Week 1: TRAUMATIC BRAIN INJURY: PATHOPHYSIOLOGY AND SEQUELAE
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
Traumatic Brain Injury
• "An alteration in brain function, or other evidence of brain pathology, caused by an external force"
• Frequently will see multi-system involvement and secondary impairments
Characteristics of the TBI PT:
What can come from having a TBI?
Competent in a wide variety of examination and intervention techniques (bc of the multisystem involvement)
- falls and accidents
- orthopedic causes
- could have a fx
• Strong communication and interpersonal skills
• React quickly and effectively to sudden changes (medical/emotional)
• Strong observation skills
TRAUMATIC BRAIN INJURY: PREVALENCE
• Leading cause of injury-related death and disability in the US
• Greatest risk: >75 yrs, 0-4 months, 14- 24 years
TRAUMATIC BRAIN INJURY: CAUSES
List 3 and age ranges
• Falls→ #1 cause; most common in what population? Over 75y/o
• Being struck by/against something
• MVAs→ most common in what population? 14-24y/o
TRAUMATIC BRAIN INJURY: IMPACT
Statistics
Long term consequences?
1 in 5 who require inpatient rehab will die in 5 years
• If survive, 50% will be readmitted to the hospital at least once
25-33% will require assistance for ADLs
LONG TERM consequences are high
• Direct medical costs
• Injury related disability
• Loss of work (these ppl will struggle w cognitive related tasks)
MECHANISM OF INJURY AND PATHOPHYSIOLOGY OF TBI
• Primary Injury
Occurs due to brain tissue coming into contact with an object OR rapid acceleration/deceleration of the brain leading to cortical disruption
There are primary and secondary injuries when someone suffers a TBI
MECHANISM OF INJURY AND PATHOPHYSIOLOGY OF TBI
• Primary Injury
- Contact Injuries
Contact Injuries
• FOCAL in nature and result in contusions, lacerations, intracerebral hematomas
Brain comes into contact with an object (skull, bullet, shrapnel)
MECHANISM OF INJURY AND PATHOPHYSIOLOGY OF TBI
• Primary Injury
Acceleration/Deceleration Injuries
• Shear, tensile, and compressive forces leading to diffuse/traumatic axonal injury (DAI), tissue tearing, and intracerebral hemorrhages
Rapid mvmt of the brain that leads to cortical disruption of the mem
MECHANISM OF INJURY: DAI - Diffuse/traumatic Axonal Injury
What is it?
What are different areas this injury can affect?
• Predominate MOI for moderate to severe TBI
• Common in high-speed MVAs, some sports injuries
• Frequently occurs in discrete areas (distinct area like... ->) - internal capsule, corpus collosum, cerebrum peduncle, brain stem
• Microscopic→ often hard to find on initial imaging
Wallerian-type axonal degeneration
= disruption of nuerofilaments in the axon (retrograde degeneration leading to cell death)
type of DAI
MECHANISM OF INJURY AND PATHOPHYSIOLOGY OF TBI: Blast Injury - type of primary injury
This is a type of primary injury, list how it can be secondary and tertiary.
Occurs when an explosive detonates
- transient shock waves cause brain damage
Primary
• Direct effect of blast overpressure on organs (brain) - this person is close to the shock waves
Secondary
• Penetration of shrapnel or other objects - penetrating the brain
Tertiary
• Individual is forcibly moved and strikes an object - wall or something and head is hit
Can cause mild mod or severe TBI
MECHANISM OF INJURY AND PATHOPHYSIOLOGY OF TBI: Secondary Injury
How does it occur?
How does it develop?
Occurs due to the primary injury that causes things in the body
Can develop over hours and can continue for days→ cell death
Cellular processes due to tissue damage: these cause cell death
• Glutamate neurotoxicity, influx of Ca/ions, free radicals, cytokines, inflammation
Effects of the primary injury:
What does an elevated ICP lead to
Hypoxemia, hypotension, ischemia, edema, elevated ICP
can lead to herniation - brain structures start to descend = med emergency
- UNCLE - uncus starts to descend
- CENTRAL = diancephalon and temp lobe start to descend
- TONSILLAR = cerebellar tonsils descend thru foramen magnum)
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION
• Neuromuscular Impairments
• Paresis - decr str
• Decreased coordination
• Impaired postural control
• Abnormal tone
• Abnormal gait
• Impaired sensation
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION: Cognitive Impairments
List them (4)
Cognitive Impairments
• VERY common due to frequency of injury to the frontal lobe
Difficulty in (potentially!) MANY areas
• Arousal, attention/concentration
• Memory
• Learning
• Executive function (planning, initiation, inhibition, sequencing, etc)
Disorders of Consciousness
SEQUELAE OF TBI: DISORDERS OF CONSCIOUSNESS
• Coma
List what it looks like
• Arousal system not functioning
• No sleep/wake cycles
• Eyes closed
• Ventilator dependent
• NO visual, auditory, communication or cognitive function
• Not generally permanent
SEQUELAE OF TBI DISORDERS OF CONSCIOUSNESS: Vegetative State (unresponsive wakefulness)
What does it look like?
• Eyes are open, but awareness of environment is absent
• Sleep/wake cycles present
• Generally no ventilator (unless SCI)
• May startle or briefly orient to auditory/visual stimuli
• No meaningful cognitive or communication function
• May see reflexive movements, not purposeful
Can be permanent
SEQUELAE OF TBI DISORDERS OF CONSCIOUSNESS: Vegetative State (unresponsive wakefulness)
When do you know when this can become permanent?
No meaningful motor or cognitive function, no awareness of self or environment at 1 year post TBI
OR
3 months post anoxic injury (bc anoxic = worse / more severe - you end up w global and widespread neuronal death = total oxygen deprivation)
SEQUELAE OF TBI DISORDERS OF CONSCIOUSNESS: Minimally Conscious State
What does it look like
• Some evidence of awareness to self or environment
• Sleep/wake cycles present
• Behaviors are inconsistently repeated or sustained (reaching for objects, visual fixation)
• Can localize to stimuli (turn around when touched on SH), may demo visual fixation
• May reach for objects
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION: Neurobehavioral Impairments
• Low frustration tolerance, irritability
• Agitation, physical/verbal aggression
• Disinhibition, emotional lability (exaggerated response)
• Apathy
• Impulsivity
• Mental inflexibility
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION: Communication Impairments
• Disorganized, tangential
• Poor precision of language, word retrieval
• Disinhibited or socially inappropriate language
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION IMPAIRMENTS
- Dysautonomia— "sympathetic storming" paroxysmal sympathetic hyperactivity
- post traumatic seizure
Dysautonomia— "sympathetic storming" paroxysmal sympathetic hyperactivity
• Increased HR, RR, BP
• Diaphoresis, hyperthermia
• Decerebrate (everything in EXT) or decorticate (UE FLEX, LE EXT) posturing
• Hypertonia
• Teeth grinding
Working in overdrive
Post-Traumatic Seizures
• Very common—up to 50%!
SEQUELAE OF TBI: BODY STRUCTURE/FUNCTION: secondary impairments and medical complications
DVT
Heterotrophic Ossification
Pressure ulcer
Pneumonia
Chronic pain
Contracture
Muscle atrophy
Fracture
Limited endurance
Peripheral nerve damage
Incontinence
High potential of immobility associated w TBI
SEQUELAE OF TBI: ACTIVITY LIMITATIONS
What activities can be affected after experiencing a TBI
Walking
High-level mobility
Eating
Dressing
Bathing
Grooming
SEQUELAE OF TBI: PARTICIPATION RESTRICTIONS
Significant, long-term restrictions
Difficulty (or inability) to return to prior life roles
• Work
• Family
• Community
SEQUELAE OF TBI: LONG-TERM COMPLICATIONS - they are at an incr R for
• Alzheimer's
• Parkinson's
• Frontotemporal dementia
• Chronic traumatic encephalopathy
• Depression
• Anxiety
**TRAUMATIC BRAIN INJURY: DIAGNOSIS, PROGNOSIS, AND CONTINUUM OF CARE**
DIAGNOSIS OF TBI
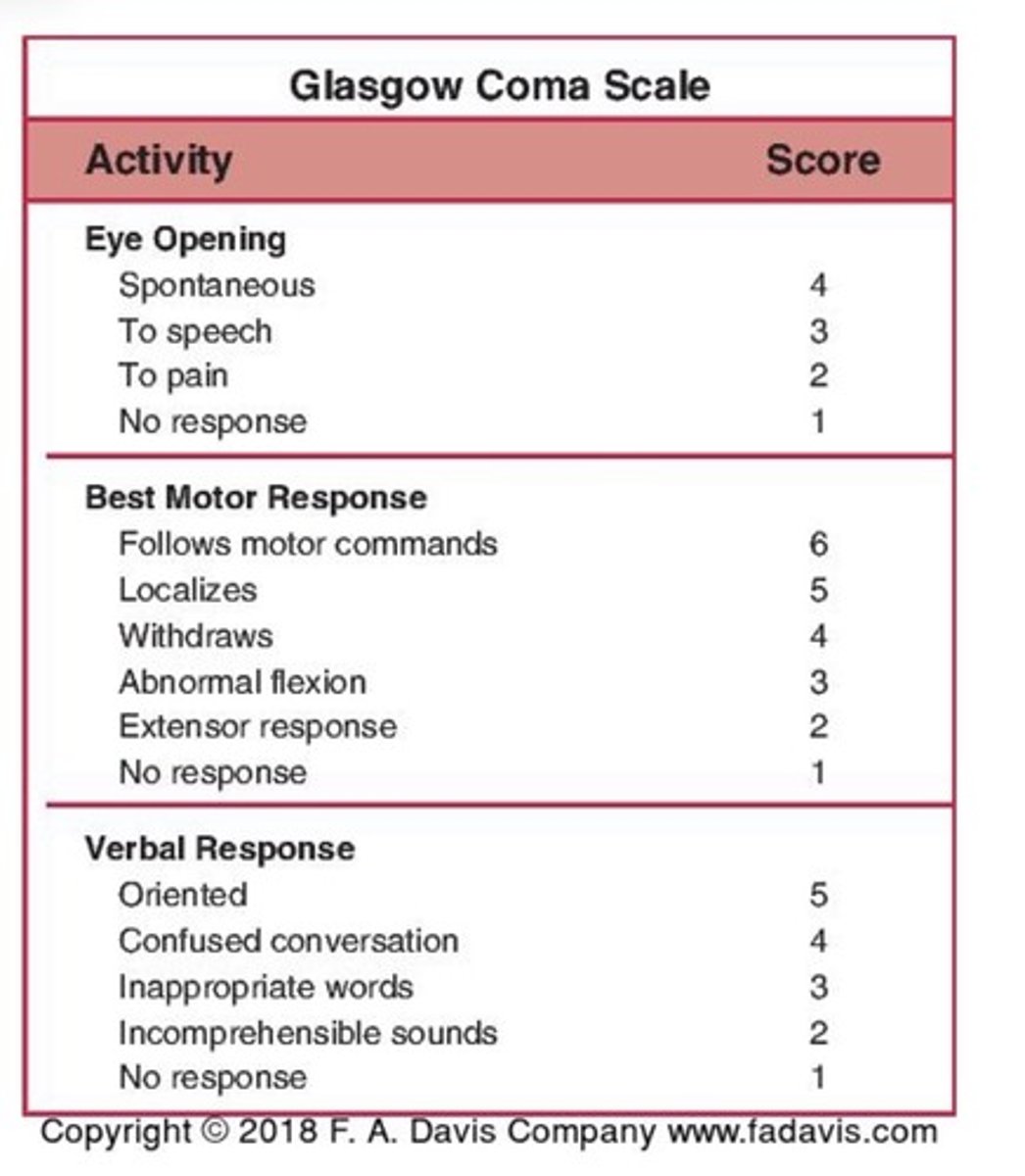
• Glasgow Coma Scale
What is it and provide the classifications
Provides classification of TBI based upon severity
• Utilizes motor responses, verbal responses, and eye opening for classification
Classifications
• Mild: 13-15
• Moderate: 9-12
• Severe:
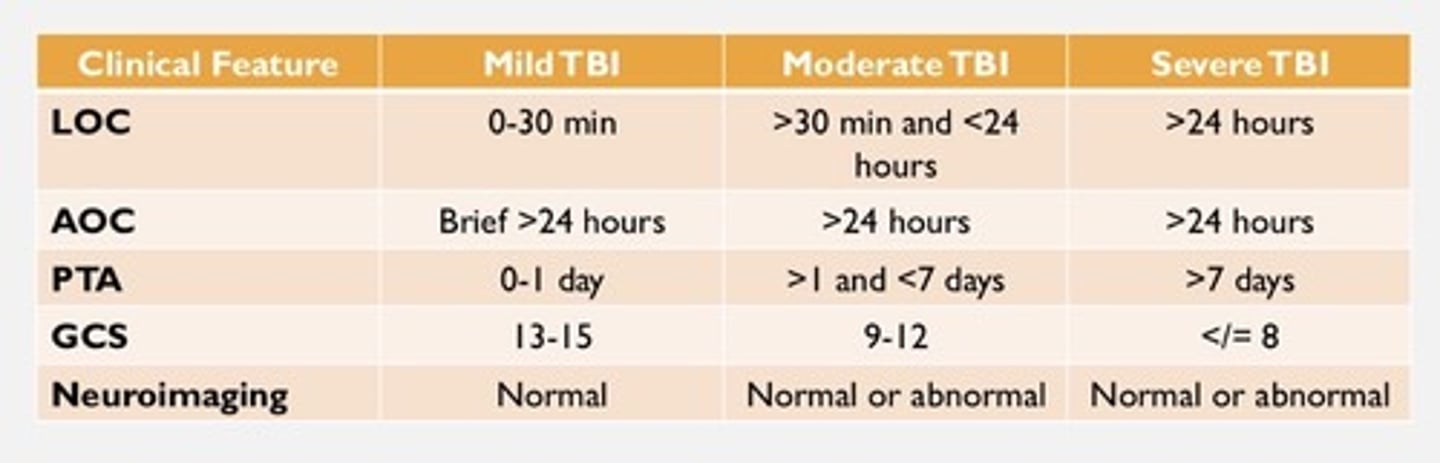
Diagnosis of TBI: Clinical Features
LOC - loss of consciousness
AOC - alteration of consciousness
PTA - post traumatic amnesia
GCS - glascow coma scale
Neuroimaging
Know the chart
PROGNOSIS OF TBI
• Indicators of Poor Recovery
• Low initial GCS scores (pupil reactivity and motor score)
• Age - old age = bad
• Race - non white do worse
• Lower education level
CT findings - peteakeal hemmorage, subarachnoid bleeds, midline shifts, subdural hematoma, obliteration (when you look at them on imaging you no longer see it bc of the incr ICP) of 3rd ven or basal
Systerns
Duration of PTA - the longer some one is in PTA the worse it is
- length of time from the injury to when the pt can remember current events
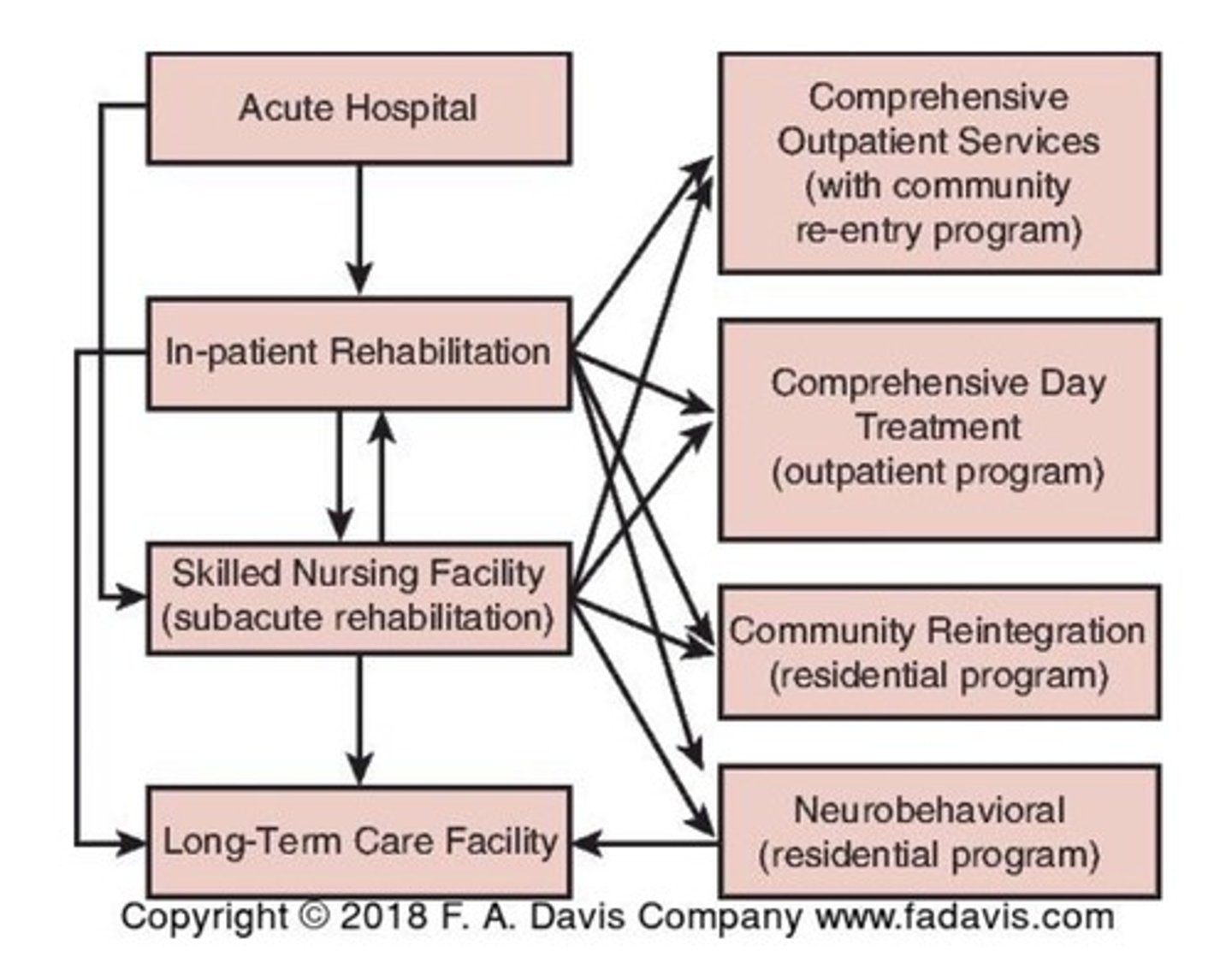
CONTINUUM OF CARE FOR THE INDIVIDUAL WITH TBI
Look at the chart
**RANCHO LOS AMIGOS LEVELS OF COGNITIVE FUNCTIONING**
PURPOSE AND USE
Valid and reliable descriptive scale to examine cognitive and behavioral recovery following brain injury.
• Consists of ten levels (originally 8!)
• Levels are useful for describing and communicating cognitive and behavioral status
• Can be helpful for treatment planning
Helps to describe the pattern of recovery
• Individuals can plateau at any level
KNOW 1-5
Know certain things from the rest
Level 1 - No Response, Total Assistance
Complete absence of observable change in behavior when presented visual, auditory, tactile, proprioceptive, vestibular or painful stimuli
In a coma - no response to any stim
Level 2 - Generalized Response, Total Assistance
Demonstrates generalized responses that inconsistent, not purposeful, and not specific
Responses can be delayed significantly and are often the same regardless of type of stimuli or location of stimuli
Responses may be physiologic, gross body movements, and/or vocalizations
Level 3 - Localized Response: Total Assistance
Responses are specific (related to the stim), but inconsistent
• Response is directly related to the stimuli
• Responds inconsistently to commands
• Responds better to some individuals than others (family/friends)
Demonstrates withdrawal or vocalization to painful stimuli
Examples
• Follows object in visual field
• Responds to discomfort by pulling at lines/tubes
• Turns to/away from auditory stimulus
Level 4 - Confused-Agitated, Maximal Assistance
Most fun and stressful level
State of heightened activity
Demonstrates purposeful attempts to remove lines/tubes, crawl out of bed, get out of a chair, etc.
Often performs motor behaviors without apparent purpose or request
Absent short and long term memory
Difficulty cooperating with treatment
• Aggressive or flight behaviors
• Incoherent and inappropriate verbalizations to the situation
• Significant mood swings without relationship to environmental context
LEVEL 5: CONFUSED, INAPPROPRIATE, NON-AGITATED-MAXIMAL
ASSISTANCE
Alert, but disoriented and highly distractible
May become agitated in response to external stimulation, and/or lack of environmental structure.
Often demonstrates inappropriate use of objects without external direction
Simple command following with structure and cues
• May perform previously learned tasks with structure and cues
• Without structure, responses are random and non-purposeful
Memory/learning
• Very poor recent memory, confusion of past and present
• Unable to learn new information
• Absent goal directed, problem solving, self-monitoring behavior
Communication
• Social, automatic level for brief periods with structure and cues
• Without structure and cues→ inappropriate, confabulatory
Level 6- Confused, appropriate, moderate assistance
Inconsistently oriented to person, time and place
- this starts here
Emerging awareness of appropriate responses to self, family, basic needs BUT unaware of impairments, disabilities, and safety risks
Poor problem solving for task completion→ mod assistance
Communication
• Consistently follows simple directions***
• Appropriate verbal expression in very familiar and structured settings**
Memory(starts to improve)/Attention/Learning (Starting new learning)
• Vague recognition of some staff
• Use memory aid with max assistance
• Remote memory > recent memory
• Attend to highly familiar tasks in non-distracting environment with mod redirection
• Supervision for old learning, but MAX assistance for new learning
• Little to no carryover for new learning, but carryover with familiar, relearned task
Level 7- Automatic, appropriate, minimal assistance for daily living skills
Consistently oriented to person and place, within highly familiar
environments. Moderate assistance for orientation to time***
Communication/Interaction
• Unaware of others' needs/feelings and unable to recognize own inappropriate social behavior
• Oppositional and uncooperative
Memory/Learning/Attention
• Min supervision for new learning (new learning and carry over) and demonstrates carryover of new learning
• Attend to highly familiar tasks in non-distracting environment with min assist to complete tasks***
Safety***
• Overestimates abilities→ min supervision for safety in routine activities
• Unable to think about consequences or realistically plan for future
• Superficial awareness of condition, but unaware of specific impairments and the impact of those impairments
Can carry out familiar personal/household routines but requires min
assistance for accuracy, completeness, or plan modification and
demonstrates limited recall of what he/she has been doing
level 8: purposeful, appropriate - stand-by assistance
Consistently oriented to person, place and time*** 100%
Communication/Interaction
• Depressed, irritable, argumentative, self-centered, poor frustration tolerance, uncharacteristically independent/dependent
• Acknowledges others' needs/feelings and responds appropriately with min assist
• Can recognize and acknowledge inappropriate social behavior and correct with min assist***
Safety
• Over- or underestimates abilities
• Thinks of consequences with min assist***
• Awareness and acknowledgement of impairment impact on function, requires min A to initiate corrective action***
Memory/Attention/Learning
• Independently attends to and completes familiar tasks for 1 hour in distracting environments***
• Uses memory devices with stand-by assistance
• Can recall and integrate past and recent events
• No assistance once new learning has occurred for tasks/activities
Can carry out familiar routines with stand-by assistance and modify if
needed with min assistance**
Level 9: purposeful, appropriate, SBA upon request
Communication/Interaction
• MAY demonstrate depression, ease of irritability, low frustration
tolerance
• Demonstrates social self monitoring with stand-by assistance
• Acknowledges others' needs/feelings and demonstrates appropriate
response with stand-by assistance***
Safety
• Awareness and acknowledgement of impact of impairment on function and initiates corrective action as needed BUT requires stand- by assistance to anticipate problems and take action to avoid***
• Can think of consequences with assistance when requested
• Understands abilities but requires stand-by assistance to adjust to task demands
Memory/Attention/Learning
• Uses memory devices with assistance only when requested
• Can independently shift between tasks and complete them accurately for up to 2 hours***
Can carry out familiar routines independently and unfamiliar tasks
with assistance when requested
Level 10-Purposeful, Appropriate: Modified Independent
Communication/Interaction
• Consistently appropriate social behavior
• Periodic depression MAY occur; irritability and low frustration tolerance only when sick, fatigued, stressed
• Recognizes needs/feelings of others and automatically responds appropriately
Safety***
• Accurately estimates abilities and can adjust to the demand of the task
• Can think of consequences but may require increased time or compensations to select the appropriate choice/action
• Can anticipate the impact of impairment on function and takes action to avoid problems but may require increased time or compensatory strategies
Memory/Attention/Learning
• Can multi-task in all environments but may require rest breaks**
• Can create and maintain memory devices**
Independently carries out familiar and unfamiliar tasks but may require increased time or compensatory strategies
Upon initial evaluation, you note that the patient demonstrates withdrawal to painful stimuli and inconsistently closes their eyes to command. This command following is better when the command comes from the patient's mother.
Lvl 3 localized response total assistance
Tina participated in her ADL routine this morning with OT. She was initially uncooperative, but with some coaxing, was agreeable to get started. She required min A to complete the ADL routine in her hospital room (with the door closed and minimal distractions) that she has been working on for a few weeks now.
7 bc she is carrying out a familiar routine in a non distractable environment
Ashlee has been assigned a 1:1 aide. She is constantly trying to get out of bed and pull out her PEG tube. When she is in her wheelchair, she is constantly attempting to roam the hallways and yells as she moves around the unit in her wheelchair.
4
Sally would like to go to the cafeteria and buy herself an ice cream. She remembers that she has been to the cafeteria before, but can't remember where it is, so she asks for help with directions. She starts to make her way there, but when she gets to the stairs, she realizes she needs to take the steps. (She needs her crutch to do the steps and does not have it with her.) She is not sure what to do, so she asks her therapist for help. Her therapist prompts her of the consequence of attempting the steps without the crutch. Sally determines she better go back to get the crutch before moving forward.
9
Uses mem aid (directions)
Can figure out consequence w assistance
Tom was just brought down to the therapy gym by the rehab aide. He is in his wheelchair waiting his therapist and he is looking all around the gym and keeps grabbing items off a nearby shelf and placing them in his wheelchair. When his therapist arrives, he does not remember her but tells her he thinks they went to high school together. His therapist wants to start the session and asks Tom
to stand up from his wheelchair using a very specific and structured set of cues so that he is successful.
5
Follows simp commands w structures and cues
Inappropriate use of objects
Confused past w present
PROGNOSIS OF TBI
• Length of PTA provides valuable information for prognosis
• PTA <48.5 days:
• PTA <27 days:
• PTA <34 days:
• PTA <53 days:
• PTA <48.5 days: higher FIM scores at D/C from acute rehab
• PTA <27 days: likely to be employed
• PTA <34 days: likely to have good overall recovery
• PTA <53 days: likely to live without assistance
Strong predictor of discharge GG scores
The shorter they are in this the better
INTERPROFESSIONAL CARE OF THE INDIVIDUAL WITH TBI
Patient/Family
Physician (physiatrist or neurologist)
SLP
OT
Rehab Nurse
Case manager/team coordinator
Social Work
Neuropsychologist
Other team members as appropriate-- respiratory therapist, recreational therapist