2. Thyroid Gland & Disorders
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
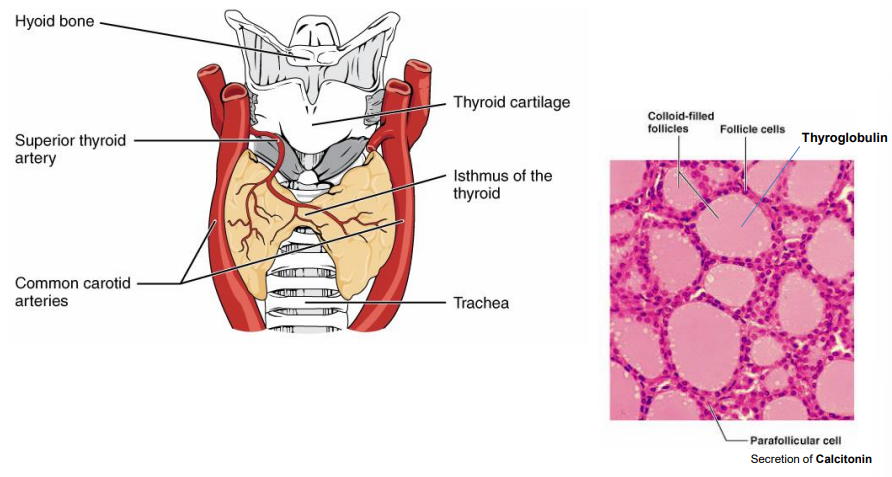
What is the structure of the thyroid gland & its hormone-related cells?
2 lobes beside trachea, linked by isthmus
Made of colloid-filled follicles with follicular cells
Follicular cells use thyroglobulin to make thyroid hormones
Parafollicular (C) cells secrete calcitonin to regulate calcium
How is thyroid hormone release regulated?
Hypothalamus releases TRH → stimulates anterior pituitary
Anterior pituitary releases TSH → stimulates thyroid follicular cells
Thyroid releases T4 → converted to active T3
↑T3 triggers negative feedback on pituitary → ↓TSH
No direct feedback from T3/T4 to hypothalamus, only to pituitary
How are thyroid hormones T3 & T4 synthesised & how do they act?
Thyroglobulin (prohormone) secreted by follicular cells into follicle
Iodine enters via Na⁺/I⁻ pump & binds thyroglobulin → forms T3 & T4
T3 & T4 enter blood → T4 converted to active T3
T3 enters nucleus, binds receptor → triggers protein synthesis & cell response
What is the role of thyroid hormones in metabolism?
↑ Basal Metabolic Rate (BMR) in all tissues
Carb metabolism: ↑ sensitivity to catecholamines, insulin & GH; ↑ gluconeogenesis, glycogenolysis & glucose use
Protein metabolism: low T3/T4 = protein synthesis; high T3/T4 = protein breakdown & weight loss
Fat metabolism: ↑ lipolysis, ↑ liver uptake of cholesterol = ↓ plasma cholesterol
What is the role of thyroid hormones in thermoregulation (calorigenesis)?
↑ O₂ consumption in most tissues (except brain, spleen, testes)
↑ heat production via ↑ Na⁺/K⁺ ATPase activity
What is the role of thyroid hormones in CNS maturation?
Essential for brain development during late foetal & early postnatal life
What is the role of thyroid hormones in skeletal growth & maturation?
Essential for normal bone growth, maturation & development of adult stature
Supports development of CVS, GI tract, teeth, skin & hair follicles
What are the causes of hypothyroidism?
Surgical removal (e.g. partial thyroidectomy)
Radioactive iodine (¹³¹I) treatment
Pituitary or hypothalamic disease → ↓ TSH
Iodine deficiency due to low dietary intake
Autoimmune thyroiditis (e.g. Hashimoto’s)
What are the features, diagnosis & treatment of congenital hypothyroidism (cretinism if untreated)?
Features: dwarfism, protruding tongue & abdomen, mental retardation, coarse scanty hair, dry yellowish skin
Diagnosis: TSH assay from heel-prick blood sample
Treatment: thyroxine replacement therapy
What are the features and treatment of juvenile hypothyroidism?
Features: stunted growth, delayed sexual development, mental retardation
Treatment: thyroxine replacement therapy
What are the causes, symptoms, and treatment of adult hypothyroidism (Hashimoto's thyroiditis)?
Causes: autoimmune destruction of the thyroid gland
Symptoms:
Painful swelling (goitre)
Low BMR (slow bodily processes, slow movements)
Weight gain, cold intolerance
Decreased sweating, constipation
Myxoedema (hair loss)
Fatigue, memory impairment, depression, slow speech
Bradycardia
Yellowish skin (due to increased plasma carotene)
Low serum T3/T4, high TSH, and possible elevated plasma cholesterol
Treatment: lifelong thyroxine replacement (Levothyroxine sodium, Liothyronine sodium)
What are the causes of hyperthyroidism?
Excess thyroid hormone intake (thyrotoxicosis factitia)
Follicular thyroid carcinoma
Amiodarone treatment
Primary hyperthyroidism (Graves’ disease – autoimmune)
What are the causes, symptoms, and hormonal findings in hyperthyroidism (Graves’ disease)?
Causes: thyroid-stimulating immunoglobulins bind to TSH receptors
Symptoms:
High BMR → heat intolerance, warm skin, excessive sweating
Weight loss
Palpitations, tachycardias
Restlessness, anxiety, irritability
Exophthalmos (eye changes)
Diffuse toxic goitre
Hormonal findings: high serum T3/T4, low serum TSH
What are the treatment options for Graves’ disease?
Antithyroid drugs
Radioactive iodine
Surgery
What are the treatment options for Graves’ disease & their key features?
Antithyroid drugs:
Carbimazole, Propylthiouracil (PTU)
Used for long-term treatment, pre-radioiodine & pre-surgery
Side effects: agranulocytosis (↓ WBC, flu-like symptoms), hepatotoxicity
Lugol’s iodine (aqueous iodine solution BP):
5% iodine in 10% potassium iodide
Used pre-surgery to ↓ thyroid size & vascularisation
β-adrenoceptor blockers:
Propranolol, nadolol, sotalol
Symptomatic relief (↓ palpitations & arrhythmias)
How does radioactive iodine (¹³¹I) treat Graves’ disease & what are the precautions?
Given orally as Na¹³¹I solution
Selectively destroys overactive thyroid tissue via local irradiation
Acts over 1–6 months
Patient must be euthyroid before treatment (i.e. must first be stabilised on antithyroid drugs to normalise T₃/T₄ levels)
Contraindicated in pregnancy & very young children
When is partial thyroidectomy used to treat Graves’ disease & what are the requirements?
Used when antithyroid drugs or radioiodine aren't suitable
It's a demanding surgical procedure
Patient must be euthyroid before surgery (i.e. stabilised on antithyroid drugs to normalise T₃/T₄ levels)