[CPR] Physical Diagnosis of the Respiratory System
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
63 Terms
What is the difference between a symptom and a sign?
A symptom is subjective and the complaint as reported by the patient, while a sign is objective and are findings by the medical professional. For example, a patient reporting pain in a certain area is a symptom that can be confirmed by palpating for tenderness in the area, which is a sign.
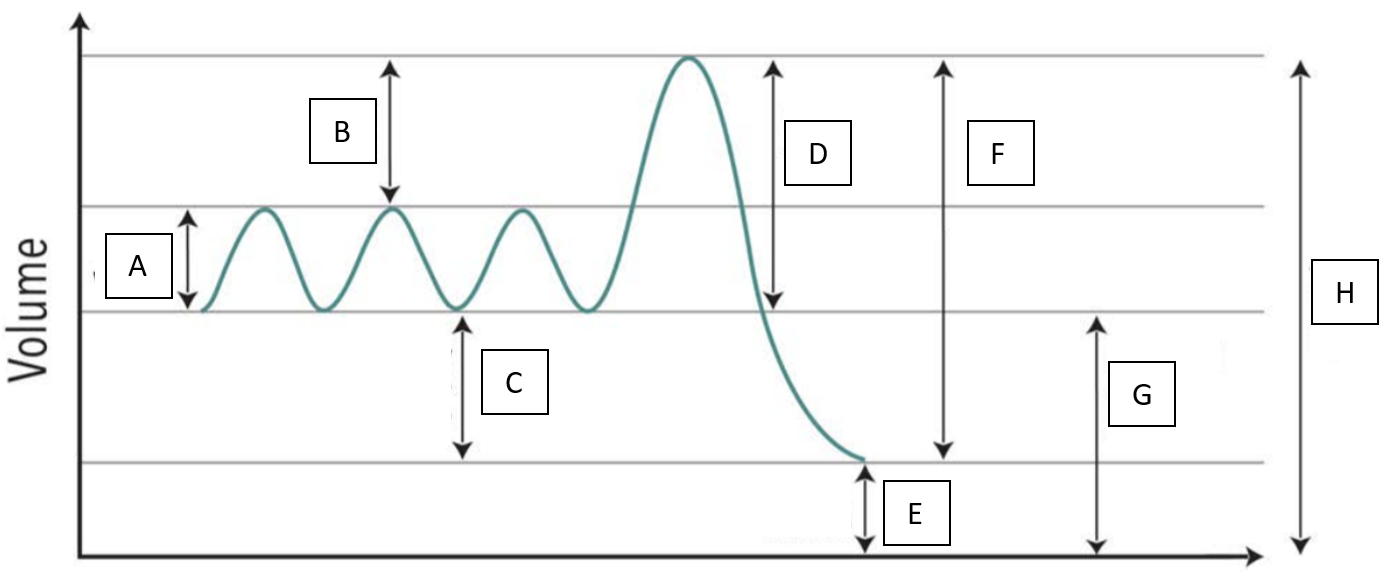
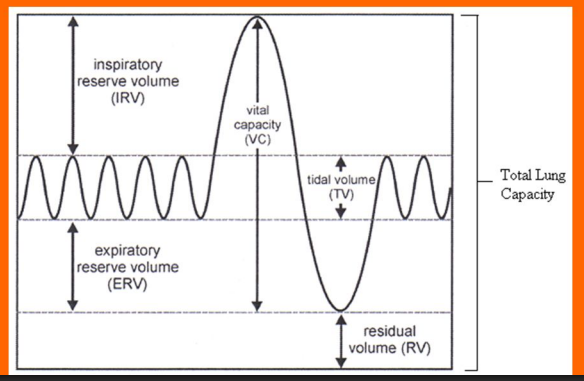
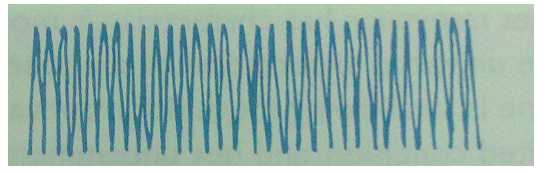
Explain all of the components of the breathing intensities graph.
Tidal Volume — amount of air that moves in or out of the lungs during normal, quiet breath
Inspiratory Reserve Volume (IRV) — extra volume of air that can be inhaled with maximum effort after a normal inhalation
Expiratory Reserve Volume (ERV) — extra volume of air that can be forcibly exhaled after a normal exhalation
Residual Volume (RV) — air that remains in the lungs even after you exhale as hard as possible; it prevents the lungs from collapsing
Vital Capacity (VC) — maximum amount of air a person can expel from the lungs after a maximum inhalation (VC = IRV + TV + ERV)
Total Lung Capacity — total volume of air in the lungs after a maximum inhalation (TLC = VC + RV)
This pattern of breathing is the normal, regular, and comfortable breathing.
Follow Up Question: What is the normal RR and how does age affect this?
Eupnea
12-20 cpm (age-dependent); older people have a lower RR while younger people have a faster RR
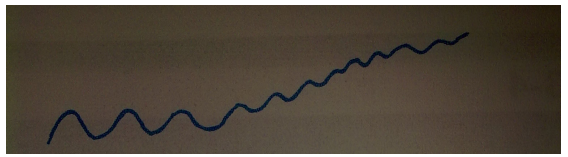
This pattern of breathing is characterized by an increased RR (>20 cpm) and may be deep or shallow. It can be caused by exercise, infection, acidosis, hypoxemia, or heart failure. It can also be due to a pulmonary, neurologic, or psychiatric condition or an obstruction.
Follow Up Question: Is deep or shallow breathing more dangerous
Tachypnea
Shallow breathing is more dangerous since a not a lot of gas exchange is occurring.
This is the term to describe the lack of oxygen in the blood.
Hypoxemia
This is the term to describe the lack of oxygen in the tissues.
Hypoxia
This is the clinical manifestation or sign of hypoxemia and hypoxia.
Cyanosis (blue skin)
This pattern of breathing is characterized by a decreased RR (>12 cpm). It can be caused by obesity, hypothyroidism, hypokalemia, electrolyte imbalances, and drugs.
Follow Up Question: How does hypokalemia and hypothyroidism slow down RR?
Bradypnea
Hypokalemia, or decreased potassium, can lead to hypokalemic paralysis, which leads to weak muscles, including the respiratory muscles. This may present as bradypnea.
Hypothyroidism also leads to bradypnea in this same way.
This breathing pattern is described as hyperventilation (>20 cpm) and deep breathing. It can have neurologic, psychologic, metabolic, and infectious causes.
Follow Up Question: What specific condition following a stroke (ACA) can lead to this type of breathing?
Hyperpnea
Neurocirculatory asthenia
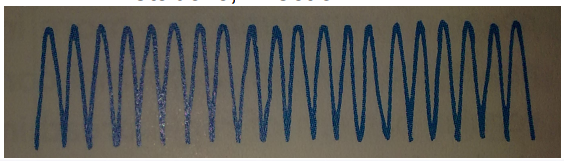
This pattern of breathing is voluntary, frequently interspersed, and of deeper breaths.
Sighing
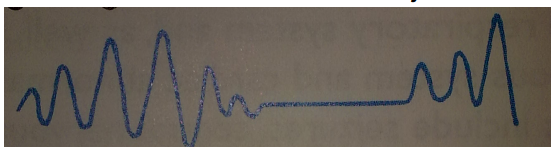
This pattern of breathing is abnormal and is characterized by increasing difficulty in getting air out or exhaling.
Air trapping
expiration; barrel-chested
Air trapping can occur in patients with what conditions?
Follow Up Question: Patients with this breathing pattern and these conditions have a problem in which specific part of breathing and what physical manifestation do they normally have?
Asthma or COPD
Expiration; barrel-chest
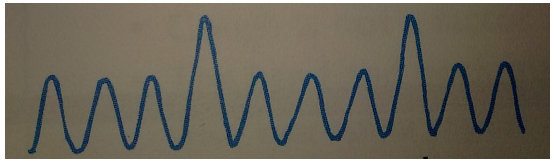
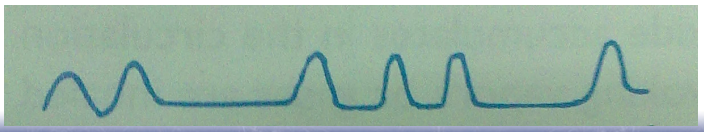
This pattern of breathing is characterized by varying periods of increasing depths interspersed with apnea.
Cheynes-Stokes
Cheynes-Stokes normally connote what?
It normally connotes a grave condition such as heart failure, stroke, brain tumors, or TBIs.
What is the immediate intervention in a patient with Cheynes-Stokes and how is it corrected?
The immediate intervention is to provide the patient with artificial respiration, such as intubation and connecting him to a respiration. It is corrected by treating the underlying metabolic problem that causes this breathing pattern.
This is common in patients post-op (with regards to the video of the post-bypass patient). It becomes a metabolic problem and not a surgical problem.
This breathing pattern is rapid, deep, and labored. It is similar to hyperventilation.
Follow Up Question: What is the difference between this breathing pattern and hyperventilation
Kussmaul breathing
Kussmaul breathing normally proceeds a medical condition while hyperventilation does not.
Kussmaul breathing normally occurs in patients with what conditions?
Acidosis or renal failure
This condition is characterized by too much acid in the blood and is seen in patients with renal failure.
Follow Up Question: How does this condition occur and how does it lead to Kussmaul breathing?
Acidosis
Because the kidneys are unable to maintain the pH level of the blood, CO2 becomes H2CO2 (carbonic acid), making the blood acidic. To maintain homeostasis, the body uses a negative feedback mechanism and exhales more CO2 by breathing faster and exhaling more.
This is the condition of patients with high acidity in the blood due to diabetes.
Follow Up Question: How does their breath smell?
Diabetic ketoacidosis
Their breath smells sweet.
This breathing pattern is characterized by irregularly interspersed periods of apnea in a disorganized sequence of breaths. It can be caused by trauma or stroke.
Follow Up Question: This breathing pattern can occur due to damage to what brain structure?
Biot
Damage or pressure to the medulla oblongata due to a hemorrhage, tumor, or traumatic causes.
This breathing pattern is characterized by significant disorganization with irregular and varying depths of respiration.
Follow Up Question: What is the prognosis of patients with this breathing pattern and damage to which brain structure leads to this breathing pattern?
Ataxic breathing
Poor prognosis; medulla oblongata
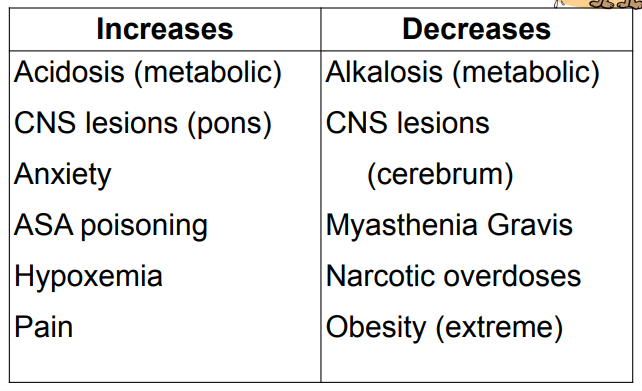
Identify the influence of the following factors or conditions on the rate and depth of breathing.
Acidosis (metabolic)
CNS lesions (pons)
Obesity (extreme)
Pain
ASA poisoning
Myasthenia Gravis
Narcotic overdoses
Anxiety
CNS lesions (cerebrum)
Hypoxemia
Alkalosis (metabolic)
Increases
Increases
Decreases
Increases
Increases
Decreases
Decreases
Increases
Decreases
Increases
Decreases
What are the brain structures responsible for voluntary and involuntary breathing respectively?
Follow Up Question: If the brain structure responsible for involuntary breathing is damaged, what effect does this have on the patient’s sleep?
Cortex for voluntary breathing and dorsal respiratory group (DRG) of the medulla for involuntary breathing
If the DRG is damaged, a patient will not be able to go to sleep.
This is the term used to describe difficulty in breathing, labored breathing, or shortness of breath. It is commonly observed in pulmonary or cardiac compromise.
Follow Up Question: Does this increase or decrease with the severity of the underlying disease?
Dyspnea
It increases with severity of the underlying disease.
What are questions to ask regarding the patient’s dyspnea?
Is it present even at rest?
How much walking? On a level surface? Up the stairs (number of stairs)?
Is it necessary to stop and rest when climbing stairs?
What other activities precipitate it? What level of physical demand (light, moderate, strenuous)?
This is dyspnea that begins or increases when the patient lies down.
Follow Up Question: How can this be quantified?
Orthopnea
Quantified by the number of pillows (6 in per pillow) needed to lie down comfortably (docu: 4-pillow orthopnea)
This is the sudden onset of dyspnea after a period of recumbency.
Follow Up Question: For patients with this, what do they do to relieve it?
Paroxysmal Nocturnal Dyspnea (PND)
Sitting up is helpful
Differentiate orthopnea and PND in terms of their pathophysiological mechanisms.
Both of them have the same mechanism of blood backflowing to the lungs due to a weaker heart being unable to adapt to the increased venous return after lying down.
Patients with orthopnea have weaker hearts as this condition occurs faster than PND, while patients with PND have stronger hearts and are able to tolerate the increased venous return for a certain amount of time.
This is dyspnea that begins or increases when the patient is upright.
Follow Up Question: What condition does this occur in and why?
Platypnea
This usually occurs in patients with cardiac defects (i.e. ASD with right-to-left shunts) and worsening VQ mismatch.
Why do patients with ASD experience platypnea?
Patients with ASD have a hole in between the two atria and normally blood flows from the left atria to the right atria due to the higher pressure in the left atria. However, when a right-to-left shunt occurs, blood can be forced back into the lungs, leading to platypnea.
This is dyspnea that is pronounced on side-lying.
Follow Up Question: Why does this occur?
Trepopnea
Due to a unilateral diseased lung
For a patient with a collapsed lung, what side should he lie on?
Side-lying on the collapsed lung
What are the 10 Ps of Dyspnea of Rapid Onset?
Pneumonia — secretions in the alveolar scas
Pneumothorax — air in the pleural space
Pulmonary Constriction/Asthma
Peanut (foreign body)
Pulmonary embolus
Pericardial tamponade — increased fluid in the pericardial sac leading to heart failure and dyspnea
Peak seekers (high altitudes)
Psychogenic
Poisons
This is a common symptom of a respiratory problem which can be due to localized or more general insults at any point of the respiratory tract. It may be a voluntary or reflexive response to an irritant.
Follow Up Question: Why is it important that post-bypass patients are able to do this?
Cough
Post-bypass patients are unable to cough due to pain and being unable to do this can lead to pneumonia or infections.
What is the sequence of events when coughing?
usually preceded by a deep inspiration closure of glottis
contraction of chest, abdominal and pelvic muscles sudden spasmodic expiration (forces open the closed glottis)
air and secretions are exhaled
What can lead to these sputum characteristics?
Yellow, green, rust (blood mixed with yellow sputum), clear, or transparent; purulent; blood streaked; mucoid, viscid
Bacterial infection
What can lead to these sputum characteristics?
Mucoid, viscid; blood streaked (not common)
Viral infection

What can lead to these sputum characteristics?
Yellow, green, rust (blood mixed with yellow sputum), clear, or transparent; purulent; blood streaked; mucoid, viscid
Particularly abundant in the early morning; slight, intermittent, blood streaking; occasionally, large amounts of blood
Chronic infectious disease
What can lead to these sputum characteristics?
Slight, persistent blood streaking
Carcinoma
What can lead to these sputum characteristics?
Blood clotted; large amounts of blood
Infarction — has more blood than CA but less than TB
What can lead to these sputum characteristics?
Large amounts of blood
Tuberculous Cavity (TB) — has more blood than CA
What would be the smell of the breath of patients with these conditions?
Diabetic ketoacidosis; starvation ketosis
Sweet, fruity
What would be the smell of the breath of patients with these conditions?
Uremia
Follow Up Question: Why is this the smell?
Fishy and stale or ammonia-like (worse)
Uremia is renal failure, meaning that the kidneys are unable to clean out toxic waste.
What would be the smell of the breath of patients with these conditions?
Fetor hepaticus: hepatic failure, portal vein thrombosis, portocaval shunts
Musty fish, clover
What would be the smell of the breath of patients with these conditions?
Intestinal obstruction, diverticulum
Foul, feculent (like fecal matter)
What would be the smell of the breath of patients with these conditions?
nasal/sinus pathology: infection, foreign body, cancer: respiratory infections: empyema, lung abscess, bronchiectasis
Foul, putrid
What would be the smell of the breath of patients with these conditions?
Tonsillitis, gingivitis, respiratory infections, vincent angina, gastroesophageal reflux, peptic ulcer disease (PUD)
Halitosis (bad breath)
What would be the smell of the breath of patients with these conditions?
Cinnamon
TB (or PTB)
What should be taken note of for the general impression of the initial assessment?
Position
Color
Mental status
Ability to speak
Respiratory effort
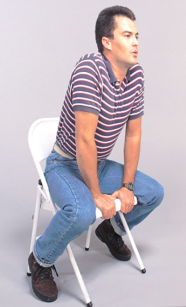
The patient being in this position can be a sign of respiratory distress as it facilitates better exchange of O2.
Tripod position
The lack of oxygen can lead to this mental state.
Alteration of mental status
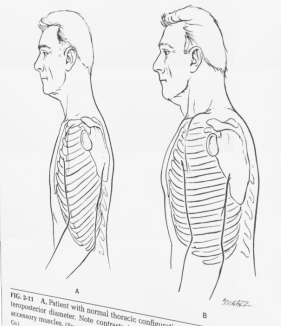
When inspecting the thoracic contour, the chest will not be absolutely symmetric. Which is bigger, the AP or the transverse diameter and by how much?
Follow Up Question: Does this increase or decrease with age?
AP < transverse diameter (>0.70-0.75)
Patients with chronic asthma, emphysema, or CF presents with this.
Barrel chest
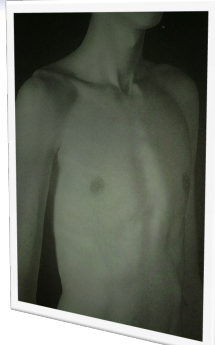
This is a common congenital chest wall deformity where the breastbone (sternum) and ribs grow inward, creating a sunken or "funnel chest" appearance.
Pectus excavatum

This is a chest wall deformity where the breastbone (sternum) and ribs protrude outward, creating a bird-like or bowed appearance.
Pectus carinatum
This is an abnormal, excessive outward curvature of the thoracic spine (upper back), resulting in a hunched or slouching posture.
Kyphosis
This is an abnormal sideways curvature of the spine, often appearing as an S or C shape.
Scoliosis
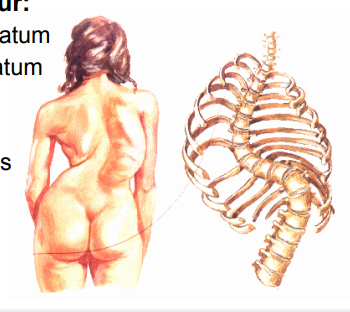
This is a complex, combined spinal deformity characterized by abnormal, concurrent curvature of the spine in both the sagittal and coronal planes, often with vertebral rotation.
Kyphoscoliosis

Chest asymmetry may occur due to unequal expansion and respiratory compromised secondary to what?
Follow Up Question: What can lead to this unequal expansion and respiratory compromise?
A collapsed lung or limitation of expansion.
Extrapleural air, fluid, or mass
This sign upon inspection suggests an obstruction to inspiration at any point in the respiratory tract. It occurs dye to intrapleural pressure becoming increasingly negative and its degree and level depend on the extent and level of the obstruction.
Retractions

What are the signs of upper airway obstruction?
inspiratory stridor (expiratory is severe)
hoarse cough or cry or barking cough
alar flaring
retraction at the suprasternal notch
cyanosis
What are the signs of a supraglottic obstruction?
stridor tends to be quieter
muffling voice (“hot potato in mouth”)
dysphagia
no cough
awkward position of head and neck to preserve the airway
drooling (since both the trachea and esophagus are blocked)
What are the signs of infraglottic obstruction?
stridor tends to be louder, rasping
hoarse voice
swallowing not affected
cough is harsh, barking
head positioning is not a factor