BH E1- Mood disorders
1/174
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
175 Terms
What classifies all mental disorders, specifying diagnostic criteria and describing manifestations of the disorder but rarely explains the causes or origins?
DSM (5-TR is current version)
What is a syndrome characterized by clinically significant disturbance in cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning?
Mental disorder
Does a culturally approved / expectable response to a common stressor or loss (ie death of a loved one) count as a mental disorder?
No
What are the 3 domains of mental health indicators?
Emotional well being, psychological well being, social well being
Does the DSM include treatment options or theoretical concepts of mental disorders?
No - purely a diagnostic tool
What is the 2nd leading cause of death in youth and young adults?
Suicide
What mental disorder is most associated with people who have attempted suicide?
MDD
What are half of suicide attempts related to?
Firearms
What are the risk factors for suicide?
Sex (F more likely to attempt, M more likely to commit)
Age (bimodal- teens & elderly)
Depression
Previous attempt!
Etoh abuse
Rational thinking loss
Social support lacking
Organized plan
No spouse
Sickness / chronic illness
What is considered a protective factor against suicide?
Having responsibility to others (ie spouse)
What scale assesses suicide risk?
Columbia suicide severity rating scale (C-SSRS)
What 3 criteria must be met to have a patient involuntarily committed (IVC) / backer act?
-Presence of mental illness
-Refused voluntary examination OR unable to consent to exam
-Poses risk to self or others w/o tx AND it is not apparent that such harm may be avoided through help of other services
What rule governs the duty to warn individuals who are being threatened & use reasonable care to protect intended victim against such danger?
Tarasoff rule
What is a period of time when a patient feels abnormally happy or sad (ie major depressive, manic, hypomanic)?
Mood episode
The following diagnostic criteria is for what condition?
≥5 sx from SIGECAPS must be present during 2 week period, and atleast 1 must be depressed mood or anhedonia
sx cause impairment in functioning & not caused by other condition
Major depressive episode (MDE)
What is anhedonia?
loss of interest/pleasure
What are the symptoms in the SIGECAPS mnemonic for major depressive epidoses (MDE)?
Sleep disturbances
Interest lost (Anhedonia)
Guilt / worthlessness
Energy dec (Fatigue)
Concentration issues
Appetite disturbances
Psychomotor changes
Suicidal ideation (SI)
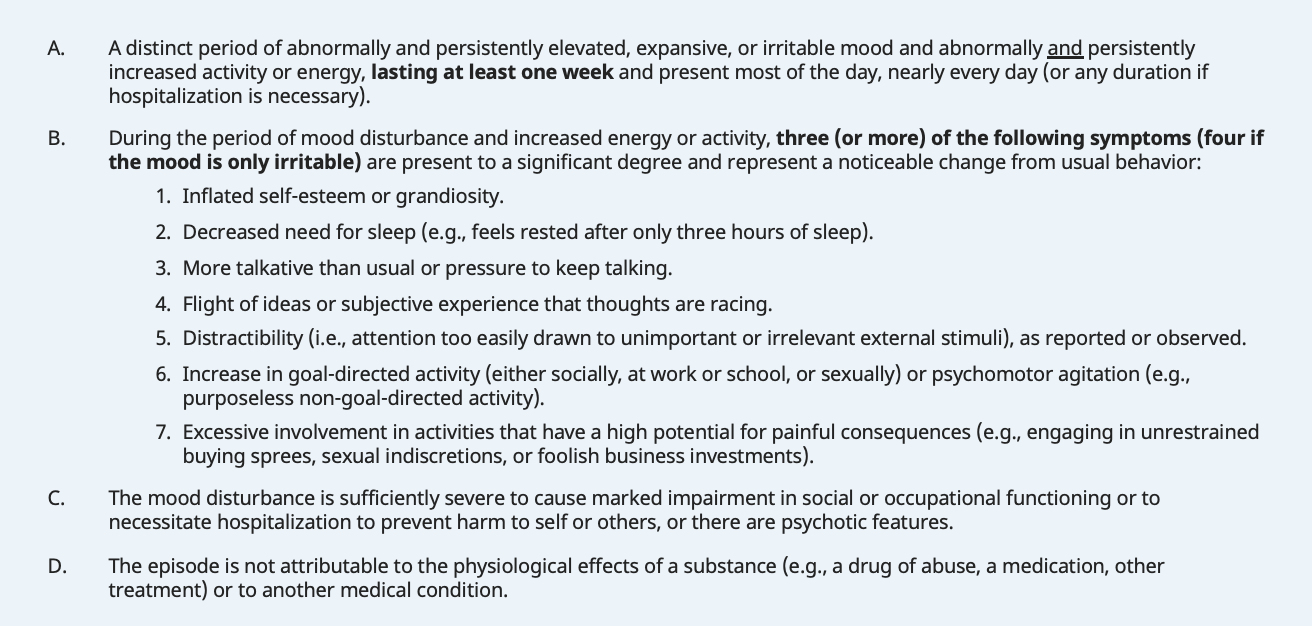
The following DSM5 criteria is for what condition?
abnormally & persistent elevated or irritably mood & inc energy, lasting atleast 1 week and present most of the day nearly every day
≥3 sx (or ≥4 if mood is only irritable)
distractibility
dec need for sleep
inc self esteem, grandiosity
flight of ideas / racing thoughts
inc goal directed activity or psychomotor agitation
activities w/ high potential for painful consequences
marked impairment in functioning or necessitates hospitalization, or psychotic features are present
not caused by other condition / substance
Manic episode
The following criteria is for what condition?
feelings of persistent irritability & elation
≥3 DIGFAST sx for atleast 4 days
distractibility
insomnia
grandiosity
flight of ideas
inc activity
speech
thoughtlessness
*does not cause significant impairment, hospitalization, or psychosis
Hypomanic episode
What mnemonic for symptoms of a manic/hypomanic episode?
Distractibility
Insomnia (dec need for sleep)
Grandiosity (inc self esteem)
Flight of ideas/racing thoughts
Activity / energy increased or psychomotor agitation
Speech (pressured or talkative)
Thoughtlessness (risky behavior)
Manic or Hypomanic episode?
lasts at least 7 days
causes severe impairment socially or occupationally
may warrant hospitalization/baker act to prevent harm to self or others
psychotic features
Manic episode
Manic or hypomanic episode?
lasts atleast 4 days
no marked impairment
does NOT require hospitlization
NO psychotic features
Hypomanic episode
What is the DSM-5 criteria for major depressive disorder (MDD)?
≥1 MDE (SIGECAPS) + NO history of mania/hypomania
What are key features of MDD?
Sadness, irritability, suicidal ideation (SI)
Who is MDD more common in?
F > M, peaks ~20 y/o; sudden or gradual onset
In what MDD patients would mortality be increased?
Comorbidities (DM, stroke, CV dz)
The following etiology is for what condition?
dec NE, 5HT, DA
abnormal B receptor regulation
thyroid disorders, dysregulation of brain pathology
fhx 1st degree relative (2-4x inc risk)
disturbance in infant/mother relationship (freud)
poor stability of family structure & social functiong
MDD
How often should primary care screen adults for depression?
annually (more often if risk factors)
How often should primary care screen a patient for depression with chronic controlled HTN on a BB?
screen every visit
How long can untreated MDD episodes last?
6-13 mos
What clinical signs are present with MDD?
Sleep complaints, appetite changes, energy/fatigue complaints, GI complaints, physical pain (ex- HAs)
When would you hospitalize a patient w/ MDD?
SI, HI, unable to care for self
What is the preferred treatment for MDD?
Combo pharmacotherapy + psychotherapy
What type of therapy often includes education, relaxation exercises, coping skills training, stress management or assertiveness training?
Cognitive behavioral therapy (CBT)
What kind of therapy focuses on individuals interpersonal life in 4 problem areas- grief over loss, interpersonal disputes, role transitions, and interpersonal skill deficits?
Interpersonal therapy (IPT)
What type of psychotherapy?
develops self insight by exploring how past experiences influence current behaviors, emotions & relationships
uncover unconscious patterns in interpersonal relationships, conflicts & desires
methods to enhance self awareness
Psychodynamic psychotherapy
What type of psychotherapy helps individuals cope & deal with illness, crisis or transient problem as well as maintain optimism and hope (offers guidance, advice, praise, etc)?
Supportive therapy
What type of psychotherapy attempts to correct distorted communications & impaired relationships by helping partner/entire family as well as the patient?
Family and couples therapy
What type of psychotherapy offers supportive networks for people who have similar difficulties?
Group therapy
What type of psychotherapy tackles specific life problems that contribute to emotional distress?
Problem solving therapy
What is integrated care?
Availability of mental health specialty care in context of primary care
What is the general approach to treatment in MDD?
Try 2 SSRIs & 1 SNRI first (only 1 at a time) for 3-4 weeks minimum
If first SSRI fails → switch to another SSRI → if fails again, try SNRI
What qualifies as treatment resistant depression (TRD)?
2-3 medication failures
What are treatment options for treatment resistant depression (TRD)?
augment w/ SGA (ex abilify), esp if psychotic features
augment with Wellbutrin or mood stabilizer (Lithium if SI)
TMS, esketamine, ECT
How long can it take for antidepressants to work?
3-4 weeks
What SSRIs are used for MDD?
Citalopram (Celexa)
Escitalopram (Lexapro)
Paroxetine (Paxil)
Sertraline (Zoloft)
Fluoxetine (Prozac)
What SNRIs are used for MDD?
Venlafaxine (Effexor), Duloxetine (Cymbalta)
What anti-psychotics that can be used as adjunct in MDD treatment?
Quetiapine (Seroquel)
Lurasidone (Latuda)
Olanzapine/fluoxetine (Symbyax)
What MAOI can be used to treat MDD?
Phenelzine
What is the first line treatment for MDD?
SSRIs >> SNRIs
What SEs are seen with SSRIs?
HA, GI disturbance, sexual dysfunction, rebound anxiety
*safer & generally better tolerated
What is the 2nd line treatment for MDD?
TCAs: Amitriptyline, Clomipramine, Nortriptyline
What SEs are seen with TCAs?
Sedation, orthostatic hypotension, anti-cholinergic SEs, long QT syndrome
lethal in overdose
What SEs are seen with anti-psychotics?
EPS (dystonia, akathisia), Tardive dyskinesia (involuntary movements)
What are indictions for ECT treatment in MDD?
Non responding, non tolerating to anti-depressants (pregnancy)
Rapid recovery required
Can use in conjunction with rx or alone; ~ 8 tx over 2-3 wks
What is the process of ECT?
premedicate w/ atropine, general anesthesia, muscle relaxants, & induce generalized seizure
What is a possible SE of electro-convulsive therapy (ECT)?
Temporary retrograde amnesia ~6 mos
What is the diagnostic triad for serotonin syndrome?
Autonomic instability, hyperthermia, seizures
What is the diagnostic criteria for Dysthymia (persistent depressive disorder)?
Depressed mood ≥2 years + never asymptomatic for >2 mos + no manic/hypomanic sx + ≥ 2 CHASES sx
The following DSM5 criteria is for what condition?
depressed mood for atleast 2 years (1 yr in kids)
≥ 2 of the following (CHASES)
poor concentration/focus, hopelessness, appetite changes, sleep changes, fatigue/low energy, low self esteem
*criteria for MDD continuously present for 2 yrs
Dysthymia / Persistent depressive disorder
What are the CHASES symptoms associated with Dysthymia?
Concentration decreased
Hopelessness
Appetite change
Sleep change
Energy decreased
Self esteem decreased
Who is dysthymia / persistent depressive disorder MC in?
F > M, onset before mid 20s, insidious onset & chronic course
What treatment regimen provides the best results / most efficacious for dysthymia?
Pharmacotherapy + psychotherapy
What is the treatment for dysthymia?
1st line: SSRI / SNRI
2nd line: MAOI, TCA
+CBT, IPT, insight oriented psychotherapy
What tools can be used for screening/assessment of MDD & Dysthymia?
MMSE, HAM-D, PHQ-9
What assessment tool administered by a clinician monitors progress of depressive disorders by serially measuring severity of symptoms (detailed & time consuming)?
Hamilton rating scale for depression (HAM-D)
What are setbacks to the PHQ-9 depression questionnaire?
illiteracy, physical impairment, impaired cognitive functioning
What is the PHQ-9 depression quesitonnaire?
self report measurement, monitors response tx, not accurate enough to definitively dx
What labs should be considered when evaluating depressive disorders?
CBC, CMP, U/A, HCG, TSH, EKG, urine toxicology, vit B12, folate
What is the etiology associated with PPD?
Genetics, dec estrogen & progesterone, TSH
What are risk factors for depression w/ peripartum onset (postpartum depression)?
Hx perinatal or nonperinatal depression, stressful life events, poor social/financial support, Fhx PPD/psychiatric illness, <25 y/o, & multiparity
“Baby blues” or postpartum depression?
MC
3-5 days after delivery, lasts days-weeks
some sleep disturbance
rare thoughts of harming baby
absent/rare feelings of guilt
no associated stressors, hx mood disorder, SI
Baby blues
“Baby blues” or postpartum depression?
3-6 mos after delivery, lasts months-years (untx)
assoc w/ stressors & hx mood disorder
sleep disturbances always present
SI, feelings of guilt & inadequacy
persistent thoughts of harming baby
Postpartum depression
What are reflags for postpartum depression?
anxiety about baby’s health / ability to care for baby, negative perception of infant temper/behavior, lack of interest in infant, lack of response to support/reassurance, alcohol / drug use
What is the first line treatment for postpartum depression in breast feeding patients?
Paroxetine (Paxil) or Sertraline (Zoloft)
*secretes less into breast milk than other SSRIs
What can also be used for treatment of postpartum depression with severe anxiety or agitation?
Low doses of Lorazepam
What benzodiazepines should be AVOIDED in PPD breastfeeding patients?
Clonazepam, Diazepam
What is another treatment option for refractory / psychotic postpartum depression (PPD)?
ECT
What condition is a severe form of PMS that can onset anytime after menarche, worsens prior to menopause, & stops after menopause?
Premenstrual dysphoric disorder (PMDD)
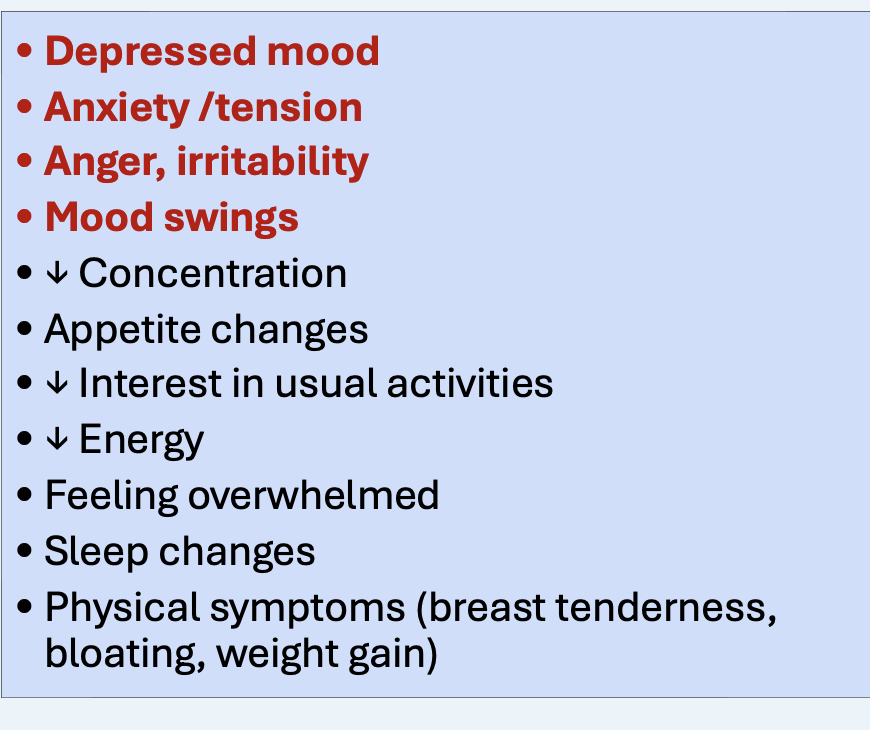
The following DSM5 criteria is associated with what condition?
≥5 sx must be present with at least 1 being from the first 4 (depressed mood, anxiety/tension, anger/irritability, mood swings)
PMDD
How do the symptoms occur in PMDD?
Sx present in final week before menses (last week of luteal phase; progesterone peaks)
Sx must improve w/in a few days after menses & are absent the week after menstruatrion
Confirmed by DRSP for at least 2 cycles
What is the first line treatment for PMDD?
SSRIs- Fluoxetine, Sertraline, Citalopram
Daily or luteal phase only treatment (start on day 14 of cycle and stop on menses onset)
What are other treatment options for PMDD?
OCPs, GNRH agonists, B/L oophorectomy w/ hysterectomy (severe)
Most psychiatric medications improve symptoms but are not disease modifying EXCEPT for which meds?
Lithium & mood stabilizers for bipolar disorder
Which SSRIs are the safest in pregnancy?
Sertraline and fluoxetine
Which SSRI has the lowest passage into breast milk?
Sertraline (Zoloft)
What is the most effective starting dose for Escitalopram (Lexapro)?
10 mg
What drug?
MDD (12+ y/o), GAD
avoid in OCD due to risk of long QT at high doses
Escitalopram (Zoloft)
What conditions can Sertraline (Zoloft) be used in?
MDD, OCD (6+ y/o), PMDD, panic disorder, PTSD, SAD
What SSRI is the most energizing and has the longest half-life & therefore lowest risk of withdrawal?
Fluoxetine (Prozac)
Which SSRI is the most antihistaminic (sedation & weight gain) and is pregnancy category D?
Paroxetine (Paxil)
What drug?
inhibits its own metabolism (titrate slowly)
potent CYP2D6 inhibitor
MDD, OCD, SAD, PTSD, GAD, PMDD, vasomotor sx, Panic disorder
Paroxetine (Paxil)
What drug?
potent inhibitor of CYP1A2
substrates: caffeine, xanax, rozerem
tx OCD (8+ y/o), SAD, MDD
Fluvoxamine (Luvox)
What drug?
newer SSRI and 5-HT1A receptor partial agonist
Vilazodone (Viibryd)
What drug?
NOT an SSRI, multimodal serotonin modulator
lower risk of sexual SEs compared to SSRIs
pro cognitive- can improve attention and memory
Vortioxetine (Trintellix)
What is the MOA of Vortioxetine (Trintellix)?
inhibit serotonin reuptake and interact with/ multiple receptors (5-HTA1 agonist, 5-HT3 anatag)
*not an SSRI
What drug?
NDRI- inc NE and DA levels
less sexual SEs than SSRIs
tx MDD, smoking cessation, & off label use in ADHD
relatively safer in bipolar disorder
Wellbutrin (Bupropion)
What are CIs to Wellbutrin?
Hx of seizures or active anorexia/bulima (seizure risk)
*also monitor BP/HR at high doses (≥300mg)
What drug?
SNRI- potent inhibitor of 5HT & NE reuptake
5HT >> NE
less sexual SEs than SNRIs,
HTN/tachycardia at doses ≥225 mg, discontinuation syndrome (short half life)
tx MDD, GAD, SAD, Panic disorder, off lane for OCD
Venlafaxine
What SNRI is notorious for discontinuation syndrome due to a short half life & needs to be tapered off slowly?
Venlafaxine (Effexor)