biochemistry profile practical (liver and pancreas)
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
a biochemistry analysis should always be accompanied by what other test?
a full hematology
what 3 blood characteristics can interfere with the results of a biochemistry analysis?
lipemia, hemolysis, bilirubinemia
to perform a biochemistry analysis, we use a ______ sample.
plasma or serum
if we want to analyze LDH, do we use plasma or serum?
plasma
if we are interested in analysing a patient's GGT or lipase, should we use a sample of plasma or serum to perform the biochemistry analysis?
serum
if we add heparin to the blood sample, will we obtain plasma or serum?
plasma
what is U?
the enzyme unit
it is the unit for the amount of the enzyme that produces a certain amount of activity (the amount that catalyzes the conversion of 1 micromole of substrate per unit), at 25 C and the pH and substrate concenration that yields the maximal substrate conversion rate
what are possible etiologies of primary hepatitis?
virus (adenovirus, FIP)
bacteria (leptospirosis, salmonellosis, septicemia)
parasites (toxoplasmosis, dirofilariosis)
toxins (Pb, aflatoxins, Cu)
what are possible etiologies of secondary hepatitis (primary conditions that can lead to a secondary hepatitis)?
acute pancreatitis
DIC
hemolysis
neoplasms
hypoxia/anoxia
diabetes mellitus
hypoadrenocorticism
corticosteroids/anticonvulsant therapy
why are enzymes in the blood a good measure of liver injury?
because when there is a liver injury, it will lead to either necrosis or increased permeability of the hepatocytic membrane, which results in the release of enzymes from the cytoskeleton to the plasma
what biochemical values do we want to check if we suspect a hepatocellular injury?
ALT (carnivores)
AST (large animals)
SDH (large animals)
GLDH (horses, carnivores)
arginase
what biochemical values do we want to check if we suspect cholestasis?
ALKP
GGT
bilirubin
what are the histological signs of an acute liver injury?
cholestatic hepatocytes
hepatocytic degeneration
kupffer cells with detritus
bile duct proliferation
mononuclear portal inflammation
if there is hepatocytic necrosis, is this an acute or chronic liver injury?
chronic
what is ALT? what does its presence in the blood indicate?
alanine transferase/GPT
it is present in the hepatocytic cytoplasm, in high concentrations. its presence in the blood indicates hepatocellular degeneration (liver damage). however, it is unspecific about the type of liver damage- we cannot distinguish whether it is a primary or secondary hepatopathy or if it is reversible. it can only be measured in carnivores.
the most common reasons of an increased ALT level in a carnivore's plasma are....
acute biliary obstruction
diabetes mellitus
hypoxia
hypoadrenocorticism
what is AST? what is it used to detect?
aspartame aminotransferase/GOT
it is present in the mitochondria of the liver, skeletal muscles, RBCs, and kidneys. it can indicate liver damage, but is NOT specific to the liver. an increase of AST and CK indicates muscle damage, but an increase of just AST indicates sever hepatocytic damage. it is only used in large animals.
if there is an increase of AST and CK, this indicates...
muscle damage
if there is an increase of AST but not CK, this indicates...
liver damage (severe hepatocytic damage)
(only used in large animals)
what is SDH? what does it indicate?
sorbitol dehydrogenase
indicates liver damage (it is liver specific). used in large animals.
is SDH hepatospecific?
yes
is AST hepatospecific?
no, it is also present in the skeletal muscles,RBCs, and kidney.
to distinguish the type of injury:
muscle injury= increase AST and CK
liver injury= increase of only AST
is ALT hepatospecific?
yes
is GLDH hepatospecific?
yes
what is GLDH/GDH? what does its presence indcate?
glutamate dehydrogenase
indicates hepatic damage in horses, dogs, cats
what is LDH and what does it indicate?
lactase dehydrogenase
indicates hepatic/muscle damage, but is not very important for the liver.
what is arginase, and what does it indicate?
an enzyme that's presence is hepatospecific
what are the clinical signs that align with cholestasis?
abdominal pain and vomiting
what is the difference between a pancreatic or bile duct injury in dogs and cats?
cats suffer more because the bile and pancreatic duct share a papilla, so any problem in the pancreas or bile duct will cause problems to the other, + the intestines
what is triaditis?
a condition in cats where the liver/gallbladder, pancreas, and intestines are all diseased
what are causes of cholestasis?
biliary obstruction, due to inflammation, choleliths, thickened bile, etc.
it can be intra or extra hepatic, but we cannot distinguish which based on a biochemistry analysis
what is ALKP/ALP? what does its presence mean?
alkaline phosphatase
it is present in the liver, bone, placenta, renal cortex, and intestinal mucosa. its increase indicates cholestasis (if there is also increased ALT), glucocorticoids, bone disease, or is normal in young animals.
it is in horses, dogs, and cats.
if there is an increase in ALKP/ALP, what does this mean?
cholestasis- if there is also increased ALT
glucocorticoids
bone disease
young animals- due to osteoclastic activity
what is GGT? what does it indicate?
Gamma glutamyl transferase
it is in the membrane of the biliary epithelial cells, and also in the pancreas, intestine, and kidney. we check the ALKP and ALT to differentiate. its increase usually indicates cholestasis
an increase in GGT indicates...
cholestasis, if the ALKP and ALT are also increased.
however, it is also present in the pancreas, intestine, and kidney.
what is the difference between hepatopathy and hepatic insufficiency?
hepatopathy- liver disease
hepatic insufficiency- the liver cannot function properly. >70% of the parenchyma is impaired.
what is hepatic insufficiency?
the liver cannot function properly, and more than 70% of the parenchyma is functionally impaired. the liver loses its ability to conjugate and excrete bilirubin. it also cannot synthesize albumin, glucose, BUN, cholesterol, and clotting factors.
which is a worse prognosis- the presence of cytosolic or non-cytosolic liver enzymes in the blood?
cytosolic, because this means that the injury is more severe, involving destruction of the entire hepatocyte.
cytosolic enzymes include: ALT, AST, GLDH, LDH, arginase
what enzymes are located in the heptatocytic cytosol?
ALT, AST, GLDH, LDH, arginase
what enzymes are located on the heptatocytic membrane (non-cytosolic)?
GGT, FAL
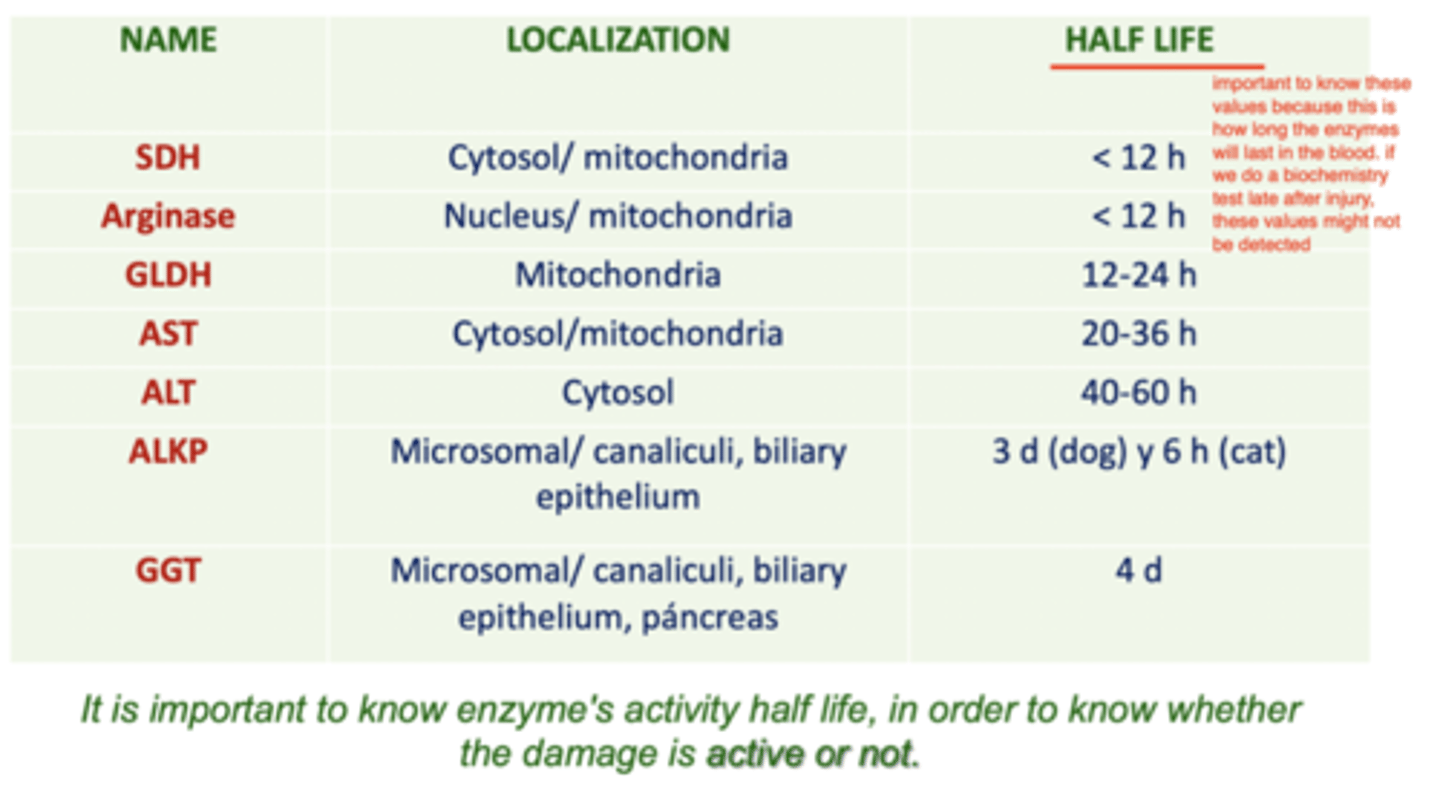
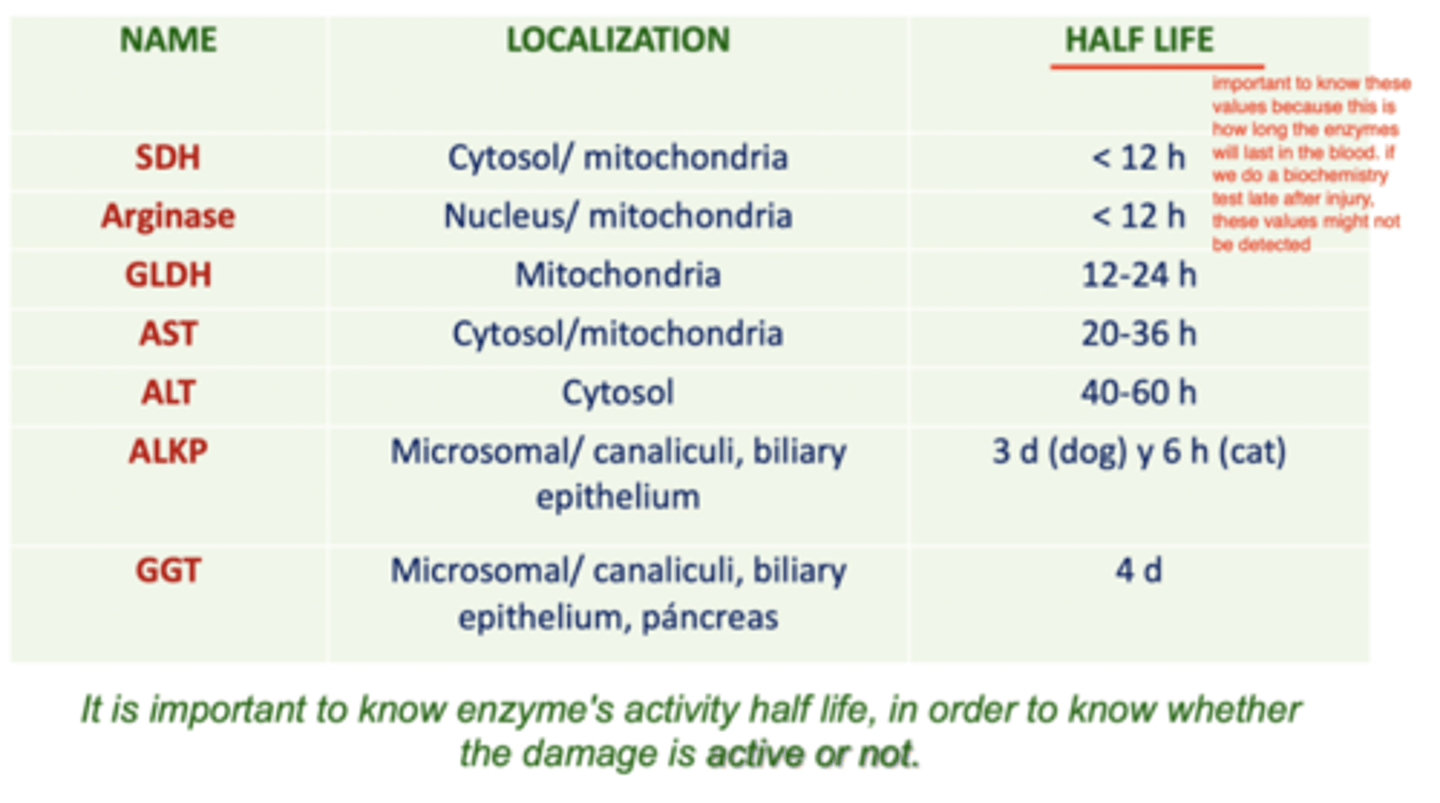
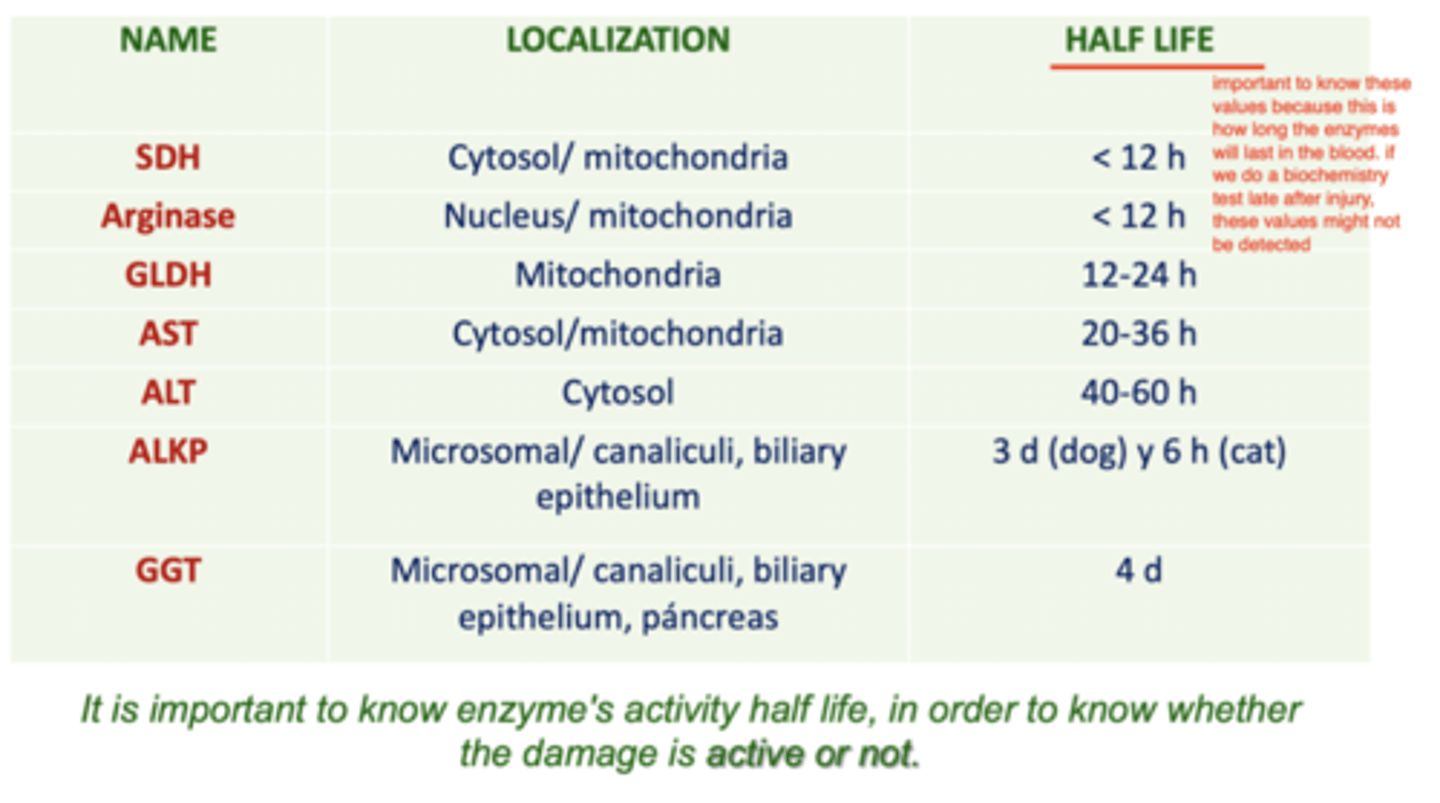
why is it important to know the half-life of the enzymes that we are measuring?
because this is how long the enzymes last in the blood- it can tell us whether the damage is active or not.
these values may not be detected if we do the biochemistry analysis too late
what are the 3 possible origins of bilirubin in the blood?
1. hemolysis
2. heme protein catabolism
3. BM erythropoiesis

what may be causes of hyperbilirubinemia?
RBC destruction- prehepatic
alteration of bilirubin capture in the liver- hepatic
alteration of bilirubin conjugation in the liver- hepatic
bile flow obstruction- post hepatic
what type of bilirubin- conjugated or unconjugated, will be increased if there is RBC destruction?
unconjugated
what is pre-hepatic bilirubinemia?
bilirubinemia due to RBC destruction.
there will be an increase in unconjugated bilirubin (but then chronically, increased conjugated)
what are the 2 types of hepatic bilirubinemia?
alteration of bilirubin capture in the liver
alteration of bilirubin conjugation
both are due to liver damage, and we will see an increase of both conjugated and unconjugated bilirubin
what are the types of bilirubinemia/jaundice?
prehepatic- RBC destruction
hepatic- liver damage
post hepatic- bile flow obstruction
what is post hepatic bilirubinemia?
bilirubinemia due to bile flow obstruction. there will be an INTENSE bilirubinuria. and an increase in both conjugated and unconjugated bilirubinemia.
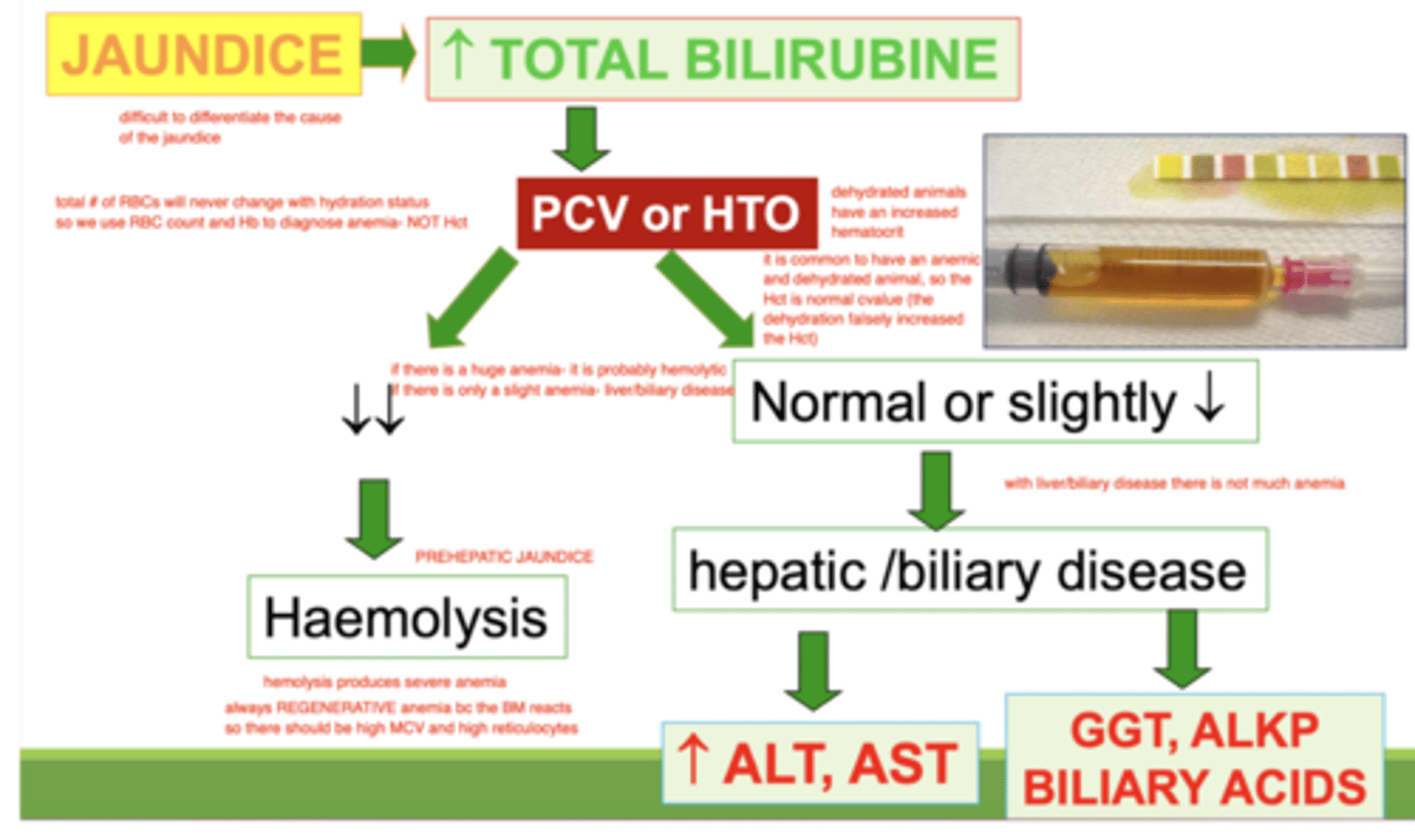
how can we differentiate the type of jaundice?
hemolysis: decreased PCV/Hct
hepatic disease: normal PCV, increased ALT and AST
biliary disease: normal PCV, increased GGT, ALKP, or biliary acids
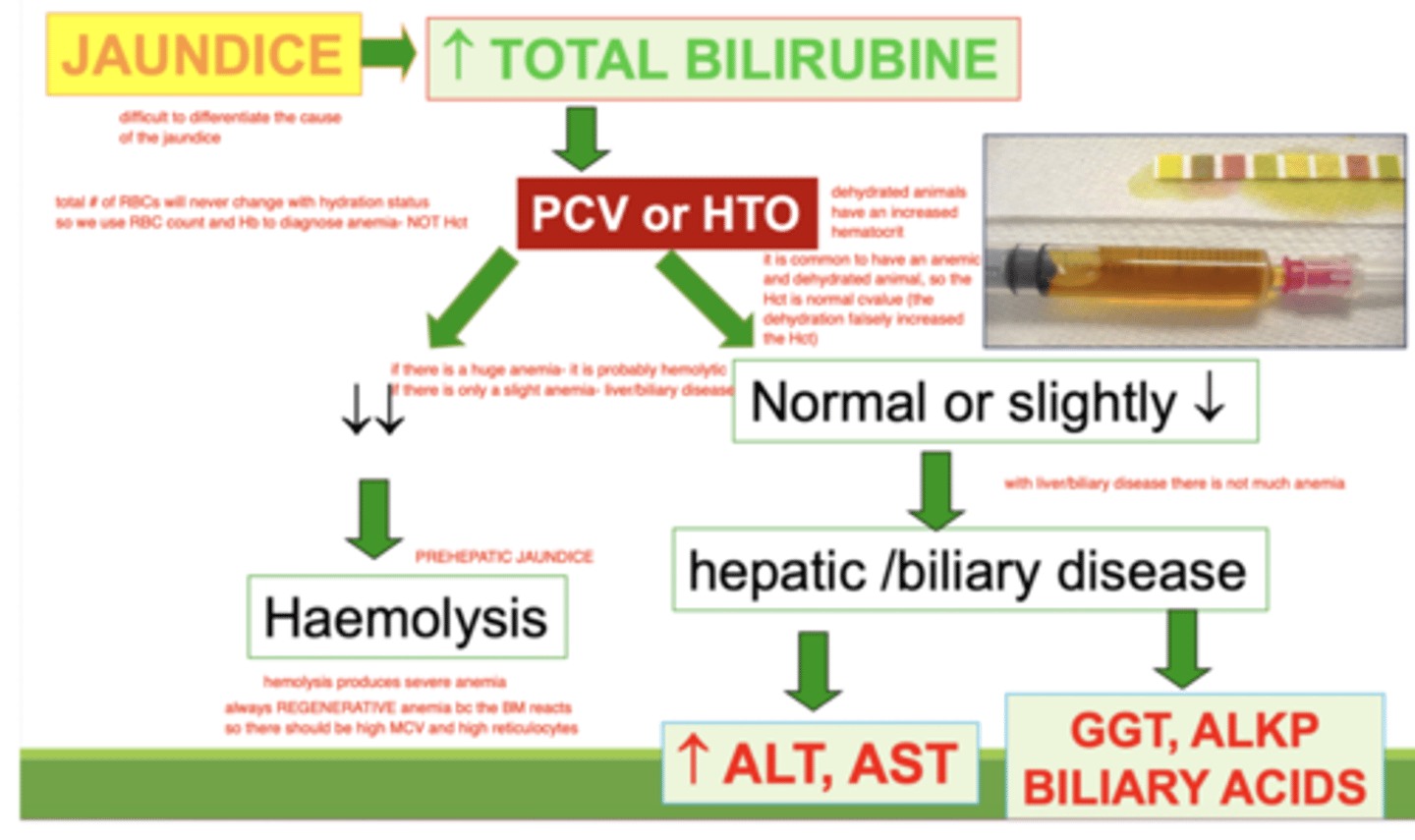
if there is jaundice and a decreased PCV in the hemogram, what do we determine is the cause?
hemolysis
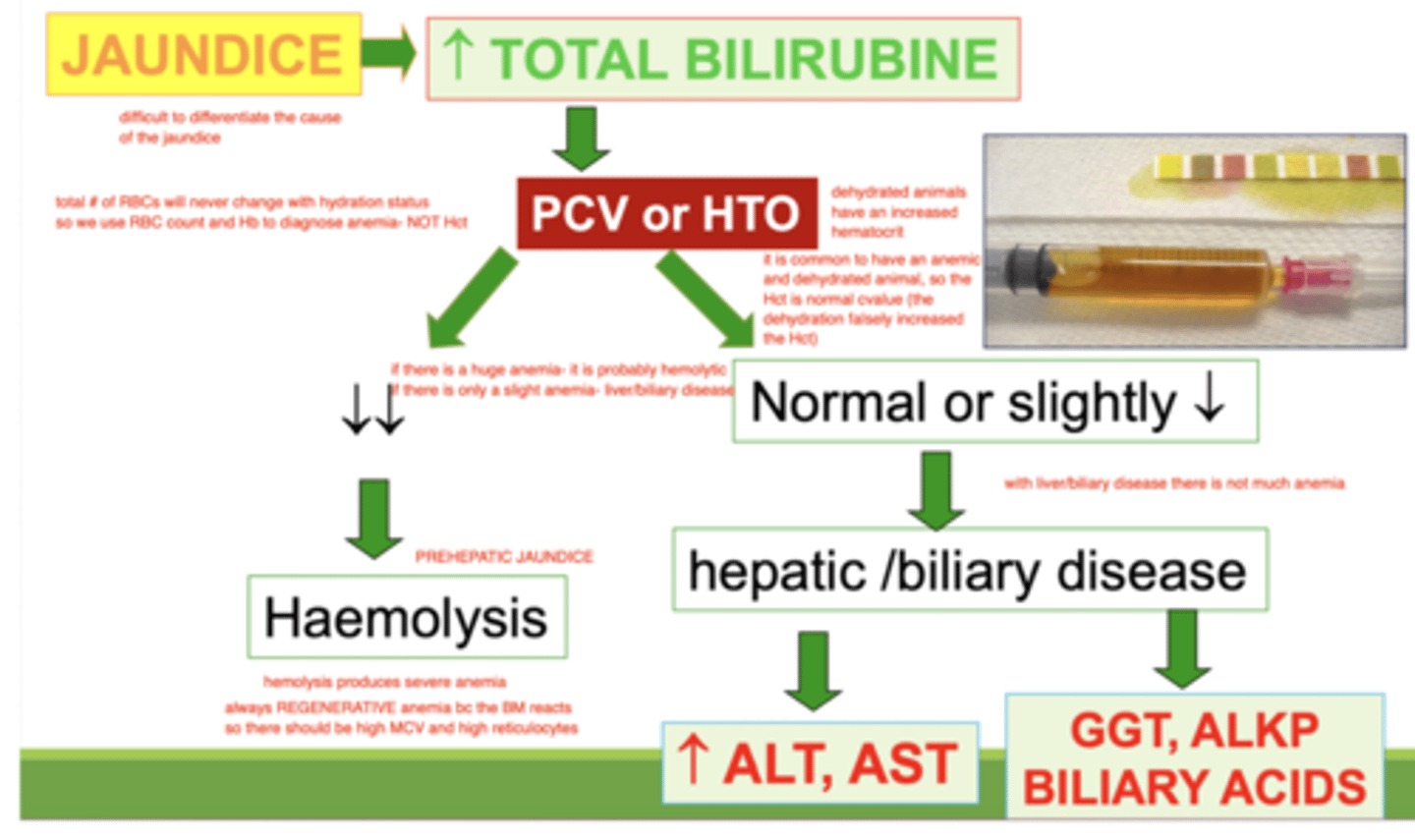
if there is jaundice and a normal PCV in the hemogram, what do we determine is the cause?
liver or bile disease
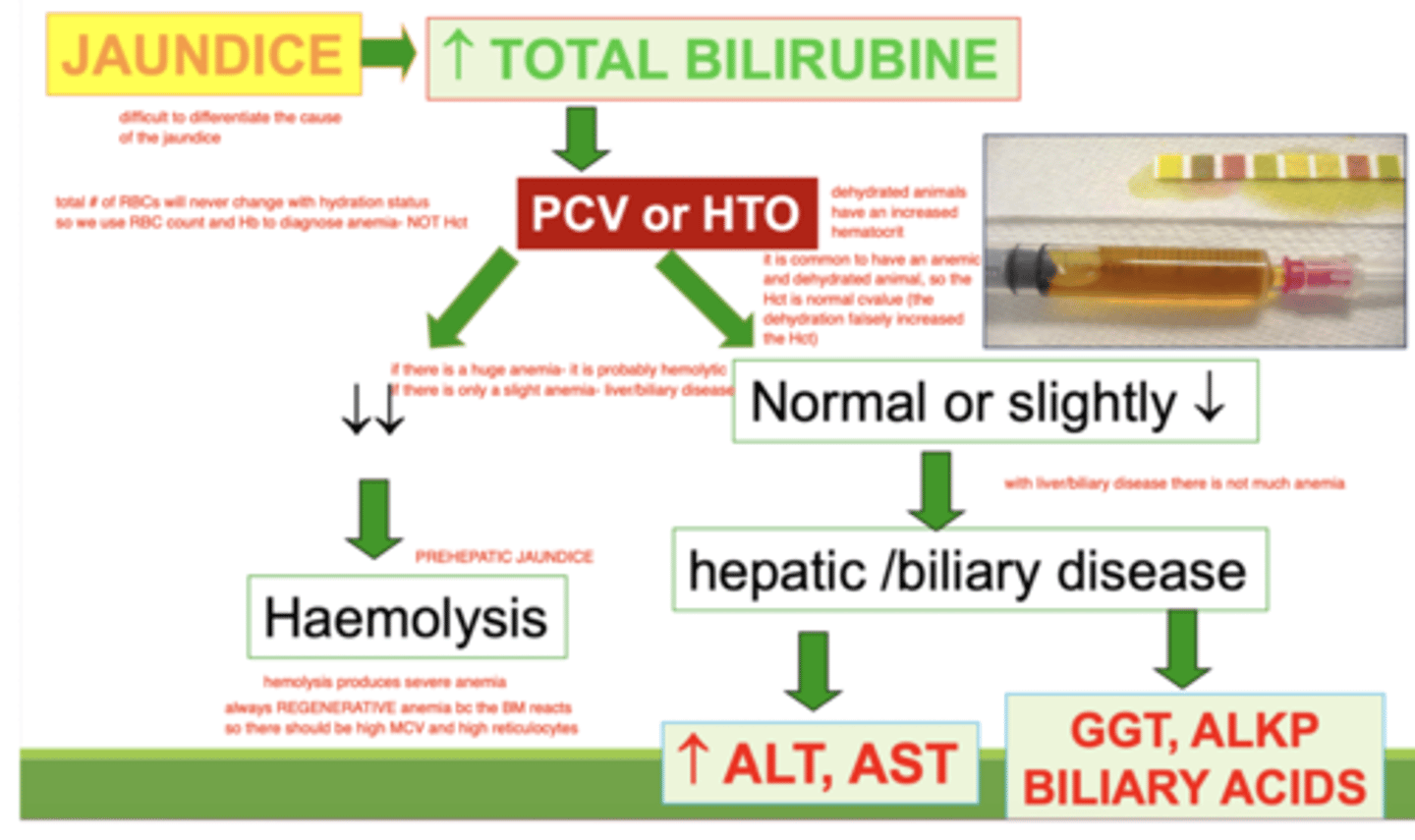
if an animal with jaundice has an increased ALT and/or AST, what is the problem?
hepatic disease
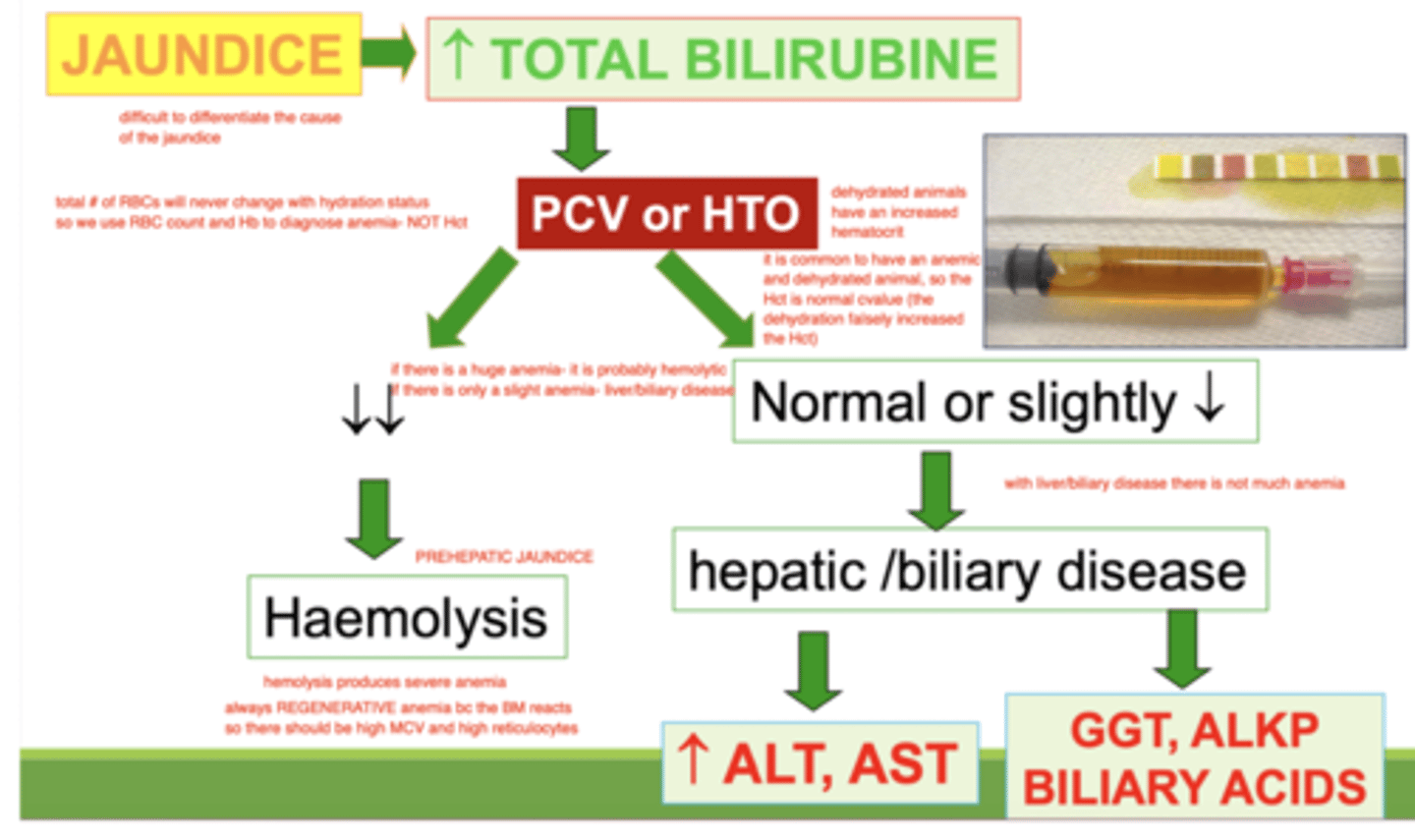
if an animal has jaundice and in the biochemistry results, there is an increased GGT and/or ALKP, what is the problem?
biliary disease
what are bile acids?
amphipathic steroids, synthesized from cholesterol by hepatocytes. they are excreted into the bile and have the function of emulsifying fats in the intestine and facilitating nutrient absorption. they are highly conserved via enterohepatic circulation.
if we measure that the bile acids are very increased, what could be the problem?
cholestasis
how does cholestasis affect the bile acids levels on a biochemistry analysis?
they will be increased by >5x
a decreased value of bile acids indicates:
liver problem (neoplasia, lipidosis, hepatopathy, shunt, etc)
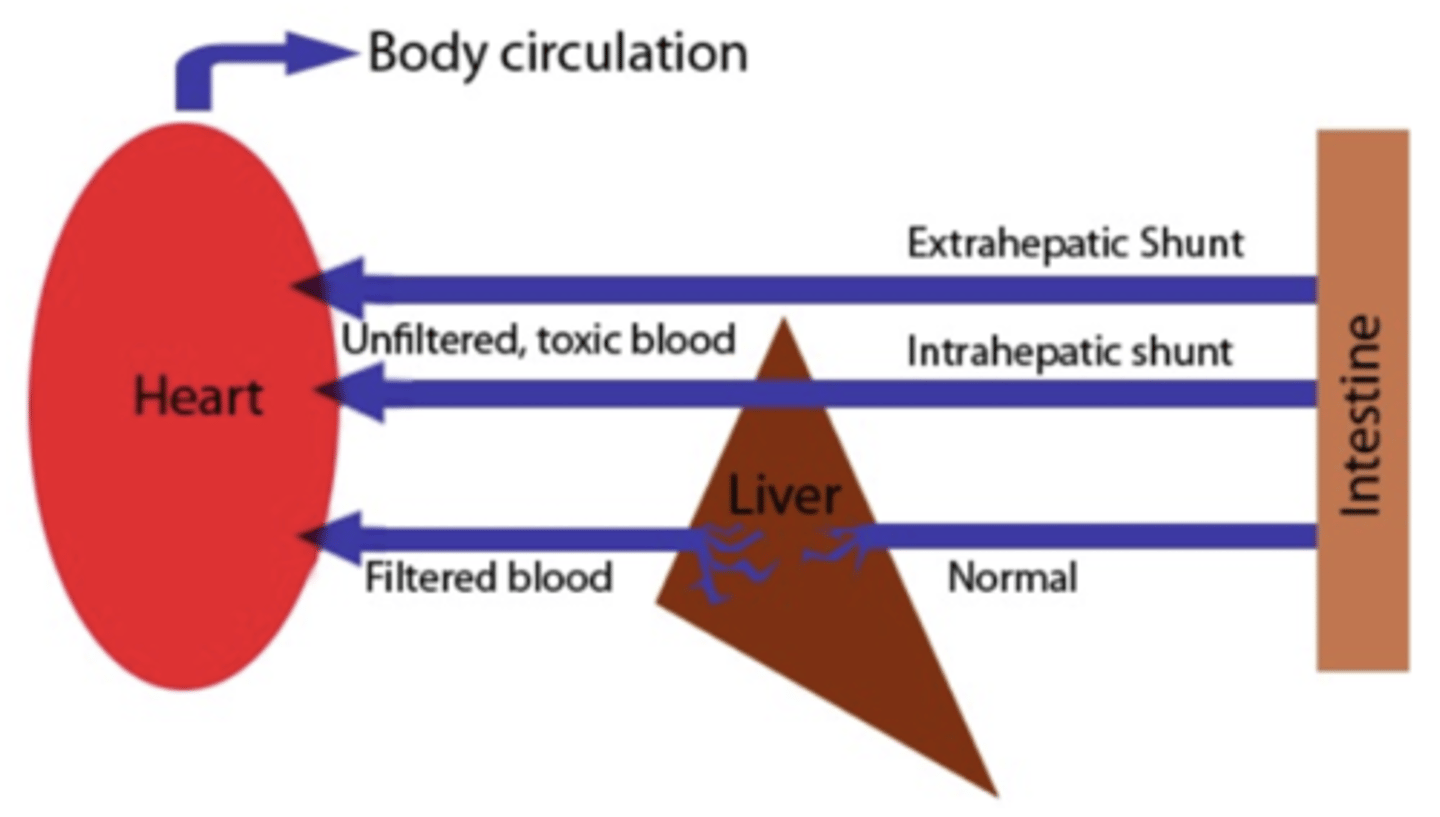
what is a shunt?
a congenital disease of a connection between a vein and an artery. the animal will get intoxicated because venous blood flows to the arterial circulation and into tissues without being "cleaned" by the liver first.
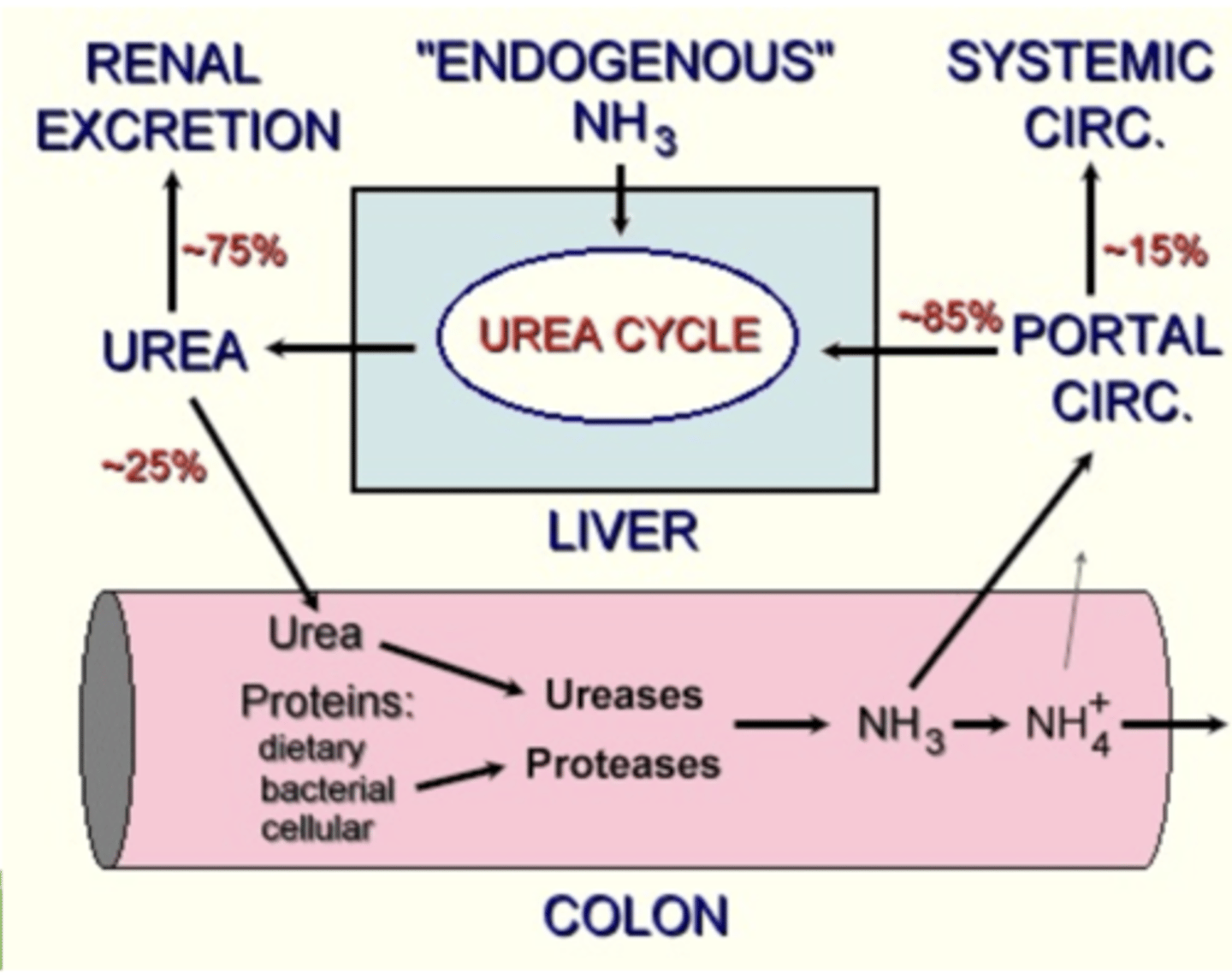
hyperammonemia can be caused by...
hepatic insufficiency
urea cycle enzyme deficiency
if on the biochemistry analysis we see an elevated amount of ammonium (hyperammonemia), what do we expect to see in the urinalysis?
ammonium biurate crystals
is ammonium present in the blood under normal conditions?
a small amount is normal.
this is because although most urea goes to the kidney, 25% goes to the colon and from there can enter the portal circulation.
if there is hyperalbuminemia, what does this mean?
at least 60% of the liver parenchyma is affected
a decrease in blood albumin levels means:
hepatic insufficiency
what does an increased amount of globulins in the blood indicate?
cirrhosis
advanced hepatic illness
neoplasia
if the BUN (urea) is increased in the blood, but the creatinine remains normal, what does this mean?
the animal is dehydrated
if both the BUN and creatinine levels are increased, what is the problem?
renal failure
this is called azotemia
what is azotemia?
increased BUN and creatinine in the blood. indicates renal failure
if there is decreased BUN in the blood, what is the problem?
hepatic insufficiency
what does an increased blood cholesterol content indicate?
cholestasis
a decreased blood cholesterol means...
cirrhosis
increased triglycerides in the blood means ________________, while decreased levels means _______________-
increased- biliary obstruction
decreased- chronic hepatitis
if the amount of clotting factors in the blood is decreased, this can indicate:
cholestasis
hepatopathy
to check the capacity of the liver to synthesize, what values should we analyze in a biochemistry exam?
albumin
urea
cholesterol
clotting factors
glucose
to check the capacity of the liver to uptake, conjugate, and secrete bilirubin, what values should we analyze in a biochemistry exam?
bilirubin
to check the capacity of the liver to clear and perform the enterohepatic circulation, what values should we analyze in a biochemistry exam?
ammonia
bile acids
what is the best indicator enzyme for muscle damage?
creatinine kinase (CK)
what is creatinine kinase (CK)?
an enzyme that is very specific of muscle damage. if the muscle is damaged, there will be an increase of CK and AST.
it has a short half life, so if appearing in a blood test, there is an active lesion. if present, the hemolysis values will falsely increase by 6-8x
what enzymes can we check to evaluate muscle damage?
CK (+ AST)
LDH-5
where is LDH-5 in the body?
liver, kidney, WBC, RBC, muscle
what is creatorrhea?
undigested meat in the feces

what is amylorrhea?
undigested starch in the feces

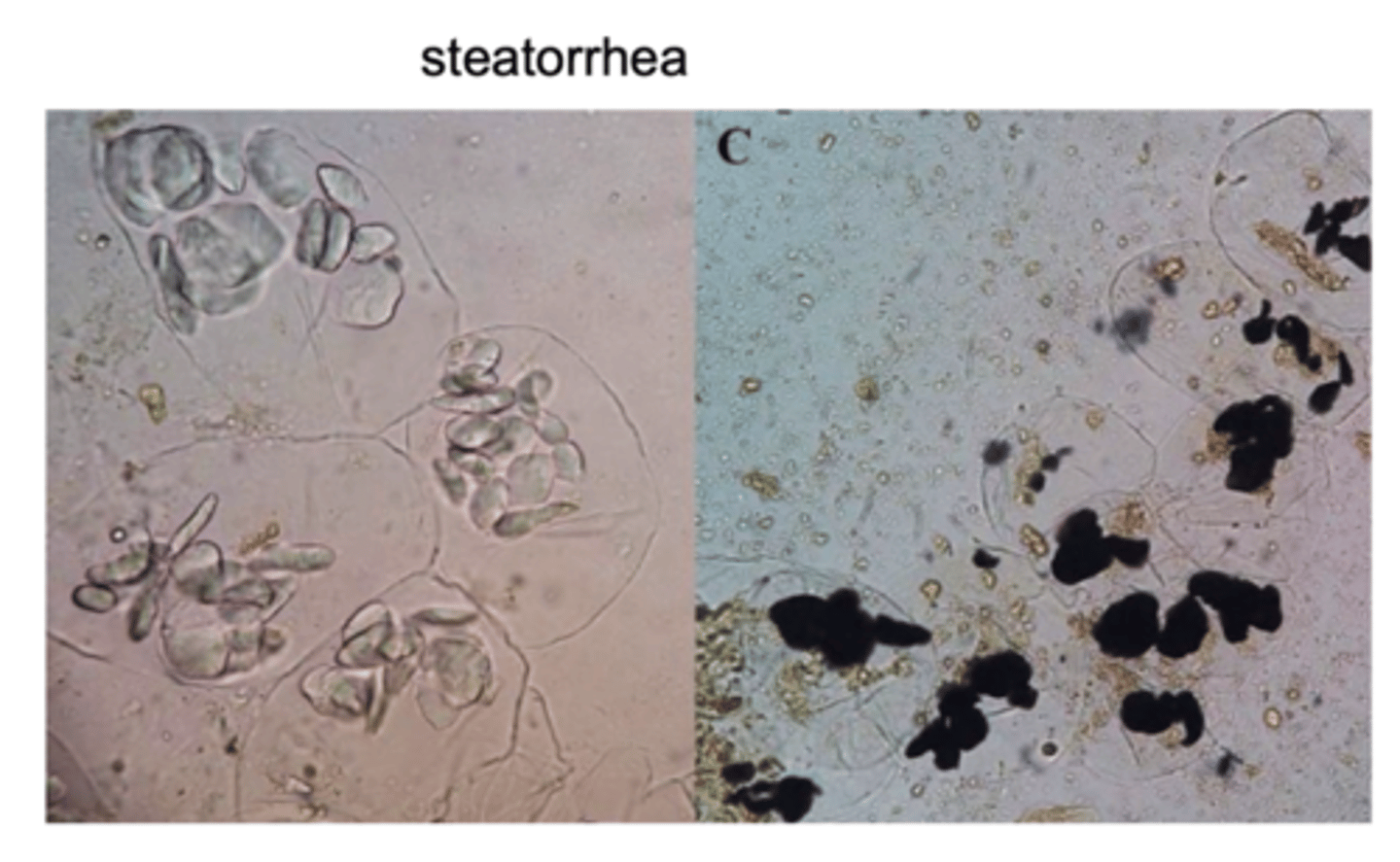
what is steatorrhea?
undigested fat in the feces.
the feces appears yellow and pasty
if the amylase values are increased, what does this indicate?
pancreatitis
abscesses
obstructions of the pancreatic duct
renal failure
IN DOGS ONLY!
in what animal do we use amylase to evaluate the pancreatic function?
dogs
if a dog has pancreatitis, what 2 values to we expect to increase?
lipase and amylase
(increased by 3-4x)
if a dog's lab results show an increase lipase and amylase, what is probably the issue?
pancreatitis
what do we use lipase values to evaluate?
pancreatitis
GI disease
renal insufficiency
only in dogs
what is TLI?
trypsin-like immunoreactivity
it is a good pancreatic marker for cats and dogs. it detects the trypsinogen and serum trypsin by immunoreactivity.
what does it mean if in a dog, the TLI is >50 micrograms/liter?
pancreatitis
(or decreased renal excretion, corticoids, food ingestion)
what does it mean if in a cat, the TLI is >100 micrograms/liter?
pancreatitis
(or decreased renal excretion, corticoids, food ingestion)
what does a decreased TLI mean?
exocrine pancreatic insufficiency (EPI).
it is a result of chronic pancreatitis, but can be congenital in some dog breeds (especially german shepherds)
what is EPI?
exocrine pancreatic insufficiency
it is a result of chronic pancreatitis, but can be congenital in some dog breeds (especially german shepherds).
the TLI will be low.
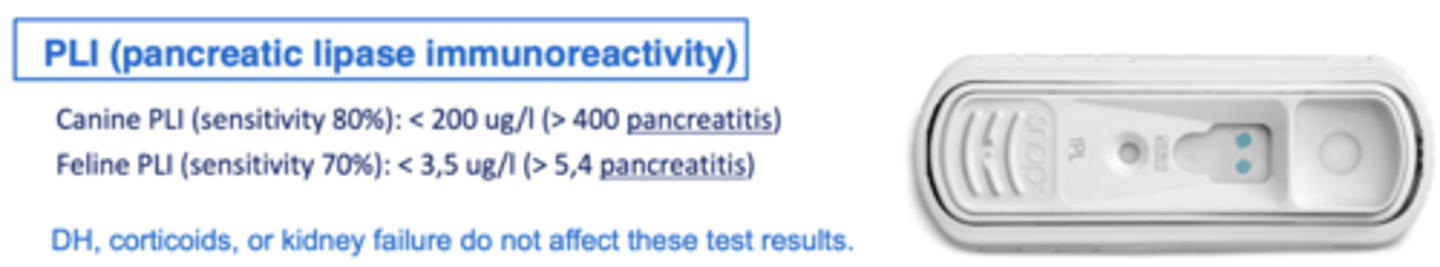
what is PLI?
pancreatic lipase immunoreactivity.
it is the gold standard test to check for pancreatitis.

what is the best test to test if a dog/cat has pancreatitis?
PLI (pancreatic lipase immunoreactivity)
what is the best test to use to check for EPI (exocrine pancreatic insufficiency)?
TLI