26. Surgical diseases of the urinary bladder & urethra. Cystotomy, cystectomy, urethrotomy & urethrostomy in dog & tomcats.
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
84 Terms
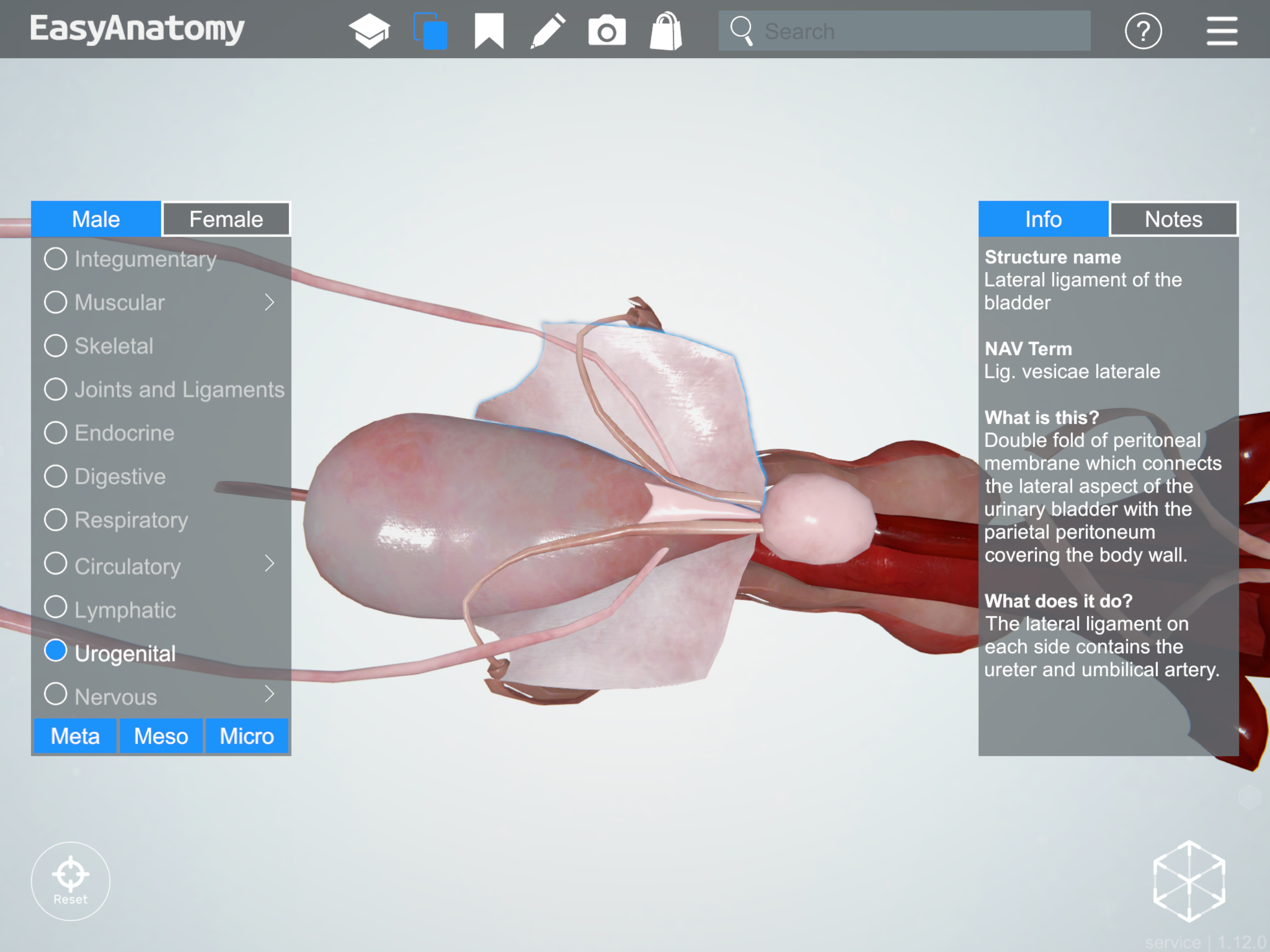
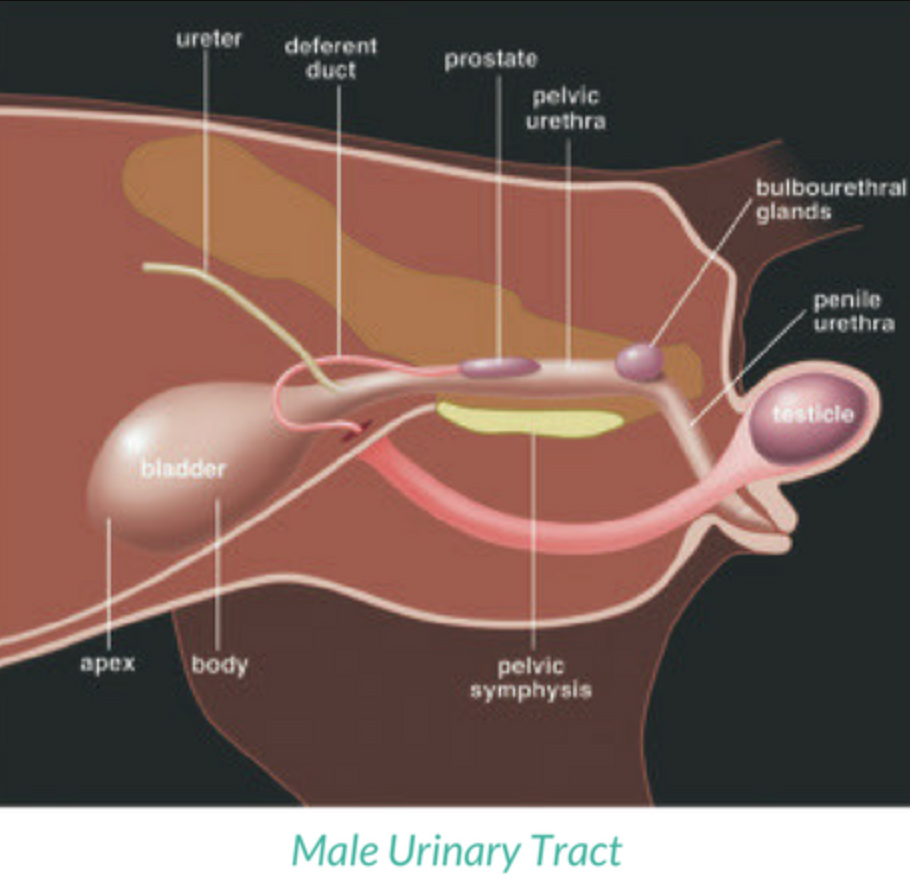
Within the peritoneal cavity, attached to the abdominal wall by loose, double-layered peritoneal ligaments
What are the names of the ligaments attaching the bladder?
Ventral median ligament: very thin structure connecting bladder to linea alba & pelvic symphysis.
Lateral ligaments: attach pelvic walls & contain fat along with distal portion of ureter & umbilical artery on each side.
What are examples of surgical diseases of the urinary bladder?
Rupture
Urolithiasis
Neoplasia
Cystitis
Trauma, severe cystitis, neoplasia, urethral obstruction (FLUTD), calculi, iatrogenic injury
Haematuria, anuria, dysuria, abdominal pain, uroabdomen, azotaemia, dehydration, metabolic acidosis, hyperkalemia, death
Higher creatinine in fluid than in serum
Stabilisation (often with other injuries e.g. pelvic fracture), exploratory laparotomy, resection of unviable tissue, omentalisation
Struvite (alkaline)
Calcium oxalate (acidic)
Conservative: Diet change, dissolution (struvite, urate, cystine)
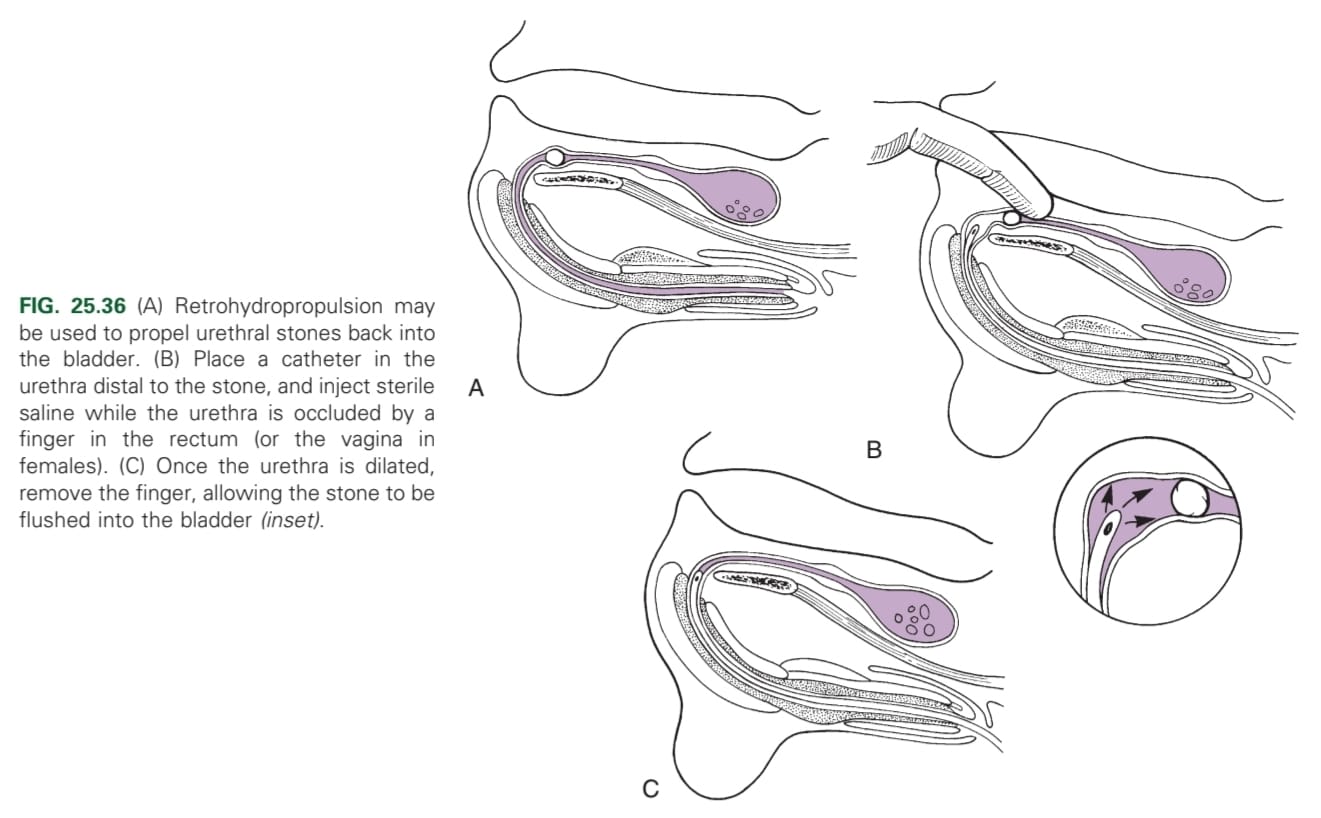
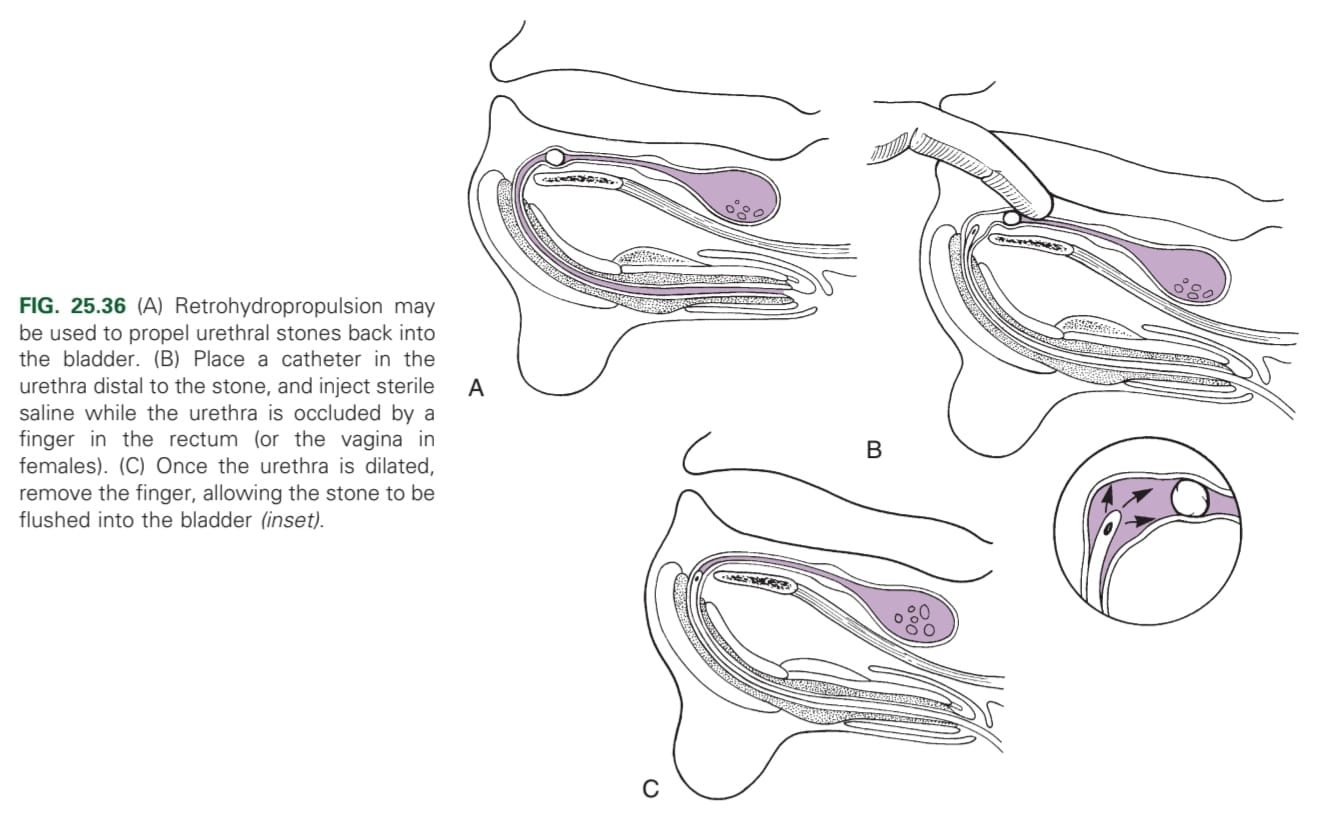
Surgical removal (cystotomy/urethrotomy), hydropropulsion
What are some types of bladder neoplasia?
Transitional cell carcinoma, lymphoma, adenocarcinoma, squamous cell carcinoma, haemangioma, haemangiosarcoma, fibroma, fibrosarcoma, leiomyoma, leiomyosarcoma
Surgical excision (may be impossible due to location), NSAIDs, chemotherapy, cystectomy
Bacterial infection, urolithiasis, neoplasia, polypoid cystitis
What is polypoid cystitis?
Uncommon, non-neoplastic inflammatory disease of the cranvioventral bladder
Pollakiuria, dysuria, stranguria. Haematuria (haemorrhage from polyp)
Palpation, X-ray (thickened bladder wall), cystoscopy
Depends on aetiology; antibiotics, NSAIDs, cystotomy (if unresponsive), resection of polyps
Monofilament, absorbable. Less drag in bladder, & less introduction of MO
Simple continuous, full-thickness provides accurate apposition
Simple interrupted appositional for irregularly shaped bladder defects after resection
Cushing or Lembert if leaking is a concern. Done after simple continuous
Schmieden suture pattern (appositional)

What is the procedure for a cystotomy?
Midline laparotomy incision from umbilicus to pubis (curving parapreputially through skin & subQ in male dogs). Identify & isolate bladder. Flip to reveal dorsal side. 4x stay sutures placed: 2 each side of incision site (very close to incision). Cystotomy incision made in midline (stab incision, remove urine & blood by suction) → Further stay sutures on either side of incision. Closure: Lembert/ Connel-Cushing suture (inverting) → double. Routine closure of linea alba.
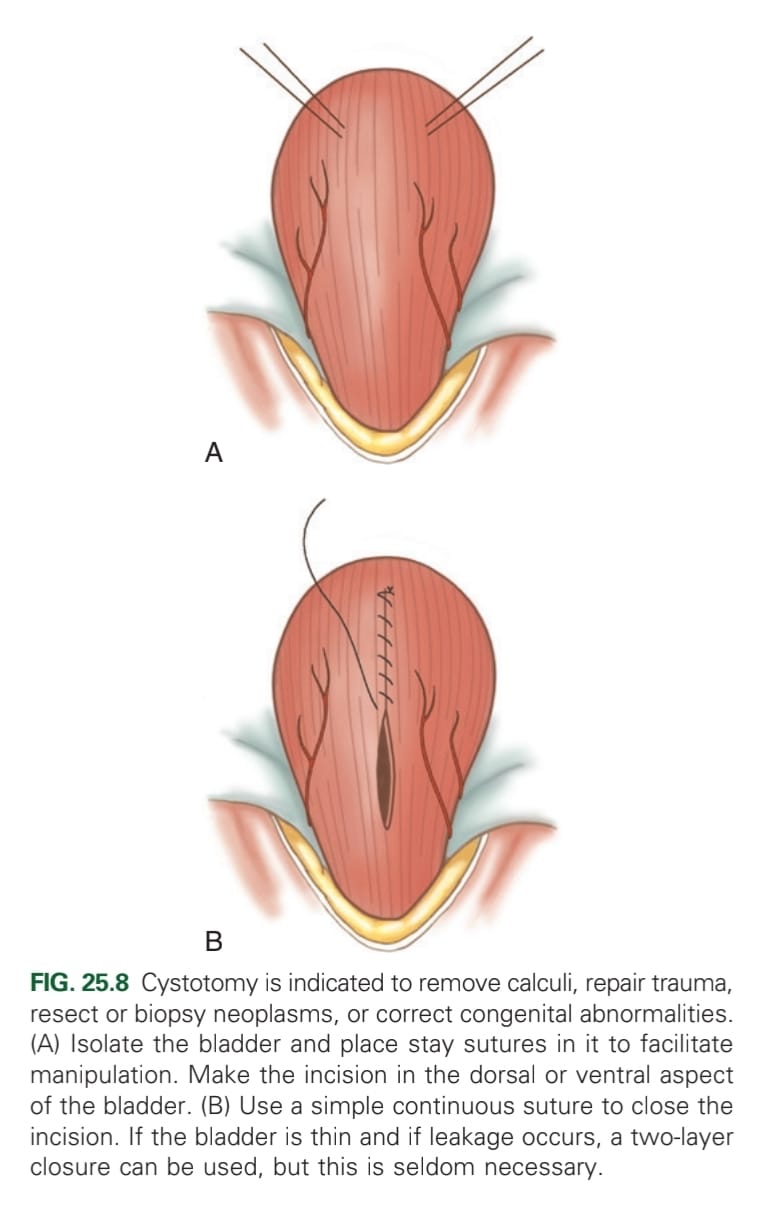
Temporary cystostomy tube or indwelling urethral catheter
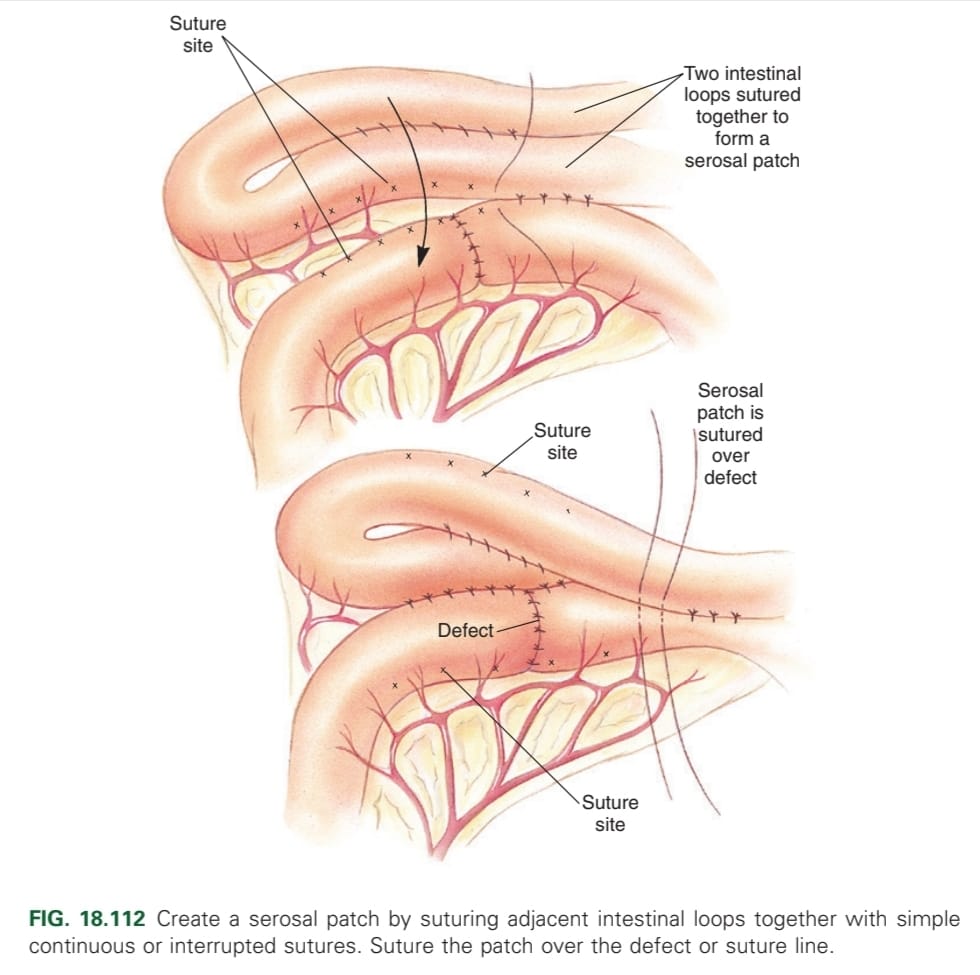
What can be done if tissues of the bladder are friable after a cystotomy?
Create a serosal patch over the incision line
What is distinct about the male cat urethra?
More distinct preprostatic urethra
What are examples of surgical diseases of the urethra?
Obstruction
Stricture
Prolapse
Calculi (Ca oxalate, struvite, cysteine, urate (hepatic encephalopathy – allopurinol))
What are some diagnostic tests for urethral obstruction?
Haematology: normal (inflammation can lead to stress leukogram)
Biochemistry: azotemia, met. acidosis, HyperP/K, hypoCa
Imaging: positive contrast urethrography, double contrast cystography or excretory urography
Urinalysis & culture (haematuria, proteinuria, crystalluria)
Medical management (pain relief, medication to relax the urethra, fluids)
Dietary change
Urohydropropulsion
Surgery (perineal urethrostomy)
What may predispose to urate stones?
Hepatic encephalopathy (allopurinol = treatment)
When is treatment for urethral strictures indicated?
Only when there are signs of obstruction
What are some clinical signs of urethral prolapse?
Congested mucosal mass protrudes from external urethral orifice with varying degrees of haemorrhage. Persistent urethral bleeding, leaking, dysuria, pollakiuria, anaemia
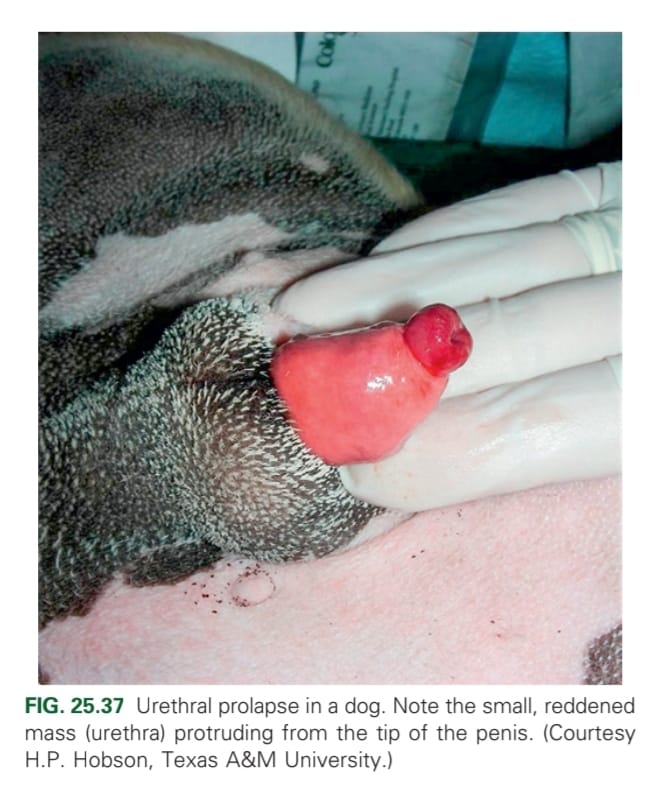
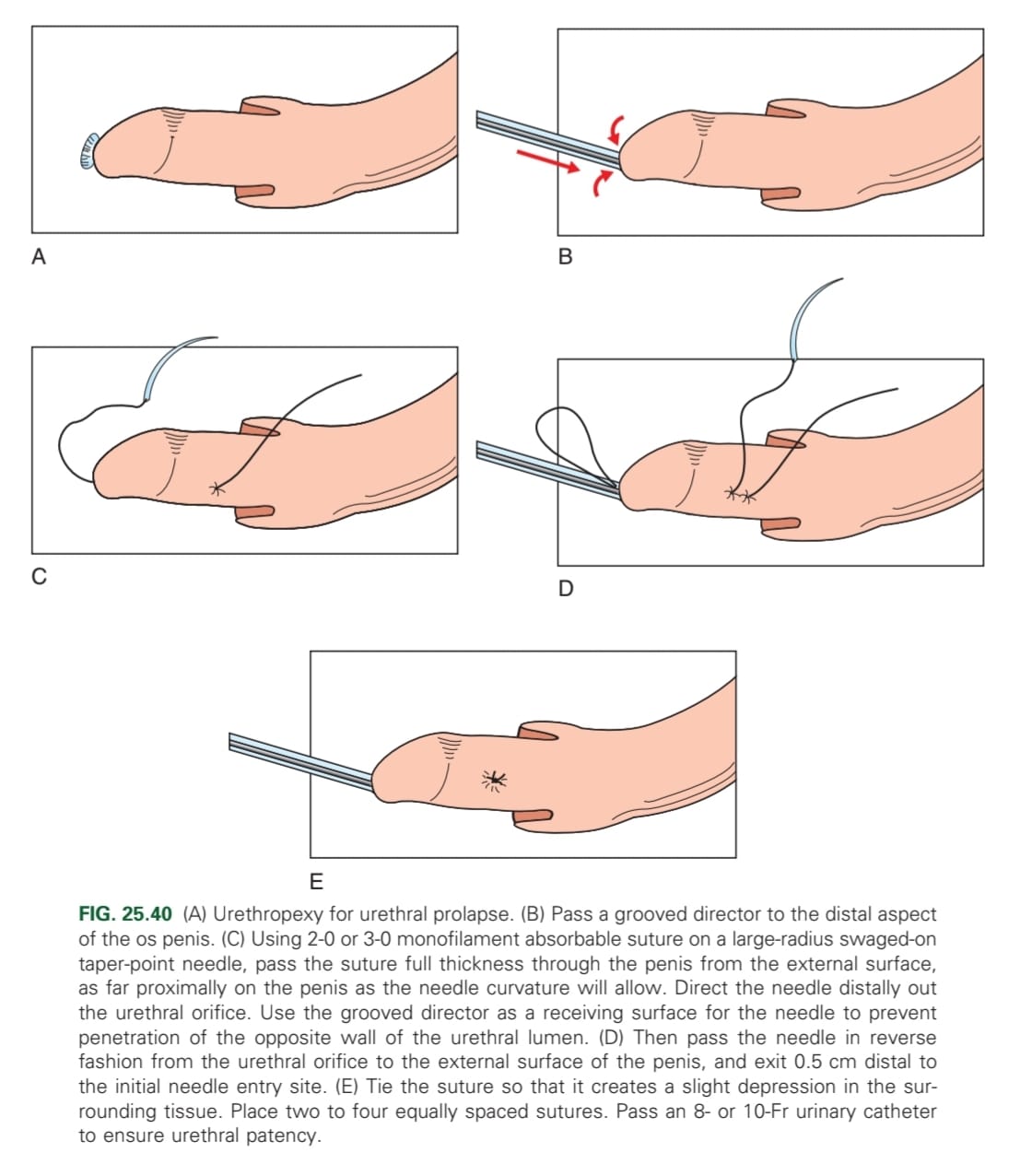
Castration, urethral resection, urethropexy, antibiotics
What are examples of urethral surgeries?
Urethrotomy
Urethrosomy
Prescrotal or perineal
What is the positioning of the animal for a prescrotal urethrotomy?
Dorsal recumbency → remove calculi from distal penile urethra
What is the positioning of the animal for a perineal urethrotomy?
Sternal recumbency → remove calculi at the level of the ischial arch
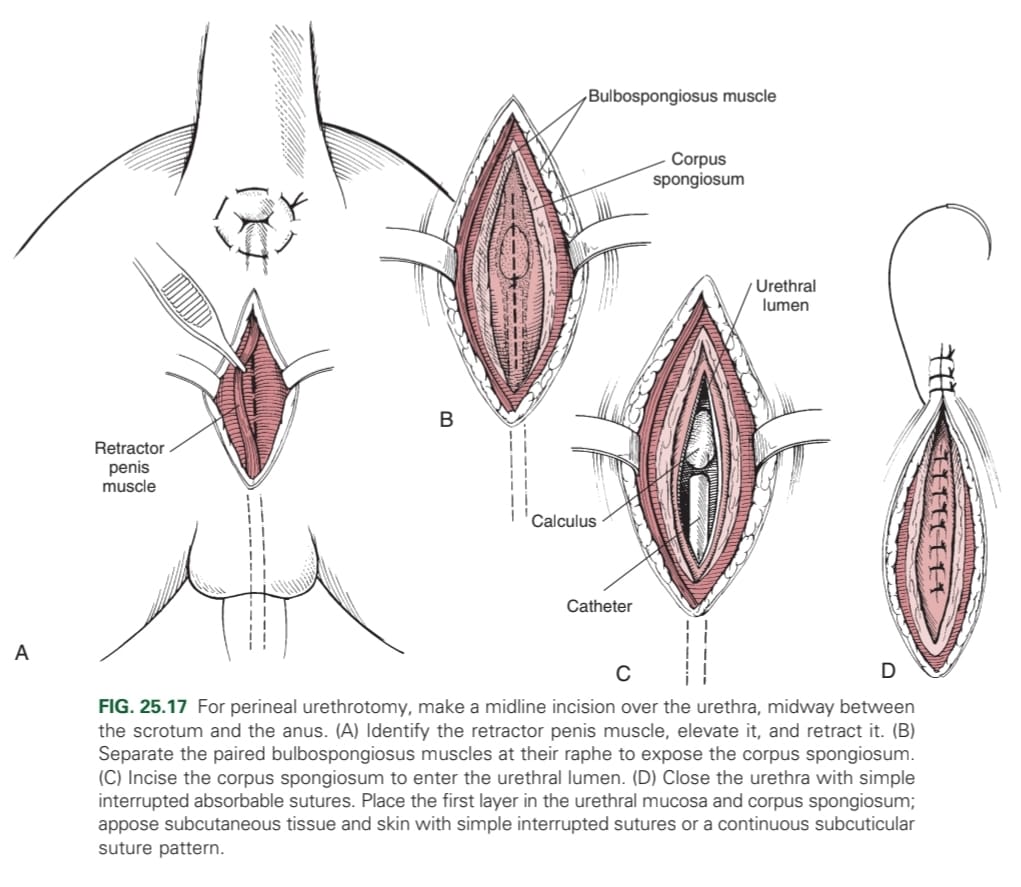
How is a perineal urethrotomy closed?
Sutures
Prescrotal, scrotal (dogs), perineal (cats), prepubic, subpubic
Perineal or subpubic
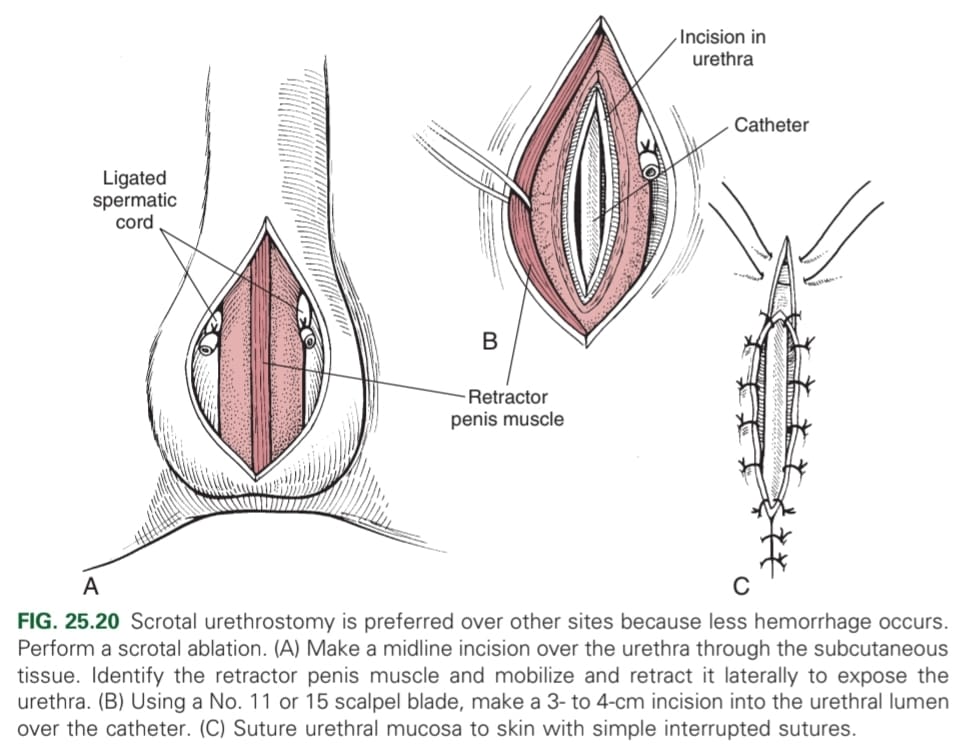
What is the general procedure for a scrotal urethrostomy?
Dorsal recumbency: place urinary catheter, elliptical incision around or near base of scrotum in intact male dogs or remnants of neutered ones.
Castration performed in routine manner.
Interrupted sutures placed on tunica albuginea to subcutaneous tissue on either side of urethrostomy site.
Incision into lumen of urethra on ventral midline.
Closed by suture to skin on each side in a single layer simple interrupted or continuous pattern, monofilament, absorbable or nonabsorbable.
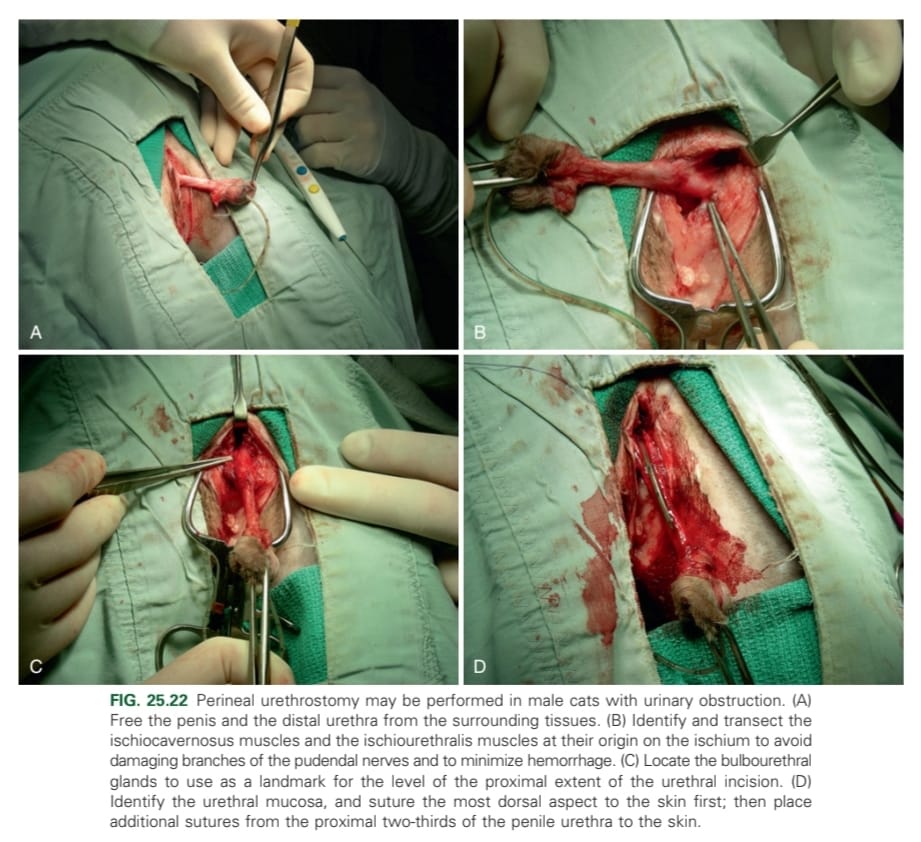
What is the general procedure for a perineal urethrostomy in cats?
Penis and distal urethra are freed from surrounding tissues
Transect m. ischiocavernosus and m. ischiourethralis near their origin on the ischium to avoid damaging the n. pudendalis branches
Urethra transected proximal to penile portion near bulbourethral glands
Pelvic urethra sutured to perineal skin from dorsal aspect
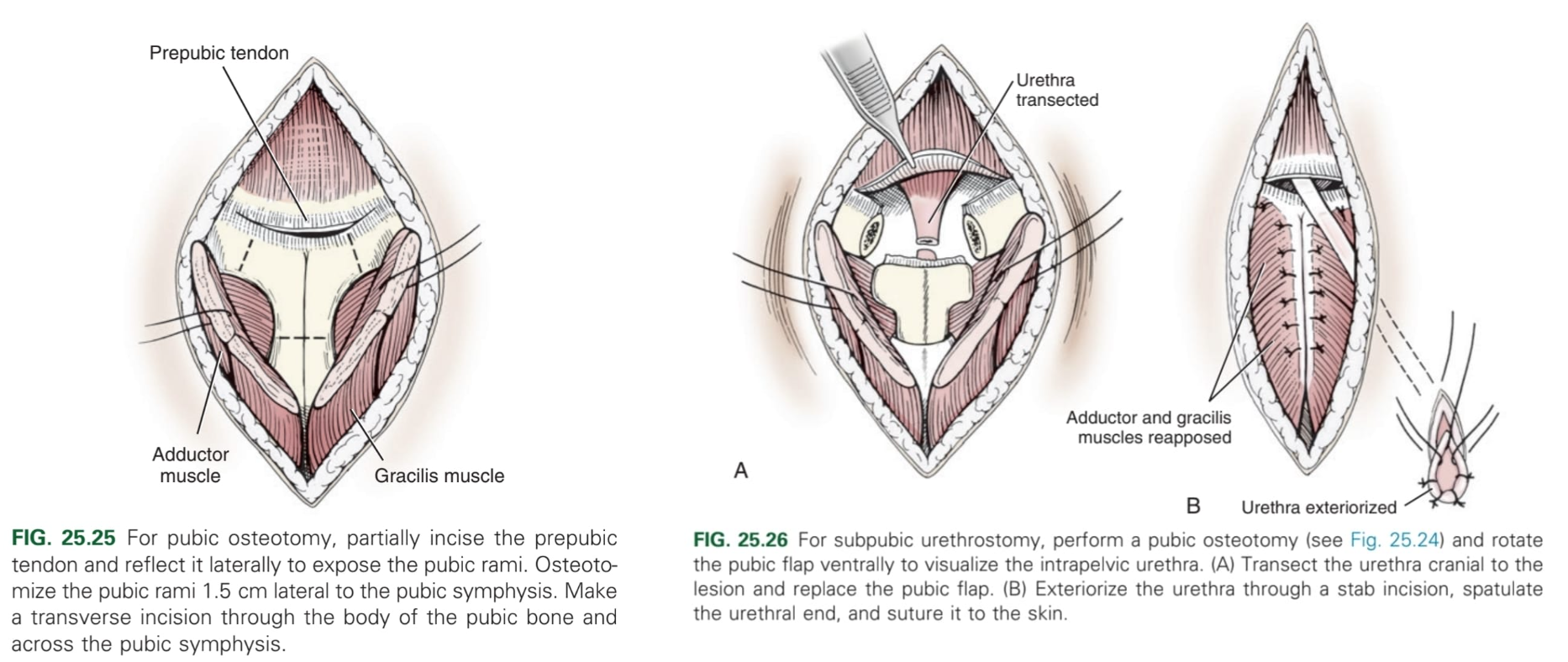
What is the procedure for a subpubic urethrostomy in cats?
Ventral midline incision from umbilicus to pubis → Partially incise prepubic tendon and reflect it laterally to expose pubic rami → (pubic osteotomy) osteotomise pubic rami 1.5 cm laterally to pubic symphysis and transverse incision through body of pubic bone → rotate pubic flap ventrally to visualise intrapelvic urethra → transect urethra cranial to lesion/obstruction and replace pubic flap → urethra exteriorised caudal to the brim of the pubis through stab incision → spatulate urethral end and suture to skin.
History, clinical signs, physical exam (thickened wall), rectal palpation, urinalysis, X-ray, ultrasound, biochemistry, haematology
Conservative (IV fluids, antibiotics, diet, opioids)
Surgical (catheterisation, cystocentesis, urethrotomy, cystotomy)
Where is the trigone of the bladder?
Dorsally
What are the ligaments of the bladder?
Ventral median ligament: very thin structure connecting bladder to linea alba & pelvic symphysis.
Lateral ligaments: attach pelvic walls & contain fat along w/ distal portion of ureter & umbilical artery on each side.
Where are incisions on the bladder made?
Ventrally as has less blood vessels
What percentage of the bladder can be removed and it still stay functional?
40%
Where are urethrostomies usually carried out?
Base of the penis where the urethra is the most narrow
Which urinary crystals are not visible on USG?
Urate, cysteine
What are the types of cystocentesis?
Blind or USG-guided