking-in phase) – first 24 hours: focus on self, relies on others for comfort and basic needs.
Dependent-independent (Taking-hold phase) – day 2–10 weeks: focus on newborn care, learning, nurturing; ideal for nurse-led education.
Interdependent (Letting-go phase) – moving forward as a family unit; reassert partner relationship, resume intimacy.
what are the 4 STAGES OF MATERNAL POSTPARTUM ADJUSTMENT according to MERCER
Commitment & preparation – during pregnancy.
Acquaintance & attachment – first 2–6 weeks postpartum; learning care, physical restoration.
Move toward new normal – adjusting to life changes.
Achievement of maternal identity – around 4 months, incorporating motherhood into self-concept.
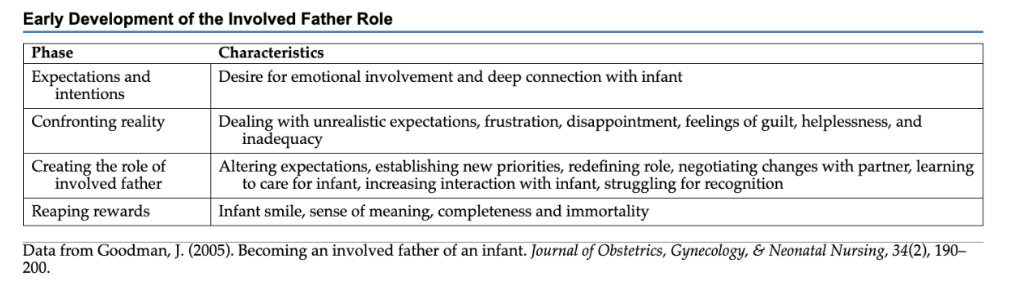
what are the 4 STAGES OF PATERNAL POSTPARTUM ADJUSTMENT according to GOODMAN
Early development: Expectations, emotional connection
Confronting reality of challenges: guilt helplessness and inadequacy
Role creation: Negotiating responsibilities, learning infant care, balancing partner and infant needs.
Reaping rewards: Infant smiles, sense of meaning; usually noticeable around six weeks.
what are some diversity considerations postpartum?
Adolescent mothers: Developmental tasks may conflict with parenting; higher risk of perinatal mood disorders.
Maternal age > 35: May have less support, more career/life conflicts.
LGBTQ2 partners: Often underrepresented in parenting support; need validation and inclusion.
Indigenous families: Historical trauma (residential schools, forced sterilization) impacts trust; care should be trauma-informed, culturally sensitive.
what is perinatal loss?
Includes infertility, premature birth, cesarean when unplanned, newborn death.
Newborn deaths in Canada: ~3.3/1000 in first month; ~4.4/1000 in first year; leading cause: prematurity.
what are the grief phases during perinatal loss?
Shock & numbness – acute, intense distress; difficulty decision-making.
Searching & yearning – sadness, guilt, anger.
Disorientation – deep depression; lasts months.
Reorganization & resolution – gradual adjustment; can take 24+ months.
what are basic nursing care when it comes to perinatal loss?
Use direct language (“baby has died” vs “gone”).
Support decision-making (autopsy, investigations).
Normalize grief; facilitate coping.
Physical comfort and memory-making (photos, footprints, keepsakes).
Documentation and legal considerations are critical.
Prepare families for physical changes postpartum, especially if lactation occurs after loss.