Resp 5 - Ventilation-Perfusion Relationship, Hb, Dissociation curve
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
Speed of gas diffusion in blood
Fast
Where does P02 of capillaries increase the most?
The first thrid of the capillary length
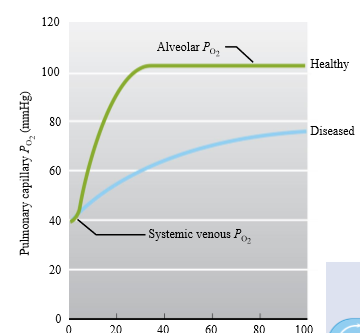
Use of PO2 increasing increasing in first third of capillary
In disease process, diffuison can continue for an extra length of time
What determines arterial levels of gases
Partial alveoli pressure of gas
Why is the pulmonary circulation low pressure
Respiratory membrane is extremely fragile
Effect of hypertension on respiratory membrane
Damages membrane, causing edema and influx of plasma/RBCs that
Why is the pulmonary circulatory system a low resistance systen
Radius of vessels is shorter and wider
R = 8nl/pir^4
Pulmonary circulation has high compliance vessels: what is the use?
- high number of arterioles with low resting tone
- Thin walls and paucity of smooth muscle can accept large amounts of blood
- Can dilate in response to modest increases in arterial pressure
What happens if alveoli capillaries are collapsible
If capillary pressure falls below alveolar pressure, the capillaries close off, diverting blood to other pulmonary capillary beds with higher pressures
Capillary system in lungs
Crates strong network within alveolar structures and that has the advantage of having a large respiratory membrane (large SA for exchange)
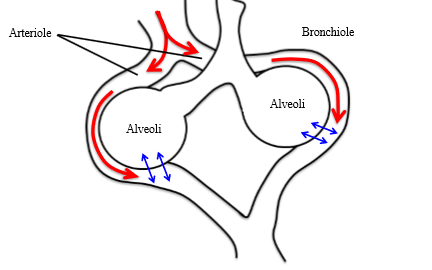
Ventilation perfusion
Inspired air has to be delivered to regions of the lung where the blood is going and vice versa
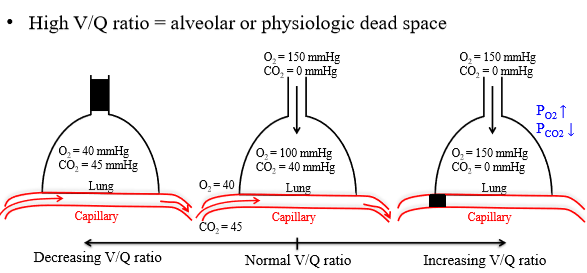
Ventilation/perfusion (V/q) ratio
Balance between the ventilation (brining O2 in/removing Co2 from alveoli) and perfusion (removing O2 from alveoli and adding CO2)
Role of the ventilation and perfusion ratio
Major factors that effect alveolar (and therefore arterial) levels of O2 and CO2
The greater the ventilation...
There is a large amount of air per unit time that enters the alveoli, which makes alveolar PO2 and PCO2 approach their respective atmospheric pressure
The greater perfusion...
the more closely the composition of local alveolar air will approach that of mixed-venous blood
Ventilation
Bringing O2 in, removing Co2 from alveoli
Perfusion
Removing O2 from alveoli and adding CO2
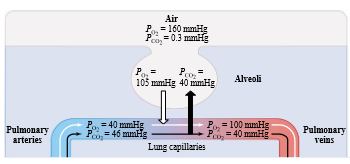
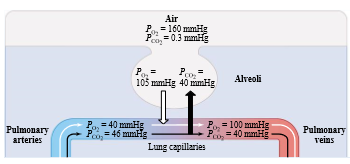
Optimal ventilation/perfusion ratios
PO2 - 100-105 mmHg
PCO2 - 40 mmhG
How to increase ventilation/perfusion ratio
Must be increase in ventilation, or decrease in diffusion
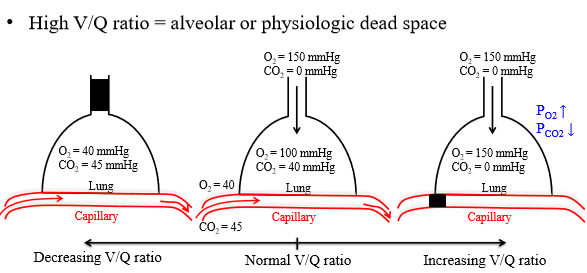
Where is a high ventilation/perfusion ratio seen
Collapsing of the lung capillaries, pleurisy, or other diseases
Also seen with alveolar or physiologic dead spaces
What causes an increased V/P ratio in alveoli
Alveoli are normally ventilated but there is very little gas exchange that occurs because no gas exchange occurs. Usually a pathological condition. Region is overventilated or under perfused
How does a alveolar dead space cause a increased V/P ratio
PO2 is increased because no O2 is passed to the lungs
PCO2 is decreased because no CO2 is delivered and diffuses from the capillary system to the alveoli
Anatomical dead volume
Conductive zone
What causes a low V/P ratio
Air way obstruction (collapsed bronchi or bronchioles)
How does an airway obstruction cause a low V/P ratio
no gas exchange between alveolar air and atmosphere. Causes decrease in PO2 and increase in PCO2
Airway obstruction shunt
Amount of blood that passes through airway obstruction - venous blood is not oxygenated and not available for gas exchange because of alveolar occlusion
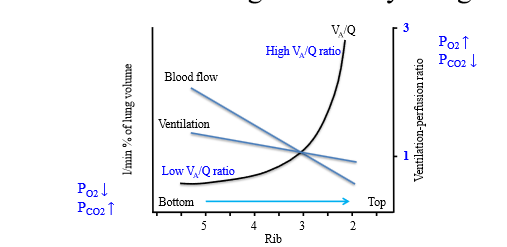
Regional differences in lung perfusion and ventilation
There are regional differences in perfusion and lung ventilation - local ratio determines local alveolar PO2 and PC02
What causes regional diffeeences in lung perfusion and ventilarion
- Weight of lungs: increases pressure in bottom regions (makes interpleural pressure less negative, causing deflated alveoli)
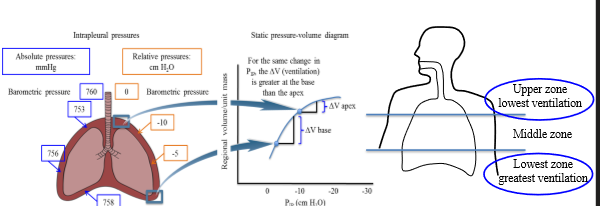
Where does perfusion occur in an upright person
At the bottom of the lungs - weight increases pressure = deflated alveoli = can expand more
How to test changes in lung perfusion
§ injecting a patient with radioactive xenon
o Patient holds breath as soon as the radioactive material is injected to measure radioactivity in the different regions of the lung
Changing position effects lung ventilation AND perfusion
Is the ventilation-perfusion relationship in healthy lungs uniform?
No. Blood flow and alveolar ventilation are reduced in the apical lung compared to the basal
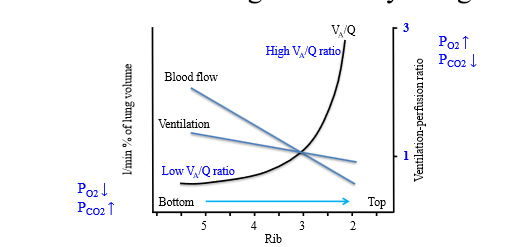
What causes the non-uniform relationship of ventilation-perfusion
Basal Ventilation-Perfusion is 0.6X the ideal
- Decreased PO2 level and increased PCO2 level compared to ideal
Apical Ventilation-Perfusion is 3X the ideal
- Increased PO2 level and decreased PCO2 level compared to ideal
Ventilation perfusion matching
Respiratory system can maintain appropriate ventilation and perfusion in different lung regions - allows for elimination of mismatch of ventilation and perfusion
What mechanisms limit the ventilation perfusion mismatch
Hemostatic mechanisms - mostly pulmonary capillaries response to low O2
Pulmonary hypoxic vasoconstriction
-blood is shunted to areas with better ventilation
-minimization of V/Q mismatch
How is ventilation and perfusion matched in a bronchoconsreiction
Bronchoconstriction makes diameter of airway smaller, leading to less ventilation (increasing alveolar PCO2, and lowering O2)
- Reduction in PO2 causes vasoconstriction of arterioles - reduces ventilation in response of reduced perfusion
- Blood is diverted to regions where ventilation is effective
How does the circulatory system react to decreased airflow to lung
1. Decreased airflow to a region of the lung
2. decreased alveolar pressure and decreased PO2
3. decreased partial pressure for oxygen at the level of the alveoli will influence the pulmonary blood PO2
4. decrease PO2 at the level of the arterial blood
5. vasoconstriction of the pulmonary vessels
6. vasoconstriction of the pulmonary vessels will decrease blood flow (local perfusion decreased to match a local decrease in ventilation)
7. blood will be diverted to regions where ventilation is improved or is still effective
local adaptive effect to this decreased airflow to a region of the lungs is to decrease blood flow
How does the respiratory system respond to decreased airflow to the lung
1. Decreased blood flow to region of the lung →
2. increase alveolar PO2 and decrease alveolar PCO2
3. bronchoconstriction
4. less air moves into the region that has decreased blood flow (local ventilation decreased to match local decrease in perfusion)
5. diversion of blood flow from a region that has low ventilation to a region that has high ventilation to match a local decrease in perfusion
2 ways oxygen is carried in the lungs
1. Dissolved (2%)
2. Combined with hemoglobin (98%)
Why is oxygen present in such low amounts in plasma compared to hemoglobin
Low solubility. The oxygen ends up diffusing into RBCs in the pulmoary capillaries
Dissolved O2 follows Henry's law - what does this mean?
O2 content is proportional to PO2 solubility
Composition of hemoglobin
Protein composed of 4 globin subunits (2 alpha, 2 beta) and 4 hemegroups
Structure of Heme group
Porphyrin ring structure containing ferrous iron for O2 to bind
How many oxygen molecules can bind to one hemoglobin
4. As there is 4 heme units
Deoxyhemoglobin
Hemoglobin without oxygen
What causes interaction between Oxygen and hemoglobin (O2 binding to Hb)
PO2
Oxygen dissociatation curve
Interaction between hemoglobin and arterial partial pressure of oxygen. Y axis is Hb saturaiton, X is PO2
Significance of 100 mmHg PO2 on dissociation curve
Value of PO2 in the blood when it exits the lung capillaries after gas exchange occurs. Hb saturation is 100% (systemic arterial)
Significance of 40 mmHg PO2 on dissociation curve
PO2 level in peripheral tissue where Hb saturation is 75%. (systemic venous) 40 mmHg and 100mmHg is the pressures where the amount of O2 unloaded in tissue capillaries
Physiological pressures of O2 at rest
between 40-100
When blood moves back into the venous system, what percentage of blood is oxygenated
70%
Oxygen capacity
The max amount of oxygen that can combine with hemoglobin
What factors effect oxygen capacity
- How much hemoglobin is in the blood
Hemoglobin saturation
Percentage of available hemoglobin binding sites that have O2 attached
= O2 combined with Hb/O2 capacity x 100
Does hemoglobin saturation tell us about oxygen capacity
No
At the level of the arterial blood where PO2 is 100 mmHg, hemoglobin saturation is about...
97.5%
At the level of the mixed venous blood were PO2 is about 40 mmHg, hemoglobin saturation is about
75%
What determines Hb saturation
PO2 (most important)
PCO2
Temperature
Why is the Hb dissociation curve sigmoidal
cooperative binding of hemoglobin
What is cooperative binding
When O2 binds to Heme, deforms the shape of associated globin chains from tense (T) to relaxed state. When one globin chain deforms, the other do and can bind with O2
Important features of the sigmoidal dissociaiton curve
Plateau between 60-100 mmHg
Steep portion between 10-60 mmHg
What causes Dissociation curve plateau
Caused by reduced alveolar PO2 (therefore arteriolar PO2)
Use dissociation curve plateau
Provides safety factor so that even a significant limitation of lung function still allows almost normal O2 saturation of Hb
- o Makes sure that the majority of the hemoglobin is bound to oxygen despite the fact that there are small changes in arterial PO2
2 regions of steep portion of dissociation curve
40-60 mmHg and 10-40 mmHg
Steep portion of dissociaiton curve (40-60 mmHg)
Unload large amounts of O2 with small decrease in PO2
Even at 40 mmHg pO2, Hemoglobin saturation is still 75%. Why
PO2 must be high in peripheral tissue capillary as this pressure drives diffusion of O2 from RBC to blood to cells and mitochondria
Since PO2 in peripehral tissue is on the steep portion of the curve, what is the effect of pH and temp?
pH and temperature enhance O2 unloading
Where is the steepest portion of the dissociaiton curve?
Between 1040 mmHg
In what situations would P02 go below 40 mmHg?
- High metabolic rate when peripheral tissues use O2
Effect of metabolic rate on tissue PO2
oncreases in metabolic rate cause further decrease in tissue PO2, which facilitates diffusion from plasma which leads to drop in plasma PO2, diffusion of O2 from RBC, drop in PO2 in RBC, additional dissociation of O2 from Hb
Thus excreting muscle can extract much more O2 from blood compared to resting conditions
Use of PO2 increasing increasing in first third of capillary